Calcium channel blocker
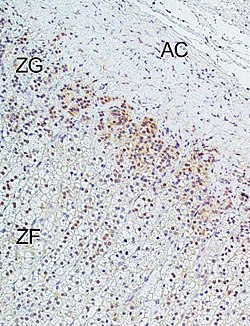
Calcium channel blockers (CCB), calcium channel antagonists or calcium antagonists[1] are several medications that disrupt the movement of calcium (Ca2+) through calcium channels.[2] Calcium channel blockers are used as antihypertensive drugs, i.e., as medications to decrease blood pressure in patients with hypertension. CCBs are particularly effective against large vessel stiffness, one of the common causes of elevated systolic blood pressure in elderly patients.[3] Calcium channel blockers are also frequently used to alter heart rate, to prevent cerebral vasospasm, and to reduce chest pain caused by angina pectoris. N-type, L-type, and T-type voltage-dependent calcium channels are present in the zona glomerulosa of the human adrenal, and CCBs can directly influence the biosynthesis of aldosterone in adrenocortical cells, with consequent impact on the clinical treatment of hypertension with these agents.[4]
Despite their effectiveness, CCB's often have a high mortality rate over extended periods of use, and have been known to have multiple side effects.[5] Potential major risks however were mainly found to be associated with short-acting CCBs.[6]
Classes
Dihydropyridine
Dihydropyridine (DHP) calcium channel blockers are derived from the molecule dihydropyridine and often used to reduce systemic vascular resistance and arterial pressure. Sometimes when they are used to treat angina, the vasodilation and hypotension can lead to reflex tachycardia, which can be detrimental for patients with ischemic symptoms because of the resulting increase in myocardial oxygen demand. Dihydropyridine calcium channel blockers can worsen proteinuria in patients with nephropathy.[7]
This CCB class is easily identified by the suffix "-dipine".
- Amlodipine (Norvasc)
- Aranidipine (Sapresta)
- Azelnidipine (Calblock)
- Barnidipine (HypoCa)
- Benidipine (Coniel)
- Cilnidipine (Atelec, Cinalong, Siscard) Not available in US
- Clevidipine (Cleviprex)
- Isradipine (DynaCirc, Prescal)
- Efonidipine (Landel)
- Felodipine (Plendil)
- Lacidipine (Motens, Lacipil)
- Lercanidipine (Zanidip)
- Manidipine (Calslot, Madipine)
- Nicardipine (Cardene, Carden SR)
- Nifedipine (Procardia, Adalat)
- Nilvadipine (Nivadil)
- Nimodipine (Nimotop) This substance can pass the blood-brain barrier and is used to prevent cerebral vasospasm.
- Nisoldipine (Baymycard, Sular, Syscor)
- Nitrendipine (Cardif, Nitrepin, Baylotensin)
- Pranidipine (Acalas)
Side effects of these drugs may include but are not limited to:
- Dizziness, headache, redness in the face
- Fluid buildup in the legs and ankle edema
- Rapid heart rate
- Slow heart rate
- Constipation
- Gingival overgrowth
Non-Dihydropyridine
Phenylalkylamine

Phenylalkylamine calcium channel blockers are relatively selective for myocardium, reduce myocardial oxygen demand and reverse coronary vasospasm, and are often used to treat angina. They have minimal vasodilatory effects compared with dihydropyridines and therefore cause less reflex tachycardia, making it appealing for treatment of angina, where tachycardia can be the most significant contributor to the heart's need for oxygen. Therefore, as vasodilation is minimal with the phenylalkylamines, the major mechanism of action is causing negative inotropy. Phenylalkylamines are thought to access calcium channels from the intracellular side, although the evidence is somewhat mixed.[8]
- Verapamil (Calan, Isoptin)
- Gallopamil
- Fendiline
Benzothiazepine

Benzothiazepine calcium channel blockers belong to the benzothiazepine class of compounds and are an intermediate class between phenylalkylamine and dihydropyridines in their selectivity for vascular calcium channels. By having both cardiac depressant and vasodilator actions, benzothiazepines are able to reduce arterial pressure without producing the same degree of reflex cardiac stimulation caused by dihydropyridines.
- Diltiazem (Cardizem) (also used experimentally to prevent migraine)
Nonselective
While most of the agents listed above are relatively selective, there are additional agents that are considered nonselective. These include mibefradil, bepridil, flunarizine (BBB crossing), fluspirilene (BBB crossing),[9] and fendiline.[10]
Others
Gabapentinoids, such as gabapentin and pregabalin, are selective blockers of α2δ subunit-containing voltage-gated calcium channels. They are used primarily to treat epilepsy and neuropathic pain.
Ziconotide, a peptide compound derived from the omega-conotoxin, is a selective N-type calcium channel blocker that has potent analgesic properties that are equivalent to approximate 1,000 times that of morphine. It must be delivered via the intrathecal (directly into the cerebrospinal fluid) route via an intrathecal infusion pump.
Toxicity
Mild CCB toxicity is treated with supportive care. Non-dihydropyridine CCB may produce profound toxicity and early decontamination, especially for slow release agents, is essential. For severe overdoses, treatment usually includes close monitoring of vital signs and the addition of vasopressive agents and intravenous fluids for blood pressure support. IV calcium gluconate (or calcium chloride if a central line is available) and atropine are first-line therapies. If the time of the overdose is known and presentation is within two hours of ingestion, activated charcoal, gastric lavage, and polyethylene glycol may be used to decontaminate the gut. Efforts for gut decontamination may be extended to within 8 hours of ingestion with extended release preparations.
Hyperinsulinemia-euglycemia (HIE) therapy has emerged as a viable form of treatment. Although the mechanism is unclear, it has been hypothesized that increased insulin mobilizes glucose from peripheral tissues to serve as an alternative fuel source for the heart (the heart mainly relies on oxidation of fatty acids). Theoretical treatment with lipid emulsion therapy has been considered in severe cases, but is not yet standard of care.
Caution should be taken when using verapamil with a Beta blocker due to the risk of severe bradycardia. If unsuccessful, ventricular pacing should be used.[11]
Mechanism of action

In the body's tissues, the concentration of calcium ions (Ca2+) outside of cells is normally about ten-thousand-fold higher than the concentration inside of cells. Embedded in the membrane of some cells are calcium channels. When these cells receive a certain signal, the channels open, letting calcium rush into the cell. The resulting increase in intracellular calcium has different effects in different types of cells. Calcium channel blockers prevent or reduce the opening of these channels and thereby reduce these effects.
There are several types of calcium channels, and a number of classes of calcium channel blockers, but almost all of them preferentially or exclusively block the L-type voltage-gated calcium channel.[12]
Voltage-dependent calcium channels are responsible for excitation-contraction coupling of skeletal, smooth, and cardiac muscle and for regulating aldosterone and cortisol secretion in endocrine cells of the adrenal cortex.[4] In the heart they are also involved in the conduction of the pacemaker signals. CCBs used as medications primarily have four effects:
- by acting on vascular smooth muscle they reduce contraction of the arteries and cause an increase in arterial diameter, a phenomenon called vasodilation (CCBs do not work on venous smooth muscle)
- by acting on cardiac muscles (myocardium), they reduce the force of contraction of the heart
- by slowing down the conduction of electrical activity within the heart, they slow down the heart beat.
- by blocking the calcium signal on adrenal cortex cells, they directly reduce aldosterone production, which corroborates to lower blood pressure.
Since blood pressure is in intimate feedback with cardiac output and peripheral resistance, with relatively low blood pressure, the afterload on the heart decreases; this decreases how hard the heart must work to eject blood into the aorta, and so the amount of oxygen required by the heart decreases accordingly. This can help ameliorate symptoms of ischaemic heart disease such as angina pectoris.
Reducing the force of contraction of the myocardium is known as the negative inotropic effect of calcium channel blockers. Slowing down the conduction of electrical activity within the heart, by blocking the calcium channel during the plateau phase of the action potential of the heart (see: cardiac action potential), results in a negative chronotropic effect, or a lowering of heart rate. This can increase the potential for heart block. The negative chronotropic effects of calcium channel blockers make them a commonly used class of agents in individuals with atrial fibrillation or flutter in whom control of the heart rate is generally a goal. Negative chronotropy can be beneficial when treating a variety of disease processes because lower heart rates represent lower cardiac oxygen requirements. Elevated heart rate can result in significantly higher "cardiac work," which can result in symptoms of angina.
The class of CCBs known as dihydropyridines mainly affect arterial vascular smooth muscle and lower blood pressure by causing vasodilation. The phenylalkylamine class of CCBs mainly affect the cells of the heart and have negative inotropic and negative chronotropic effects. The benzothiazepine class of CCBs combine effects of the other two classes.
It is because of the negative inotropic effects that the nondihydropyridine calcium channel blockers should be avoided (or used with caution) in individuals with cardiomyopathy.[13]
Unlike beta blockers, calcium channel blockers do not decrease the responsiveness of the heart to input from the sympathetic nervous system. Since moment-to-moment blood pressure regulation is carried out by the sympathetic nervous system (via the baroreceptor reflex), calcium channel blockers allow blood pressure to be maintained more effectively than do beta blockers. However, because dihydropyridine calcium channel blockers result in a decrease in blood pressure, the baroreceptor reflex often initiates a reflexive increase in sympathetic activity leading to increased heart rate and contractility.
Ionic calcium is antagonized by magnesium ions in the nervous system. Because of this, bioavailable supplements of magnesium, possibly including magnesium chloride, magnesium lactate, and magnesium aspartate, may increase or enhance the effects of calcium channel blockade.[14]
N-type calcium channels are found in neurons and are involved in the release of neurotransmitter at synapses. Ziconotide is a selective blocker of these calcium channels and acts as an analgesic.
History
Calcium channel blockers were first identified in the lab of German pharmacologist Albrecht Fleckenstein beginning in 1964.[15]
See also
References
- ^ Olson, Kent (2011). "Calcium Channel Antagonists". Poisoning & drug overdose (6th ed. ed.). New York: McGraw-Hill Medical. pp. Chapter 40. ISBN 0071668330.
{{cite book}}:|edition=has extra text (help) - ^ "calcium channel blocker" at Dorland's Medical Dictionary
- ^ Nelson M (2010). "Drug treatment of elevated blood pressure" (pdf). Australian Prescriber. 33 (4): 108–112.
- ^ a b c Felizola SJA, Maekawa T, Nakamura Y, Satoh F, Ono Y, Kikuchi K, Aritomi S, Ikeda K, Yoshimura M, Tojo K, Sasano H. (2014). "Voltage-gated calcium channels in the human adrenal and primary aldosteronism". J Steroid Biochem Mol Biol. 144 (part B): 410–416. doi:10.1016/j.jsbmb.2014.08.012. PMID 25151951.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ "Calcium Channel Blockers". MedicineNet. p. 2.
- ^ Norman M Kaplan, MD; Burton D Rose, MD (Apr 3, 2000). "Major side effects and safety of calcium channel blockers". Chinese Medical & Biological Information.
- ^ Remuzzi G, Scheppati A, Ruggenenti P (2002). "Clinical Practice. Nephropathy in Patients with Type 2 Diabetes". New England Journal of Medicine. 346 (15): 1145–1151. doi:10.1056/NEJMcp011773. PMID 11948275.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Hockerman, G.H.; Peterson, B.Z.; Johnson, B.D.; Catterall, W.A. (1997). "Molecular Determinants of Drug Binding and Action on L-Type Calcium Channels". Annual Review of Pharmacology and Toxicology. 37: 361–396. doi:10.1146/annurev.pharmtox.37.1.361. PMID 9131258.
- ^ Bezprozvanny I, Tsien RW (1995). "Voltage-Dependent Blockade of Diverse Types of Voltage-Gated Ca2+ Channels Expressed in Xenopus Oocytes by the Ca2+ Channel Antagonist Mibefradil (Ro 40-5967)". Molecular Pharmacology. 48 (3): 540–549. PMID 7565636.
- ^ Scultéty S, Tamáskovits E (1991). "Effect of Ca2+ Antagonists on Isolated Rabbit Detrusor Muscle". Acta Physiologica Hungarica. 77 (3–4): 269–278. PMID 1755331.
- ^ Buckley N, Dawson A, Whyte I (2007). "Calcium Channel Blockers". Medicine. 35 (11): 599–602. doi:10.1016/j.mpmed.2007.08.025.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Yousef; et al. (2005). "The mechanism of action of calcium channel blockers in the treatment of diabetic nephropathy" (PDF). Int J Diabetes & Metabolism. 13: 76–82.
{{cite journal}}: Explicit use of et al. in:|author=(help) - ^ Lehne R (2010). Pharmacology for Nursing Care (7th ed.). St. Louis, Missouri: Saunders Elsevier. p. 505. ISBN 978-1-4160-6249-3.
- ^ Iseri LT, French JH (1984). "Magnesium: Nature's Physiologic Calcium Blocker". American Heart Journal. 108 (1): 188–193. doi:10.1016/0002-8703(84)90572-6. PMID 6375330.
- ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 6339106, please use {{cite journal}} with
|pmid=6339106instead.
External links
- Calcium+Channel+Blockers at the U.S. National Library of Medicine Medical Subject Headings (MeSH)
- Official Adalat (Nifedipine) site, Bayer
- Video - Calcium Channel Blockers
