Niacin
| |||
| Names | |||
|---|---|---|---|
| IUPAC name
pyridine-3-carboxylic acid[1]
| |||
| Systematic IUPAC name
Pyridine-3-carboxylic acid[2] | |||
| Other names
Bionic
Vitamin B3 | |||
| Identifiers | |||
3D model (JSmol)
|
|||
| 3DMet | |||
| 109591 | |||
| ChEBI | |||
| ChEMBL | |||
| ChemSpider | |||
| DrugBank | |||
| ECHA InfoCard | 100.000.401 | ||
| EC Number |
| ||
| 3340 | |||
| KEGG | |||
| MeSH | Niacin | ||
PubChem CID
|
|||
| RTECS number |
| ||
| UNII | |||
CompTox Dashboard (EPA)
|
|||
| |||
| |||
| Properties | |||
| C 6NH 5O 2 | |||
| Molar mass | 123.1094 g mol−1 | ||
| Appearance | White, translucent crystals | ||
| Density | 1.473 g cm−3 | ||
| Melting point | 237 °C; 458 °F; 510 K | ||
| 18 g L−1 | |||
| log P | 0.219 | ||
| Acidity (pKa) | 2.201 | ||
| Basicity (pKb) | 11.796 | ||
| Isoelectric point | 4.75 | ||
Refractive index (nD)
|
1.4936 | ||
| 0.1271305813 D | |||
| Thermochemistry | |||
Std enthalpy of
formation (ΔfH⦵298) |
−344.9 kJ mol−1 | ||
Std enthalpy of
combustion (ΔcH⦵298) |
−2.73083 MJ mol−1 | ||
| Pharmacology | |||
| Intramuscular, Oral | |||
| Pharmacokinetics: | |||
| 20-45 min | |||
| Hazards | |||
| NFPA 704 (fire diamond) | |||
| Flash point | 193 °C | ||
Except where otherwise noted, data are given for materials in their standard state (at 25 °C [77 °F], 100 kPa).
| |||
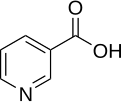
Niacin (also known as vitamin B3, nicotinic acid, or less commonly vitamin PP; archaic terms include pellagra-preventive and anti-dermatitis factor) is an organic compound with the formula C
6H
5NO
2 and, depending on the definition used, one of the 40 to 80 essential human nutrients.
Not enough Niacin in the diet can cause nausea, skin and mouth lesions, anemia, headaches, and tiredness. Chronic Niacin deficiency leads to a disease called Pellagra. The lack of niacin may also be observed in pandemic deficiency disease which is caused by a lack of five crucial vitamins: niacin, vitamin C, thiamin, vitamin D and vitamin A, and is usually found in areas of widespread poverty and malnutrition.
Niacin has been used for over 50 years to increase levels of HDL in the blood and has been found to decrease the risk of cardiovascular events modestly in a number of controlled human trials.[3]
This colorless, water-soluble solid is a derivative of pyridine, with a carboxyl group (COOH) at the 3-position. Other forms of vitamin B3 include the corresponding amide, nicotinamide ("niacinamide"), where the carboxyl group has been replaced by a carboxamide group (CONH
2), as well as more complex amides and a variety of esters. Nicotinic acid and niacinamide are convertible to each other with steady world demand rising from 8,500 tonnes per year in 1980s to 40,000 in recent years.[4]
Niacin cannot be directly converted to nicotinamide, but both compounds could be converted to and are precursors of NAD and NADP in vivo.[5] Nicotinic acid, nicotinamide, and tryptophan (via quinoline acid) are co-factors for nicotinamide adenine dinucleotide (NAD) and nicotinamide adenine dinucleotide phosphate (NADP). NAD converts to NADP by phosphorylation in the presence of the enzyme NAD+ kinase. NADP and NAD are coenzyme for many dehydrogenases, participating in many hydrogen transfer processes.[6] NAD is important in catabolism of fat, carbohydrate, protein, and alcohol, as well as cell signaling and DNA repair, and NADP mostly in anabolism reactions such as fatty acid and cholesterol synthesis.[6] High energy requirements (brain) or high turnover rate (gut, skin) organs are usually the most susceptible to their deficiency.[7]
Although the two are identical in their vitamin activity, nicotinamide does not have the same pharmacological effects (lipid modifying effects) as niacin. Nicotinamide does not reduce cholesterol or cause flushing.[8] Nicotinamide may be toxic to the liver at doses exceeding 3 g/day for adults.[9] Niacin is involved in both DNA repair, and the production of steroid hormones in the adrenal gland.
Dietary needs
One recommended daily allowance of niacin is 2–12 mg/day for children, 14 mg/day for women, 16 mg/day for men, and 18 mg/day for pregnant or breast-feeding women.[10] Tolerable upper intake levels (UL) for adult men and women is considered to be 35 mg/day by the Dietary Reference Intake system to avoid flushing. In general, niacin status is tested through urinary biomarkers,[11] which are believed to be more reliable than plasma levels.[12]
Deficiency

At present, niacin deficiency is sometimes seen in developed countries, and it is usually apparent in conditions of poverty, malnutrition, and chronic alcoholism.[13] It also tends to occur in areas where people eat maize (corn, the only grain low in digestible niacin) as a staple food. A special cooking technique called nixtamalization is needed to increase the bioavailability of niacin during maize meal/flour production.
Mild niacin deficiency has been shown to slow metabolism, causing decreased tolerance to cold.
Severe deficiency of niacin in the diet causes the disease pellagra, which is characterized by diarrhea, dermatitis, and dementia, as well as “Casal's necklace” lesions on the lower neck, hyperpigmentation, thickening of the skin, inflammation of the mouth and tongue, digestive disturbances, amnesia, delirium, and eventually death, if left untreated.[14] Common psychiatric symptoms of niacin deficiency include irritability, poor concentration, anxiety, fatigue, restlessness, apathy, and depression.[14] Studies have indicated that, in patients with alcoholic pellagra, niacin deficiency may be an important factor influencing both the onset and severity of this condition. Patients with alcoholism typically experience increased intestinal permeability, leading to negative health outcomes.
Hartnup’s disease is a hereditary nutritional disorder resulting in niacin deficiency.[14] This condition was first identified in the 1950s by the Hartnup family in London. It is due to a deficit in the intestines and kidneys, making it difficult for the body to break down and absorb dietary tryptophan. The resulting condition is similar to pellagra, including symptoms of red, scaly rash, and sensitivity to sunlight. Oral niacin is given as a treatment for this condition in doses ranging from 40–200 mg, with a good prognosis if identified and treated early.[14] Niacin synthesis is also deficient in carcinoid syndrome, because of metabolic diversion of its precursor tryptophan to form serotonin.
Therapeutic effects
In 1955, Altschul et al. (1955)[15] described niacin as lipid lowering property for the first time that followed by subsequent studies. Niacin is the oldest lipid lowering drug with unique anti atherosclerotic property. It reduces traditional parameters such as low density lipoprotein cholesterol (LDL), very low-density lipoprotein cholesterol (VLDL-C), and triglycerides (TG), but effectively increases high density lipoprotein cholesterol (HDL).[16] Despite the importance of other cardiovascular risk factors, high HDL correlated to lower cardiovascular event independent of LDL reduction.[17][18] Other effects include anti-thrombotic and vascular inflammation, improving endothelial function, and plaque stability.[19] Niacin alone[20] or in combination with other lipid lowering agents such as statin[21] or ezetimibe[22] significantly reduces risk of cardiovascular disease and arthrosclerosis progression.[23]
Niacin therapeutic effect is mostly through its specific G protein coupled receptor (GPR109A and GPR109B) recently named as hydroxyl carboxylic acid (HCA) receptor 2[23] that highly expressed in adipose tissue, spleen, immune cells and keratinocytes but not in other expected organs such as liver, kidney, heart or intestine.[24][25] GPR109A inhibits cyclic adenosine monophosphate production and thus lipolysis and free fatty acids available for liver to produce TG and VLDL and consequently LDL.[26][27] Decrease in free fatty acids also suppress hepatic expression of apolipoprotein C3 (APOC3) and PPARg coactivator-1b (PGC-1b) thus increase VLDL turn over and reduce its production.[28] It also inhibits diacylglycerol acyltransferase-2 (important hepatic TG synthesis).
The mechanism behind increasing HDL is not totally understood but it seems to be done in various ways. Niacin increase apolipoprotein A1 levels due to anti catabolic effects resulting in higher reverse cholesterol transport. It also inhibits HDL hepatic uptake, down regulating production of cholesterol ester transfer protein (CETP) gene.[16] Finally, it stimulates ABCA1 transporter in monocytes and macrophages and up regulates peroxisome proliferator-activated receptor γ results in reverse cholesterol transport.[29]
Improving vascular endothelial function has been reported in few experiments using niacin. In an experiment on type 2 diabetes, nicotinic acid improved endothelial function comparing with control. Daily dose of 1 g niacin shows significant lipid modifying properties and reach the plateau using 2 grams. GPR109A in immune cells such as monocytes, macrophages, and dendritic cells is responsible for atherosclerosis effects of niacin by reducing the immune cells’ infiltration of vessel wall[30][31] It also down regulates endothelial adhesion molecules such as vascular cell adhesion molecule 1 (VCAM-1) or of chemokines such as monocyte chemotactic protein 1 (MCP-1) and inflammatory proteins which results in atherosclerotic stabilization and antithrombotic effects.[19] The changes in adhesion molecules and chemokines might be through activation of receptor GPR109A on immune cells.[30]
Adipokines are the adipocytes’ produced mediators. Some adipokines such as tumor necrosis factor (TNF)-a, interleukins and chemokines, have pro-inflammatory effect and some others such as adiponectin have anti-inflammatory effect that regulates inflammatory process, decrease vascular progression and atherosclerosis.[32][33] Nicotinic acid increase adiponectin plasma levels in humans and mice[34][35] but inhibits pro-inflammatory chemokines such as MCP-1 and fractalkin.[36] Other recently explored therapeutic effect of nicotinic acid are neuroprotective and anti-inflammatory effects, beneficial in animal models of arthritis, chronic renal failure, or sepsis; however, more work is needed in this area.
Following Coronary Drug Project (CDP), one of the first experiments done to study long term clinical lipid-lowering effect of niacin in the 1960s to early 1970’s,[37] many other experiments have been done. Their results, summarized in two meta-analyses, concluded that therapeutic doses of niacin alone or in combination with other lipid-modifying agents such as statin reduce cardiovascular events and atherosclerosis progression significantly.[20][38] This agrees with the current National Cholesterol Education Program (NCEP) on high cholesterol treatment. NCEP recommends niacin alone for cardiovascular and atherogenic dyslipidemia in mild or normal LDL levels or in combination for higher LDL levels (NCEP, 2002).[39] 1500 mg Immediate release niacin daily results in 13% LDL, 20% LP, 10% TG reduction and 19% HDL increase comparing to placebo.[40] Extended release niacin alone or with anti-flushing agent (laropiprant) shows similar effects.[41][42]
Niacin binds to and stimulates a G-protein-coupled receptor, GPR109A, which causes the inhibition of fat breakdown in adipose tissue.[43] Nicotinamide does not bind this receptor which explains why it does not affect blood lipid levels. Lipids that are liberated from adipose tissue are normally used to build very-low-density lipoproteins (VLDL) in the liver, which are precursors of low-density lipoprotein (LDL) or "bad" cholesterol. Because niacin blocks the breakdown of fats, it causes a decrease in free fatty acids in the blood and, as a consequence, decreases the secretion of VLDL and cholesterol by the liver.[44]
By lowering VLDL levels, niacin also increases the level of high-density lipoprotein (HDL) or "good" cholesterol in blood, and therefore it is sometimes prescribed for people with low HDL, who are also at high risk of a heart attack.[45][46]
The ARBITER 6-HALTS study, reported at the 2009 annual meeting of the American Heart Association and in the New England Journal of Medicine[47] concluded that, when added to statins, 2000 mg/day of extended-release niacin was more effective than ezetimibe (Zetia) in reducing carotid intima-media thickness, a marker of atherosclerosis.[48] Additionally, a recent meta-analysis covering 11 randomized controlled clinical trials found positive effects of niacin alone or in combination on all cardiovascular events and on atherosclerosis evolution.[20]
However, a 2011 study (AIM-HIGH) was halted early because patients showed no decrease in cardiovascular events, but did experience an increase in the risk of stroke. These patients already had LDL levels well controlled by a statin drug, and the aim of the study was to evaluate extended-release niacin (2000 mg per day) to see if raising HDL levels had an additional positive effect on risk. In this study, it did not have such an effect, and appeared to increase stroke risk.[49] The role of niacin in patients whose LDL is not well-controlled (as in the majority of previous studies with niacin) is still under study and debate. However, it does not seem to offer benefits via raising HDL, in patients already lowering LDL by taking a statin.
Niacin prescriptions
Many preparations of niacin are available over-the-counter as dietary supplements. Immediate release niacin is effective at lowering cholesterol levels, and has minimal hepatotoxic side effects due to its rapid elimination from the body. However, it has the main drawback of causing strong vasodilation side effects with sensations of flushing and skin tingling that can be unpleasant to many patients. Non-prescription extended release niacin, such as Endur-acin, which uses a wax matrix to delay release are available as well.[50][51] A prescription extended release niacin, Niaspan, has a film coating that delays release of the niacin, resulting in an absorption over a period of 8–12 hours. The extended release formulations generally reduce vasodilation and flushing side effects, but increase the risk of hepatotoxicity compared to the immediate release forms.[52][53][54]
A formulation of Laropiprant (Merck & Co., Inc.) and niacin had previously been approved for use in Europe and marketed as Tredaptive. Laropiprant is a prostaglandin D2 binding drug shown to reduce vasodilatation and flushing up to 73%[16][55][56] The HPS2-THRIVE study,[57] a study sponsored by Merck, showed no additional efficacy of Tredaptive in lowering cholesterol when used together with other statin drugs, but did show an increase in other side effects. The study resulted in the complete withdrawal of Tredaptive from the international market.[58][59]
Over-the counter niacin dietary supplements generally lack the safety and efficacy data required for FDA regulatory approval. Some “no flush” types, such as inositol hexanicotinate contain convertible niacin compounds, but have with little clinical efficacy in reducing cholesterol levels[60][61] or “slow release” has higher hepatotoxic activity hence non-prescription niacin is not recommended due to potential harm.[16]
Toxicity
Pharmacological doses of niacin (1.5 - 6 g per day) lead to side effects that can include dermatological conditions such as skin flushing and itching, dry skin, and skin rashes including eczema exacerbation and acanthosis nigricans. Some of these symptoms are generally related to niacin's role as the rate limiting cofactor in the histidine decarboxylase enzyme which converts l-histidine into histamine.[citation needed] H1 and H2 receptor mediated histamine is metabolized via a sequence of mono (or di-) amine oxidase and COMT into methylhistamine which is then conjugated through the liver's CYP450 pathways. Persistent flushing and other symptoms may indicate deficiencies in one or more of the cofactors responsible for this enzymatic cascade. Gastrointestinal complaints, such as dyspepsia (indigestion), nausea and liver toxicity fulminant hepatic failure, have also been reported. Side effects of hyperglycemia, cardiac arrhythmias and "birth defects in experimental animals" have also been reported.[62]
Flushing usually lasts for about 15 to 30 minutes, though it can sometimes last up to two hours. It is sometimes accompanied by a prickly or itching sensation, in particular, in areas covered by clothing. Flushing is mediated by prostaglandin E2 and D2 due to GPR109A activation of epidermal langerhans’ cells and keratinocytes.[63][64] Langerhans use cyclooxygenase type 1 (COX-1) for PGE2 production and are more responsible for acute flushing while keratinocutes are COX-2 dependent and are in active continued vaso-dilation.[65][66] To reduce flushing many studies focused on altering or blocking the prostaglandin mediated pathway.[67] This effect is mediated by GPR109A-mediated prostaglandin release from the Langerhans cells of the skin and can be blocked by taking 300 mg of aspirin half an hour before taking niacin, by taking one tablet of ibuprofen per day or by co-administering the prostaglandin receptor antagonist laropiprant. Taking the niacin with meals also helps reduce this side effect. After several weeks of a consistent dose, most patients no longer flush.[68] Slow- or "sustained"-release forms of niacin have been developed to lessen these side effects.[69][70] One study showed the incidence of flushing was significantly lower with a sustained release formulation[71] though doses above 2 g per day have been associated with liver damage, in particular, with slow-release formulations.[62] Flushing is often thought to involve histamine, but histamine has been shown not to be involved in the reaction.[72] Prostaglandin (PGD2) is the primary cause of the flushing reaction, with serotonin appearing to have a secondary role in this reaction.[72]
Hepatotoxicity is another side effect of niacin. Metabolizing niacin occurs in liver in two ways: one through conjugation pathway producing nicotinuric acid metabolite related to flushing and the other through amidation resulting in NAD production related to hepatotoxicity.[26]
Although high doses of niacin may elevate blood sugar, thereby worsening diabetes mellitus,[62] recent studies show the actual effect on blood sugar to be only 5–10%. Patients with diabetes who continued to take anti-diabetes drugs containing niacin did not experience major blood glucose changes. Thus overall, niacin continues to be recommended as a drug for preventing cardiovascular disease in patients with diabetes.
Hyperuricemia is another side effect of taking high-dose niacin, and may exacerbate gout.[73]
Niacin in doses used to lower cholesterol levels has been associated with birth defects in laboratory animals, with possible consequences for infant development in pregnant women.[62]
Niacin, particularly the time-release variety, at extremely high doses can cause acute toxic reactions.[74] Extremely high doses of niacin can also cause niacin maculopathy, a thickening of the macula and retina, which leads to blurred vision and blindness. This maculopathy is reversible after niacin intake ceases.[75]
Nicotinamide
Nicotinamide may be obtained from the diet where it is present primarily as NAD+ and NADP+. These are hydrolysed in the intestine and the resulting nicotinamide is absorbed either as such, or following its hydrolysis to nicotinic acid. Nicotinamide is present in nature in only small amounts. In unprepared foods, niacin is present mainly in the form of the cellular pyridine nucleotides NAD and NADP. Enzymatic hydrolysis of the co-enzymes can occur during the course of food preparation. Boiling releases most of the total niacin present in sweet corn as nicotinamide (up to 55 mg/kg).[76]
Inositol hexanicotinate
One form of dietary supplement is inositol hexanicotinate (IHN), which is inositol that has been esterified with niacin on all six of inositol's alcohol groups. IHN is usually sold as "flush-free" or "no-flush" niacin in units of 250, 500, or 1000 mg/tablets or capsules. It is sold as an over-the-counter formulation, and often is marketed and labeled as niacin, thus misleading consumers into thinking they are getting the active form of the medication. While this form of niacin does not cause the flushing associated with the immediate-release products, the evidence that it has lipid-modifying functions is contradictory, at best. As the clinical trials date from the early 1960s (Dorner, Welsh) or the late 1970s (Ziliotto, Kruse, Agusti), it is difficult to assess them by today's standards.[77] One of the last of those studies affirmed the superiority of inositol and xantinol esters of nicotinic acid for reducing serum free fatty acid,[78] but other studies conducted during the same period found no benefit.[79] Studies explain that this is primarily because "flush-free" preparations do not contain any free nicotinic acid. A more recent placebo-controlled trial was small (n=11/group), but results after three months at 1500 mg/day showed no trend for improvements in total cholesterol, LDL-C, HDL-C or triglycerides.[80] Thus, so far there is not enough evidence to recommend IHN to treat dyslipidemia. Furthermore, the American Heart Association and the National Cholesterol Education Program both take the position that only prescription niacin should be used to treat dyslipidemias, and only under the management of a physician. The reason given is that niacin at effective intakes of 1500–3000 mg/day can also potentially have severe adverse effects. Thus liver function tests to monitor liver enzymes are necessary when taking therapeutic doses of niacin, including alkaline phosphatase (ALP), aspartate transaminase (AST), and alanine transaminase (ALT).
Biosynthesis and chemical synthesis

The liver can synthesize niacin from the essential amino acid tryptophan, requiring 60 mg of tryptophan to make one mg of niacin.[81] The 5-membered aromatic heterocycle of tryptophan is cleaved and rearranged with the alpha amino group of tryptophan into the 6-membered aromatic heterocycle of niacin. Riboflavin, vitamin B6 and iron are required in some of the reactions involved in the conversion of tryptophan to NAD.
Several thousand tons of niacin are manufactured each year, starting from 3-methylpyridine.
Receptor
In addition to its effects as NAD and NADP, niacin may have additional effects by receptor activation. The receptor for niacin is a G protein-coupled receptor called HM74A.[82] It couples to the Gi alpha subunit.[83]
Food sources
Niacin is found in variety of foods, including liver, chicken, beef, fish, cereal, peanuts and legumes, and is also synthesized from tryptophan, an essential amino acid found in most forms of protein.
Animal products:
- liver, heart and kidney (9 – 15 mg niacin per 100 grams)
- chicken, chicken breast (6.5 mg)
- beef (5 – 6 mg)
- fish: tuna, salmon, halibut (2.5 – 13 mg)
- eggs (0.1 mg)
- venison (8.43 mg)
Fruits and vegetables:
- avocados (1 mg niacin per 100 grams)
- dates (2 mg)
- tomatoes (0.7 mg)
- leaf vegetables (0.3 - 0.4 mg)
- broccoli (0.6 mg)
- carrots (0.3 - 0.6 mg)
- sweet potatoes (0.5 - 0.6 mg)
- asparagus (0.4 mg)
Seeds:
- nuts (2 mg niacin per 100 grams)
- whole grain products (4 - 29.5 mg)
- legumes (0.4 – 16 mg)
- saltbush seeds
Fungi:
- mushrooms, shiitake mushrooms (3.5 – 4 mg niacin per 100 grams)
- brewer's yeast (36 mg)
Other:
- Monster Energy drink (40 mg per 16 ounces)
- Rockstar Energy (100% in the Super Sours flavors)
- Red Bull Energy Drink (28 mg per 12 ounces)
- Five Hour Energy drink (30 mg per 1.93 ounces)
- Ovaltine (18 mg)
- Peanut butter (15 mg)
- Tofu
- Soy sauce (0.4 mg)
- Vegemite (from spent brewer's yeast) (110 mg niacin per 100 grams)
- Marmite (from spent brewer's yeast) (110 mg niacin per 100 grams)
History
Niacin was first described by chemist Hugo Weidel in 1873 in his studies of nicotine.[85] The original preparation remains useful: The oxidation of nicotine using nitric acid.[86] For the first time, niacin was extracted by Casimir Funk, but he thought that it was thiamine and due to the discovered amine group he coined the term "vitamine". Niacin was extracted from livers by biochemist Conrad Elvehjem in 1937, who later identified the active ingredient, then referred to as the "pellagra-preventing factor" and the "anti-blacktongue factor."[87] Soon after, in studies conducted in Alabama and Cincinnati, Dr. Tom Spies found that nicotinic acid cured the sufferers of pellagra.[88]
When the biological significance of nicotinic acid was realized, it was thought appropriate to choose a name to dissociate it from nicotine, to avoid the perception that vitamins or niacin-rich food contains nicotine, or that cigarettes contain vitamins. The resulting name 'niacin' was derived from nicotinic acid + vitamin.[citation needed]
Carpenter found in 1951 that niacin in corn is biologically unavailable, and can be released only in very alkaline lime water of pH 11.[89] This process, known as nixtamalization, was discovered by the prehistoric civilizations of Mesoamerica.[90]
Niacin is referred to as vitamin B3 because it was the third of the B vitamins to be discovered. It has historically been referred to as "vitamin PP" or "vitamin P-P," both of which are derived from the term "pellagra-preventive factor."
Research
As of August 2008[update], a combination of niacin with laropiprant is being tested in a clinical trial. Laropiprant reduces facial flushes induced by niacin.[91]
References
- ^ "Niacin". DrugBank: a knowledgebase for drugs, drug actions and drug targets. Retrieved 14-January-2012.
{{cite web}}: Check date values in:|accessdate=(help) - ^ CID 938 from PubChem
- ^ Bruckert, E (2010 Jun). "Meta-analysis of the effect of nicotinic acid alone or in combination on cardiovascular events and atherosclerosis". Atherosclerosis. 210 (2): 353–61. doi:10.1016/j.atherosclerosis.2009.12.023. PMID 20079494.
{{cite journal}}: Check date values in:|date=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Cantarella, L; Gallifuoco, A; Malandra, A; Martínková, L; Spera, A; Cantarella, M (2011). "High-yield continuous production of nicotinic acid via nitrile hydratase-amidase cascade reactions using cascade CSMRs". Enzyme and Microbial Technology. 48 (4–5): 345–50. doi:10.1016/j.enzmictec.2010.12.010. PMID 22112948.
- ^ Cox, Michael; Lehninger, Albert L; Nelson, David R. (2000). Lehninger principles of biochemistry. New York: Worth Publishers. ISBN 1-57259-153-6.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ^ a b Wan, P; Moat, S; Anstey, A (2011). "Pellagra: A review with emphasis on photosensitivity". The British journal of dermatology. 164 (6): 1188–200. doi:10.1111/j.1365-2133.2010.10163.x. PMID 21128910.
- ^ Ishii, N; Nishihara, Y (1981). "Pellagra among chronic alcoholics: Clinical and pathological study of 20 necropsy cases". Journal of neurology, neurosurgery, and psychiatry. 44 (3): 209–15. doi:10.1136/jnnp.44.3.209. PMC 490893. PMID 7229643.
- ^ Jaconello P (1992). "Niacin versus niacinamide". CMAJ. 147 (7): 990. PMC 1336277. PMID 1393911.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Knip M, Douek IF, Moore WP; et al. (2000). "Safety of high-dose nicotinamide: a review". Diabetologia. 43 (11): 1337–45. doi:10.1007/s001250051536. PMID 11126400.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Jacobson, EL (2007). "Niacin". Linus Pauling Institute. Retrieved 2011-08-08.
- ^ Institute of Medicine (2006). Dietary Reference Intakes Research Synthesis: Workshop Summary. National Academies Press. p. 37.
- ^ Jacob RA, Swendseid ME, McKee RW, Fu CS, Clemens RA (1989). "Biochemical markers for assessment of niacin status in young men: urinary and blood levels of niacin metabolites". J. Nutr. 119 (4): 591–8. PMID 2522982.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Pitsavas S, Andreou C, Bascialla F, Bozikas VP, Karavatos A (2004). "Pellagra encephalopathy following B-complex vitamin treatment without niacin". Int J Psychiatry Med. 34 (1): 91–5. doi:10.2190/29XV-1GG1-U17K-RGJH. PMID 15242145.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b c d Prakash, Ravi (2008). "Rapid resolution of delusional parasitosis in pellagra with niacin augmentation therapy". General Hospital Psychiatry. 30 (6): 581–4. doi:10.1016/j.genhosppsych.2008.04.011. PMID 19061687.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Altschul, R; Hoffer, A; Stephen, JD (1955). "Influence of nicotinic acid on serum cholesterol in man". Archives of biochemistry and biophysics. 54 (2): 558–9. doi:10.1016/0003-9861(55)90070-9. PMID 14350806.
- ^ a b c d Villines, TC; Kim, AS; Gore, RS; Taylor, AJ (2012). "Niacin: The evidence, clinical use, and future directions". Current atherosclerosis reports. 14 (1): 49–59. doi:10.1007/s11883-011-0212-1. PMID 22037771.
- ^ Barter, P; Gotto, AM; Larosa, JC; Maroni, J; Szarek, M; Grundy, SM; Kastelein, JJ; Bittner, V; Fruchart, JC (2007). "HDL cholesterol, very low levels of LDL cholesterol, and cardiovascular events". The New England Journal of Medicine. 357 (13): 1301–10. doi:10.1056/NEJMoa064278. PMID 17898099.
- ^ Jafri, H; Alsheikh-Ali, AA; Karas, RH (2010). "Meta-analysis: Statin therapy does not alter the association between low levels of high-density lipoprotein cholesterol and increased cardiovascular risk". Annals of internal medicine. 153 (12): 800–8. doi:10.1059/0003-4819-153-12-201012210-00006. PMID 21173414.
- ^ a b Wu, BJ; Yan, L; Charlton, F; Witting, P; Barter, PJ; Rye, KA (2010). "Evidence that niacin inhibits acute vascular inflammation and improves endothelial dysfunction independent of changes in plasma lipids". Arteriosclerosis, thrombosis, and vascular biology. 30 (5): 968–75. doi:10.1161/ATVBAHA.109.201129. PMID 20167660.
- ^ a b c Bruckert, E; Labreuche, J; Amarenco, P (2010). "Meta-analysis of the effect of nicotinic acid alone or in combination on cardiovascular events and atherosclerosis". Atherosclerosis. 210 (2): 353–61. doi:10.1016/j.atherosclerosis.2009.12.023. PMID 20079494.
- ^ Taylor, AJ; Lee, HJ; Sullenberger, LE (2006). "The effect of 24 months of combination statin and extended-release niacin on carotid intima-media thickness: ARBITER 3". Current medical research and opinion. 22 (11): 2243–50. doi:10.1185/030079906X148508. PMID 17076985.
- ^ Taylor, AJ; Villines, TC; Stanek, EJ; Devine, PJ; Griffen, L; Miller, M; Weissman, NJ; Turco, M (2009). "Extended-release niacin or ezetimibe and carotid intima-media thickness". The New England Journal of Medicine. 361 (22): 2113–22. doi:10.1056/NEJMoa0907569. PMID 19915217.
- ^ a b Lukasova, M; Hanson, J; Tunaru, S; Offermanns, S (2011). "Nicotinic acid (niacin): New lipid-independent mechanisms of action and therapeutic potentials". Trends in pharmacological sciences. 32 (12): 700–7. doi:10.1016/j.tips.2011.08.002. PMID 21944259.
- ^ Soga, T; Kamohara, M; Takasaki, J; Matsumoto, S; Saito, T; Ohishi, T; Hiyama, H; Matsuo, A; Matsushime, H (2003). "Molecular identification of nicotinic acid receptor". Biochemical and Biophysical Research Communications. 303 (1): 364–9. doi:10.1016/S0006-291X(03)00342-5. PMID 12646212.
- ^ Wise, A; Foord, SM; Fraser, NJ; Barnes, AA; Elshourbagy, N; Eilert, M; Ignar, DM; Murdock, PR; Steplewski, K (2003). "Molecular identification of high and low affinity receptors for nicotinic acid". The Journal of Biological Chemistry. 278 (11): 9869–74. doi:10.1074/jbc.M210695200. PMID 12522134.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ a b Gille, A; Bodor, ET; Ahmed, K; Offermanns, S (2008). "Nicotinic acid: Pharmacological effects and mechanisms of action". Annual review of pharmacology and toxicology. 48: 79–106. doi:10.1146/annurev.pharmtox.48.113006.094746. PMID 17705685.
- ^ Wanders, D; Judd, RL (2011). "Future of GPR109A agonists in the treatment of dyslipidaemia". Diabetes, obesity & metabolism. 13 (8): 685–91. doi:10.1111/j.1463-1326.2011.01400.x. PMID 21418500.
- ^ Hernandez, C; Molusky, M; Li, Y; Li, S; Lin, JD (2010). "Regulation of hepatic ApoC3 expression by PGC-1β mediates hypolipidemic effect of nicotinic acid". Cell metabolism. 12 (4): 411–9. doi:10.1016/j.cmet.2010.09.001. PMC 2950832. PMID 20889132.
- ^ Rubic, T; Trottmann, M; Lorenz, RL (2004). "Stimulation of CD36 and the key effector of reverse cholesterol transport ATP-binding cassette A1 in monocytoid cells by niacin". Biochemical pharmacology. 67 (3): 411–9. doi:10.1016/j.bcp.2003.09.014. PMID 15037193.
- ^ a b Lukasova, M; Malaval, C; Gille, A; Kero, J; Offermanns, S (2011). "Nicotinic acid inhibits progression of atherosclerosis in mice through its receptor GPR109A expressed by immune cells". The Journal of Clinical Investigation. 121 (3): 1163–73. doi:10.1172/JCI41651. PMC 3048854. PMID 21317532.
- ^ Holzhäuser, E; Albrecht, C; Zhou, Q; Buttler, A; Preusch, MR; Blessing, E; Katus, HA; Bea, F (2011). "Nicotinic acid has anti-atherogenic and anti-inflammatory properties on advanced atherosclerotic lesions independent of its lipid-modifying capabilities". Journal of cardiovascular pharmacology. 57 (4): 447–54. doi:10.1097/FJC.0b013e31820dc1db. PMID 21242806.
- ^ Benjó, AM; Maranhão, RC; Coimbra, SR; Andrade, AC; Favarato, D; Molina, MS; Brandizzi, LI; Da Luz, PL (2006). "Accumulation of chylomicron remnants and impaired vascular reactivity occur in subjects with isolated low HDL cholesterol: Effects of niacin treatment". Atherosclerosis. 187 (1): 116–22. doi:10.1016/j.atherosclerosis.2005.08.025. PMID 16458316.
- ^ Gustafson, B (2010). "Adipose tissue, inflammation and atherosclerosis". Journal of atherosclerosis and thrombosis. 17 (4): 332–41. doi:10.5551/jat.3939. PMID 20124732.
- ^ Plaisance, EP; Lukasova, M; Offermanns, S; Zhang, Y; Cao, G; Judd, RL (2009). "Niacin stimulates adiponectin secretion through the GPR109A receptor". American journal of physiology. Endocrinology and metabolism. 296 (3): E549–58. doi:10.1152/ajpendo.91004.2008. PMID 19141678.
- ^ Westphal, S; Luley, C (2008). "Preferential increase in high-molecular weight adiponectin after niacin". Atherosclerosis. 198 (1): 179–83. doi:10.1016/j.atherosclerosis.2007.09.036. PMID 17996241.
- ^ Digby, JE; McNeill, E; Dyar, OJ; Lam, V; Greaves, DR; Choudhury, RP (2010). "Anti-inflammatory effects of nicotinic acid in adipocytes demonstrated by suppression of fractalkine, RANTES, and MCP-1 and upregulation of adiponectin". Atherosclerosis. 209 (1): 89–95. doi:10.1016/j.atherosclerosis.2009.08.045. PMC 2839075. PMID 19781706.
- ^ JAMA. (1975). "Clofibrate and niacin in coronary heart disease." JAMA 231(4) 360-381.
- ^ Duggal, JK; Singh, M; Attri, N; Singh, PP; Ahmed, N; Pahwa, S; Molnar, J; Singh, S; Khosla, S (2010). "Effect of niacin therapy on cardiovascular outcomes in patients with coronary artery disease". Journal of cardiovascular pharmacology and therapeutics. 15 (2): 158–66. doi:10.1177/1074248410361337. PMID 20208032.
- ^ NCEP. (2002). "Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report." Circulation 106(25) 3143-3421.
- ^ Knopp, RH; Alagona, P; Davidson, M; Goldberg, AC; Kafonek, SD; Kashyap, M; Sprecher, D; Superko, HR; Jenkins, S (1998). "Equivalent efficacy of a time-release form of niacin (Niaspan) given once-a-night versus plain niacin in the management of hyperlipidemia". Metabolism: clinical and experimental. 47 (9): 1097–104. doi:10.1016/S0026-0495(98)90284-0. PMID 9751239.
- ^ Bays, H; Shah, A; Dong, Q; McCrary Sisk, C; MacCubbin, D (2011). "Extended-release niacin/laropiprant lipid-altering consistency across patient subgroups". International journal of clinical practice. 65 (4): 436–45. doi:10.1111/j.1742-1241.2010.02620.x. PMID 21401833.
- ^ McKenney, J; Bays, H; Koren, M; Ballantyne, CM; Paolini, JF; Mitchel, Y; Betteridge, A; Kuznetsova, O; Sapre, A (2010). "Safety of extended-release niacin/laropiprant in patients with dyslipidemia". Journal of clinical lipidology. 4 (2): 105–112.e1. doi:10.1016/j.jacl.2010.02.002. PMID 21122637.
- ^ Gille A, Bodor ET, Ahmed K, Offermanns S (2008). "Nicotinic acid: pharmacological effects and mechanism of action". Annu Rev Pharmacol Toxicol. 48: 79–106. doi:10.1146/annurev.pharmtox.48.113006.094746. PMID 17705685.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Katzung, Bertram G. (2006). Basic and clinical pharmacology. New York: McGraw-Hill Medical Publishing Division. ISBN 0-07-145153-6.
- ^ McGovern ME (2005). "Taking aim at HDL-C. Raising levels to reduce cardiovascular risk". Postgrad Med. 117 (4): 29–30, 33–5, 39 passim. doi:10.3810/pgm.2005.04.1610. PMID 15842130.
- ^ Canner PL, Berge KG, Wenger NK; et al. (1986). "Fifteen year mortality in Coronary Drug Project patients: long-term benefit with niacin". J. Am. Coll. Cardiol. 8 (6): 1245–55. doi:10.1016/S0735-1097(86)80293-5. PMID 3782631.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Taylor AJ, Villines TC, Stanek EJ; et al. (2009). "Extended-release niacin or ezetimibe and carotid intima-media thickness". N. Engl. J. Med. 361 (22): 2113–22. doi:10.1056/NEJMoa0907569. PMID 19915217.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Singer, Natasha (November 15, 2009). "Study Raises Questions About Cholesterol Drug's Benefit". The New York Times. Retrieved November 16, 2009.
- ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 22085343, please use {{cite journal}} with
|pmid= 22085343instead. - ^ Endur-Acin Oral : Uses, Side Effects, Interactions, Pictures, Warnings & Dosing - WebMD
- ^ L-arginine, niacin, phytosterols, pantethine, calcium, vitamin c, b complex, cholesterol control without diet, 8 week cholesterol cure, linus pauling
- ^ Pharmacokinetics and dose recommendations of Niaspan® in chronic kidney disease and dialysis patients
- ^ Niaspan (Niacin) Drug Information: Description, User Reviews, Drug Side Effects, Interactions - Prescribing Information at RxList
- ^ About NIASPAN® (niacin extended-release)
- ^ Lai, E; De Lepeleire, I; Crumley, TM; Liu, F; Wenning, LA; Michiels, N; Vets, E; O'Neill, G; Wagner, JA (2007). "Suppression of niacin-induced vasodilation with an antagonist to prostaglandin D2 receptor subtype 1". Clinical pharmacology and therapeutics. 81 (6): 849–57. doi:10.1038/sj.clpt.6100180. PMID 17392721.
- ^ Kamanna, VS; Vo, A; Kashyap, ML (2008). "Nicotinic acid: Recent developments". Current Opinion in Cardiology. 23 (4): 393–8. doi:10.1097/HCO.0b013e3283021c82. PMID 18520725..
- ^ Treatment of HDL to Reduce the Incidence of Vascular Events HPS2-THRIVE - Full Text View - ClinicalTrials.gov
- ^ Medscape: Medscape Access
- ^ Merck begins overseas recall of HDL cholesterol drug | Reuters
- ^ Study Finds Extended Release Niacin, but not IHN, Effective in Lowering Cholesterol Levels
- ^ Norris, RB (2006). ""Flush-free niacin": Dietary supplement may be "benefit-free"". Preventive cardiology. 9 (1): 64–5. doi:10.1111/j.1520-037X.2006.04736.x. PMID 16407706.
- ^ a b c d Keith Parker; Laurence Brunton; Goodman, Louis Sanford; Lazo, John S.; Gilman, Alfred (2006). Goodman & Gilman's the pharmacological basis of therapeutics. New York: McGraw-Hill. ISBN 0-07-142280-3.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ^ Benyó, Z; Gille, A; Kero, J; Csiky, M; Suchánková, MC; Nüsing, RM; Moers, A; Pfeffer, K; Offermanns, S (2005). "GPR109A (PUMA-G/HM74A) mediates nicotinic acid-induced flushing". The Journal of Clinical Investigation. 115 (12): 3634–40. doi:10.1172/JCI23626. PMC 1297235. PMID 16322797.
- ^ Benyó, Z; Gille, A; Bennett, CL; Clausen, BE; Offermanns, S (2006). "Nicotinic acid-induced flushing is mediated by activation of epidermal langerhans cells". Molecular Pharmacology. 70 (6): 1844–9. doi:10.1124/mol.106.030833. PMID 17008386.
- ^ Hanson, J; Gille, A; Zwykiel, S; Lukasova, M; Clausen, BE; Ahmed, K; Tunaru, S; Wirth, A; Offermanns, S (2010). "Nicotinic acid- and monomethyl fumarate-induced flushing involves GPR109A expressed by keratinocytes and COX-2-dependent prostanoid formation in mice". The Journal of Clinical Investigation. 120 (8): 2910–9. doi:10.1172/JCI42273. PMC 2912194. PMID 20664170.
- ^ Maciejewski-Lenoir, D; Richman, JG; Hakak, Y; Gaidarov, I; Behan, DP; Connolly, DT (2006). "Langerhans cells release prostaglandin D2 in response to nicotinic acid". The Journal of investigative dermatology. 126 (12): 2637–46. doi:10.1038/sj.jid.5700586. PMID 17008871.
- ^ Kamanna, VS; Kashyap, ML (2008). "Mechanism of action of niacin". The American journal of cardiology. 101 (8A): 20B–26B. doi:10.1016/j.amjcard.2008.02.029. PMID 18375237.
- ^ "Guidelines for Niacin Therapy For the Treatment of Elevated Lipoprotein a (Lpa)" (PDF). Rush Hemophilia & Thrombophilia Center. August 15, 2002, Revised July 27, 2005. Retrieved 20 November 2009.
facial flushing is a common side effect of niacin therapy that usually subsides after several weeks of consistent niacin use
{{cite web}}: Check date values in:|date=(help) - ^ Katzung, Bertram G. (2006). Basic and clinical pharmacology. New York: McGraw-Hill Medical Publishing Division. ISBN 0-07-145153-6.
- ^ Barter, P (2006). "Options for therapeutic intervention: How effective are the different agents?". European Heart Journal Supplements. 8 (F): F47–F53. doi:10.1093/eurheartj/sul041.
- ^ Chapman MJ, Assmann G, Fruchart JC, Shepherd J, Sirtori C (2004). "Raising high-density lipoprotein cholesterol with reduction of cardiovascular risk: the role of nicotinic acid—a position paper developed by the European Consensus Panel on HDL-C". Curr Med Res Opin. 20 (8): 1253–68. doi:10.1185/030079904125004402. PMID 15324528.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Papaliodis D, Boucher W, Kempuraj D, Michaelian M, Wolfberg A, House M, Theoharides TC (December 2008). "Niacin-induced "Flush" Involves Release of Prostaglandin D2 from Mast Cells and Serotonin from Platelets: Evidence from Human Cells in Vitro and an Animal Model". J Pharmacol Exp Ther. 327 (3): 665–72. doi:10.1124/jpet.108.141333. PMID 18784348.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Capuzzi DM, Morgan JM, Brusco OA, Intenzo CM (2000). "Niacin dosing: relationship to benefits and adverse effects". Curr Atheroscler Rep. 2 (1): 64–71. doi:10.1007/s11883-000-0096-y. PMID 11122726.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Mittal MK, Florin T, Perrone J, Delgado JH, Osterhoudt KC (2007). "Toxicity from the use of niacin to beat urine drug screening". Ann Emerg Med. 50 (5): 587–90. doi:10.1016/j.annemergmed.2007.01.014. PMID 17418450.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Gass JD (2003). "Nicotinic acid maculopathy". Retina (Philadelphia, Pa.). 23 (6 Suppl): 500–10. PMID 15035390.
- ^ F. Aguilar, U.R. Charrondiere, B. Dusemund, P. Galtier, J. Gilbert, D.M. Gott, S. Grilli, R. Guertler, G.E.N. Kass, J. Koenig, C. Lambré, J-C. Larsen, J-C. Leblanc, A. Mortensen, D. Parent-Massin, I. Pratt, I.M.C.M. Rietjens, I. Stankovic, P. Tobback, T. Verguieva, R.A. Woutersen (2009). "Inositol hexanicotinate (inositol hexaniacinate) as a source of niacin (vitamin B3) added for nutritional purposes in food supplements" (PDF). The EFSA Journal. 949: 1–20.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Taheri, R (2003-01-15). "No-Flush Niacin for the Treatment of Hyperlipidemia". Medscape. Retrieved 2008-03-31.
- ^ Kruse W, Kruse W, Raetzer H, Heuck CC, Oster P, Schellenberg B, Schlierf G (1979). "Nocturnal inhibition of lipolysis in man by nicotinic acid and derivatives". European Journal of Clinical Pharmacology. 16 (1): 11–15. doi:10.1007/BF00644960. PMID 499296.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Meyers CD, Carr MC, Park S, Brunzell JD (2003). "Varying cost and free nicotinic acid content in over-the-counter niacin preparations for dyslipidemia". Annals of Internal Medicine. 139 (12): 996–1002. doi:10.7326/0003-4819-139-12-200312160-00009. PMID 14678919.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Benjó AM, Maranhão RC, Coimbra SR, Andrade AC, Favarato D, Molina MS, Brandizzi LI, da Luz PL (2006). "Accumulation of chylomicron remnants and impaired vascular reactivity occur in subjects with isolated low HDL cholesterol: effects of niacin treatment". Atherosclerosis. 187 (1): 116–122. doi:10.1016/j.atherosclerosis.2005.08.025. PMID 16458316.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Jacobson, EL (2007). "Niacin". Linus Pauling Institute. Retrieved 2008-03-31.
- ^ Zhang Y, Schmidt RJ, Foxworthy P; et al. (2005). "Niacin mediates lipolysis in adipose tissue through its G-protein coupled receptor HM74A". Biochem. Biophys. Res. Commun. 334 (2): 729–32. doi:10.1016/j.bbrc.2005.06.141. PMID 16018973.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Zellner C, Pullinger CR, Aouizerat BE; et al. (2005). "Variations in human HM74 (GPR109B) and HM74A (GPR109A) niacin receptors". Hum. Mutat. 25 (1): 18–21. doi:10.1002/humu.20121. PMID 15580557.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ "Food Data Chart - Niacin". Retrieved 7 September 2012.
- ^ Weidel, H (1873). "Zur Kenntniss des Nicotins". Justus Liebigs Annalen der Chemie und Pharmacie. 165 (2): 330–349. doi:10.1002/jlac.18731650212.
- ^ Samuel M. McElvain (1941). "Nicotinic Acid" (PDF). Organic Syntheses; Collected Volumes, vol. 1, p. 385.
- ^ Elvehjem CA, Madden RJ, Strongandd FM, Woolley DW (1938). "The isolation and identification of the anti-blacktongue factor J" (PDF). J. Biol. Chem. 123 (1): 137–149.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Dr. Joseph Goldberger and the war on Pellagra - Office of NIH History
- ^ LAGUNA J, CARPENTER KJ (1951). "Raw versus processed corn in niacin-deficient diets". J. Nutr. 45 (1): 21–8. PMID 14880960.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ "Vitamin B3". University of Maryland Medical Center. 2002-01-04. Retrieved 2008-03-31.
- ^ Paolini JF, Bays HE, Ballantyne CM; et al. (November 2008). "Extended-release niacin/laropiprant: reducing niacin-induced flushing to better realize the benefit of niacin in improving cardiovascular risk factors". Cardiol Clin. 26 (4): 547–60. doi:10.1016/j.ccl.2008.06.007. PMID 19031552.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link)
External links
- Niacin bound to proteins in the PDB