Pandemic: Difference between revisions
Marchino61 (talk | contribs) m →Definition: transmissible is usually used in a medical context, not transmittable |
Robertpedley (talk | contribs) /* Diseases / alphabetical order |
||
| (4 intermediate revisions by the same user not shown) | |||
| Line 171: | Line 171: | ||
HIV originated in Africa, and spread to the United States via Haiti between 1966 and 1972.<ref>{{cite web |date=30 October 2007 |title=Analysis clarifies route of AIDS |url=http://articles.latimes.com/2007/oct/30/science/sci-aids30 |access-date=6 July 2014 |work=Los Angeles Times |vauthors=Chong JR}}</ref> [[AIDS]] is currently a pandemic in Africa, with infection rates as high as 25% in some regions of southern and eastern Africa. In 2006, the HIV prevalence among pregnant women in [[South Africa]] was 29%.<ref>{{cite web |date=2006 |title=The South African Department of Health Study |url=http://www.avert.org/safricastats.htm |access-date=26 August 2010 |publisher=Avert.org}}</ref> Effective education about safer sexual practices and [[bloodborne infection]] precautions training have helped to slow down infection rates in several African countries sponsoring national education programs.{{citation needed|date=March 2020}} There were an estimated 1.5 million new infections of [[HIV/AIDS]] in 2020. {{As of|2021}} there have been about a total of 40.1 million deaths related to HIV/AIDS since the epidemic started.<ref>{{cite web |title=Global HIV & AIDS statistics — 2021 fact sheet |url=https://www.unaids.org/en/resources/fact-sheet |access-date=2021-07-01 |website=www.unaids.org |publisher=UNAIDS |language=en}}</ref> |
HIV originated in Africa, and spread to the United States via Haiti between 1966 and 1972.<ref>{{cite web |date=30 October 2007 |title=Analysis clarifies route of AIDS |url=http://articles.latimes.com/2007/oct/30/science/sci-aids30 |access-date=6 July 2014 |work=Los Angeles Times |vauthors=Chong JR}}</ref> [[AIDS]] is currently a pandemic in Africa, with infection rates as high as 25% in some regions of southern and eastern Africa. In 2006, the HIV prevalence among pregnant women in [[South Africa]] was 29%.<ref>{{cite web |date=2006 |title=The South African Department of Health Study |url=http://www.avert.org/safricastats.htm |access-date=26 August 2010 |publisher=Avert.org}}</ref> Effective education about safer sexual practices and [[bloodborne infection]] precautions training have helped to slow down infection rates in several African countries sponsoring national education programs.{{citation needed|date=March 2020}} There were an estimated 1.5 million new infections of [[HIV/AIDS]] in 2020. {{As of|2021}} there have been about a total of 40.1 million deaths related to HIV/AIDS since the epidemic started.<ref>{{cite web |title=Global HIV & AIDS statistics — 2021 fact sheet |url=https://www.unaids.org/en/resources/fact-sheet |access-date=2021-07-01 |website=www.unaids.org |publisher=UNAIDS |language=en}}</ref> |
||
=== |
=== Pandemics in history === |
||
{{See also|List of epidemics and pandemics}} |
|||
{{Expand section|[[Dengue fever]] and [[Chikungunya]]|date=June 2020}} |
|||
[[File:FlorentineCodex BK12 F54 smallpox.jpg|thumb|Aztecs dying of smallpox, ''[[Florentine Codex]]'' (compiled 1540–1585)]] |
[[File:FlorentineCodex BK12 F54 smallpox.jpg|thumb|Aztecs dying of smallpox, ''[[Florentine Codex]]'' (compiled 1540–1585)]] |
||
[[File:The Triumph of Death P001393.jpg|thumb|upright=1.3|[[Pieter Brueghel the Elder|Pieter Bruegel]]'s ''[[The Triumph of Death]]'' (c. 1562) reflects the social upheaval and terror that followed the plague, which devastated medieval Europe.]] |
[[File:The Triumph of Death P001393.jpg|thumb|upright=1.3|[[Pieter Brueghel the Elder|Pieter Bruegel]]'s ''[[The Triumph of Death]]'' (c. 1562) reflects the social upheaval and terror that followed the plague, which devastated medieval Europe.]] |
||
| Line 182: | Line 182: | ||
* [[Antonine Plague]] (165 to 180 AD): Possibly measles or smallpox brought to the Italian peninsula by soldiers returning from the Near East, it killed a quarter of those infected, up to five million in total.<ref>[http://news.bbc.co.uk/2/hi/health/4381924.stm Past pandemics that ravaged Europe]. ''BBC News'', 7{{nbsp}}November. 2005</ref> |
* [[Antonine Plague]] (165 to 180 AD): Possibly measles or smallpox brought to the Italian peninsula by soldiers returning from the Near East, it killed a quarter of those infected, up to five million in total.<ref>[http://news.bbc.co.uk/2/hi/health/4381924.stm Past pandemics that ravaged Europe]. ''BBC News'', 7{{nbsp}}November. 2005</ref> |
||
* [[Plague of Cyprian]] (251–266 AD): A second outbreak of what may have been the same disease as the Antonine Plague killed (it was said) 5,000 people a day in [[Rome]].{{Citation needed|date=November 2021}} |
* [[Plague of Cyprian]] (251–266 AD): A second outbreak of what may have been the same disease as the Antonine Plague killed (it was said) 5,000 people a day in [[Rome]].{{Citation needed|date=November 2021}} |
||
* [[Plague of Justinian]] (541 to 549 AD): |
* [[Plague of Justinian]] (541 to 549 AD): Also known as the ''FIrst Plague Pandemic''. This epidemic started in [[Egypt]] and reached [[Constantinople]] the following spring, killing (according to the Byzantine chronicler [[Procopius]]) 10,000 a day at its height, and perhaps 40% of the city's inhabitants. The plague went on to eliminate a quarter to half the [[human population]] of the known world and was identified in 2013 as being caused by [[bubonic plague]].<ref>{{cite web |date=May 20, 2013 |title=Modern lab reaches across the ages to resolve plague DNA debate |url=http://phys.org/news/2013-05-modern-lab-ages-plague-dna.html |website=phys.org}}</ref><ref>{{cite web|url=http://www.cambridge.org/us/catalogue/catalogue.asp?isbn=0521846390&ss=fro |title=Cambridge Catalogue page 'Plague and the End of Antiquity' |publisher=Cambridge.org |access-date=26 August 2010}}</ref><ref>[http://www.speakeasy-forum.com/lofiversion/index.php/t18579.html Quotes from book "Plague and the End of Antiquity"] {{Webarchive|url=https://web.archive.org/web/20110716114235/http://www.speakeasy-forum.com/lofiversion/index.php/t18579.html |date=16 July 2011}} Lester K. Little, ed., ''Plague and the End of Antiquity: The Pandemic of 541–750'', Cambridge, 2006. {{ISBN|0-521-84639-0}}</ref> |
||
* [[Black Death]] (1331 to 1353): The total number of deaths worldwide is estimated at 75 to 200 million |
* [[Black Death]] (1331 to 1353): Also known as the ''Second Plague Pandemic.'' The total number of deaths worldwide is estimated at 75 to 200 million. Starting in Asia, the disease reached the Mediterranean and western Europe in 1348 (possibly from Italian merchants fleeing fighting in [[Crimea]]) and killed an estimated 20 to 30 million Europeans in six years;<ref>[http://www.medhunters.com/articles/deathOnAGrandScale.html Death on a Grand Scale]. ''MedHunters.''</ref> a third of the total population,<ref>Stéphane Barry and Norbert Gualde, in ''[[L'Histoire]]'' No. 310, June 2006, pp. 45–46, say "between one-third and two-thirds"; Robert Gottfried (1983). "Black Death" in ''[[Dictionary of the Middle Ages]]'', volume 2, pp. 257–267, says "between 25 and 45 percent".</ref> and up to a half in the worst-affected urban areas.<ref>{{cite EB1911 |wstitle=Plague |volume=21 |pages=693–705}}</ref> It was the first of a cycle of European [[Second plague pandemic|plague epidemics]] that continued until the 18th century;<ref>{{cite web |url=http://urbanrim.org.uk/plague%20list.htm |title=A List of National Epidemics of Plague in England 1348–1665 |publisher=Urbanrim.org.uk |date=4 August 2010 |access-date=26 August 2010 |archive-url=https://web.archive.org/web/20090508010316/http://urbanrim.org.uk/plague%20list.htm |archive-date=8 May 2009 |url-status=dead }}</ref> there were more than 100 plague epidemics in Europe during this period, <ref>{{cite news |url=https://www.theguardian.com/uk/2004/may/16/health.books |title=Black Death blamed on man, not rats |newspaper=The Observer | vauthors = Revill J |date= 16 May 2004|access-date=3 November 2008 | location=London}}</ref> including the [[Great Plague of London]] of 1665–66 which killed approximately 100,000 people, 20% of London's population.<ref>[http://ocp.hul.harvard.edu/contagion/plague.html The Great Plague of London, 1665]. ''The Harvard University Library, Open Collections Program: Contagion.''</ref> |
||
* [[1817–1824 cholera pandemic]]. Previously restricted to the [[Indian subcontinent]], the pandemic began in [[Bengal]], then spread across India by 1820. 10,000 British troops and thousands of Indians died during this pandemic.{{cn|date=February 2023}} It extended as far as China, [[Indonesia]] (where more than 100,000 people succumbed on the island of [[Java]] alone) and the [[Caspian Sea]] before receding. Deaths in the Indian subcontinent between 1817 and 1860 are estimated to have exceeded 15 million. Another 23 million died between 1865 and 1917. [[Russian Empire|Russian]] deaths during a similar period exceeded 2{{nbsp}}million.<ref>{{cite web |author=G. William Beardslee |title=The 1832 Cholera Epidemic in New York State |url=http://www.earlyamerica.com/review/2000_fall/1832_cholera_part1.html |access-date=26 August 2010 |publisher=Earlyamerica.com}}</ref> |
|||
* [[Third plague pandemic]] (1855): Starting in China, it spread into India, where 10 million people died.<ref>{{cite web |url=https://www.who.int/vaccine_research/diseases/zoonotic/en/index4.html |title=Zoonotic Infections: Plague |publisher=World Health Organization |archive-url=https://web.archive.org/web/20090420003315/http://www.who.int/vaccine_research/diseases/zoonotic/en/index4.html |archive-date=20 April 2009 |access-date=5 July 2014}}</ref> During this pandemic, the United States saw its first outbreak: the [[San Francisco plague of 1900–1904]].<ref>[https://www.pbs.org/wgbh/aso/databank/entries/dm00bu.html Bubonic plague hits San Francisco 1900–1909]. ''A Science Odyssey. Public Broadcasting Service (PBS).''</ref> Today, sporadic cases of [[sylvatic plague|plague]] still occur in the western United States.<ref>{{Cite web|url=https://www.cdc.gov/mmwr/preview/mmwrhtml/00026077.htm|title=Human Plague—United States, 1993–1994|website=[[cdc.gov]]}}</ref> |
* [[Third plague pandemic]] (1855): Starting in China, it spread into India, where 10 million people died.<ref>{{cite web |url=https://www.who.int/vaccine_research/diseases/zoonotic/en/index4.html |title=Zoonotic Infections: Plague |publisher=World Health Organization |archive-url=https://web.archive.org/web/20090420003315/http://www.who.int/vaccine_research/diseases/zoonotic/en/index4.html |archive-date=20 April 2009 |access-date=5 July 2014}}</ref> During this pandemic, the United States saw its first outbreak: the [[San Francisco plague of 1900–1904]].<ref>[https://www.pbs.org/wgbh/aso/databank/entries/dm00bu.html Bubonic plague hits San Francisco 1900–1909]. ''A Science Odyssey. Public Broadcasting Service (PBS).''</ref> Today, sporadic cases of [[sylvatic plague|plague]] still occur in the western United States.<ref>{{Cite web|url=https://www.cdc.gov/mmwr/preview/mmwrhtml/00026077.htm|title=Human Plague—United States, 1993–1994|website=[[cdc.gov]]}}</ref> |
||
* The 1918–1920 [[Spanish flu]] infected half a billion people<ref name="Taubenberger" /> around the world, including on remote [[Pacific islands]] and in the [[Arctic]]—killing 20 to 100 million.<ref name="Taubenberger" /><ref>{{cite web| title=Historical Estimates of World Population| url=https://www.census.gov/population/international/data/worldpop/table_history.php| archive-url=https://web.archive.org/web/20120709092946/https://www.census.gov/population/international/data/worldpop/table_history.php| url-status=dead| archive-date=9 July 2012| access-date=29 March 2013}}</ref> Most influenza outbreaks disproportionately kill the very young and the very old, but the 1918 pandemic had an unusually high mortality rate for young adults.<ref>{{cite journal | vauthors = Gagnon A, Miller MS, Hallman SA, Bourbeau R, Herring DA, Earn DJ, Madrenas J | title = Age-specific mortality during the 1918 influenza pandemic: unravelling the mystery of high young adult mortality | journal = PLOS ONE | volume = 8 | issue = 8 | pages = e69586 | year = 2013 | pmid = 23940526 | pmc = 3734171 | doi = 10.1371/journal.pone.0069586 | bibcode = 2013PLoSO...869586G | doi-access = free }}</ref> It killed more people in 25 weeks than AIDS did in its first 25 years.<ref>{{Cite web|url=https://virus.stanford.edu/uda/|title=The 1918 Influenza Pandemic|website=virus.stanford.edu}}</ref><ref>[https://web.archive.org/web/20100127100727/http://www.channel4.com/news/articles/world/spanish%20flu%20facts/111285 Spanish flu facts by Channel{{nbsp}}4 News].</ref> Mass troop movements and close quarters during World War{{nbsp}}I caused it to spread and [[mutation|mutate]] faster, and the susceptibility of soldiers to the flu may have been increased by stress, [[malnourishment]] and [[chemical attack]]s.<ref>{{cite book| vauthors = Qureshi AI | title=Ebola Virus Disease: From Origin to Outbreak| url=https://books.google.com/books?id=7zyXCgAAQBAJ&q=Ebola+Virus+Disease:+From+Origin+to+Outbreak+Adnan+1918+pandemic&pg=PA42| page=42| publisher=Academic Press| date=2016| isbn=978-0128042427}}</ref> Improved transportation systems made it easier for soldiers, sailors and civilian travelers to spread the disease.<ref>[https://web.archive.org/web/20131211093810/http://www.xtimeline.com/evt/view.aspx?id=65022 Spanish flu strikes during World War I], 14 January 2010</ref> |
* The 1918–1920 [[Spanish flu]] infected half a billion people<ref name="Taubenberger">{{cite journal |vauthors=Taubenberger JK, Morens DM |date=January 2006 |title=1918 Influenza: the mother of all pandemics |url=https://www.cdc.gov/ncidod/eid/vol12no01/05-0979.htm |url-status=dead |journal=Emerging Infectious Diseases |volume=12 |issue=1 |pages=15–22 |doi=10.3201/eid1201.050979 |pmc=3291398 |pmid=16494711 |archive-url=https://web.archive.org/web/20091006002531/http://www.cdc.gov/ncidod/eid/vol12no01/05-0979.htm |archive-date=6 October 2009 |access-date=7 September 2017}}</ref> around the world, including on remote [[Pacific islands]] and in the [[Arctic]]—killing 20 to 100 million.<ref name="Taubenberger" /><ref>{{cite web| title=Historical Estimates of World Population| url=https://www.census.gov/population/international/data/worldpop/table_history.php| archive-url=https://web.archive.org/web/20120709092946/https://www.census.gov/population/international/data/worldpop/table_history.php| url-status=dead| archive-date=9 July 2012| access-date=29 March 2013}}</ref> Most influenza outbreaks disproportionately kill the very young and the very old, but the 1918 pandemic had an unusually high mortality rate for young adults.<ref>{{cite journal | vauthors = Gagnon A, Miller MS, Hallman SA, Bourbeau R, Herring DA, Earn DJ, Madrenas J | title = Age-specific mortality during the 1918 influenza pandemic: unravelling the mystery of high young adult mortality | journal = PLOS ONE | volume = 8 | issue = 8 | pages = e69586 | year = 2013 | pmid = 23940526 | pmc = 3734171 | doi = 10.1371/journal.pone.0069586 | bibcode = 2013PLoSO...869586G | doi-access = free }}</ref> It killed more people in 25 weeks than AIDS did in its first 25 years.<ref>{{Cite web|url=https://virus.stanford.edu/uda/|title=The 1918 Influenza Pandemic|website=virus.stanford.edu}}</ref><ref>[https://web.archive.org/web/20100127100727/http://www.channel4.com/news/articles/world/spanish%20flu%20facts/111285 Spanish flu facts by Channel{{nbsp}}4 News].</ref> Mass troop movements and close quarters during World War{{nbsp}}I caused it to spread and [[mutation|mutate]] faster, and the susceptibility of soldiers to the flu may have been increased by stress, [[malnourishment]] and [[chemical attack]]s.<ref>{{cite book| vauthors = Qureshi AI | title=Ebola Virus Disease: From Origin to Outbreak| url=https://books.google.com/books?id=7zyXCgAAQBAJ&q=Ebola+Virus+Disease:+From+Origin+to+Outbreak+Adnan+1918+pandemic&pg=PA42| page=42| publisher=Academic Press| date=2016| isbn=978-0128042427}}</ref> Improved transportation systems made it easier for soldiers, sailors and civilian travelers to spread the disease.<ref>[https://web.archive.org/web/20131211093810/http://www.xtimeline.com/evt/view.aspx?id=65022 Spanish flu strikes during World War I], 14 January 2010</ref> |
||
Encounters between European explorers and populations in the rest of the world often introduced epidemics of extraordinary virulence. Disease killed part of the native population of the [[Canary Islands]] in the 16th century ([[Guanches]]). Half the native population of [[Hispaniola]] in 1518 was killed by smallpox. [[Smallpox]] also ravaged Mexico in the 1520s, killing 150,000 in [[Tenochtitlán]] alone, including the emperor, and in [[Peru]] in the 1530s, aiding the European conquerors.<ref>{{cite web|url=https://www.bbc.co.uk/history/british/empire_seapower/smallpox_01.shtml |title=Smallpox: Eradicating the Scourge |publisher=Bbc.co.uk |date=5 November 2009 |access-date=26 August 2010}}</ref> [[Measles]] killed a further two million native Mexicans in the 17th century. In 1618–1619, smallpox wiped out 90% of the [[Massachusetts Bay]] Native Americans.<ref>[http://www.ucpress.edu/books/pages/9968/9968.ch01.html Smallpox The Fight to Eradicate a Global Scourge] {{Webarchive|url=https://web.archive.org/web/20080907093641/http://www.ucpress.edu/books/pages/9968/9968.ch01.html |date=7 September 2008 }}, David A. Koplow</ref> During the 1770s, smallpox killed at least 30% of the [[Pacific Northwest]] Native Americans.<ref>Greg Lange,[http://www.historylink.org/essays/output.cfm?file_id=5100 "Smallpox epidemic ravages Native Americans on the northwest coast of North America in the 1770s"], 23 January 2003, HistoryLink.org, ''Online Encyclopedia of Washington State History'', accessed 2 June 2008</ref> Smallpox epidemics in [[North American smallpox epidemic|1780–1782]] and [[1837-38 smallpox epidemic|1837–1838]] brought devastation and drastic depopulation among the [[Plains Indians]].<ref>{{cite journal | vauthors = Houston CS, Houston S | title = The first smallpox epidemic on the Canadian Plains: In the fur-traders' words | journal = The Canadian Journal of Infectious Diseases | volume = 11 | issue = 2 | pages = 112–115 | date = March 2000 | pmid = 18159275 | pmc = 2094753 | doi = 10.1155/2000/782978 | doi-access = free }}</ref> Some believe the death of up to 95% of the [[Population history of indigenous peoples of the Americas|Native American population]] of the [[New World]] was caused by Europeans introducing [[Old World]] diseases such as smallpox, measles and influenza.<ref>{{cite web|url=https://www.pbs.org/gunsgermssteel/variables/smallpox.html |title=The Story Of ... Smallpox—and other Deadly Eurasian Germs |publisher=Pbs.org |access-date=26 August 2010}}</ref> Over the centuries, Europeans had developed high degrees of [[herd immunity]] to these diseases, while the [[indigenous peoples]] had no such immunity.<ref>{{Cite web|url=http://www.millersville.edu/~columbus/papers/goodling.html|archive-url=https://web.archive.org/web/20080510163413/http://www.millersville.edu/~columbus/papers/goodling.html|url-status=dead|title=Stacy Goodling, "Effects of European Diseases on the Inhabitants of the New World"|archive-date=10 May 2008}}</ref> |
Encounters between European explorers and populations in the rest of the world often introduced epidemics of extraordinary virulence. Disease killed part of the native population of the [[Canary Islands]] in the 16th century ([[Guanches]]). Half the native population of [[Hispaniola]] in 1518 was killed by smallpox. [[Smallpox]] also ravaged Mexico in the 1520s, killing 150,000 in [[Tenochtitlán]] alone, including the emperor, and in [[Peru]] in the 1530s, aiding the European conquerors.<ref>{{cite web|url=https://www.bbc.co.uk/history/british/empire_seapower/smallpox_01.shtml |title=Smallpox: Eradicating the Scourge |publisher=Bbc.co.uk |date=5 November 2009 |access-date=26 August 2010}}</ref> [[Measles]] killed a further two million native Mexicans in the 17th century. In 1618–1619, smallpox wiped out 90% of the [[Massachusetts Bay]] Native Americans.<ref>[http://www.ucpress.edu/books/pages/9968/9968.ch01.html Smallpox The Fight to Eradicate a Global Scourge] {{Webarchive|url=https://web.archive.org/web/20080907093641/http://www.ucpress.edu/books/pages/9968/9968.ch01.html |date=7 September 2008 }}, David A. Koplow</ref> During the 1770s, smallpox killed at least 30% of the [[Pacific Northwest]] Native Americans.<ref>Greg Lange,[http://www.historylink.org/essays/output.cfm?file_id=5100 "Smallpox epidemic ravages Native Americans on the northwest coast of North America in the 1770s"], 23 January 2003, HistoryLink.org, ''Online Encyclopedia of Washington State History'', accessed 2 June 2008</ref> Smallpox epidemics in [[North American smallpox epidemic|1780–1782]] and [[1837-38 smallpox epidemic|1837–1838]] brought devastation and drastic depopulation among the [[Plains Indians]].<ref>{{cite journal | vauthors = Houston CS, Houston S | title = The first smallpox epidemic on the Canadian Plains: In the fur-traders' words | journal = The Canadian Journal of Infectious Diseases | volume = 11 | issue = 2 | pages = 112–115 | date = March 2000 | pmid = 18159275 | pmc = 2094753 | doi = 10.1155/2000/782978 | doi-access = free }}</ref> Some believe the death of up to 95% of the [[Population history of indigenous peoples of the Americas|Native American population]] of the [[New World]] was caused by Europeans introducing [[Old World]] diseases such as smallpox, measles and influenza.<ref>{{cite web|url=https://www.pbs.org/gunsgermssteel/variables/smallpox.html |title=The Story Of ... Smallpox—and other Deadly Eurasian Germs |publisher=Pbs.org |access-date=26 August 2010}}</ref> Over the centuries, Europeans had developed high degrees of [[herd immunity]] to these diseases, while the [[indigenous peoples]] had no such immunity.<ref>{{Cite web|url=http://www.millersville.edu/~columbus/papers/goodling.html|archive-url=https://web.archive.org/web/20080510163413/http://www.millersville.edu/~columbus/papers/goodling.html|url-status=dead|title=Stacy Goodling, "Effects of European Diseases on the Inhabitants of the New World"|archive-date=10 May 2008}}</ref> |
||
| Line 199: | Line 200: | ||
}}</ref> In the 20th century, the world saw the biggest increase in its [[World population|population]] in human history due to a drop in the [[mortality rate]] in many countries as a result of [[History of medicine#Modern medicine|medical advances]].<ref>{{Cite journal |jstor = 182701|title = The Origins of African Population Growth|journal = The Journal of African History|volume = 30|issue = 1|pages = 165–169| vauthors = Iliffe J |year = 1989|doi = 10.1017/S0021853700030942|s2cid = 59931797}}</ref> The [[world population]] has grown from 1.6 billion in 1900 to an estimated 6.8 billion in 2011.<ref>{{cite web |url=https://www.census.gov/population/popclockworld.html |title=World Population Clock—U.S. Census Bureau |publisher=U.S. Census Bureau |access-date=18 November 2011 |archive-url=https://web.archive.org/web/20111118011415/http://www.census.gov/population/popclockworld.html |archive-date=18 November 2011 |url-status=dead }}</ref> |
}}</ref> In the 20th century, the world saw the biggest increase in its [[World population|population]] in human history due to a drop in the [[mortality rate]] in many countries as a result of [[History of medicine#Modern medicine|medical advances]].<ref>{{Cite journal |jstor = 182701|title = The Origins of African Population Growth|journal = The Journal of African History|volume = 30|issue = 1|pages = 165–169| vauthors = Iliffe J |year = 1989|doi = 10.1017/S0021853700030942|s2cid = 59931797}}</ref> The [[world population]] has grown from 1.6 billion in 1900 to an estimated 6.8 billion in 2011.<ref>{{cite web |url=https://www.census.gov/population/popclockworld.html |title=World Population Clock—U.S. Census Bureau |publisher=U.S. Census Bureau |access-date=18 November 2011 |archive-url=https://web.archive.org/web/20111118011415/http://www.census.gov/population/popclockworld.html |archive-date=18 November 2011 |url-status=dead }}</ref> |
||
=== Diseases with pandemic potential === |
|||
==== Cholera ==== |
|||
{{Further|Emerging infectious disease}}In order to encourage research, a number of organisations which monitor global health have drawn up lists of diseases which may have pandemic potential; see table below.{{Efn|As of June 2023, the WHO is reviewing its list}} |
|||
{{Main|Cholera outbreaks and pandemics}} |
|||
[[File:Il cholera di Palermo del 1835.jpg|thumb|Disposal of dead bodies during the cholera epidemic in [[Palermo]] in 1835]] |
|||
Since it became widespread in the 19th century, cholera has killed tens of millions of people.<ref>[[Kelley Lee]] (2003) ''Health impacts of globalization: towards global governance''. Palgrave Macmillan. p. 131. {{ISBN|0-333-80254-3}}</ref> |
|||
* [[1817–1824 cholera pandemic]]. Previously restricted to the [[Indian subcontinent]], the pandemic began in [[Bengal]], then spread across India by 1820. 10,000 British troops and thousands of Indians died during this pandemic.{{cn|date=February 2023}} It extended as far as China, [[Indonesia]] (where more than 100,000 people succumbed on the island of [[Java]] alone) and the [[Caspian Sea]] before receding. Deaths in the Indian subcontinent between 1817 and 1860 are estimated to have exceeded 15 million. Another 23 million died between 1865 and 1917. [[Russian Empire|Russian]] deaths during a similar period exceeded 2{{nbsp}}million.<ref>{{cite web|author=G. William Beardslee |url=http://www.earlyamerica.com/review/2000_fall/1832_cholera_part1.html |title=The 1832 Cholera Epidemic in New York State |publisher=Earlyamerica.com |access-date=26 August 2010}}</ref> |
|||
* [[1826–1837 cholera pandemic]]. Reached Russia (see [[Cholera Riots]]), Hungary (about 100,000 deaths) and Germany in 1831, London in 1832 (more than 55,000 persons died in the United Kingdom),<ref>{{cite web|url=http://www.ph.ucla.edu/EPI/snow/pandemic1826-37.html |title=Asiatic Cholera Pandemic of 1826–37 |publisher=Ph.ucla.edu |access-date=26 August 2010}}</ref> France, Canada ([[Ontario]]), and United States (New York City) in the same year,<ref>{{cite web|url=http://www.tngenweb.org/darkside/cholera.html |title=The Cholera Epidemic Years in the United States |publisher=Tngenweb.org |access-date=26 August 2010}}</ref> and the Pacific coast of [[North America]] by 1834. It is believed that more than 150,000 Americans died of cholera between 1832 and 1849.<ref name=Cholera>[http://www.earlyamerica.com/review/2000_fall/1832_cholera_part2.html The 1832 Cholera Epidemic in New York State. p. 2]. By G. William Beardslee</ref> |
|||
* [[1846–1860 cholera pandemic]]. Deeply affected Russia, with more than a million deaths. A two-year outbreak began in England and Wales in 1848 and claimed 52,000 lives.<ref>[http://www.cbc.ca/health/story/2008/05/09/f-cholera-outbreaks.html Cholera's seven pandemics], cbc.ca, 2 December 2008</ref> Throughout Spain, cholera caused more than 236,000 deaths in 1854–55.<ref>{{Cite book | vauthors = Kohn GC | title = Encyclopedia of plague and pestilence: from ancient times to the present | url = https://books.google.com/books?id=tzRwRmb09rgC&pg=PA369 | publisher = Infobase Publishing | year = 2008 | page = 369 | isbn = 978-0-8160-6935-4 }} |
|||
</ref> It claimed 200,000 lives in Mexico.<ref>{{Cite book | vauthors = Byrne JP | title = Encyclopedia of Pestilence, Pandemics, and Plagues: A–M | url = https://books.google.com/books?id=5Pvi-ksuKFIC&pg=PA101 | publisher = ABC-CLIO | year = 2008 | page = 101 | isbn = 978-0-313-34102-1 }} |
|||
</ref> |
|||
* [[1863–1875 cholera pandemic]]. Spread mostly in Europe and Africa. At least 30,000 of the 90,000 [[Mecca]] pilgrims were affected by the disease. Cholera killed 90,000 people in Russia in 1866.<ref>{{cite web|url=http://www.kehilalinks.jewishgen.org/Myadel/pandemics.htm |title=Eastern European Plagues and Epidemics 1300–1918 |publisher=kehilalinks.jewishgen.org |access-date=26 August 2010}}</ref> |
|||
* In 1866, there was an outbreak in North America. It killed some 50,000 Americans.<ref name=Cholera/> |
|||
* [[1881–1896 cholera pandemic]]. The 1883–1887 epidemic cost 250,000 lives in Europe and at least 50,000 in the Americas.<ref>{{Cite journal | vauthors = Küskü F |date= January 2021 |title=Mekteplerde Hijyen, Dezenfeksiyon ve Karantina (1876-1909) / Hygiene, Disinfection and Quarantine in the Schools (1876-1909) |url=https://www.academia.edu/79059563 |journal=Osmanlı Mektepleri (Bir Modernleşme Çabası Olarak Osmanlı Eğitiminde Yeni Arayışlar)}}</ref> Cholera claimed 267,890 lives in [[Russian Empire|Russia]] (1892);<ref>{{cite EB1911 |wstitle=Cholera |volume=6 |pages=262–267}}</ref> 120,000 in Spain;<ref>{{cite news |url=https://query.nytimes.com/gst/abstract.html?res=9E05EED7123BE533A25753C2A9609C94619ED7CF |title=The cholera in Spain | work=New York Times |date=20 June 1890 |access-date=8 December 2008}}</ref> 90,000 in Japan and 60,000 in [[Iran|Persia]]. |
|||
* In 1892, cholera contaminated the water supply of [[Hamburg]] and caused 8,606 deaths.<ref>{{cite book| vauthors = Barry JM |author-link = John M. Barry|title=The Great Influenza: The Epic Story of the Greatest Plague in History|publisher=Viking Penguin|year=2004|isbn=978-0-670-89473-4|url=https://archive.org/details/greatinfluenzaep00john}}</ref> |
|||
* [[1899–1923 cholera pandemic]]. Had little effect in Europe because of advances in [[public health]], but Russia was badly affected again (more than 500,000 people dying of cholera during the first quarter of the 20th century).<ref>[https://www.britannica.com/EBchecked/topic/114078/cholera/253250/Seven-pandemics cholera :: Seven pandemics], Britannica Online Encyclopedia</ref> The sixth pandemic killed more than 800,000 in India. The 1902–1904 cholera epidemic claimed more than 200,000 lives in the [[Philippines]].<ref>[http://www3.wooster.edu/History/jgates/book-ch3.html John M. Gates, Ch. 3, "The U.S. Army and Irregular Warfare"] {{webarchive|url=https://web.archive.org/web/20140629045949/http://www3.wooster.edu/History/jgates/book-ch3.html |date=29 June 2014 }}</ref> |
|||
* [[1961–1975 cholera pandemic|Seventh cholera pandemic (1961–present)]]. Began in [[Indonesia]], called [[El Tor]] after the new biotype responsible for the pandemic, and reached [[Bangladesh]] in 1963, India in 1964, and the [[Soviet Union]] in 1966. The pandemic thereafter reached Africa in 1971 and the Americas in 1991. As of March 2022, the World Health Organization continues to define this outbreak as a current pandemic, noting that cholera has become [[endemic]] in many countries. In 2017, WHO announced a global strategy aimed at this pandemic with the goal of reducing cholera deaths by 90% by 2030.<ref name="WHO">{{cite press release |author=<!--Not stated--> |title=Cholera factsheet |url=https://www.who.int/news-room/fact-sheets/detail/cholera |location=Geneva, Switzerland |publisher=[[World Health Organization]] |
|||
|date=March 30, 2022|access-date=May 4, 2022}}</ref> |
|||
==== Dengue fever ==== |
|||
Dengue is spread by several species of female mosquitoes of the Aedes type, principally ''A. aegypti''. The virus has five types; infection with one type usually gives lifelong immunity to that type, but only short-term immunity to the others. Subsequent infection with a different type increases the risk of severe complications. Several tests are available to confirm the diagnosis including detecting antibodies to the virus or its RNA. |
|||
==== Influenza ==== |
|||
{{Main|Influenza pandemic}} |
|||
[[File:Pandemie.jpg|thumb|upright]]The Greek physician [[Hippocrates]], the "Father of Medicine", first described influenza in 412{{nbsp}}BC.<ref>{{cite web | url = http://who.int/inf-pr-1999/en/pr99-11.html | title = 50 Years of Influenza Surveillance | archive-url = https://web.archive.org/web/20090501165850/http://www.who.int/inf-pr-1999/en/pr99-11.html | archive-date=1 May 2009 | work = World Health Organization }}</ref> |
|||
* The first influenza pandemic to be pathologically described [[1510 influenza pandemic|occurred in 1510]]. Since the pandemic of 1580, influenza pandemics have occurred every 10 to 30 years.<ref>{{cite web | url = http://www.gov.im/dhss/about/Public_Health/hp/pandemicflu/ | title = Pandemic Flu | work = Department of Health and Social Security. | archive-url = https://web.archive.org/web/20120107000431/http://www.gov.im/dhss/about/Public_Health/hp/pandemicflu/ | archive-date=7 January 2012 }}</ref><ref>{{cite book | vauthors = Beveridge WI | date = 1977 | title = Influenza: The Last Great Plague: An Unfinished Story of Discovery | location = New York: Prodist | quote = Return of the Germs: For more than a century drugs and vaccines made astounding progress against infectious diseases. Now our best defenses may be social changes| isbn = 0-88202-118-4}}</ref><ref>{{cite journal | vauthors = Potter CW | title = A history of influenza | journal = Journal of Applied Microbiology | volume = 91 | issue = 4 | pages = 572–579 | date = October 2001 | pmid = 11576290 | doi = 10.1046/j.1365-2672.2001.01492.x | s2cid = 26392163 | doi-access = free }}</ref> |
|||
* The [[1889–1890 pandemic]] was attributed to influenza at the time but more recent research suggests it may have been caused by [[human coronavirus OC43]]. Also known as Russian Flu or Asiatic Flu, it was first reported in May 1889 in [[Bukhara]], [[Uzbekistan]]. By October, it had reached [[Tomsk]] and the [[Caucasus]]. It rapidly spread west and hit North America in December 1889, South America in February–April 1890, India in February–March 1890, and Australia in March–April 1890. The [[H3N8]] and [[H2N2]] subtypes of the [[influenza A virus]] have each been identified as possible causes. It had a very high attack and [[mortality rate]], causing around a million fatalities.<ref>{{cite web | url = http://www.cidrap.umn.edu/cidrap/content/influenza/panflu/biofacts/index.html | work = CIDRAP | title = Pandemic Influenza | date = 16 June 2011 }}</ref> |
|||
* The "[[Spanish flu]]", 1918–1920. First identified early in March 1918 in U.S. troops training at [[Fort Riley|Camp Funston]], [[Kansas]]. By October 1918, it had spread to become a worldwide pandemic on all continents, and eventually infected about one-third of the [[world's population]] (or ≈500 million persons).<ref name="Taubenberger" /> Unusually deadly and virulent, it persisted in pandemic form for at least two years before settling into more endemic patterns.<ref>{{Cite journal | vauthors = Chandra S, Christensen J, Likhtman S |date=November 2020 |title=Connectivity and seasonality: the 1918 influenza and COVID-19 pandemics in global perspective |journal=Journal of Global History |volume=15 |issue=3 |pages=413–414 |doi=10.1017/S1740022820000261|s2cid=228988279 |doi-access=free }}</ref> Within six months, some 50{{nbsp}}million people were dead;<ref name="Taubenberger">{{cite journal | vauthors = Taubenberger JK, Morens DM | title = 1918 Influenza: the mother of all pandemics | journal = Emerging Infectious Diseases | volume = 12 | issue = 1 | pages = 15–22 | date = January 2006 | pmid = 16494711 | pmc = 3291398 | doi = 10.3201/eid1201.050979 | url = https://www.cdc.gov/ncidod/eid/vol12no01/05-0979.htm | access-date = 7 September 2017 | url-status = dead | archive-url = https://web.archive.org/web/20091006002531/http://www.cdc.gov/ncidod/eid/vol12no01/05-0979.htm | archive-date = 6 October 2009 }}</ref> some estimates put the total number of fatalities worldwide at over twice that number.<ref>{{cite web | url = https://www.sciencedaily.com/articles/s/spanish_flu.htm | title = Spanish flu | archive-url = https://web.archive.org/web/20150325113108/http://www.sciencedaily.com/articles/s/spanish_flu.htm | archive-date=25 March 2015 | work = ScienceDaily }}</ref> About 17{{nbsp}}million died in India, 675,000 in the United States,<ref>{{cite web | url = http://1918.pandemicflu.gov/the_pandemic/index.htm | title = The Great Pandemic: The United States in 1918–1919 | archive-url = https://web.archive.org/web/20111126082941/http://1918.pandemicflu.gov/the_pandemic/index.htm | archive-date=26 November 2011 | work = U.S. Department of Health & Human Services }}</ref> and 200,000 in the United Kingdom. The virus that caused Spanish flu was also implicated as a cause of [[encephalitis lethargica]] in children.<ref>{{cite journal | vauthors = Vilensky JA, Foley P, Gilman S | title = Children and encephalitis lethargica: a historical review | journal = Pediatric Neurology | volume = 37 | issue = 2 | pages = 79–84 | date = August 2007 | pmid = 17675021 | doi = 10.1016/j.pediatrneurol.2007.04.012 }}</ref> The virus was recently reconstructed by scientists at the [[Centers for Disease Control and Prevention|CDC]] studying remains preserved by the Alaskan [[permafrost]]. The [[Pandemic H1N1/09 virus|2009 pandemic H1N1 virus]] has a small but crucial structure that is similar to the Spanish flu.<ref>{{Cite web|url=https://blogs.scientificamerican.com/observations/h1n1-shares-key-similar-structures-to-1918-flu-providing-research-avenues-for-better-vaccines/|title=H1N1 shares key similar structures to 1918 flu, providing research avenues for better vaccines| vauthors= Harmon K |website=Scientific American Blog Network}}</ref> |
|||
* The "[[1957–1958 influenza pandemic|Asian flu]]", 1957–58. An [[Influenza A virus subtype H2N2|H2N2]] virus was first identified in China in late February 1957 but not recognized globally until after an outbreak in [[Hong Kong]] in April.<ref name=":1">{{Cite journal |date=1958-12-01 |title=Symposium on the Asian Influenza Epidemic, 1957 |journal=Proceedings of the Royal Society of Medicine |language=en |volume=51 |issue=12 |pages=1009–1018 |doi=10.1177/003591575805101205 |issn=0035-9157 |doi-access=free}}</ref><ref name=":16">{{cite journal | vauthors = Murray R | title = Production and testing in the USA of influenza virus vaccine made from the Hong Kong variant in 1968-69 | journal = Bulletin of the World Health Organization | volume = 41 | issue = 3 | pages = 495–496 | date = 1969 | pmid = 5309463 | pmc = 2427701 | hdl = 10665/262478 }}</ref> From there, it spread throughout [[Southeast Asia]] and the greater continent during the spring and throughout the [[Southern Hemisphere]] during the middle months of the year, causing extensive outbreaks. By the end of September, nearly the entire inhabited world had been infected or at least seeded with the virus. The [[Northern Hemisphere]] experienced widespread outbreaks during the fall and winter, and some parts of the world saw a second wave during this time or in early 1958.<ref name=":1" /> The pandemic caused about two million deaths globally.<ref>{{cite web | url = http://news.bbc.co.uk/2/hi/health/8017585.stm | title = Q&A: Swine flu | work = BBC News | date = 27 April 2009 }}</ref> |
|||
* The "[[Hong Kong flu]]", 1968–70. An [[Influenza A virus subtype H3N2|H3N2]] virus was first detected in Hong Kong in July 1968 and spread across the world, lasting until 1970. This pandemic exhibited a more "smoldering" pattern as compared with other influenza pandemics, with uneven impact in different places over time.<ref name="Viboud">{{cite journal | vauthors = Viboud C, Grais RF, Lafont BA, Miller MA, Simonsen L | title = Multinational impact of the 1968 Hong Kong influenza pandemic: evidence for a smoldering pandemic | journal = The Journal of Infectious Diseases | volume = 192 | issue = 2 | pages = 233–248 | date = July 2005 | pmid = 15962218 | doi = 10.1086/431150 }}</ref> Its course at first resembled that of the 1957 pandemic, but after a couple of months its spread faltered; the virus did not immediately result in extensive outbreaks in some places, despite repeated introductions.<ref name=":12">{{cite journal | vauthors = Cockburn WC, Delon PJ, Ferreira W | title = Origin and progress of the 1968-69 Hong Kong influenza epidemic | journal = Bulletin of the World Health Organization | volume = 41 | issue = 3 | pages = 345–348 | year = 1969 | pmid = 5309437 | pmc = 2427756 }}</ref> The United States notably experienced an intense epidemic during the 1968–1969 flu season, the first with the pandemic virus, while European and Asian countries were relatively less affected.<ref name=":12" /><ref name="Viboud" /> During the 1969–1970 season, however, the United States was much less affected, while Europe and Asia experienced extensive outbreaks of the pandemic virus. In the Southern Hemisphere, Australia experienced a pattern more akin to Europe and Asia, with a more severe second wave.<ref name="Viboud" /> This pandemic killed approximately one million people worldwide.<ref>{{cite book| vauthors = Dumar AM |title=Swine Flu: What You Need to Know|date=2009|publisher=Wildside Press LLC|isbn=978-1434458322|page=20}}</ref> |
|||
* The "[[1977 Russian flu]]", 1977–79. An H1N1 virus was first reported by the Soviet Union in 1977. The pandemic caused an estimated 700,000 deaths worldwide<ref name=":6">{{cite journal | vauthors = Michaelis M, Doerr HW, Cinatl J | title = Novel swine-origin influenza A virus in humans: another pandemic knocking at the door | journal = Medical Microbiology and Immunology | volume = 198 | issue = 3 | pages = 175–183 | date = August 2009 | pmid = 19543913 | doi = 10.1007/s00430-009-0118-5 | s2cid = 20496301 | doi-access = free }}</ref><ref name="1977flu">{{cite journal | vauthors = Petrovski BÉ, Lumi X, Znaor L, Ivastinović D, Confalonieri F, Petrovič MG, Petrovski G | title = Reorganize and survive-a recommendation for healthcare services affected by COVID-19-the ophthalmology experience | journal = Eye | volume = 34 | issue = 7 | pages = 1177–1179 | date = July 2020 | pmid = 32313170 | pmc = 7169374 | doi = 10.1038/s41433-020-0871-7 }}</ref> and mostly affected the younger population.<ref name="1977flu2">{{cite journal | vauthors = Rozo M, Gronvall GK | title = The Reemergent 1977 H1N1 Strain and the Gain-of-Function Debate | journal = mBio | volume = 6 | issue = 4 | date = August 2015 | pmid = 26286690 | pmc = 4542197 | doi = 10.1128/mBio.01013-15 }}</ref> |
|||
* The "[[2009 swine flu pandemic|Swine flu]]", 2009–10. An H1N1 virus first detected in Mexico in early 2009. Estimates for the mortality of this pandemic range from 150 to 500 thousand.<ref>{{cite journal | vauthors = Trifonov V, Khiabanian H, Rabadan R | title = Geographic dependence, surveillance, and origins of the 2009 influenza A (H1N1) virus | journal = The New England Journal of Medicine | volume = 361 | issue = 2 | pages = 115–119 | date = July 2009 | pmid = 19474418 | doi = 10.1056/NEJMp0904572 | df = dmy-all | s2cid = 205105276 }}</ref><ref>{{Cite web|url=https://www.cdc.gov/flu/pandemic-resources/2009-h1n1-pandemic.html|title=2009 H1N1 Pandemic|date=11 June 2019|website=Centers for Disease Control and Prevention}}</ref> |
|||
==== Typhus ==== |
|||
[[Typhus]] is sometimes called "camp fever" because of its pattern of flaring up in times of strife. (It is also known as "gaol fever", "Aryotitus fever" and "ship fever", for its habits of spreading wildly in cramped quarters, such as jails and ships.) Emerging during the [[Crusades]], it had its first impact in Europe in 1489, in Spain. During fighting between the Christian Spaniards and the Muslims in [[Granada]], the Spanish lost 3,000 to war casualties, and 20,000 to typhus. In 1528, the French lost 18,000 troops in Italy, and lost supremacy in Italy to the Spanish. In 1542, 30,000 soldiers died of typhus while fighting the [[Ottoman Empire|Ottomans]] in the Balkans. |
|||
During the [[Thirty Years' War]] (1618–1648), about eight million Germans were killed by bubonic plague and typhus.<ref>[https://web.archive.org/web/20090921004137/http://www.time.com/time/magazine/article/0,9171,794989,00.html War and Pestilence]. ''Time.'' 29 April 1940</ref> The disease also played a major role in the destruction of [[Napoleon]]'s ''[[La Grande Armée|Grande Armée]]'' in Russia in 1812. During the retreat from Moscow, more French military personnel died of [[typhus]] than were killed by the Russians.<ref>[http://entomology.montana.edu/historybug/TYPHUS-Conlon.pdf The Historical Impact of Epidemic Typhus] {{webarchive|url=https://web.archive.org/web/20100611213940/http://entomology.montana.edu/historybug/TYPHUS-Conlon.pdf |date=11 June 2010}}. Joseph M. Conlon.</ref> Of the 450,000 soldiers who crossed the [[Neman River|Neman]] on 25 June 1812, fewer than 40,000 returned. More military personnel were killed from 1500 to 1914 by typhus than from military action.<ref name="TIME Magazine 1940">[https://web.archive.org/web/20090921004137/http://www.time.com/time/magazine/article/0,9171,794989,00.html War and Pestilence]. ''Time''.</ref> In early 1813, Napoleon raised a new army of 500,000 to replace his Russian losses. In the campaign of that year, more than 219,000 of Napoleon's soldiers died of typhus.<ref name=Typhus/> Typhus played a major factor in the [[Great Famine (Ireland)|Great Famine of Ireland]]. During [[World War I]], typhus epidemics killed more than 150,000 in [[Serbia]]. There were about 25 million infections and 3{{nbsp}}million deaths from [[epidemic typhus]] in Russia from 1918 to 1922.<ref name=Typhus>{{cite web |url=http://entomology.montana.edu/historybug/TYPHUS-Conlon.pdf |title=The historical impact of epidemic typhus | vauthors = Conlon JM |access-date=21 April 2009 |url-status=dead |archive-url=https://web.archive.org/web/20100611213940/http://entomology.montana.edu/historybug/TYPHUS-Conlon.pdf |archive-date=11 June 2010 }}</ref> Typhus also killed numerous prisoners in the [[Nazi concentration camps]] and Soviet prisoner of war camps during World War{{nbsp}}II. More than 3.5 million [[Nazi crimes against Soviet POWs|Soviet POWs]] died out of the 5.7 million in Nazi custody.<ref>[http://www.historynet.com/soviet-prisoners-of-war-forgotten-nazi-victims-of-world-war-ii.htm Soviet Prisoners of War: Forgotten Nazi Victims of World War II] By Jonathan Nor, TheHistoryNet</ref> |
|||
==== Smallpox ==== |
|||
[[File:Child with Smallpox Wellcome L0032953.jpg|thumb|Child with smallpox, {{circa|1908}}]] |
|||
[[Smallpox]] was a contagious disease caused by the [[variola virus]]. The disease killed an estimated 400,000 Europeans per year during the closing years of the 18th century.<ref>[https://www.ncbi.nlm.nih.gov/books/bv.fcgi?rid=vacc.chapter.3 Smallpox and Vaccinia] {{webarchive|url=https://web.archive.org/web/20090601172056/http://www.ncbi.nlm.nih.gov/books/bv.fcgi?rid=vacc.chapter.3 |date=1 June 2009}}. ''National Center for Biotechnology Information.''</ref> During the 20th century, it is estimated that smallpox was responsible for 300–500 million deaths.<ref>{{cite web|url=http://ucdavismagazine.ucdavis.edu/issues/su06/feature_1b.html |title=UC Davis Magazine, Summer 2006: Epidemics on the Horizon |access-date=3 January 2008 |url-status=dead |archive-url=https://web.archive.org/web/20081211181455/http://ucdavismagazine.ucdavis.edu/issues/su06/feature_1b.html |archive-date=11 December 2008 }}</ref><ref>[https://www.sciencedaily.com/releases/2008/01/080131122956.htm How Poxviruses Such As Smallpox Evade The Immune System], ScienceDaily, 1{{nbsp}}February 2008</ref> As recently as the early 1950s, an estimated 50 million cases of smallpox occurred in the world each year.<ref>[https://www.who.int/mediacentre/factsheets/smallpox/en/ "Smallpox"] {{webarchive|url=https://web.archive.org/web/20070921235036/http://www.who.int/mediacentre/factsheets/smallpox/en/ |date=21 September 2007 }}. ''WHO Factsheet.'' Retrieved on 22 September 2007.</ref> After successful [[vaccination]] campaigns throughout the 19th and 20th centuries, the WHO certified the eradication of smallpox in December 1979. To this day, smallpox is the only human infectious disease to have been completely eradicated,<ref>{{cite journal | vauthors = De Cock KM | title = (Book Review) The Eradication of Smallpox: Edward Jenner and The First and Only Eradication of a Human Infectious Disease| journal = Nature Medicine | year = 2001 | volume = 7 | pages = 15–16 | doi = 10.1038/83283 |doi-access=free| issue=1 }}</ref> and one of two infectious viruses ever to be eradicated, along with [[rinderpest]].<ref>{{Cite web|url=https://www.oie.int/en/for-the-media/rinderpest/|title=Rinderpest: OIE—World Organisation for Animal Health|website=oie.int}}</ref> |
|||
==== Measles ==== |
|||
Historically, [[measles]] was prevalent throughout the world, as it is highly contagious. According to the U.S. [[National Immunization Program]], by 1962 90% of people were infected with measles by age 15.<ref>{{cite journal | vauthors = Orenstein WA, Papania MJ, Wharton ME | title = Measles elimination in the United States | journal = The Journal of Infectious Diseases | volume = 189 | issue = Supplement_1 | pages = S1–S3 | date = May 2004 | pmid = 15106120 | doi = 10.1086/377693 | doi-access = free }}</ref> Before the vaccine was introduced in 1963, there were an estimated three to four million cases in the U.S. each year.<ref name=autogenerated1>Center for Disease Control & National Immunization Program. Measles History, article online 2001. Available from https://www.cdc.gov/measles/about/history.html</ref> Measles killed around 200 million people worldwide over the last 150 years.<ref name=Measles/> In 2000 alone, measles killed some 777,000 worldwide out of 40 million cases globally.<ref>{{cite journal | vauthors = Stein CE, Birmingham M, Kurian M, Duclos P, Strebel P | title = The global burden of measles in the year 2000--a model that uses country-specific indicators | journal = The Journal of Infectious Diseases | volume = 187| issue = Suppl 1 | pages = S8-14 | date = May 2003 | pmid = 12721886 | doi = 10.1086/368114 | doi-access = free }}</ref> |
|||
Measles is an [[endemic disease]], meaning it has been continually present in a community, and many people develop resistance. In populations that have not been exposed to measles, exposure to a new disease can be devastating. In 1529, a measles outbreak in [[Cuba]] killed two-thirds of the natives who had previously survived smallpox.<ref>''Man and Microbes: Disease and Plagues in History and Modern Times''; by [[Arno Karlen]]</ref> The disease had ravaged Mexico, [[Central America]], and the [[Inca]] civilization.<ref>[http://www.millersville.edu/~columbus/data/art/RUVALCA1.ART "Measles and Small Pox as an Allied Army of the Conquistadors of America"] {{Webarchive|url=https://web.archive.org/web/20090502200745/http://www.millersville.edu/~columbus/data/art/RUVALCA1.ART |date=2 May 2009 }} by Carlos Ruvalcaba, translated by Theresa M. Betz in "Encounters" (Double Issue No. 5–6, pp. 44–45)</ref> |
|||
==== Tuberculosis ==== |
|||
{{see also|History of tuberculosis#Epidemic tuberculosis}} |
|||
[[File:Tuberculosis-prevalence-WHO-2009.svg|thumb|In 2007, the prevalence of TB per 100,000 people was highest in [[Sub-Saharan Africa]], and was also relatively high in Asian countries, e.g. India.]] |
|||
One-quarter of the [[World population|world's current population]] has been infected with ''[[Mycobacterium tuberculosis]]'', and new infections occur at a rate of one per second.<ref name="WHO2004data">[[World Health Organization]] (WHO). [https://www.who.int/mediacentre/factsheets/fs104/en/index.html Tuberculosis Fact sheet No. 104—Global and regional incidence.] March 2006, Retrieved on 6 October 2006.</ref> About 5–10% of these latent infections will eventually progress to active disease, which, if left untreated, kills more than half its victims. Annually, eight million people become ill with tuberculosis, and two million die from the disease worldwide.<ref name=CDC>[[Centers for Disease Control]]. [https://www.cdc.gov/od/oc/Media/pressrel/fs050317.htm Fact Sheet: Tuberculosis in the United States.] {{webarchive|url=https://web.archive.org/web/20090423234343/http://www.cdc.gov/od/oc/media/pressrel/fs050317.htm |date=23 April 2009 }} 17 March 2005, Retrieved on 6 October 2006.</ref> In the 19th century, tuberculosis killed an estimated one-quarter of the adult population of Europe;<ref>{{Cite web |url=https://www.cdc.gov/TB/pubs/mdrtb/default.htm |title=Multidrug-Resistant Tuberculosis |access-date=7 September 2017 |archive-url=https://web.archive.org/web/20100309043219/http://www.cdc.gov/TB/pubs/mdrtb/default.htm |archive-date=9 March 2010 |url-status=dead }}</ref> by 1918, one in six deaths in France were still caused by tuberculosis. During the 20th century, tuberculosis killed approximately 100 million people.<ref name=Measles>{{cite web |url=http://birdflubook.com/a.php?id=40&t=p |author1=Torrey, EF |author2=Yolken, RH |title=Their bugs are worse than their bite |date=3 April 2005 |page=B01 |publisher=Birdflubook.com |access-date=26 August 2010 |archive-url=https://web.archive.org/web/20130626090223/http://birdflubook.com/a.php?id=40&t=p |archive-date=26 June 2013 |url-status=dead }}</ref> TB is still one of the most important health problems in the developing world.<ref>{{cite journal | vauthors = Rook GA, Dheda K, Zumla A | title = Immune responses to tuberculosis in developing countries: implications for new vaccines | journal = Nature Reviews. Immunology | volume = 5 | issue = 8 | pages = 661–667 | date = August 2005 | pmid = 16056257 | doi = 10.1038/nri1666 | s2cid = 9004625 }}</ref> In 2021, Tuberculosis became the second leading cause of death from an infectious disease, with roughly 1.6 million deaths worldwide, below [[COVID-19]].<ref>{{cite web |title=Tuberculosis |url=https://www.who.int/news-room/fact-sheets/detail/tuberculosis |website=WHO |date=24 March 2020 |access-date=31 May 2020 }}</ref> |
|||
==== Leprosy ==== |
|||
[[Leprosy]], also known as Hansen's disease, is caused by a [[Bacillus (shape)|bacillus]], ''[[Mycobacterium leprae]]''. It is a [[chronic disease]] with an incubation period of up to five years. Since 1985, 15 million people worldwide have been cured of leprosy.<ref>[http://news.bbc.co.uk/2/hi/health/6522023.stm Leprosy 'could pose new threat']. BBC News. 3 April 2007.</ref> |
|||
Historically, leprosy has affected people since at least 600 BC.<ref name=WHO_Factsheet>{{cite web | title = Leprosy | work = WHO | url =https://www.who.int/mediacentre/factsheets/fs101/en/ | access-date = 22 August 2007}}</ref> Leprosy outbreaks began to occur in Western Europe around 1000 AD.<ref>{{Cite journal | jstor=41887256| title=Medieval Leprosy Reconsidered| journal=International Social Science Review| volume=81| issue=1/2| pages=16–28| vauthors = Miller TS, Smith-Savage R | year=2006}}</ref><ref>{{cite journal | vauthors = Boldsen JL | title = Leprosy and mortality in the Medieval Danish village of Tirup | journal = American Journal of Physical Anthropology | volume = 126 | issue = 2 | pages = 159–168 | date = February 2005 | pmid = 15386293 | doi = 10.1002/ajpa.20085 }}</ref> Numerous ''leprosoria'', or [[Leper colony|leper hospitals]], sprang up in the [[Middle Ages]]; [[Matthew Paris]] estimated that in the early 13th century, there were 19,000 of them across Europe.<ref>{{CathEncy|wstitle=Leprosy}}</ref> |
|||
==== Malaria ==== |
|||
[[File:World-map-of-past-and-current-malaria-prevalence-world-development-report-2009.png|thumb|Past and current malaria prevalence in 2009]] |
|||
[[Malaria]] is widespread in [[Tropics|tropical]] and subtropical regions, including parts of the Americas, Asia, and Africa. Each year, there are approximately 350–500 million cases of malaria.<ref>{{Cite web |url=https://www.cdc.gov/malaria/facts.htm |title=Malaria Facts |access-date=7 September 2017 |archive-url=https://web.archive.org/web/20121229091605/http://www.cdc.gov/malaria/facts.htm |archive-date=29 December 2012 |url-status=dead }}</ref> [[Drug resistance]] poses a growing problem in the treatment of malaria in the 21st century, since resistance is now common against all classes of antimalarial drugs, except for the [[artemisinin]]s.<ref>{{cite journal | vauthors = White NJ | title = Antimalarial drug resistance | journal = The Journal of Clinical Investigation | volume = 113 | issue = 8 | pages = 1084–1092 | date = April 2004 | pmid = 15085184 | pmc = 385418 | doi = 10.1172/JCI21682 }}</ref> |
|||
Malaria was once common in most of Europe and North America, where it is now for all purposes non-existent.<ref>[http://www.cambridge.org/catalogue/catalogue.asp?isbn=9780511254819&ss=exc Vector- and Rodent-Borne Diseases in Europe and North America]. Norman G. Gratz. ''World Health Organization, Geneva.''</ref> Malaria may have contributed to the decline of the [[Roman Empire]].<ref>[http://news.bbc.co.uk/2/hi/science/nature/1180469.stm DNA clues to malaria in ancient Rome]. ''BBC News.'' 20 February 2001.</ref> The disease became known as "[[Roman Fever (disease)|Roman fever]]".<ref>[http://www.abc.net.au/rn/talks/perspective/stories/s776423.htm "Malaria and Rome"] {{webarchive|url=https://web.archive.org/web/20110511184622/http://www.abc.net.au/rn/talks/perspective/stories/s776423.htm |date=11 May 2011}}. Robert Sallares. ''ABC.net.au.'' 29 January 2003.</ref> ''[[Plasmodium falciparum]]'' became a real threat to colonists and [[indigenous people]] alike when it was introduced into the Americas along with the [[slave trade]]. Malaria devastated the [[Jamestown, Virginia|Jamestown]] colony and regularly ravaged the South and Midwest of the United States. By 1830, it had reached the Pacific Northwest.<ref>[https://web.archive.org/web/20090619083534/http://www.washington.edu/uwired/outreach/cspn/Website/Course%20Index/Lessons/7/7.html "The Changing World of Pacific Northwest Indians"]. ''Center for the Study of the Pacific Northwest, University of Washington.''</ref> During the [[American Civil War]], there were more than 1.2 million cases of malaria among |
|||
soldiers of both sides.<ref>{{cite web|url=http://www.infoplease.com/cig/dangerous-diseases-epidemics/malaria.html |title=A Brief History of Malaria |publisher=Infoplease.com |access-date=26 August 2010}}</ref> The [[Southern United States|southern U.S.]] continued to be affected by millions of cases of malaria into the 1930s.<ref>[http://ngm.nationalgeographic.com/ngm/0707/feature1/text3.html Malaria]. By [[Michael Finkel]]. ''National Geographic Magazine.''</ref> |
|||
==== Yellow fever ==== |
|||
[[Yellow fever]] has been a source of several devastating epidemics.<ref>{{cite EB1911 |wstitle=Yellow_Fever |volume=28 |pages=910–911}}.</ref> Cities as far north as New York, Philadelphia, and Boston were hit with epidemics. In 1793, one of the largest [[Yellow Fever Epidemic of 1793|yellow fever epidemics]] in U.S. history killed as many as 5,000 people in Philadelphia—roughly 10% of the population. About half of the residents had fled the city, including President George Washington.<ref>{{cite web | vauthors = Arnebeck B | title=A Short History of Yellow Fever in the US | work=Benjamin Rush, Yellow Fever and the Birth of Modern Medicine | date=30 January 2008 | url=http://www.geocities.com/bobarnebeck/history.html | access-date=4 December 2008 |archive-url=https://web.archive.org/web/20071107163908/http://www.geocities.com/bobarnebeck/history.html|archive-date=7 November 2007}}</ref> |
|||
Another major outbreak of the disease struck the Mississippi River Valley in 1878, with deaths estimated at 20,000. Among the hardest-hit places was Memphis, Tennessee, where 5,000 people were killed and over 20,000 fled, then representing over half the city's population, many of whom never returned. In colonial times, West Africa became known as "the white man's grave" because of malaria and yellow fever.<ref>[https://www.nytimes.com/1995/10/15/weekinreview/the-world-africa-s-nations-start-to-be-theirbrothers-keepers.html Africa's Nations Start to Be Their Brothers' Keepers]. ''The New York Times'', 15 October 1995.</ref> |
|||
== Concerns about future pandemics == |
|||
{{See also|Pandemic prevention}} |
|||
In a press conference on 28 December 2020, Mike Ryan, head of the WHO Emergencies Program, and other officials said the current COVID-19 pandemic is "not necessarily the big one" and "the next pandemic may be more severe." They called for preparation.<ref>{{Cite web|date=29 December 2020|title=WHO official: 'Next pandemic may be more severe'|url=https://arab.news/yx8p9|access-date=30 December 2020|website=Arab News|language=en}}</ref> The WHO and the UN, have warned the world must tackle the cause of pandemics and not just the health and economic symptoms.<ref>{{Cite web| vauthors = Carrington D |date=2021-03-09|title=Inaction leaves world playing 'Russian roulette' with pandemics, say experts|url=http://www.theguardian.com/environment/2021/mar/09/inaction-leaves-world-playing-russian-roulette-pandemics-experts|access-date=2021-03-10|website=The Guardian|language=en}}</ref> |
|||
The October 2020 'era of pandemics' report by the [[United Nations]]' [[Intergovernmental Science-Policy Platform on Biodiversity and Ecosystem Services]], written by 22 experts in a variety of fields, said the anthropogenic destruction of [[biodiversity]] is paving the way to the pandemic era and could result in as many as 850,000 viruses being transmitted from animals—in particular [[birds]] and [[mammals]]—to humans. The [[Overconsumption|"exponential rise" in consumption]] and trade of commodities such as [[meat]], [[palm oil]], and metals, largely facilitated by developed nations, and a [[Population growth|growing human population]], are the primary drivers of this destruction. According to [[Peter Daszak]], the chair of the group who produced the report, "there is no great mystery about the cause of the Covid-19 pandemic or any modern pandemic. The same human activities that drive [[climate change and biodiversity loss]] also drive pandemic risk through their impacts on our environment." Proposed policy options from the report include taxing meat production and consumption, cracking down on the illegal wildlife trade, removing high-risk species from the legal wildlife trade, eliminating subsidies to businesses that are harmful to the natural world, and establishing a global surveillance network.<ref>{{cite news | vauthors = Woolaston K, Fisher JL |date=29 October 2020 |title=UN report says up to 850,000 animal viruses could be caught by humans, unless we protect nature |url=https://theconversation.com/un-report-says-up-to-850-000-animal-viruses-could-be-caught-by-humans-unless-we-protect-nature-148911 |work= [[The Conversation (website)|The Conversation]]|access-date=1 December 2020}}</ref><ref>{{cite news | vauthors = Carrington D |date=29 October 2020 |title=Protecting nature is vital to escape 'era of pandemics' – report |url=https://www.theguardian.com/environment/2020/oct/29/protecting-nature-vital-pandemics-report-outbreaks-wild |work=The Guardian |access-date=1 December 2020}}</ref><ref>{{cite news |author=<!--Staff writer(s); no by-line.--> |date=29 October 2020 |title=Escaping the 'Era of Pandemics': experts warn worse crises to come; offer options to reduce risk |url=https://www.eurekalert.org/pub_releases/2020-10/tca-et102820.php |work=EurekAlert! |access-date=1 December 2020}}</ref> |
|||
In June 2021, a team of scientists assembled by the [[Harvard Medical School Center for Health and the Global Environment]] warned that the primary cause of pandemics so far, the anthropogenic destruction of the natural world through such activities including [[deforestation]] and [[hunting]], is being ignored by world leaders.<ref>{{cite news | vauthors = Carrington D |date=June 4, 2021 |title=World leaders 'ignoring' role of the destruction of nature in causing pandemics |url=https://www.theguardian.com/world/2021/jun/04/end-destruction-of-nature-to-stop-future-pandemics-say-scientists |work=The Guardian |location= |access-date=June 4, 2021}}</ref> |
|||
=== Pandemic prevention === |
|||
{{See also|Pandemic prevention}} |
|||
Prevention of future pandemics requires steps to identify future causes of pandemics and to take preventive measures before the disease moves uncontrollably into the human population. |
|||
For example, influenza is a rapidly evolving disease which has caused pandemics in the past and has potential to cause future pandemics. The World Health Organisation collates the findings of 144 national influenza centres worldwide which monitor emerging flu viruses. Virus variants which are assessed as likely to represent a significant risk are identified and can then be incorporated into the next seasonal influenza vaccine program.<ref>{{Cite web |date=3 November 2022 |title=Selecting Viruses for the Seasonal Flu Vaccine |url=https://www.cdc.gov/flu/prevent/vaccine-selection.htm |access-date=30 June 2023 |website=Centers for Disease Control and Prevention |language=en-us}}</ref> |
|||
In order to encourage research, a number of organisations which monitor global health have drawn up lists of diseases which may have pandemic potential; see table below.{{Efn|As of June 2023, the WHO is reviewing its list}} |
|||
{| class="wikitable" |
{| class="wikitable" |
||
|+List of potential pandemic diseases according to global health organisations |
|+List of potential pandemic diseases according to global health organisations |
||
| Line 357: | Line 275: | ||
|} |
|} |
||
=== |
==== Coronaviruses ==== |
||
{{Main| |
{{Main|Coronavirus|Coronavirus diseases}} |
||
{{Further|2002–2004 SARS outbreak|COVID-19 pandemic}} |
|||
[[File:SARS-CoV-2 without background.png|thumb|right|Illustration created at the [[Centers for Disease Control and Prevention]] (CDC), reveals ultrastructural morphology exhibited by coronaviruses; note the [[coronavirus spike protein|spikes]] that adorn the outer surface, which impart the look of a corona surrounding the [[virion]].<ref>{{cite journal |name-list-style=vanc |vauthors=Sonnevend J |date=December 2020 |title=A virus as an icon: the 2020 pandemic in images |journal=American Journal of Cultural Sociology |publisher=[[Palgrave Macmillan]] |volume=8 |issue=3 |pages=451–461 |doi=10.1057/s41290-020-00118-7 |eissn=2049-7121 |pmc=7537773 |pmid=33042541 |doi-access=free |veditors=Alexander JC, Jacobs RN, Smith P}}</ref>]] |
|||
[[Coronavirus]]es (CoV) are a large family of viruses that cause illness ranging from the [[common cold]] to more severe diseases such as [[Middle East respiratory syndrome]] (MERS-CoV) and [[severe acute respiratory syndrome]] (SARS-CoV-1).<ref name="ACAIM-WACEM COVID-19 Consensus Paper" /> A new strain of coronavirus (SARS-CoV-2) causes [[Coronavirus disease 2019]], or COVID-19,<ref>{{cite news |title=When a danger is growing exponentially, everything looks fine until it doesn't |language=en |newspaper=Washington Post |url=https://www.washingtonpost.com/opinions/2020/03/10/coronavirus-what-matters-isnt-what-you-can-see-what-you-cant/ |access-date=15 March 2020 |vauthors=McArdle M}}</ref> which was declared as a [[COVID-19 pandemic|pandemic]] by the WHO on 11 March 2020.<ref name="ACAIM-WACEM COVID-19 Consensus Paper" /> |
|||
Antibiotic-resistant microorganisms, which sometimes are referred to as "[[Antibiotic resistance|superbug]]s", may contribute to the re-emergence of diseases with pandemic potential that are currently well controlled.<ref>[http://www.pasteur.fr/actu/presse/press/07pesteTIGR_E.htm Researchers sound the alarm: the multidrug resistance of the plague bacillus could spread] {{Webarchive|url=https://web.archive.org/web/20071014012153/http://www.pasteur.fr/actu/presse/press/07pesteTIGR_E.htm|date=14 October 2007}}. Pasteur.fr</ref> |
|||
Some coronaviruses are [[zoonotic]], meaning they are transmitted between animals and people. Detailed investigations found that SARS-CoV-1 was transmitted from [[Masked palm civet|civet cats]] to humans and MERS-CoV from dromedary camels to humans. Several known coronaviruses are circulating in animals that have not yet infected humans. Common signs of infection include respiratory symptoms, [[fever]], [[cough]], shortness of breath, and breathing difficulties. In more severe cases, an infection can cause pneumonia, [[acute respiratory distress syndrome]], kidney failure, and even death. Standard recommendations to prevent the spread of infection include regular hand washing, wearing a face mask, going outdoors when meeting people, and avoiding close contact with people who have tested positive regardless of whether they have symptoms or not. It is recommended that people stay two meters or six feet away from others, commonly called social distancing. |
|||
For example, cases of tuberculosis that are resistant to traditionally effective treatments remain a cause of great concern to health professionals. Every year, nearly half a million new cases of [[multidrug-resistant tuberculosis]] (MDR-TB) are estimated to occur worldwide.<ref>[https://web.archive.org/web/20090406170131/http://www.who.int/mediacentre/news/releases/2009/tuberculosis_drug_resistant_20090402/en/index.html Health ministers to accelerate efforts against drug-resistant TB]. ''World Health Organization.''</ref> China and India have the highest rate of MDR-TB.<ref>[https://www.theguardian.com/society/2009/apr/01/bill-gates-tb-timebomb-china Bill Gates joins Chinese government in tackling TB 'timebomb']. ''Guardian.co.uk''. 1 April 2009</ref> The [[World Health Organization]] (WHO) reports that approximately 50 million people worldwide are infected with MDR-TB, with 79 percent of those cases resistant to three or more antibiotics. Extensively drug-resistant tuberculosis ([[XDR TB|XDR-TB]]) was first identified in Africa in 2006 and subsequently discovered to exist in 49 countries. During 2021 there were estimated to be around 25,000 cases XDR-TB worldwide.<ref>{{Cite web |title=Global Tuberculosis Report |url=https://www.who.int/teams/global-tuberculosis-programme/tb-reports |access-date=2023-06-30 |website=World Health Organisation |language=en}}</ref> |
|||
==== Dengue fever ==== |
|||
In the past 20 years, other common bacteria including ''[[Staphylococcus aureus]]'', ''[[Serratia marcescens]]'' and ''[[Enterococcus]]'', have developed resistance to a wide range of [[antibiotics]]. Antibiotic-resistant organisms have become an important cause of healthcare-associated ([[Hospital-acquired infection|nosocomial]]) infections.<ref name=":8">{{cite journal |vauthors=Murray CJ, Ikuta KS, Sharara F, Swetschinski L, Aguilar GR, Gray A, etal |date=February 2022 |title=Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis |journal=Lancet |language=English |volume=399 |issue=10325 |pages=629–655 |doi=10.1016/S0140-6736(21)02724-0 |pmc=8841637 |pmid=35065702 |s2cid=246077406 |collaboration=Antimicrobial Resistance Collaborators}}</ref> |
|||
Dengue is spread by several species of female mosquitoes of the Aedes type, principally ''A. aegypti''. The virus has five types; infection with one type usually gives lifelong immunity to that type, but only short-term immunity to the others. Subsequent infection with a different type increases the risk of severe complications. Several tests are available to confirm the diagnosis including detecting antibodies to the virus or its RNA. |
|||
=== |
==== Influenza ==== |
||
{{Main|Influenza pandemic}} |
|||
{{See|Effects of global warming on human health#Impact on infectious diseases}} |
|||
[[File:Pandemie.jpg|thumb|upright]]The Greek physician [[Hippocrates]], the "Father of Medicine", first described influenza in 412{{nbsp}}BC.<ref>{{cite web |title=50 Years of Influenza Surveillance |url=http://who.int/inf-pr-1999/en/pr99-11.html |archive-url=https://web.archive.org/web/20090501165850/http://www.who.int/inf-pr-1999/en/pr99-11.html |archive-date=1 May 2009 |work=World Health Organization}}</ref> |
|||
* The first influenza pandemic to be pathologically described [[1510 influenza pandemic|occurred in 1510]]. Since the pandemic of 1580, influenza pandemics have occurred every 10 to 30 years.<ref>{{cite web |title=Pandemic Flu |url=http://www.gov.im/dhss/about/Public_Health/hp/pandemicflu/ |archive-url=https://web.archive.org/web/20120107000431/http://www.gov.im/dhss/about/Public_Health/hp/pandemicflu/ |archive-date=7 January 2012 |work=Department of Health and Social Security.}}</ref><ref>{{cite book |title=Influenza: The Last Great Plague: An Unfinished Story of Discovery |vauthors=Beveridge WI |date=1977 |isbn=0-88202-118-4 |location=New York: Prodist |quote=Return of the Germs: For more than a century drugs and vaccines made astounding progress against infectious diseases. Now our best defenses may be social changes}}</ref><ref>{{cite journal |vauthors=Potter CW |date=October 2001 |title=A history of influenza |journal=Journal of Applied Microbiology |volume=91 |issue=4 |pages=572–579 |doi=10.1046/j.1365-2672.2001.01492.x |pmid=11576290 |s2cid=26392163 |doi-access=free}}</ref> |
|||
* The [[1889–1890 pandemic]] was attributed to influenza at the time but more recent research suggests it may have been caused by [[human coronavirus OC43]]. Also known as Russian Flu or Asiatic Flu, it was first reported in May 1889 in [[Bukhara]], [[Uzbekistan]]. By October, it had reached [[Tomsk]] and the [[Caucasus]]. It rapidly spread west and hit North America in December 1889, South America in February–April 1890, India in February–March 1890, and Australia in March–April 1890. The [[H3N8]] and [[H2N2]] subtypes of the [[influenza A virus]] have each been identified as possible causes. It had a very high attack and [[mortality rate]], causing around a million fatalities.<ref>{{cite web |date=16 June 2011 |title=Pandemic Influenza |url=http://www.cidrap.umn.edu/cidrap/content/influenza/panflu/biofacts/index.html |work=CIDRAP}}</ref> |
|||
* The "[[Spanish flu]]", 1918–1920. First identified early in March 1918 in U.S. troops training at [[Fort Riley|Camp Funston]], [[Kansas]]. By October 1918, it had spread to become a worldwide pandemic on all continents, and eventually infected about one-third of the [[world's population]] (or ≈500 million persons).<ref name="Taubenberger" /> Unusually deadly and virulent, it persisted in pandemic form for at least two years before settling into more endemic patterns.<ref>{{Cite journal |vauthors=Chandra S, Christensen J, Likhtman S |date=November 2020 |title=Connectivity and seasonality: the 1918 influenza and COVID-19 pandemics in global perspective |journal=Journal of Global History |volume=15 |issue=3 |pages=413–414 |doi=10.1017/S1740022820000261 |s2cid=228988279 |doi-access=free}}</ref> Within six months, some 50{{nbsp}}million people were dead;<ref name="Taubenberger" /> some estimates put the total number of fatalities worldwide at over twice that number.<ref>{{cite web |title=Spanish flu |url=https://www.sciencedaily.com/articles/s/spanish_flu.htm |archive-url=https://web.archive.org/web/20150325113108/http://www.sciencedaily.com/articles/s/spanish_flu.htm |archive-date=25 March 2015 |work=ScienceDaily}}</ref> About 17{{nbsp}}million died in India, 675,000 in the United States,<ref>{{cite web |title=The Great Pandemic: The United States in 1918–1919 |url=http://1918.pandemicflu.gov/the_pandemic/index.htm |archive-url=https://web.archive.org/web/20111126082941/http://1918.pandemicflu.gov/the_pandemic/index.htm |archive-date=26 November 2011 |work=U.S. Department of Health & Human Services}}</ref> and 200,000 in the United Kingdom. The virus that caused Spanish flu was also implicated as a cause of [[encephalitis lethargica]] in children.<ref>{{cite journal |vauthors=Vilensky JA, Foley P, Gilman S |date=August 2007 |title=Children and encephalitis lethargica: a historical review |journal=Pediatric Neurology |volume=37 |issue=2 |pages=79–84 |doi=10.1016/j.pediatrneurol.2007.04.012 |pmid=17675021}}</ref> The virus was recently reconstructed by scientists at the [[Centers for Disease Control and Prevention|CDC]] studying remains preserved by the Alaskan [[permafrost]]. The [[Pandemic H1N1/09 virus|2009 pandemic H1N1 virus]] has a small but crucial structure that is similar to the Spanish flu.<ref>{{Cite web |title=H1N1 shares key similar structures to 1918 flu, providing research avenues for better vaccines |url=https://blogs.scientificamerican.com/observations/h1n1-shares-key-similar-structures-to-1918-flu-providing-research-avenues-for-better-vaccines/ |website=Scientific American Blog Network |vauthors=Harmon K}}</ref> |
|||
* The "[[1957–1958 influenza pandemic|Asian flu]]", 1957–58. An [[Influenza A virus subtype H2N2|H2N2]] virus was first identified in China in late February 1957 but not recognized globally until after an outbreak in [[Hong Kong]] in April.<ref name=":1">{{Cite journal |date=1958-12-01 |title=Symposium on the Asian Influenza Epidemic, 1957 |journal=Proceedings of the Royal Society of Medicine |language=en |volume=51 |issue=12 |pages=1009–1018 |doi=10.1177/003591575805101205 |issn=0035-9157 |doi-access=free}}</ref><ref name=":16">{{cite journal |vauthors=Murray R |date=1969 |title=Production and testing in the USA of influenza virus vaccine made from the Hong Kong variant in 1968-69 |journal=Bulletin of the World Health Organization |volume=41 |issue=3 |pages=495–496 |pmc=2427701 |pmid=5309463 |hdl=10665/262478}}</ref> From there, it spread throughout [[Southeast Asia]] and the greater continent during the spring and throughout the [[Southern Hemisphere]] during the middle months of the year, causing extensive outbreaks. By the end of September, nearly the entire inhabited world had been infected or at least seeded with the virus. The [[Northern Hemisphere]] experienced widespread outbreaks during the fall and winter, and some parts of the world saw a second wave during this time or in early 1958.<ref name=":1" /> The pandemic caused about two million deaths globally.<ref>{{cite web |date=27 April 2009 |title=Q&A: Swine flu |url=http://news.bbc.co.uk/2/hi/health/8017585.stm |work=BBC News}}</ref> |
|||
* The "[[Hong Kong flu]]", 1968–70. An [[Influenza A virus subtype H3N2|H3N2]] virus was first detected in Hong Kong in July 1968 and spread across the world, lasting until 1970. This pandemic exhibited a more "smoldering" pattern as compared with other influenza pandemics, with uneven impact in different places over time.<ref name="Viboud">{{cite journal |vauthors=Viboud C, Grais RF, Lafont BA, Miller MA, Simonsen L |date=July 2005 |title=Multinational impact of the 1968 Hong Kong influenza pandemic: evidence for a smoldering pandemic |journal=The Journal of Infectious Diseases |volume=192 |issue=2 |pages=233–248 |doi=10.1086/431150 |pmid=15962218}}</ref> Its course at first resembled that of the 1957 pandemic, but after a couple of months its spread faltered; the virus did not immediately result in extensive outbreaks in some places, despite repeated introductions.<ref name=":12">{{cite journal |vauthors=Cockburn WC, Delon PJ, Ferreira W |year=1969 |title=Origin and progress of the 1968-69 Hong Kong influenza epidemic |journal=Bulletin of the World Health Organization |volume=41 |issue=3 |pages=345–348 |pmc=2427756 |pmid=5309437}}</ref> The United States notably experienced an intense epidemic during the 1968–1969 flu season, the first with the pandemic virus, while European and Asian countries were relatively less affected.<ref name=":12" /><ref name="Viboud" /> During the 1969–1970 season, however, the United States was much less affected, while Europe and Asia experienced extensive outbreaks of the pandemic virus. In the Southern Hemisphere, Australia experienced a pattern more akin to Europe and Asia, with a more severe second wave.<ref name="Viboud" /> This pandemic killed approximately one million people worldwide.<ref>{{cite book |title=Swine Flu: What You Need to Know |vauthors=Dumar AM |date=2009 |publisher=Wildside Press LLC |isbn=978-1434458322 |page=20}}</ref> |
|||
* The "[[1977 Russian flu]]", 1977–79. An H1N1 virus was first reported by the Soviet Union in 1977. The pandemic caused an estimated 700,000 deaths worldwide<ref name=":6">{{cite journal |vauthors=Michaelis M, Doerr HW, Cinatl J |date=August 2009 |title=Novel swine-origin influenza A virus in humans: another pandemic knocking at the door |journal=Medical Microbiology and Immunology |volume=198 |issue=3 |pages=175–183 |doi=10.1007/s00430-009-0118-5 |pmid=19543913 |s2cid=20496301 |doi-access=free}}</ref><ref name="1977flu">{{cite journal |vauthors=Petrovski BÉ, Lumi X, Znaor L, Ivastinović D, Confalonieri F, Petrovič MG, Petrovski G |date=July 2020 |title=Reorganize and survive-a recommendation for healthcare services affected by COVID-19-the ophthalmology experience |journal=Eye |volume=34 |issue=7 |pages=1177–1179 |doi=10.1038/s41433-020-0871-7 |pmc=7169374 |pmid=32313170}}</ref> and mostly affected the younger population.<ref name="1977flu2">{{cite journal |vauthors=Rozo M, Gronvall GK |date=August 2015 |title=The Reemergent 1977 H1N1 Strain and the Gain-of-Function Debate |journal=mBio |volume=6 |issue=4 |doi=10.1128/mBio.01013-15 |pmc=4542197 |pmid=26286690}}</ref> |
|||
* The "[[2009 swine flu pandemic|Swine flu]]", 2009–10. An H1N1 virus first detected in Mexico in early 2009. Estimates for the mortality of this pandemic range from 150 to 500 thousand.<ref>{{cite journal |vauthors=Trifonov V, Khiabanian H, Rabadan R |date=July 2009 |title=Geographic dependence, surveillance, and origins of the 2009 influenza A (H1N1) virus |journal=The New England Journal of Medicine |volume=361 |issue=2 |pages=115–119 |doi=10.1056/NEJMp0904572 |pmid=19474418 |s2cid=205105276 |df=dmy-all}}</ref><ref>{{Cite web |date=11 June 2019 |title=2009 H1N1 Pandemic |url=https://www.cdc.gov/flu/pandemic-resources/2009-h1n1-pandemic.html |website=Centers for Disease Control and Prevention}}</ref> |
|||
[[File:Barack Obama being briefed on swine flu oubreak 4-29.jpg|thumb|President [[Barack Obama]] is briefed in the Situation Room about the [[2009 swine flu pandemic|2009 flu pandemic]], which killed as many as 17,000 Americans.<ref>{{cite news |date=12 February 2010 |title=Swine flu has killed up to 17,000 in U.S.: report |work=Reuters |url=https://www.reuters.com/article/us-flu-usa/swine-flu-has-killed-up-to-17000-in-u-s-report-idUSN1223579720100212}}</ref>]] |
|||
Wild aquatic birds are the natural hosts for a range of influenza A viruses. Occasionally, viruses are transmitted from these species to other species, and may then cause outbreaks in domestic poultry or, rarely, in humans.<ref name="sobrino6">{{cite book |author=Klenk |title=Animal Viruses: Molecular Biology |publisher=Caister Academic Press |year=2008 |isbn=978-1-904455-22-6 |chapter=Avian Influenza: Molecular Mechanisms of Pathogenesis and Host Range |display-authors=etal |chapter-url=http://www.horizonpress.com/avir}}</ref><ref name="Kawaoka">{{cite book |url=http://www.horizonpress.com/flu |title=Influenza Virology: Current Topics |publisher=Caister Academic Press |year=2006 |isbn=978-1-904455-06-6 |veditors=Kawaoka Y}}</ref> |
|||
=== |
==== Leprosy ==== |
||
[[Leprosy]], also known as Hansen's disease, is caused by a [[Bacillus (shape)|bacillus]], ''[[Mycobacterium leprae]]''. It is a [[chronic disease]] with an incubation period of up to five years. Since 1985, 15 million people worldwide have been cured of leprosy.<ref>[http://news.bbc.co.uk/2/hi/health/6522023.stm Leprosy 'could pose new threat']. BBC News. 3 April 2007.</ref> |
|||
{{See|Human overpopulation#Epidemics and pandemics}} |
|||
Historically, leprosy has affected people since at least 600 BC.<ref name="WHO_Factsheet">{{cite web |title=Leprosy |url=https://www.who.int/mediacentre/factsheets/fs101/en/ |access-date=22 August 2007 |work=WHO}}</ref> Leprosy outbreaks began to occur in Western Europe around 1000 AD.<ref>{{Cite journal |vauthors=Miller TS, Smith-Savage R |year=2006 |title=Medieval Leprosy Reconsidered |journal=International Social Science Review |volume=81 |issue=1/2 |pages=16–28 |jstor=41887256}}</ref><ref>{{cite journal |vauthors=Boldsen JL |date=February 2005 |title=Leprosy and mortality in the Medieval Danish village of Tirup |journal=American Journal of Physical Anthropology |volume=126 |issue=2 |pages=159–168 |doi=10.1002/ajpa.20085 |pmid=15386293}}</ref> Numerous ''leprosoria'', or [[Leper colony|leper hospitals]], sprang up in the [[Middle Ages]]; [[Matthew Paris]] estimated that in the early 13th century, there were 19,000 of them across Europe.<ref>{{CathEncy|wstitle=Leprosy}}</ref> |
|||
=== Encroaching into wildlands === |
|||
{{See|Zoonosis#Biodiversity loss and environmental degradation|Human–wildlife conflict|Wildland–urban interface|Urban sprawl}} |
|||
=== |
==== Malaria ==== |
||
[[File:World-map-of-past-and-current-malaria-prevalence-world-development-report-2009.png|thumb|Past and current malaria prevalence in 2009]] |
|||
{{Expand section|[[Henipavirus]]es|date=June 2020}}{{Further|Emerging infectious disease}} |
|||
[[Malaria]] is widespread in [[Tropics|tropical]] and subtropical regions, including parts of the Americas, Asia, and Africa. Each year, there are approximately 350–500 million cases of malaria.<ref>{{Cite web |title=Malaria Facts |url=https://www.cdc.gov/malaria/facts.htm |url-status=dead |archive-url=https://web.archive.org/web/20121229091605/http://www.cdc.gov/malaria/facts.htm |archive-date=29 December 2012 |access-date=7 September 2017}}</ref> [[Drug resistance]] poses a growing problem in the treatment of malaria in the 21st century, since resistance is now common against all classes of antimalarial drugs, except for the [[artemisinin]]s.<ref>{{cite journal |vauthors=White NJ |date=April 2004 |title=Antimalarial drug resistance |journal=The Journal of Clinical Investigation |volume=113 |issue=8 |pages=1084–1092 |doi=10.1172/JCI21682 |pmc=385418 |pmid=15085184}}</ref> |
|||
==== Viral hemorrhagic fevers ==== |
|||
{{Main articles|Viral hemorrhagic fever}} |
|||
Viral hemorrhagic fevers such as [[Ebola virus disease]], [[Lassa fever virus|Lassa fever]], [[Rift Valley fever]], [[Marburg virus|Marburg virus disease]], [[Severe fever with thrombocytopenia syndrome|Severe fever with thrombocytopenia]] as well as [[Argentine hemorrhagic fever|Argentine]], [[Bolivian hemorrhagic fever|Bolivian]], [[Brazilian hemorrhagic fever|Brazilian]], [[Crimean–Congo hemorrhagic fever|Crimean-Congo]] and [[Venezuelan hemorrhagic fever|Venezuelan]] hemorrhagic fevers<ref>{{cite journal | vauthors = Park ES, Shimojima M, Nagata N, Ami Y, Yoshikawa T, Iwata-Yoshikawa N, Fukushi S, Watanabe S, Kurosu T, Kataoka M, Okutani A, Kimura M, Imaoka K, Hanaki K, Suzuki T, Hasegawa H, Saijo M, Maeda K, Morikawa S | display-authors = 6 | title = Severe Fever with Thrombocytopenia Syndrome Phlebovirus causes lethal viral hemorrhagic fever in cats | journal = Scientific Reports | volume = 9 | issue = 1 | pages = 11990 | date = August 2019 | pmid = 31427690 | pmc = 6700174 | doi = 10.1038/s41598-019-48317-8 | doi-access = free | bibcode = 2019NatSR...911990P }}</ref> are highly contagious and deadly diseases, with the theoretical potential to become pandemics.<ref>{{cite news |title=Fears of Ebola pandemic if violent attacks continue in DR Congo |url=https://www.aljazeera.com/news/2019/05/fears-ebola-pandemic-drc-violent-attacks-continue-190522231352900.html |work=Al-Jazeera |date=23 May 2019}}</ref><ref>{{cite journal | vauthors = Wojda TR, Valenza PL, Cornejo K, McGinley T, Galwankar SC, Kelkar D, Sharpe RP, Papadimos TJ, Stawicki SP | display-authors = 6 | title = The Ebola Outbreak of 2014-2015: From Coordinated Multilateral Action to Effective Disease Containment, Vaccine Development, and Beyond | journal = Journal of Global Infectious Diseases | volume = 7 | issue = 4 | pages = 127–138 | year = 2015 | pmid = 26752867 | pmc = 4693303 | doi = 10.4103/0974-777X.170495 | doi-access = free }}</ref> Their ability to spread efficiently enough to cause a pandemic is limited, however, as transmission of these viruses requires close contact with the infected [[Vector (epidemiology)|vector]], and the vector has only a short time before death or serious illness. Furthermore, the short time between a vector becoming infectious and the onset of symptoms allows medical professionals to quickly [[quarantine]] vectors and prevent them from carrying the pathogen elsewhere. Genetic mutations could occur, which could elevate their potential for causing widespread harm; thus, close observation by contagious disease specialists is merited.{{citation needed|date=October 2016}} |
|||
Malaria was once common in most of Europe and North America, where it is now for all purposes non-existent.<ref>[http://www.cambridge.org/catalogue/catalogue.asp?isbn=9780511254819&ss=exc Vector- and Rodent-Borne Diseases in Europe and North America]. Norman G. Gratz. ''World Health Organization, Geneva.''</ref> Malaria may have contributed to the decline of the [[Roman Empire]].<ref>[http://news.bbc.co.uk/2/hi/science/nature/1180469.stm DNA clues to malaria in ancient Rome]. ''BBC News.'' 20 February 2001.</ref> The disease became known as "[[Roman Fever (disease)|Roman fever]]".<ref>[http://www.abc.net.au/rn/talks/perspective/stories/s776423.htm "Malaria and Rome"] {{webarchive|url=https://web.archive.org/web/20110511184622/http://www.abc.net.au/rn/talks/perspective/stories/s776423.htm|date=11 May 2011}}. Robert Sallares. ''ABC.net.au.'' 29 January 2003.</ref> ''[[Plasmodium falciparum]]'' became a real threat to colonists and [[indigenous people]] alike when it was introduced into the Americas along with the [[slave trade]]. Malaria devastated the [[Jamestown, Virginia|Jamestown]] colony and regularly ravaged the South and Midwest of the United States. By 1830, it had reached the Pacific Northwest.<ref>[https://web.archive.org/web/20090619083534/http://www.washington.edu/uwired/outreach/cspn/Website/Course%20Index/Lessons/7/7.html "The Changing World of Pacific Northwest Indians"]. ''Center for the Study of the Pacific Northwest, University of Washington.''</ref> During the [[American Civil War]], there were more than 1.2 million cases of malaria among |
|||
==== Coronaviruses ==== |
|||
soldiers of both sides.<ref>{{cite web |title=A Brief History of Malaria |url=http://www.infoplease.com/cig/dangerous-diseases-epidemics/malaria.html |access-date=26 August 2010 |publisher=Infoplease.com}}</ref> The [[Southern United States|southern U.S.]] continued to be affected by millions of cases of malaria into the 1930s.<ref>[http://ngm.nationalgeographic.com/ngm/0707/feature1/text3.html Malaria]. By [[Michael Finkel]]. ''National Geographic Magazine.''</ref> |
|||
{{Main|Coronavirus|Coronavirus diseases}} |
|||
{{Further|2002–2004 SARS outbreak|COVID-19 pandemic}} |
|||
[[File:SARS-CoV-2 without background.png|thumb|right|Illustration created at the [[Centers for Disease Control and Prevention]] (CDC), reveals ultrastructural morphology exhibited by coronaviruses; note the [[coronavirus spike protein|spikes]] that adorn the outer surface, which impart the look of a corona surrounding the [[virion]].<ref>{{cite journal | vauthors = Sonnevend J | title = A virus as an icon: the 2020 pandemic in images | journal = American Journal of Cultural Sociology | volume = 8 | issue = 3 | pages = 451–461 | date = December 2020 | pmid = 33042541 | pmc = 7537773 | doi = 10.1057/s41290-020-00118-7 | veditors = Alexander JC, Jacobs RN, Smith P | eissn = 2049-7121 | publisher = [[Palgrave Macmillan]] | doi-access = free | name-list-style = vanc }}</ref>]] |
|||
==== Measles ==== |
|||
[[Coronavirus]]es (CoV) are a large family of viruses that cause illness ranging from the [[common cold]] to more severe diseases such as [[Middle East respiratory syndrome]] (MERS-CoV) and [[severe acute respiratory syndrome]] (SARS-CoV-1).<ref name="ACAIM-WACEM COVID-19 Consensus Paper"/> A new strain of coronavirus (SARS-CoV-2) causes [[Coronavirus disease 2019]], or COVID-19,<ref>{{cite news | vauthors = McArdle M |title=When a danger is growing exponentially, everything looks fine until it doesn't |url=https://www.washingtonpost.com/opinions/2020/03/10/coronavirus-what-matters-isnt-what-you-can-see-what-you-cant/ |newspaper=Washington Post |access-date=15 March 2020 |language=en}}</ref> which was declared as a [[COVID-19 pandemic|pandemic]] by the WHO on 11 March 2020.<ref name="ACAIM-WACEM COVID-19 Consensus Paper"/> |
|||
Historically, [[measles]] was prevalent throughout the world, as it is highly contagious. According to the U.S. [[National Immunization Program]], by 1962 90% of people were infected with measles by age 15.<ref>{{cite journal |vauthors=Orenstein WA, Papania MJ, Wharton ME |date=May 2004 |title=Measles elimination in the United States |journal=The Journal of Infectious Diseases |volume=189 |issue=Supplement_1 |pages=S1–S3 |doi=10.1086/377693 |pmid=15106120 |doi-access=free}}</ref> Before the vaccine was introduced in 1963, there were an estimated three to four million cases in the U.S. each year.<ref name="autogenerated1">Center for Disease Control & National Immunization Program. Measles History, article online 2001. Available from https://www.cdc.gov/measles/about/history.html</ref> Measles killed around 200 million people worldwide over the last 150 years.<ref name="Measles" /> In 2000 alone, measles killed some 777,000 worldwide out of 40 million cases globally.<ref>{{cite journal |vauthors=Stein CE, Birmingham M, Kurian M, Duclos P, Strebel P |date=May 2003 |title=The global burden of measles in the year 2000--a model that uses country-specific indicators |journal=The Journal of Infectious Diseases |volume=187 |issue=Suppl 1 |pages=S8-14 |doi=10.1086/368114 |pmid=12721886 |doi-access=free}}</ref> |
|||
Measles is an [[endemic disease]], meaning it has been continually present in a community, and many people develop resistance. In populations that have not been exposed to measles, exposure to a new disease can be devastating. In 1529, a measles outbreak in [[Cuba]] killed two-thirds of the natives who had previously survived smallpox.<ref>''Man and Microbes: Disease and Plagues in History and Modern Times''; by [[Arno Karlen]]</ref> The disease had ravaged Mexico, [[Central America]], and the [[Inca]] civilization.<ref>[http://www.millersville.edu/~columbus/data/art/RUVALCA1.ART "Measles and Small Pox as an Allied Army of the Conquistadors of America"] {{Webarchive|url=https://web.archive.org/web/20090502200745/http://www.millersville.edu/~columbus/data/art/RUVALCA1.ART|date=2 May 2009}} by Carlos Ruvalcaba, translated by Theresa M. Betz in "Encounters" (Double Issue No. 5–6, pp. 44–45)</ref> |
|||
Some coronaviruses are [[zoonotic]], meaning they are transmitted between animals and people. Detailed investigations found that SARS-CoV-1 was transmitted from [[Masked palm civet|civet cats]] to humans and MERS-CoV from dromedary camels to humans. Several known coronaviruses are circulating in animals that have not yet infected humans. Common signs of infection include respiratory symptoms, [[fever]], [[cough]], shortness of breath, and breathing difficulties. In more severe cases, an infection can cause pneumonia, [[acute respiratory distress syndrome]], kidney failure, and even death. Standard recommendations to prevent the spread of infection include regular hand washing, wearing a face mask, going outdoors when meeting people, and avoiding close contact with people who have tested positive regardless of whether they have symptoms or not. It is recommended that people stay two meters or six feet away from others, commonly called social distancing. |
|||
===== Severe acute respiratory syndrome ===== |
===== Severe acute respiratory syndrome ===== |
||
After the [[2002–2004 SARS outbreak|SARS outbreak]], in 2003 the Italian physician [[Carlo Urbani]] (1956–2003) was the first to identify severe acute respiratory syndrome ([[SARS]]) as a new and dangerously contagious disease, although he became infected and died. It is caused by a coronavirus dubbed [[Severe acute respiratory syndrome coronavirus|SARS-CoV-1]]. Rapid action by national and international health authorities such as the [[World Health Organization]] helped to slow transmission and eventually broke the chain of transmission, which ended the localized epidemics before they could become a pandemic. However, the disease has not been eradicated and could re-emerge. This warrants monitoring and reporting of suspicious cases of atypical pneumonia.<ref>{{Cite web|url=https://www.who.int/mediacentre/news/releases/2003/pr56/en/|archive-url=https://web.archive.org/web/20040825184057/http://www.who.int/mediacentre/news/releases/2003/pr56/en/ |
After the [[2002–2004 SARS outbreak|SARS outbreak]], in 2003 the Italian physician [[Carlo Urbani]] (1956–2003) was the first to identify severe acute respiratory syndrome ([[SARS]]) as a new and dangerously contagious disease, although he became infected and died. It is caused by a coronavirus dubbed [[Severe acute respiratory syndrome coronavirus|SARS-CoV-1]]. Rapid action by national and international health authorities such as the [[World Health Organization]] helped to slow transmission and eventually broke the chain of transmission, which ended the localized epidemics before they could become a pandemic. However, the disease has not been eradicated and could re-emerge. This warrants monitoring and reporting of suspicious cases of atypical pneumonia.<ref>{{Cite web |title=WHO | SARS outbreak contained worldwide |url=https://www.who.int/mediacentre/news/releases/2003/pr56/en/ |url-status=dead |archive-url=https://web.archive.org/web/20040825184057/http://www.who.int/mediacentre/news/releases/2003/pr56/en/ |archive-date=25 August 2004 |website=WHO}} |
||
be safe be active</ref> |
be safe be active</ref> |
||
==== |
==== Typhus ==== |
||
[[Typhus]] is sometimes called "camp fever" because of its pattern of flaring up in times of strife. (It is also known as "gaol fever", "Aryotitus fever" and "ship fever", for its habits of spreading wildly in cramped quarters, such as jails and ships.) Emerging during the [[Crusades]], it had its first impact in Europe in 1489, in Spain. During fighting between the Christian Spaniards and the Muslims in [[Granada]], the Spanish lost 3,000 to war casualties, and 20,000 to typhus. In 1528, the French lost 18,000 troops in Italy, and lost supremacy in Italy to the Spanish. In 1542, 30,000 soldiers died of typhus while fighting the [[Ottoman Empire|Ottomans]] in the Balkans. |
|||
{{Main|Influenza pandemic}} |
|||
[[File:Barack Obama being briefed on swine flu oubreak 4-29.jpg|thumb|President [[Barack Obama]] is briefed in the Situation Room about the [[2009 swine flu pandemic|2009 flu pandemic]], which killed as many as 17,000 Americans.<ref>{{cite news |title=Swine flu has killed up to 17,000 in U.S.: report |url=https://www.reuters.com/article/us-flu-usa/swine-flu-has-killed-up-to-17000-in-u-s-report-idUSN1223579720100212 |work=Reuters |date=12 February 2010}}</ref>]] |
|||
Wild aquatic birds are the natural hosts for a range of influenza A viruses. Occasionally, viruses are transmitted from these species to other species, and may then cause outbreaks in domestic poultry or, rarely, in humans.<ref name=sobrino6>{{cite book |chapter-url=http://www.horizonpress.com/avir |author=Klenk|year=2008 |chapter=Avian Influenza: Molecular Mechanisms of Pathogenesis and Host Range |title=Animal Viruses: Molecular Biology |publisher=Caister Academic Press |isbn=978-1-904455-22-6|display-authors=etal}}</ref><ref name=Kawaoka>{{cite book | veditors = Kawaoka Y |title=Influenza Virology: Current Topics |publisher=Caister Academic Press |year=2006 |url=http://www.horizonpress.com/flu |isbn=978-1-904455-06-6}}</ref> |
|||
During the [[Thirty Years' War]] (1618–1648), about eight million Germans were killed by bubonic plague and typhus.<ref>[https://web.archive.org/web/20090921004137/http://www.time.com/time/magazine/article/0,9171,794989,00.html War and Pestilence]. ''Time.'' 29 April 1940</ref> The disease also played a major role in the destruction of [[Napoleon]]'s ''[[La Grande Armée|Grande Armée]]'' in Russia in 1812. During the retreat from Moscow, more French military personnel died of [[typhus]] than were killed by the Russians.<ref>[http://entomology.montana.edu/historybug/TYPHUS-Conlon.pdf The Historical Impact of Epidemic Typhus] {{webarchive|url=https://web.archive.org/web/20100611213940/http://entomology.montana.edu/historybug/TYPHUS-Conlon.pdf |date=11 June 2010}}. Joseph M. Conlon.</ref> Of the 450,000 soldiers who crossed the [[Neman River|Neman]] on 25 June 1812, fewer than 40,000 returned. More military personnel were killed from 1500 to 1914 by typhus than from military action.<ref name="TIME Magazine 1940">[https://web.archive.org/web/20090921004137/http://www.time.com/time/magazine/article/0,9171,794989,00.html War and Pestilence]. ''Time''.</ref> In early 1813, Napoleon raised a new army of 500,000 to replace his Russian losses. In the campaign of that year, more than 219,000 of Napoleon's soldiers died of typhus.<ref name="Typhus" /> Typhus played a major factor in the [[Great Famine (Ireland)|Great Famine of Ireland]]. During [[World War I]], typhus epidemics killed more than 150,000 in [[Serbia]]. There were about 25 million infections and 3{{nbsp}}million deaths from [[epidemic typhus]] in Russia from 1918 to 1922.<ref name="Typhus">{{cite web |url=http://entomology.montana.edu/historybug/TYPHUS-Conlon.pdf |title=The historical impact of epidemic typhus | vauthors = Conlon JM |access-date=21 April 2009 |url-status=dead |archive-url=https://web.archive.org/web/20100611213940/http://entomology.montana.edu/historybug/TYPHUS-Conlon.pdf |archive-date=11 June 2010 }}</ref> Typhus also killed numerous prisoners in the [[Nazi concentration camps]] and Soviet prisoner of war camps during World War{{nbsp}}II. More than 3.5 million [[Nazi crimes against Soviet POWs|Soviet POWs]] died out of the 5.7 million in Nazi custody.<ref>[http://www.historynet.com/soviet-prisoners-of-war-forgotten-nazi-victims-of-world-war-ii.htm Soviet Prisoners of War: Forgotten Nazi Victims of World War II] By Jonathan Nor, TheHistoryNet</ref> |
|||
===== H5N1 (Avian flu) ===== |
|||
{{Main|Influenza A virus subtype H5N1}} |
|||
==== Smallpox ==== |
|||
In February 2004, [[avian influenza]] virus was detected in birds in [[Vietnam]], increasing fears of the emergence of new variant strains. It is feared that if the avian influenza virus combines with a human influenza virus (in a bird or a human), the new subtype created could be both highly contagious and highly lethal in humans. Such a subtype could cause a global influenza pandemic, similar to the [[Spanish flu]] or the lower mortality pandemics such as the Asian flu and the Hong Kong flu.{{cn|date=March 2023}} |
|||
[[File:Child with Smallpox Wellcome L0032953.jpg|thumb|Child with smallpox, {{circa|1908}}]] |
|||
[[Smallpox]] was a contagious disease caused by the [[variola virus]]. The disease killed an estimated 400,000 Europeans per year during the closing years of the 18th century.<ref>[https://www.ncbi.nlm.nih.gov/books/bv.fcgi?rid=vacc.chapter.3 Smallpox and Vaccinia] {{webarchive|url=https://web.archive.org/web/20090601172056/http://www.ncbi.nlm.nih.gov/books/bv.fcgi?rid=vacc.chapter.3 |date=1 June 2009}}. ''National Center for Biotechnology Information.''</ref> During the 20th century, it is estimated that smallpox was responsible for 300–500 million deaths.<ref>{{cite web|url=http://ucdavismagazine.ucdavis.edu/issues/su06/feature_1b.html |title=UC Davis Magazine, Summer 2006: Epidemics on the Horizon |access-date=3 January 2008 |url-status=dead |archive-url=https://web.archive.org/web/20081211181455/http://ucdavismagazine.ucdavis.edu/issues/su06/feature_1b.html |archive-date=11 December 2008 }}</ref><ref>[https://www.sciencedaily.com/releases/2008/01/080131122956.htm How Poxviruses Such As Smallpox Evade The Immune System], ScienceDaily, 1{{nbsp}}February 2008</ref> As recently as the early 1950s, an estimated 50 million cases of smallpox occurred in the world each year.<ref>[https://www.who.int/mediacentre/factsheets/smallpox/en/ "Smallpox"] {{webarchive|url=https://web.archive.org/web/20070921235036/http://www.who.int/mediacentre/factsheets/smallpox/en/ |date=21 September 2007 }}. ''WHO Factsheet.'' Retrieved on 22 September 2007.</ref> After successful [[vaccination]] campaigns throughout the 19th and 20th centuries, the WHO certified the eradication of smallpox in December 1979. To this day, smallpox is the only human infectious disease to have been completely eradicated,<ref>{{cite journal | vauthors = De Cock KM | title = (Book Review) The Eradication of Smallpox: Edward Jenner and The First and Only Eradication of a Human Infectious Disease| journal = Nature Medicine | year = 2001 | volume = 7 | pages = 15–16 | doi = 10.1038/83283 |doi-access=free| issue=1 }}</ref> and one of two infectious viruses ever to be eradicated, along with [[rinderpest]].<ref>{{Cite web|url=https://www.oie.int/en/for-the-media/rinderpest/|title=Rinderpest: OIE—World Organisation for Animal Health|website=oie.int}}</ref> |
|||
From October 2004 to February 2005, some 3,700 test kits of the 1957 pandemic influenza virus, H2N2, were accidentally spread around the world from a lab in the U.S.<ref>{{cite web |author=MacKenzie, D |url=https://www.newscientist.com/article/dn7261 |title=Pandemic-causing 'Asian flu' accidentally released |date=13 April 2005 |work=New Scientist }}</ref> |
|||
==== Tuberculosis ==== |
|||
In May 2005, scientists urgently called upon nations to prepare for a global influenza pandemic that could strike as much as 20% of the world's population.<ref>{{cite news |url=https://www.theguardian.com/world/2005/may/25/birdflu |title=Flu pandemic 'could hit 20% of world's population' |work=guardian.co.uk |date=25 May 2005 | location=London | access-date=21 May 2010}}</ref> |
|||
{{see also|History of tuberculosis#Epidemic tuberculosis}} |
|||
[[File:Tuberculosis-prevalence-WHO-2009.svg|thumb|In 2007, the prevalence of TB per 100,000 people was highest in [[Sub-Saharan Africa]], and was also relatively high in Asian countries, e.g. India.]] |
|||
One-quarter of the [[World population|world's current population]] has been infected with ''[[Mycobacterium tuberculosis]]'', and new infections occur at a rate of one per second.<ref name="WHO2004data">[[World Health Organization]] (WHO). [https://www.who.int/mediacentre/factsheets/fs104/en/index.html Tuberculosis Fact sheet No. 104—Global and regional incidence.] March 2006, Retrieved on 6 October 2006.</ref> About 5–10% of these latent infections will eventually progress to active disease, which, if left untreated, kills more than half its victims. Annually, eight million people become ill with tuberculosis, and two million die from the disease worldwide.<ref name="CDC">[[Centers for Disease Control]]. [https://www.cdc.gov/od/oc/Media/pressrel/fs050317.htm Fact Sheet: Tuberculosis in the United States.] {{webarchive|url=https://web.archive.org/web/20090423234343/http://www.cdc.gov/od/oc/media/pressrel/fs050317.htm |date=23 April 2009 }} 17 March 2005, Retrieved on 6 October 2006.</ref> In the 19th century, tuberculosis killed an estimated one-quarter of the adult population of Europe;<ref>{{Cite web |url=https://www.cdc.gov/TB/pubs/mdrtb/default.htm |title=Multidrug-Resistant Tuberculosis |access-date=7 September 2017 |archive-url=https://web.archive.org/web/20100309043219/http://www.cdc.gov/TB/pubs/mdrtb/default.htm |archive-date=9 March 2010 |url-status=dead }}</ref> by 1918, one in six deaths in France were still caused by tuberculosis. During the 20th century, tuberculosis killed approximately 100 million people.<ref name="Measles">{{cite web |url=http://birdflubook.com/a.php?id=40&t=p |author1=Torrey, EF |author2=Yolken, RH |title=Their bugs are worse than their bite |date=3 April 2005 |page=B01 |publisher=Birdflubook.com |access-date=26 August 2010 |archive-url=https://web.archive.org/web/20130626090223/http://birdflubook.com/a.php?id=40&t=p |archive-date=26 June 2013 |url-status=dead }}</ref> TB is still one of the most important health problems in the developing world.<ref>{{cite journal | vauthors = Rook GA, Dheda K, Zumla A | title = Immune responses to tuberculosis in developing countries: implications for new vaccines | journal = Nature Reviews. Immunology | volume = 5 | issue = 8 | pages = 661–667 | date = August 2005 | pmid = 16056257 | doi = 10.1038/nri1666 | s2cid = 9004625 }}</ref> In 2021, Tuberculosis became the second leading cause of death from an infectious disease, with roughly 1.6 million deaths worldwide, below [[COVID-19]].<ref>{{cite web |title=Tuberculosis |url=https://www.who.int/news-room/fact-sheets/detail/tuberculosis |website=WHO |date=24 March 2020 |access-date=31 May 2020 }}</ref> |
|||
In October 2005, cases of the avian flu (the deadly strain H5N1) were identified in Turkey. EU Health Commissioner Markos Kyprianou said: "We have received now confirmation that the virus found in Turkey is an avian flu H5N1 virus. There is a direct relationship with viruses found in Russia, Mongolia, and China." Cases of bird flu were also identified shortly thereafter in Romania, and then Greece. Possible cases of the virus have also been found in Croatia, Bulgaria, and the United Kingdom.<ref>{{cite news |url=http://news.bbc.co.uk/1/hi/world/europe/4348404.stm |title=Bird flu is confirmed in Greece |work=BBC News |date=17 October 2005 | access-date=3 January 2010}}</ref> |
|||
==== Yellow fever ==== |
|||
By November 2007, numerous confirmed cases of the H5N1 strain had been identified across Europe.<ref>{{cite news |url=http://news.bbc.co.uk/1/shared/spl/hi/world/05/bird_flu_map/html/1.stm |title=Bird Flu Map |work=BBC News | access-date=3 January 2010}}</ref> However, by the end of October, only 59 people had died as a result of H5N1, which was atypical of previous influenza pandemics. |
|||
[[Yellow fever]] has been a source of several devastating epidemics.<ref>{{cite EB1911 |wstitle=Yellow_Fever |volume=28 |pages=910–911}}.</ref> Cities as far north as New York, Philadelphia, and Boston were hit with epidemics. In 1793, one of the largest [[Yellow Fever Epidemic of 1793|yellow fever epidemics]] in U.S. history killed as many as 5,000 people in Philadelphia—roughly 10% of the population. About half of the residents had fled the city, including President George Washington.<ref>{{cite web | vauthors = Arnebeck B | title=A Short History of Yellow Fever in the US | work=Benjamin Rush, Yellow Fever and the Birth of Modern Medicine | date=30 January 2008 | url=http://www.geocities.com/bobarnebeck/history.html | access-date=4 December 2008 |archive-url=https://web.archive.org/web/20071107163908/http://www.geocities.com/bobarnebeck/history.html|archive-date=7 November 2007}}</ref> |
|||
Another major outbreak of the disease struck the Mississippi River Valley in 1878, with deaths estimated at 20,000. Among the hardest-hit places was Memphis, Tennessee, where 5,000 people were killed and over 20,000 fled, then representing over half the city's population, many of whom never returned. In colonial times, West Africa became known as "the white man's grave" because of malaria and yellow fever.<ref>[https://www.nytimes.com/1995/10/15/weekinreview/the-world-africa-s-nations-start-to-be-theirbrothers-keepers.html Africa's Nations Start to Be Their Brothers' Keepers]. ''The New York Times'', 15 October 1995.</ref> |
|||
Avian flu cannot be categorized as a "pandemic" because the virus cannot yet cause sustained and efficient human-to-human transmission. Cases so far are recognized to have been transmitted from bird to human, but as of December 2006 there had been few (if any) cases of proven human-to-human transmission.<ref>{{cite journal | vauthors = Beigel JH, Farrar J, Han AM, Hayden FG, Hyer R, de Jong MD, Lochindarat S, Nguyen TK, Nguyen TH, Tran TH, Nicoll A, Touch S, Yuen KY | display-authors = 6 | title = Avian influenza A (H5N1) infection in humans | journal = The New England Journal of Medicine | volume = 353 | issue = 13 | pages = 1374–1385 | date = September 2005 | pmid = 16192482 | doi = 10.1056/NEJMra052211 | collaboration = The Writing Committee of the World Health Organization (WHO) Consultation on Human Influenza A/H5 | hdl = 10722/45195 | doi-access = free }}</ref> Regular influenza viruses establish infection by attaching to receptors in the throat and lungs, but the avian influenza virus can attach only to receptors located deep in the lungs of humans, requiring close, prolonged contact with infected patients, and thus limiting person-to-person transmission.{{cn|date=March 2023}} |
|||
==== Zika virus ==== |
==== Zika virus ==== |
||
{{Main |
{{Main|2015–16 Zika virus epidemic|Zika virus|Zika fever}} |
||
An outbreak of [[Zika virus]] began in 2015 and strongly intensified throughout the start of 2016, with more than 1.5 million cases across more than a dozen countries in [[the Americas]]. The World Health Organization warned that Zika had the potential to become an explosive global pandemic if the outbreak was not controlled.<ref>{{cite web |date=28 January 2016 |title=Zika virus could become 'explosive pandemic' |url=https://www.bbc.co.uk/news/world-us-canada-35425731 |website=bbc.co.uk}}</ref><ref name="The Emergence of Zika Virus as a Global Health Security Threat: A Review and a Consensus Statement of the INDUSEM Joint Working Group (JWG)">{{cite journal |display-authors=6 |vauthors=Sikka V, Chattu VK, Popli RK, Galwankar SC, Kelkar D, Sawicki SG, Stawicki SP, Papadimos TJ |year=2016 |title=The Emergence of Zika Virus as a Global Health Security Threat: A Review and a Consensus Statement of the INDUSEM Joint working Group (JWG) |journal=Journal of Global Infectious Diseases |volume=8 |issue=1 |pages=3–15 |doi=10.4103/0974-777X.176140 |pmc=4785754 |pmid=27013839 |doi-access=free}}</ref> |
|||
== Concerns about future pandemics == |
|||
{{See also|Pandemic prevention}} |
|||
Prevention of future pandemics requires steps to identify future causes of pandemics and to take preventive measures before the disease moves uncontrollably into the human population. |
|||
For example, influenza is a rapidly evolving disease which has caused pandemics in the past and has potential to cause future pandemics. The World Health Organisation collates the findings of 144 national influenza centres worldwide which monitor emerging flu viruses. Virus variants which are assessed as likely to represent a significant risk are identified and can then be incorporated into the next seasonal influenza vaccine program.<ref>{{Cite web |date=3 November 2022 |title=Selecting Viruses for the Seasonal Flu Vaccine |url=https://www.cdc.gov/flu/prevent/vaccine-selection.htm |access-date=30 June 2023 |website=Centers for Disease Control and Prevention |language=en-us}}</ref> |
|||
In a press conference on 28 December 2020, Mike Ryan, head of the WHO Emergencies Program, and other officials said the current COVID-19 pandemic is "not necessarily the big one" and "the next pandemic may be more severe." They called for preparation.<ref>{{Cite web|date=29 December 2020|title=WHO official: 'Next pandemic may be more severe'|url=https://arab.news/yx8p9|access-date=30 December 2020|website=Arab News|language=en}}</ref> The WHO and the UN, have warned the world must tackle the cause of pandemics and not just the health and economic symptoms.<ref>{{Cite web| vauthors = Carrington D |date=2021-03-09|title=Inaction leaves world playing 'Russian roulette' with pandemics, say experts|url=http://www.theguardian.com/environment/2021/mar/09/inaction-leaves-world-playing-russian-roulette-pandemics-experts|access-date=2021-03-10|website=The Guardian|language=en}}</ref> |
|||
The October 2020 'era of pandemics' report by the [[United Nations]]' [[Intergovernmental Science-Policy Platform on Biodiversity and Ecosystem Services]], written by 22 experts in a variety of fields, said the anthropogenic destruction of [[biodiversity]] is paving the way to the pandemic era and could result in as many as 850,000 viruses being transmitted from animals—in particular [[birds]] and [[mammals]]—to humans. The [[Overconsumption|"exponential rise" in consumption]] and trade of commodities such as [[meat]], [[palm oil]], and metals, largely facilitated by developed nations, and a [[Population growth|growing human population]], are the primary drivers of this destruction. According to [[Peter Daszak]], the chair of the group who produced the report, "there is no great mystery about the cause of the Covid-19 pandemic or any modern pandemic. The same human activities that drive [[climate change and biodiversity loss]] also drive pandemic risk through their impacts on our environment." Proposed policy options from the report include taxing meat production and consumption, cracking down on the illegal wildlife trade, removing high-risk species from the legal wildlife trade, eliminating subsidies to businesses that are harmful to the natural world, and establishing a global surveillance network.<ref>{{cite news | vauthors = Woolaston K, Fisher JL |date=29 October 2020 |title=UN report says up to 850,000 animal viruses could be caught by humans, unless we protect nature |url=https://theconversation.com/un-report-says-up-to-850-000-animal-viruses-could-be-caught-by-humans-unless-we-protect-nature-148911 |work= [[The Conversation (website)|The Conversation]]|access-date=1 December 2020}}</ref><ref>{{cite news | vauthors = Carrington D |date=29 October 2020 |title=Protecting nature is vital to escape 'era of pandemics' – report |url=https://www.theguardian.com/environment/2020/oct/29/protecting-nature-vital-pandemics-report-outbreaks-wild |work=The Guardian |access-date=1 December 2020}}</ref><ref>{{cite news |author=<!--Staff writer(s); no by-line.--> |date=29 October 2020 |title=Escaping the 'Era of Pandemics': experts warn worse crises to come; offer options to reduce risk |url=https://www.eurekalert.org/pub_releases/2020-10/tca-et102820.php |work=EurekAlert! |access-date=1 December 2020}}</ref> |
|||
In June 2021, a team of scientists assembled by the [[Harvard Medical School Center for Health and the Global Environment]] warned that the primary cause of pandemics so far, the anthropogenic destruction of the natural world through such activities including [[deforestation]] and [[hunting]], is being ignored by world leaders.<ref>{{cite news | vauthors = Carrington D |date=June 4, 2021 |title=World leaders 'ignoring' role of the destruction of nature in causing pandemics |url=https://www.theguardian.com/world/2021/jun/04/end-destruction-of-nature-to-stop-future-pandemics-say-scientists |work=The Guardian |location= |access-date=June 4, 2021}}</ref> |
|||
=== Antibiotic resistance === |
|||
An outbreak of [[Zika virus]] began in 2015 and strongly intensified throughout the start of 2016, with more than 1.5 million cases across more than a dozen countries in [[the Americas]]. The World Health Organization warned that Zika had the potential to become an explosive global pandemic if the outbreak was not controlled.<ref>{{cite web |url=https://www.bbc.co.uk/news/world-us-canada-35425731 |title=Zika virus could become 'explosive pandemic' |date=28 January 2016 |website=bbc.co.uk}}</ref><ref name="The Emergence of Zika Virus as a Global Health Security Threat: A Review and a Consensus Statement of the INDUSEM Joint Working Group (JWG)">{{cite journal | vauthors = Sikka V, Chattu VK, Popli RK, Galwankar SC, Kelkar D, Sawicki SG, Stawicki SP, Papadimos TJ | display-authors = 6 | title = The Emergence of Zika Virus as a Global Health Security Threat: A Review and a Consensus Statement of the INDUSEM Joint working Group (JWG) | journal = Journal of Global Infectious Diseases | volume = 8 | issue = 1 | pages = 3–15 | year = 2016 | pmid = 27013839 | pmc = 4785754 | doi = 10.4103/0974-777X.176140 | doi-access = free }}</ref> |
|||
{{Main|Antibiotic resistance}} |
|||
Antibiotic-resistant microorganisms, which sometimes are referred to as "[[Antibiotic resistance|superbug]]s", may contribute to the re-emergence of diseases with pandemic potential that are currently well controlled.<ref>[http://www.pasteur.fr/actu/presse/press/07pesteTIGR_E.htm Researchers sound the alarm: the multidrug resistance of the plague bacillus could spread] {{Webarchive|url=https://web.archive.org/web/20071014012153/http://www.pasteur.fr/actu/presse/press/07pesteTIGR_E.htm|date=14 October 2007}}. Pasteur.fr</ref> |
|||
For example, cases of tuberculosis that are resistant to traditionally effective treatments remain a cause of great concern to health professionals. Every year, nearly half a million new cases of [[multidrug-resistant tuberculosis]] (MDR-TB) are estimated to occur worldwide.<ref>[https://web.archive.org/web/20090406170131/http://www.who.int/mediacentre/news/releases/2009/tuberculosis_drug_resistant_20090402/en/index.html Health ministers to accelerate efforts against drug-resistant TB]. ''World Health Organization.''</ref> China and India have the highest rate of MDR-TB.<ref>[https://www.theguardian.com/society/2009/apr/01/bill-gates-tb-timebomb-china Bill Gates joins Chinese government in tackling TB 'timebomb']. ''Guardian.co.uk''. 1 April 2009</ref> The [[World Health Organization]] (WHO) reports that approximately 50 million people worldwide are infected with MDR-TB, with 79 percent of those cases resistant to three or more antibiotics. Extensively drug-resistant tuberculosis ([[XDR TB|XDR-TB]]) was first identified in Africa in 2006 and subsequently discovered to exist in 49 countries. During 2021 there were estimated to be around 25,000 cases XDR-TB worldwide.<ref>{{Cite web |title=Global Tuberculosis Report |url=https://www.who.int/teams/global-tuberculosis-programme/tb-reports |access-date=2023-06-30 |website=World Health Organisation |language=en}}</ref> |
|||
In the past 20 years, other common bacteria including ''[[Staphylococcus aureus]]'', ''[[Serratia marcescens]]'' and ''[[Enterococcus]]'', have developed resistance to a wide range of [[antibiotics]]. Antibiotic-resistant organisms have become an important cause of healthcare-associated ([[Hospital-acquired infection|nosocomial]]) infections.<ref name=":8">{{cite journal |vauthors=Murray CJ, Ikuta KS, Sharara F, Swetschinski L, Aguilar GR, Gray A, etal |date=February 2022 |title=Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis |journal=Lancet |language=English |volume=399 |issue=10325 |pages=629–655 |doi=10.1016/S0140-6736(21)02724-0 |pmc=8841637 |pmid=35065702 |s2cid=246077406 |collaboration=Antimicrobial Resistance Collaborators}}</ref> |
|||
=== Climate change === |
|||
{{See|Effects of global warming on human health#Impact on infectious diseases}} |
|||
=== Overpopulation === |
|||
{{See|Human overpopulation#Epidemics and pandemics}} |
|||
=== Encroaching into wildlands === |
|||
{{See|Zoonosis#Biodiversity loss and environmental degradation|Human–wildlife conflict|Wildland–urban interface|Urban sprawl}} |
|||
Viral hemorrhagic fevers{{Main articles|Viral hemorrhagic fever}} |
|||
Viral hemorrhagic fevers such as [[Ebola virus disease]], [[Lassa fever virus|Lassa fever]], [[Rift Valley fever]], [[Marburg virus|Marburg virus disease]], [[Severe fever with thrombocytopenia syndrome|Severe fever with thrombocytopenia]] as well as [[Argentine hemorrhagic fever|Argentine]], [[Bolivian hemorrhagic fever|Bolivian]], [[Brazilian hemorrhagic fever|Brazilian]], [[Crimean–Congo hemorrhagic fever|Crimean-Congo]] and [[Venezuelan hemorrhagic fever|Venezuelan]] hemorrhagic fevers<ref>{{cite journal | vauthors = Park ES, Shimojima M, Nagata N, Ami Y, Yoshikawa T, Iwata-Yoshikawa N, Fukushi S, Watanabe S, Kurosu T, Kataoka M, Okutani A, Kimura M, Imaoka K, Hanaki K, Suzuki T, Hasegawa H, Saijo M, Maeda K, Morikawa S | display-authors = 6 | title = Severe Fever with Thrombocytopenia Syndrome Phlebovirus causes lethal viral hemorrhagic fever in cats | journal = Scientific Reports | volume = 9 | issue = 1 | pages = 11990 | date = August 2019 | pmid = 31427690 | pmc = 6700174 | doi = 10.1038/s41598-019-48317-8 | doi-access = free | bibcode = 2019NatSR...911990P }}</ref> are highly contagious and deadly diseases, with the theoretical potential to become pandemics.<ref>{{cite news |title=Fears of Ebola pandemic if violent attacks continue in DR Congo |url=https://www.aljazeera.com/news/2019/05/fears-ebola-pandemic-drc-violent-attacks-continue-190522231352900.html |work=Al-Jazeera |date=23 May 2019}}</ref><ref>{{cite journal | vauthors = Wojda TR, Valenza PL, Cornejo K, McGinley T, Galwankar SC, Kelkar D, Sharpe RP, Papadimos TJ, Stawicki SP | display-authors = 6 | title = The Ebola Outbreak of 2014-2015: From Coordinated Multilateral Action to Effective Disease Containment, Vaccine Development, and Beyond | journal = Journal of Global Infectious Diseases | volume = 7 | issue = 4 | pages = 127–138 | year = 2015 | pmid = 26752867 | pmc = 4693303 | doi = 10.4103/0974-777X.170495 | doi-access = free }}</ref> Their ability to spread efficiently enough to cause a pandemic is limited, however, as transmission of these viruses requires close contact with the infected [[Vector (epidemiology)|vector]], and the vector has only a short time before death or serious illness. Furthermore, the short time between a vector becoming infectious and the onset of symptoms allows medical professionals to quickly [[quarantine]] vectors and prevent them from carrying the pathogen elsewhere. Genetic mutations could occur, which could elevate their potential for causing widespread harm; thus, close observation by contagious disease specialists is merited.{{citation needed|date=October 2016}} |
|||
== Economic consequences == |
== Economic consequences == |
||
Revision as of 11:25, 12 July 2023

A pandemic (/pænˈdɛmɪk/ pan-DEM-ik) is an epidemic of an infectious disease that has spread across a large region, for instance multiple continents or worldwide, affecting a substantial number of individuals. Widespread endemic diseases with a stable number of infected individuals such as recurrences of seasonal influenza are generally excluded as they occur simultaneously in large regions of the globe rather than being spread worldwide.
Throughout human history, there have been a number of pandemics of diseases such as smallpox. The most fatal pandemic in recorded history was the Black Death—also known as The Plague—which killed an estimated 75–200 million people in the 14th century.[2][3][4][5] The term had not been used then but was used for later epidemics, including the 1918 influenza pandemic—more commonly known as the Spanish flu.[6][7][8]
Current pandemics include HIV/AIDS and COVID-19.[9][10][11][12]
In response to the COVID-19 pandemic, recently 194 member states of the World Health Organization began negotiations on an International Treaty on Pandemic Prevention, Preparedness and Response with a requirement to submit a draft of this treaty to the 77th World Health Assembly during its 2024 convention. This is expected to set rules for dealing with a pandemic by the international community.[13][14]
Definition
A medical dictionary definition of pandemic is "an epidemic occurring on a scale that crosses international boundaries, usually affecting people on a worldwide scale".[15] A disease or condition is not a pandemic merely because it is widespread or kills many people; it must also be infectious. For instance, cancer is responsible for many deaths but is not considered a pandemic because the disease is not contagious—i.e. easily transmissible—and not even simply infectious.[16] This definition differs from colloquial usage in that it encompasses outbreaks of relatively mild diseases.[17][18]
The World Health Organization (WHO) nearest equivalent of "pandemic" is the Public Health Emergency of International Concern, defined as “an extraordinary event which is determined to constitute a public health risk to other States through the international spread of disease and to potentially require a coordinated international response”.[19] There is a rigorous process underlying this categorisation and a clearly defined trajectory of responses.[20]
A WHO-sponsored international body, tasked with preparing an international agreement on pandemic prevention, preparedness and response has defined a pandemic as "the global spread of a pathogen or variant that infects human populations with limited or no immunity through sustained and high transmissibility from person to person, overwhelming health systems with severe morbidity and high mortality, and causing social and economic disruptions, all of which require effective national and global collaboration and coordination for its control".[21]
The word comes from the Greek παν- pan- meaning "all", or "every" and δῆμος demos "people".
Assessment
Stages
For a novel influenza virus, the World Health Organization previously applied a six-stage classification to describe the process by which the virus moves from the first few infections in humans through to a pandemic. It starts when mostly animals are infected with a virus and a few cases where animals infect people, then moves to the stage where the virus begins to be transmitted directly between people and ends with the stage when infections in humans from the virus have spread worldwide. In February 2020, a WHO spokesperson clarified that "there is no official category [for a pandemic]".[a][22]
| Phase | Probability | Transmission route | |
|---|---|---|---|
| 1 | Uncertain | Animal-to-animal infection only | – |
| 2 | Uncertain | Animal-to-human infection | (Considered a human pandemic threat) |
| 3 | Uncertain | Sporadic or clustered cases in humans | No sustained community-level outbreaks |
| 4 | Medium to high | Human-to-human transmission | Sustained community-level outbreaks |
| 5 | High to certain | Sustained in two countries in one WHO region | |
| 6 | Pandemic in progress | Sustained in-country in another WHO region | |
| Post-peak | Levels drop below the peak in most countries[Note 1] | ||
| Possible new wave | Activity rising again in most countries[Note 1] | ||
| Post-pandemic | Levels return to ordinary seasonal levels |
- ^ a b Among countries with adequate surveillance
During the 2009 influenza pandemic, Keiji Fukuda, Assistant Director-General ad interim for Health Security and Environment, WHO said "An easy way to think about pandemic ... is to say: a pandemic is a global outbreak. Then you might ask yourself: 'What is a global outbreak?' Global outbreak means that we see both the spread of the agent ... and then we see disease activities in addition to the spread of the virus."[24]
In planning for a possible influenza pandemic, the WHO published a document on pandemic preparedness guidance in 1999, which was revised in 2005 and 2009. It defined phases and appropriate actions for each phase in an aide-mémoire titled WHO pandemic phase descriptions and main actions by phase. The 2009 revision, including descriptions of a pandemic and the phases leading to its declaration, was finalized in February 2009. The 2009 H1N1 virus pandemic was neither on the horizon at that time nor mentioned in the document.[25][26] All versions of this document refer to influenza. The phases are defined by the spread of the disease; virulence and mortality are not mentioned in the current WHO definition, although these factors have previously been included.[27]

In 2014, the United States Centers for Disease Control and Prevention introduced an analogous framework to the WHO's pandemic stages titled the Pandemic Intervals Framework.[28] It includes two pre-pandemic intervals,
- Investigation
- Recognition
and four pandemic intervals,
- Initiation
- Acceleration
- Deceleration
- Preparation
It also includes a table defining the intervals and mapping them to the WHO pandemic stages.
Severity
In 2014, the United States Centers for Disease Control and Prevention adopted the Pandemic Severity Assessment Framework (PSAF) to assess the severity of pandemics.[28] The PSAF superseded the 2007 linear Pandemic Severity Index, which assumed 30% spread and measured case fatality rate (CFR) to assess the severity and evolution of the pandemic.[30]
Historically, measures of pandemic severity were based on the case fatality rate.[31] However, the case fatality rate might not be an adequate measure of pandemic severity during a pandemic response because:[29]
- Deaths may lag several weeks behind cases, making the case fatality rate an underestimate
- The total number of cases may not be known, making the case fatality rate an overestimate[32]
- A single case fatality rate for the entire population may obscure the effect on vulnerable sub-populations, such as children, the elderly, those with chronic conditions, and members of certain racial and ethnic minorities
- Fatalities alone may not account for the full effects of the pandemic, such as absenteeism or demand for healthcare services
To account for the limitations of measuring the case fatality rate alone, the PSAF rates the severity of a disease outbreak on two dimensions: clinical severity of illness in infected persons; and the transmissibility of the infection in the population.[29] Each dimension can be measured using more than one metric, which are scaled to allow comparison of the different metrics. Clinical severity can instead be measured, for example, as the ratio of deaths to hospitalizations or using genetic markers of virulence. Transmissibility can be measured, for example, as the basic reproduction number R0 and serial interval or via underlying population immunity. The framework gives guidelines for scaling the various measures and examples of assessing past pandemics using the framework.
Management

The basic strategies in the control of an outbreak are containment and mitigation. Containment may be undertaken in the early stages of the outbreak, including contact tracing and isolating infected individuals to stop the disease from spreading to the rest of the population, other public health interventions on infection control, and therapeutic countermeasures such as vaccinations which may be effective if available.[40] When it becomes apparent that it is no longer possible to contain the spread of the disease, management will then move on to the mitigation stage, in which measures are taken to slow the spread of the disease and mitigate its effects on society and the healthcare system. In reality, containment and mitigation measures may be undertaken simultaneously.[41]
A key part of managing an infectious disease outbreak is trying to decrease the epidemic peak, known as "flattening the curve".[33][36] This helps decrease the risk of health services being overwhelmed and provides more time for a vaccine and treatment to be developed.[33][36] A broad group of the so-called non-pharmaceutical interventions may be taken to manage the outbreak.[36] In a flu pandemic, these actions may include personal preventive measures such as hand hygiene, wearing face-masks, and self-quarantine; community measures aimed at social distancing such as closing schools and canceling mass gatherings; community engagement to encourage acceptance and participation in such interventions; and environmental measures such as cleaning of surfaces.[34]
Another strategy, suppression, requires more extreme long-term non-pharmaceutical interventions to reverse the pandemic by reducing the basic reproduction number to less than 1. The suppression strategy, which includes stringent population-wide social distancing, home isolation of cases, and household quarantine, was undertaken by China during the COVID-19 pandemic where entire cities were placed under lockdown; such a strategy may carry with it considerable social and economic costs.[42]
Notable pandemics and outbreaks
Current outbreaks
Mpox

Commencement: 2022. Status: Ongoing
An outbreak of mpox (formerly known as "monkeypox") was identified in May 2022.[43] This zoonotic disease is endemic to tropical Africa where there is a natural reservoir of infection in small mammals. The virus is genetically related to smallpox but with milder symptoms and fewer fatalities. The first few cases were identified in the United Kingdom, [44] with a subsequent exponential increase in cases in Europe, the Americas, Asia, Africa, and in Oceania. In July 2022, the World Health Organization (WHO), declared the outbreak a public health emergency of international concern (PHEIC); this status was withdrawn in May 2023.[45][46] The majority of confirmed cases occurred men who have sex with men (MSM) who had recent sexual contact with new or multiple partners.[47] The international response to this outbreak included re-purposing stockpiles of smallpox vaccine and targeting vulnerable groups for vaccination,[48] together with public awareness campaigns.[49] As of 27 April 2023, there had been a total of 87,113 confirmed cases in over 111 countries with 130 deaths, and the number of cases reported weekly was steadily declining.[50]
COVID-19
Commencement: 2019. Status: Ongoing

SARS-CoV-2, a new strain of coronavirus, was first detected in the city of Wuhan, Hubei Province, China, in December 2019.[52] It caused a pandemic of an acute respiratory disease, known as COVID-19.[36] More than 200 countries and territories have been affected by COVID-19, with major outbreaks occurring in Brazil, Russia, India, Mexico, Peru, South Africa,[53][54] Western Europe, and the United States.[36] In March 2020, the World Health Organization characterized the spread of COVID-19 as a Public Health Emergency of International Concern (PHEIC - equivalent to a pandemic). Three years later, in May 2023, WHO declared COVID-19 to no longer be a PHEIC, but stated this did not constitute an end to the pandemic itself.[55][56] As of 19 June 2023, the number of people infected with COVID-19 has reached more than 767 million worldwide, with a death toll of 6.9 million.[57] It is believed that these figures underestimate true totals as testing was not widely available in the initial stages of the outbreak and many people infected by the virus have no or only mild symptoms. Similarly, the number of deaths may also be understated as fatalities may have not been tested or are attributed to other conditions.[36]
HIV/AIDS
Commencement: 1966. Status: Ongoing

Although the WHO uses the term "global epidemic" to describe HIV,[61] as HIV is no longer an uncontrollable outbreak outside of Africa, some authors use the term "pandemic".[62] HIV originated in Africa, and spread to the United States via Haiti between 1966 and 1972.[63] AIDS is currently a pandemic in Africa, with infection rates as high as 25% in some regions of southern and eastern Africa. In 2006, the HIV prevalence among pregnant women in South Africa was 29%.[64] Effective education about safer sexual practices and bloodborne infection precautions training have helped to slow down infection rates in several African countries sponsoring national education programs.[citation needed] There were an estimated 1.5 million new infections of HIV/AIDS in 2020. As of 2021[update] there have been about a total of 40.1 million deaths related to HIV/AIDS since the epidemic started.[65]
Pandemics in history



In human history, it is generally zoonoses such as influenza and tuberculosis which constitute most of the widespread outbreaks, resulting from the domestication of animals. There have been many particularly significant epidemics that deserve mention above the "mere" destruction of cities:
- Plague of Athens (430 to 426 BC): During the Peloponnesian War, typhoid fever killed a quarter of the Athenian troops and a quarter of the population. This disease fatally weakened the dominance of Athens, but the sheer virulence of the disease prevented its wider spread; i.e., it killed off its hosts at a rate faster than they could spread it. The exact cause of the plague was unknown for many years. In January 2006, researchers from the University of Athens analyzed teeth recovered from a mass grave underneath the city and confirmed the presence of bacteria responsible for typhoid.[67]
- Antonine Plague (165 to 180 AD): Possibly measles or smallpox brought to the Italian peninsula by soldiers returning from the Near East, it killed a quarter of those infected, up to five million in total.[68]
- Plague of Cyprian (251–266 AD): A second outbreak of what may have been the same disease as the Antonine Plague killed (it was said) 5,000 people a day in Rome.[citation needed]
- Plague of Justinian (541 to 549 AD): Also known as the FIrst Plague Pandemic. This epidemic started in Egypt and reached Constantinople the following spring, killing (according to the Byzantine chronicler Procopius) 10,000 a day at its height, and perhaps 40% of the city's inhabitants. The plague went on to eliminate a quarter to half the human population of the known world and was identified in 2013 as being caused by bubonic plague.[69][70][71]
- Black Death (1331 to 1353): Also known as the Second Plague Pandemic. The total number of deaths worldwide is estimated at 75 to 200 million. Starting in Asia, the disease reached the Mediterranean and western Europe in 1348 (possibly from Italian merchants fleeing fighting in Crimea) and killed an estimated 20 to 30 million Europeans in six years;[72] a third of the total population,[73] and up to a half in the worst-affected urban areas.[74] It was the first of a cycle of European plague epidemics that continued until the 18th century;[75] there were more than 100 plague epidemics in Europe during this period, [76] including the Great Plague of London of 1665–66 which killed approximately 100,000 people, 20% of London's population.[77]
- 1817–1824 cholera pandemic. Previously restricted to the Indian subcontinent, the pandemic began in Bengal, then spread across India by 1820. 10,000 British troops and thousands of Indians died during this pandemic.[citation needed] It extended as far as China, Indonesia (where more than 100,000 people succumbed on the island of Java alone) and the Caspian Sea before receding. Deaths in the Indian subcontinent between 1817 and 1860 are estimated to have exceeded 15 million. Another 23 million died between 1865 and 1917. Russian deaths during a similar period exceeded 2 million.[78]
- Third plague pandemic (1855): Starting in China, it spread into India, where 10 million people died.[79] During this pandemic, the United States saw its first outbreak: the San Francisco plague of 1900–1904.[80] Today, sporadic cases of plague still occur in the western United States.[81]
- The 1918–1920 Spanish flu infected half a billion people[82] around the world, including on remote Pacific islands and in the Arctic—killing 20 to 100 million.[82][83] Most influenza outbreaks disproportionately kill the very young and the very old, but the 1918 pandemic had an unusually high mortality rate for young adults.[84] It killed more people in 25 weeks than AIDS did in its first 25 years.[85][86] Mass troop movements and close quarters during World War I caused it to spread and mutate faster, and the susceptibility of soldiers to the flu may have been increased by stress, malnourishment and chemical attacks.[87] Improved transportation systems made it easier for soldiers, sailors and civilian travelers to spread the disease.[88]
Encounters between European explorers and populations in the rest of the world often introduced epidemics of extraordinary virulence. Disease killed part of the native population of the Canary Islands in the 16th century (Guanches). Half the native population of Hispaniola in 1518 was killed by smallpox. Smallpox also ravaged Mexico in the 1520s, killing 150,000 in Tenochtitlán alone, including the emperor, and in Peru in the 1530s, aiding the European conquerors.[89] Measles killed a further two million native Mexicans in the 17th century. In 1618–1619, smallpox wiped out 90% of the Massachusetts Bay Native Americans.[90] During the 1770s, smallpox killed at least 30% of the Pacific Northwest Native Americans.[91] Smallpox epidemics in 1780–1782 and 1837–1838 brought devastation and drastic depopulation among the Plains Indians.[92] Some believe the death of up to 95% of the Native American population of the New World was caused by Europeans introducing Old World diseases such as smallpox, measles and influenza.[93] Over the centuries, Europeans had developed high degrees of herd immunity to these diseases, while the indigenous peoples had no such immunity.[94]
Smallpox, introduced by European settlers in 1789 to the Australian continent, devastated the Australian Aboriginal population, killing up to 50% of those infected with the disease during the first decades of colonisation.[95] It also killed many New Zealand Māori.[96] In 1848–49, as many as 40,000 out of 150,000 Hawaiians are estimated to have died of measles, whooping cough and influenza. Introduced diseases, notably smallpox, nearly wiped out the native population of Easter Island.[97] Measles killed more than 40,000 Fijians, approximately one-third of the population, in 1875,[98] and in the early 19th century devastated the Great Andamanese population.[99] The Ainu population decreased drastically in the 19th century, due in large part to infectious diseases brought by Japanese settlers pouring into Hokkaido.[100]

Researchers concluded that syphilis was carried from the New World to Europe after Columbus's voyages. The findings suggested Europeans could have carried the nonvenereal tropical bacteria home, where the organisms may have mutated into a more deadly form in the different conditions of Europe.[101] The disease was more frequently fatal than it is today. Syphilis was a major killer in Europe during the Renaissance.[102] Between 1602 and 1796, the Dutch East India Company sent almost a million Europeans to work in Asia. Ultimately, fewer than a third made their way back to Europe. The majority died of diseases.[103] Disease killed more British soldiers in India and South Africa than war.[104]
As early as 1803, the Spanish Crown organized a mission (the Balmis expedition) to transport the smallpox vaccine to the Spanish colonies and establish mass vaccination programs there.[105] By 1832, the federal government of the United States established a smallpox vaccination program for Native Americans.[106] From the beginning of the 20th century onwards, the elimination or control of disease in tropical countries became a driving force for all colonial powers.[107] The sleeping sickness epidemic in Africa was arrested due to mobile teams systematically screening millions of people at risk.[108] In the 20th century, the world saw the biggest increase in its population in human history due to a drop in the mortality rate in many countries as a result of medical advances.[109] The world population has grown from 1.6 billion in 1900 to an estimated 6.8 billion in 2011.[110]
Diseases with pandemic potential
In order to encourage research, a number of organisations which monitor global health have drawn up lists of diseases which may have pandemic potential; see table below.[b]
| WHO[111] | CEPI[112] | GAVI[113] | |
|---|---|---|---|
| Chikungunya | Yes | ||
| COVID-19 | Yes | ||
| Crimean-Congo haemorrhagic fever | Yes | Yes | |
| Ebola virus disease | Yes | Yes | Yes |
| Lassa fever | Yes | Yes | Yes |
| Marburg virus disease | Yes | Yes | |
| Mpox | Yes | ||
| Middle East respiratory syndrome coronavirus (MERS-CoV) | Yes | Yes | |
| Nipah and other henipaviral diseases | Yes | Yes | Yes |
| Rift Valley fever | Yes | Yes | Yes |
| Severe Acute Respiratory Syndrome (SARS) | Yes | Yes | Yes |
| Zika | Yes | Yes | |
| Disease X [c] | Yes | Yes |
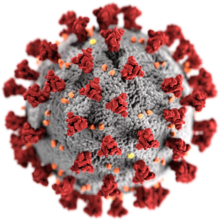
Coronaviruses (CoV) are a large family of viruses that cause illness ranging from the common cold to more severe diseases such as Middle East respiratory syndrome (MERS-CoV) and severe acute respiratory syndrome (SARS-CoV-1).[36] A new strain of coronavirus (SARS-CoV-2) causes Coronavirus disease 2019, or COVID-19,[115] which was declared as a pandemic by the WHO on 11 March 2020.[36]
Some coronaviruses are zoonotic, meaning they are transmitted between animals and people. Detailed investigations found that SARS-CoV-1 was transmitted from civet cats to humans and MERS-CoV from dromedary camels to humans. Several known coronaviruses are circulating in animals that have not yet infected humans. Common signs of infection include respiratory symptoms, fever, cough, shortness of breath, and breathing difficulties. In more severe cases, an infection can cause pneumonia, acute respiratory distress syndrome, kidney failure, and even death. Standard recommendations to prevent the spread of infection include regular hand washing, wearing a face mask, going outdoors when meeting people, and avoiding close contact with people who have tested positive regardless of whether they have symptoms or not. It is recommended that people stay two meters or six feet away from others, commonly called social distancing.
Dengue fever
Dengue is spread by several species of female mosquitoes of the Aedes type, principally A. aegypti. The virus has five types; infection with one type usually gives lifelong immunity to that type, but only short-term immunity to the others. Subsequent infection with a different type increases the risk of severe complications. Several tests are available to confirm the diagnosis including detecting antibodies to the virus or its RNA.
Influenza

The Greek physician Hippocrates, the "Father of Medicine", first described influenza in 412 BC.[116]
- The first influenza pandemic to be pathologically described occurred in 1510. Since the pandemic of 1580, influenza pandemics have occurred every 10 to 30 years.[117][118][119]
- The 1889–1890 pandemic was attributed to influenza at the time but more recent research suggests it may have been caused by human coronavirus OC43. Also known as Russian Flu or Asiatic Flu, it was first reported in May 1889 in Bukhara, Uzbekistan. By October, it had reached Tomsk and the Caucasus. It rapidly spread west and hit North America in December 1889, South America in February–April 1890, India in February–March 1890, and Australia in March–April 1890. The H3N8 and H2N2 subtypes of the influenza A virus have each been identified as possible causes. It had a very high attack and mortality rate, causing around a million fatalities.[120]
- The "Spanish flu", 1918–1920. First identified early in March 1918 in U.S. troops training at Camp Funston, Kansas. By October 1918, it had spread to become a worldwide pandemic on all continents, and eventually infected about one-third of the world's population (or ≈500 million persons).[82] Unusually deadly and virulent, it persisted in pandemic form for at least two years before settling into more endemic patterns.[121] Within six months, some 50 million people were dead;[82] some estimates put the total number of fatalities worldwide at over twice that number.[122] About 17 million died in India, 675,000 in the United States,[123] and 200,000 in the United Kingdom. The virus that caused Spanish flu was also implicated as a cause of encephalitis lethargica in children.[124] The virus was recently reconstructed by scientists at the CDC studying remains preserved by the Alaskan permafrost. The 2009 pandemic H1N1 virus has a small but crucial structure that is similar to the Spanish flu.[125]
- The "Asian flu", 1957–58. An H2N2 virus was first identified in China in late February 1957 but not recognized globally until after an outbreak in Hong Kong in April.[126][127] From there, it spread throughout Southeast Asia and the greater continent during the spring and throughout the Southern Hemisphere during the middle months of the year, causing extensive outbreaks. By the end of September, nearly the entire inhabited world had been infected or at least seeded with the virus. The Northern Hemisphere experienced widespread outbreaks during the fall and winter, and some parts of the world saw a second wave during this time or in early 1958.[126] The pandemic caused about two million deaths globally.[128]
- The "Hong Kong flu", 1968–70. An H3N2 virus was first detected in Hong Kong in July 1968 and spread across the world, lasting until 1970. This pandemic exhibited a more "smoldering" pattern as compared with other influenza pandemics, with uneven impact in different places over time.[129] Its course at first resembled that of the 1957 pandemic, but after a couple of months its spread faltered; the virus did not immediately result in extensive outbreaks in some places, despite repeated introductions.[130] The United States notably experienced an intense epidemic during the 1968–1969 flu season, the first with the pandemic virus, while European and Asian countries were relatively less affected.[130][129] During the 1969–1970 season, however, the United States was much less affected, while Europe and Asia experienced extensive outbreaks of the pandemic virus. In the Southern Hemisphere, Australia experienced a pattern more akin to Europe and Asia, with a more severe second wave.[129] This pandemic killed approximately one million people worldwide.[131]
- The "1977 Russian flu", 1977–79. An H1N1 virus was first reported by the Soviet Union in 1977. The pandemic caused an estimated 700,000 deaths worldwide[132][133] and mostly affected the younger population.[134]
- The "Swine flu", 2009–10. An H1N1 virus first detected in Mexico in early 2009. Estimates for the mortality of this pandemic range from 150 to 500 thousand.[135][136]

Wild aquatic birds are the natural hosts for a range of influenza A viruses. Occasionally, viruses are transmitted from these species to other species, and may then cause outbreaks in domestic poultry or, rarely, in humans.[138][139]
Leprosy
Leprosy, also known as Hansen's disease, is caused by a bacillus, Mycobacterium leprae. It is a chronic disease with an incubation period of up to five years. Since 1985, 15 million people worldwide have been cured of leprosy.[140]
Historically, leprosy has affected people since at least 600 BC.[141] Leprosy outbreaks began to occur in Western Europe around 1000 AD.[142][143] Numerous leprosoria, or leper hospitals, sprang up in the Middle Ages; Matthew Paris estimated that in the early 13th century, there were 19,000 of them across Europe.[144]
Malaria

Malaria is widespread in tropical and subtropical regions, including parts of the Americas, Asia, and Africa. Each year, there are approximately 350–500 million cases of malaria.[145] Drug resistance poses a growing problem in the treatment of malaria in the 21st century, since resistance is now common against all classes of antimalarial drugs, except for the artemisinins.[146]
Malaria was once common in most of Europe and North America, where it is now for all purposes non-existent.[147] Malaria may have contributed to the decline of the Roman Empire.[148] The disease became known as "Roman fever".[149] Plasmodium falciparum became a real threat to colonists and indigenous people alike when it was introduced into the Americas along with the slave trade. Malaria devastated the Jamestown colony and regularly ravaged the South and Midwest of the United States. By 1830, it had reached the Pacific Northwest.[150] During the American Civil War, there were more than 1.2 million cases of malaria among soldiers of both sides.[151] The southern U.S. continued to be affected by millions of cases of malaria into the 1930s.[152]
Measles
Historically, measles was prevalent throughout the world, as it is highly contagious. According to the U.S. National Immunization Program, by 1962 90% of people were infected with measles by age 15.[153] Before the vaccine was introduced in 1963, there were an estimated three to four million cases in the U.S. each year.[154] Measles killed around 200 million people worldwide over the last 150 years.[155] In 2000 alone, measles killed some 777,000 worldwide out of 40 million cases globally.[156]
Measles is an endemic disease, meaning it has been continually present in a community, and many people develop resistance. In populations that have not been exposed to measles, exposure to a new disease can be devastating. In 1529, a measles outbreak in Cuba killed two-thirds of the natives who had previously survived smallpox.[157] The disease had ravaged Mexico, Central America, and the Inca civilization.[158]
Severe acute respiratory syndrome
After the SARS outbreak, in 2003 the Italian physician Carlo Urbani (1956–2003) was the first to identify severe acute respiratory syndrome (SARS) as a new and dangerously contagious disease, although he became infected and died. It is caused by a coronavirus dubbed SARS-CoV-1. Rapid action by national and international health authorities such as the World Health Organization helped to slow transmission and eventually broke the chain of transmission, which ended the localized epidemics before they could become a pandemic. However, the disease has not been eradicated and could re-emerge. This warrants monitoring and reporting of suspicious cases of atypical pneumonia.[159]
Typhus
Typhus is sometimes called "camp fever" because of its pattern of flaring up in times of strife. (It is also known as "gaol fever", "Aryotitus fever" and "ship fever", for its habits of spreading wildly in cramped quarters, such as jails and ships.) Emerging during the Crusades, it had its first impact in Europe in 1489, in Spain. During fighting between the Christian Spaniards and the Muslims in Granada, the Spanish lost 3,000 to war casualties, and 20,000 to typhus. In 1528, the French lost 18,000 troops in Italy, and lost supremacy in Italy to the Spanish. In 1542, 30,000 soldiers died of typhus while fighting the Ottomans in the Balkans.
During the Thirty Years' War (1618–1648), about eight million Germans were killed by bubonic plague and typhus.[160] The disease also played a major role in the destruction of Napoleon's Grande Armée in Russia in 1812. During the retreat from Moscow, more French military personnel died of typhus than were killed by the Russians.[161] Of the 450,000 soldiers who crossed the Neman on 25 June 1812, fewer than 40,000 returned. More military personnel were killed from 1500 to 1914 by typhus than from military action.[162] In early 1813, Napoleon raised a new army of 500,000 to replace his Russian losses. In the campaign of that year, more than 219,000 of Napoleon's soldiers died of typhus.[163] Typhus played a major factor in the Great Famine of Ireland. During World War I, typhus epidemics killed more than 150,000 in Serbia. There were about 25 million infections and 3 million deaths from epidemic typhus in Russia from 1918 to 1922.[163] Typhus also killed numerous prisoners in the Nazi concentration camps and Soviet prisoner of war camps during World War II. More than 3.5 million Soviet POWs died out of the 5.7 million in Nazi custody.[164]
Smallpox
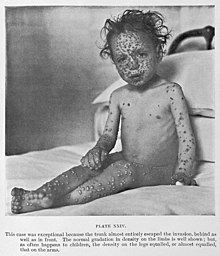
Smallpox was a contagious disease caused by the variola virus. The disease killed an estimated 400,000 Europeans per year during the closing years of the 18th century.[165] During the 20th century, it is estimated that smallpox was responsible for 300–500 million deaths.[166][167] As recently as the early 1950s, an estimated 50 million cases of smallpox occurred in the world each year.[168] After successful vaccination campaigns throughout the 19th and 20th centuries, the WHO certified the eradication of smallpox in December 1979. To this day, smallpox is the only human infectious disease to have been completely eradicated,[169] and one of two infectious viruses ever to be eradicated, along with rinderpest.[170]
Tuberculosis
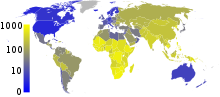
One-quarter of the world's current population has been infected with Mycobacterium tuberculosis, and new infections occur at a rate of one per second.[171] About 5–10% of these latent infections will eventually progress to active disease, which, if left untreated, kills more than half its victims. Annually, eight million people become ill with tuberculosis, and two million die from the disease worldwide.[172] In the 19th century, tuberculosis killed an estimated one-quarter of the adult population of Europe;[173] by 1918, one in six deaths in France were still caused by tuberculosis. During the 20th century, tuberculosis killed approximately 100 million people.[155] TB is still one of the most important health problems in the developing world.[174] In 2021, Tuberculosis became the second leading cause of death from an infectious disease, with roughly 1.6 million deaths worldwide, below COVID-19.[175]
Yellow fever
Yellow fever has been a source of several devastating epidemics.[176] Cities as far north as New York, Philadelphia, and Boston were hit with epidemics. In 1793, one of the largest yellow fever epidemics in U.S. history killed as many as 5,000 people in Philadelphia—roughly 10% of the population. About half of the residents had fled the city, including President George Washington.[177] Another major outbreak of the disease struck the Mississippi River Valley in 1878, with deaths estimated at 20,000. Among the hardest-hit places was Memphis, Tennessee, where 5,000 people were killed and over 20,000 fled, then representing over half the city's population, many of whom never returned. In colonial times, West Africa became known as "the white man's grave" because of malaria and yellow fever.[178]
Zika virus
An outbreak of Zika virus began in 2015 and strongly intensified throughout the start of 2016, with more than 1.5 million cases across more than a dozen countries in the Americas. The World Health Organization warned that Zika had the potential to become an explosive global pandemic if the outbreak was not controlled.[179][180]
Concerns about future pandemics
Prevention of future pandemics requires steps to identify future causes of pandemics and to take preventive measures before the disease moves uncontrollably into the human population.
For example, influenza is a rapidly evolving disease which has caused pandemics in the past and has potential to cause future pandemics. The World Health Organisation collates the findings of 144 national influenza centres worldwide which monitor emerging flu viruses. Virus variants which are assessed as likely to represent a significant risk are identified and can then be incorporated into the next seasonal influenza vaccine program.[181]
In a press conference on 28 December 2020, Mike Ryan, head of the WHO Emergencies Program, and other officials said the current COVID-19 pandemic is "not necessarily the big one" and "the next pandemic may be more severe." They called for preparation.[182] The WHO and the UN, have warned the world must tackle the cause of pandemics and not just the health and economic symptoms.[183]
The October 2020 'era of pandemics' report by the United Nations' Intergovernmental Science-Policy Platform on Biodiversity and Ecosystem Services, written by 22 experts in a variety of fields, said the anthropogenic destruction of biodiversity is paving the way to the pandemic era and could result in as many as 850,000 viruses being transmitted from animals—in particular birds and mammals—to humans. The "exponential rise" in consumption and trade of commodities such as meat, palm oil, and metals, largely facilitated by developed nations, and a growing human population, are the primary drivers of this destruction. According to Peter Daszak, the chair of the group who produced the report, "there is no great mystery about the cause of the Covid-19 pandemic or any modern pandemic. The same human activities that drive climate change and biodiversity loss also drive pandemic risk through their impacts on our environment." Proposed policy options from the report include taxing meat production and consumption, cracking down on the illegal wildlife trade, removing high-risk species from the legal wildlife trade, eliminating subsidies to businesses that are harmful to the natural world, and establishing a global surveillance network.[184][185][186]
In June 2021, a team of scientists assembled by the Harvard Medical School Center for Health and the Global Environment warned that the primary cause of pandemics so far, the anthropogenic destruction of the natural world through such activities including deforestation and hunting, is being ignored by world leaders.[187]
Antibiotic resistance
Antibiotic-resistant microorganisms, which sometimes are referred to as "superbugs", may contribute to the re-emergence of diseases with pandemic potential that are currently well controlled.[188]
For example, cases of tuberculosis that are resistant to traditionally effective treatments remain a cause of great concern to health professionals. Every year, nearly half a million new cases of multidrug-resistant tuberculosis (MDR-TB) are estimated to occur worldwide.[189] China and India have the highest rate of MDR-TB.[190] The World Health Organization (WHO) reports that approximately 50 million people worldwide are infected with MDR-TB, with 79 percent of those cases resistant to three or more antibiotics. Extensively drug-resistant tuberculosis (XDR-TB) was first identified in Africa in 2006 and subsequently discovered to exist in 49 countries. During 2021 there were estimated to be around 25,000 cases XDR-TB worldwide.[191]
In the past 20 years, other common bacteria including Staphylococcus aureus, Serratia marcescens and Enterococcus, have developed resistance to a wide range of antibiotics. Antibiotic-resistant organisms have become an important cause of healthcare-associated (nosocomial) infections.[192]
Climate change
Overpopulation
Encroaching into wildlands
Viral hemorrhagic fevers
Viral hemorrhagic fevers such as Ebola virus disease, Lassa fever, Rift Valley fever, Marburg virus disease, Severe fever with thrombocytopenia as well as Argentine, Bolivian, Brazilian, Crimean-Congo and Venezuelan hemorrhagic fevers[193] are highly contagious and deadly diseases, with the theoretical potential to become pandemics.[194][195] Their ability to spread efficiently enough to cause a pandemic is limited, however, as transmission of these viruses requires close contact with the infected vector, and the vector has only a short time before death or serious illness. Furthermore, the short time between a vector becoming infectious and the onset of symptoms allows medical professionals to quickly quarantine vectors and prevent them from carrying the pathogen elsewhere. Genetic mutations could occur, which could elevate their potential for causing widespread harm; thus, close observation by contagious disease specialists is merited.[citation needed]
Economic consequences
In 2016, the commission on a Global Health Risk Framework for the Future estimated that pandemic disease events would cost the global economy over $6 trillion in the 21st century—over $60 billion per year.[196] The same report recommended spending $4.5 billion annually on global prevention and response capabilities to reduce the threat posed by pandemic events, a figure that the World Bank Group raised to $13 billion in a 2019 report.[197] It has been suggested that such costs be paid from a tax on aviation rather than from, e.g., income taxes,[198] given the crucial role of air traffic in transforming local epidemics into pandemics (being the only factor considered in state-of-the-art models of long-range disease transmission [199]).
The COVID-19 pandemic is expected to have a profound negative effect on the global economy, potentially for years to come, with substantial drops in GDP accompanied by increases in unemployment noted around the world.[36] The slowdown of economic activity early in the COVID-19 pandemic had a profound effect on emissions of pollutants and greenhouse gases.[200][201][202] The reduction of air pollution, and economic activity associated with it during a pandemic was first documented by Alexander F. More for the Black Death plague pandemic, showing the lowest pollution levels in the last 2000 years occurring during that pandemic, due to its 40 to 60% death rate throughout Eurasia.[203][204][205][206][207]
See also
- Asian Flu of 1957
- Biological hazard
- Compartmental models in epidemiology
- Contagious disease
- Crowdmapping
- Disease X
- European Centre for Disease Prevention and Control (ECDC)
- Hong Kong Flu of 1968
- Immunization
- Index case
- Mortality from infectious diseases
- List of pandemics and epidemics
- Mathematical modelling of infectious disease
- Medieval demography
- Pandemic fatigue
- Pandemic severity index
- Public health emergency of international concern
- Super-spreader
- Syndemic
- Tropical disease
- Timeline of global health
- Twindemic
- Vaccination
- WHO pandemic phases
Notes
- ^ For clarification, WHO does not use the old system of six phases—ranging from phase 1 (no reports of animal influenza causing human infections) to phase 6 (a pandemic)—that some people may be familiar with from H1N1 in 2009.
- ^ As of June 2023, the WHO is reviewing its list
- ^ Disease X represents the knowledge that a serious international epidemic could be caused by a pathogen currently unknown to cause human disease.
References
- ^ a b Serbu J (27 March 2020). "Army Corps sees convention centers as good option to build temporary hospitals". Federal News Network. Archived from the original on 14 April 2020.
- ^ "Black death 'discriminated' between victims (ABC News in Science)". Australian Broadcasting Corporation. 29 January 2008. Archived from the original on 20 December 2016. Retrieved 3 November 2008.
- ^ "Black Death's Gene Code Cracked". Wired. 3 October 2001. Archived from the original on 26 April 2015. Retrieved 12 February 2015.
- ^ "Health: De-coding the Black Death". BBC. 3 October 2001. Archived from the original on 7 July 2017. Retrieved 3 November 2008.
- ^ DeLeo FR, Hinnebusch BJ (September 2005). "A plague upon the phagocytes". Nature Medicine. 11 (9): 927–928. doi:10.1038/nm0905-927. PMID 16145573. S2CID 31060258.
- ^ 1918 Pandemics (H1N1 virus). Centers for Disease Control and Prevention. Retrieved 18 April 2020.
- ^ Rosenwald MS (7 April 2020). "History's deadliest pandemics, from ancient Rome to modern America". The Washington Post. Archived from the original on 7 April 2020. Retrieved 11 April 2020.
- ^ "Weekly Virological Update on 05 August 2010". World Health Organization (WHO). 5 August 2010. Archived from the original on 7 August 2015. Retrieved 8 April 2020.
- ^ Wingfield T, Cuevas LE, MacPherson P, Millington KA, Squire SB (June 2020). "Tackling two pandemics: a plea on World Tuberculosis Day". The Lancet. Respiratory Medicine. 8 (6): 536–538. doi:10.1016/S2213-2600(20)30151-X. PMC 7118542. PMID 32220280.
- ^ Roychoudhury S, Das A, Sengupta P, Dutta S, Roychoudhury S, Choudhury AP, et al. (December 2020). "Viral Pandemics of the Last Four Decades: Pathophysiology, Health Impacts and Perspectives". International Journal of Environmental Research and Public Health. 17 (24): 9411. doi:10.3390/ijerph17249411. PMC 7765415. PMID 33333995.
- ^ "Why the HIV epidemic is not over". www.who.int. Retrieved 22 September 2022.
- ^ Eisinger RW, Fauci AS (March 2018). "Ending the HIV/AIDS Pandemic1". Emerging Infectious Diseases. 24 (3): 413–416. doi:10.3201/eid2403.171797. PMC 5823353. PMID 29460740.
- ^ "World Health Assembly agrees to launch process to develop historic global accord on pandemic prevention, preparedness and response". World Health Organization. 1 December 2021. Retrieved 2 December 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ Cumming-Bruce N (1 December 2021). "W.H.O. members agree to begin talks on a global pandemic treaty". The New York Times. ISSN 0362-4331. Retrieved 2 December 2021.
- ^ Porta M, ed. (2008). Dictionary of Epidemiology. Oxford University Press. p. 179. ISBN 978-0-19-531449-6. Retrieved 14 September 2012.
- ^ Dumar AM (2009). Swine Flu: What You Need to Know. Wildside Press LLC. p. 7. ISBN 978-1434458322.
- ^ Morens D, Folkers G, Fauci A (1 October 2009). "What Is a Pandemic?". Oxford University Press. The Journal of Infectious Diseases. Retrieved 7 June 2023.
- ^ Doshi P (July 2011). "The elusive definition of pandemic influenza". Bulletin of the World Health Organization. 89 (7): 532–538. doi:10.2471/BLT.11.086173. PMC 3127275. PMID 21734768.
- ^ "Emergencies: International health regulations and emergency committees". World Health Organisation. 19 December 2019. Retrieved 7 June 2023.
- ^ Ross E (20 October 2022). "What is the difference between a pandemic and a PHEIC? (Video)". Chatham House, The Royal Institute of International Affairs. Retrieved 7 June 2023.
- ^ "Zero draft of the WHO convention, agreement or other international instrument on pandemic prevention, preparedness and response ("WHO CA+")" (PDF). World Health Organization - Intergovernmental Negotiating Body. 1 February 2023. Retrieved 7 June 2023.
- ^ "WHO says it no longer uses 'pandemic' category, but virus still emergency". Reuters. 24 February 2020. Archived from the original on 18 March 2020.
- ^ "Table 3: WHO Pandemic Phase Descriptions and Main Actions by Phase". ncbi.nlm.nih.gov. National Center for Biotechnology Information, National Library of Medicine, National Institutes of Health. Archived from the original on 21 April 2020. Retrieved 23 April 2020.Table/Figure 3 is from Chapter 4 of (2009). (WHO chart in April 2020).
- ^ "WHO press conference on 2009 pandemic influenza" (PDF). World Health Organization. 26 May 2009. Retrieved 26 August 2010.
- ^ "Pandemic influenza preparedness and response" (PDF). World Health Organization. Archived from the original (PDF) on 13 May 2011.
- ^ "WHO pandemic phase descriptions and main actions by phase" (PDF). Archived from the original (PDF) on 10 September 2011.
- ^ "A whole industry is waiting for an epidemic". Der Spiegel. 21 July 2009. Retrieved 26 August 2010.
- ^ a b Holloway R, Rasmussen SA, Zaza S, Cox NJ, Jernigan DB (September 2014). "Updated preparedness and response framework for influenza pandemics" (PDF). MMWR. Recommendations and Reports. 63 (RR-06). Center for Surveillance, Epidemiology, and Laboratory Services, Centers for Disease Control and Prevention: 1–18. PMID 25254666. Retrieved 10 May 2020.
- ^ a b c d Reed C, Biggerstaff M, Finelli L, Koonin LM, Beauvais D, Uzicanin A, et al. (January 2013). "Novel framework for assessing epidemiologic effects of influenza epidemics and pandemics". Emerging Infectious Diseases. 19 (1): 85–91. doi:10.3201/eid1901.120124. PMC 3557974. PMID 23260039.
- ^ Qualls N, Levitt A, Kanade N, Wright-Jegede N, Dopson S, Biggerstaff M, et al. (April 2017). "Community Mitigation Guidelines to Prevent Pandemic Influenza - United States, 2017". MMWR. Recommendations and Reports. 66 (1). Center for Surveillance, Epidemiology, and Laboratory Services, Centers for Disease Control and Prevention: 1–34. doi:10.15585/mmwr.rr6601a1. PMC 5837128. PMID 28426646.
- ^ Interim Pre-Pandemic Planning Guidance: Community Strategy for Pandemic Influenza Mitigation in the United States (PDF). Centers for Disease Control and Prevention. February 2007. p. 9.
- ^ Rajgor DD, Lee MH, Archuleta S, Bagdasarian N, Quek SC (July 2020). "The many estimates of the COVID-19 case fatality rate". The Lancet. Infectious Diseases. 20 (7). Elsevier Ltd.: 776–777. doi:10.1016/S1473-3099(20)30244-9. PMC 7270047. PMID 32224313.
- ^ a b c Anderson RM, Heesterbeek H, Klinkenberg D, Hollingsworth TD (March 2020). "How will country-based mitigation measures influence the course of the COVID-19 epidemic?". Lancet. 395 (10228): 931–934. doi:10.1016/S0140-6736(20)30567-5. PMC 7158572. PMID 32164834.
A key issue for epidemiologists is helping policymakers decide the main objectives of mitigation—e.g., minimizing morbidity and associated mortality, avoiding an epidemic peak that overwhelms health-care services, keeping the effects on the economy within manageable levels, and flattening the epidemic curve to wait for vaccine development and manufacture on the scale and antiviral drug therapies.
- ^ a b "Community Mitigation Guidelines to Prevent Pandemic Influenza—United States, 2017". Recommendations and Reports. 66 (1). Centers for Disease Control and Prevention. 12 April 2017.
- ^ Barclay E, Scott D, Animashaun A (7 April 2020). "The US doesn't just need to flatten the curve. It needs to "raise the line."". Vox. Archived from the original on 7 April 2020.
- ^ a b c d e f g h i j Stawicki SP, Jeanmonod R, Miller AC, Paladino L, Gaieski DF, Yaffee AQ, et al. (2020). "The 2019-2020 Novel Coronavirus (Severe Acute Respiratory Syndrome Coronavirus 2) Pandemic: A Joint American College of Academic International Medicine-World Academic Council of Emergency Medicine Multidisciplinary COVID-19 Working Group Consensus Paper". Journal of Global Infectious Diseases. 12 (2): 47–93. doi:10.4103/jgid.jgid_86_20. PMC 7384689. PMID 32773996. S2CID 218754925.
- ^ Anderson RM, Heesterbeek H, Klinkenberg D, Hollingsworth TD (March 2020). "How will country-based mitigation measures influence the course of the COVID-19 epidemic?". Lancet. 395 (10228): 931–934. doi:10.1016/S0140-6736(20)30567-5. PMC 7158572. PMID 32164834.
- ^ Maier BF, Brockmann D (May 2020). "Effective containment explains subexponential growth in recent confirmed COVID-19 cases in China". Science. 368 (6492): 742–746. arXiv:2002.07572. Bibcode:2020Sci...368..742M. doi:10.1126/science.abb4557. PMC 7164388. PMID 32269067. ("...initial exponential growth expected for an unconstrained outbreak.")
- ^ "Gauze Mask to Halt Spread of Plague". The Washington Times. 27 September 1918. p. 3.
- ^ "3. Strategies for Disease Containment". Ethical and Legal Considerations in Mitigating Pandemic Disease: Workshop Summary. National Academies Press (US). 2007.
- ^ Baird RP (11 March 2020). "What It Means to Contain and Mitigate the Coronavirus". The New Yorker.
- ^ "Impact of non-pharmaceutical interventions (NPIs) to reduce COVID19 mortality and healthcare demand" (PDF). Imperial College COVID-19 Response Team. 16 March 2020.
- ^ "Multi-country monkeypox outbreak in non-endemic countries". World Health Organization. 21 May 2022. Archived from the original on 22 May 2022. Retrieved 25 May 2022.
- ^ "Monkeypox – United Kingdom of Great Britain and Northern Ireland". World Health Organization. 16 May 2022. Archived from the original on 17 May 2022. Retrieved 17 May 2022.
- ^ "WHO Director-General declares the ongoing monkeypox outbreak a Public Health Emergency of International Concern". World Health Organization (WHO). 23 July 2022. Retrieved 4 August 2022.
- ^ Kimball, Spencer (11 May 2023). "WHO says mpox outbreak, the largest in history, no longer global health emergency". CNBC. Retrieved 11 May 2023.
- ^ "Multi-country monkeypox outbreak: situation update". World Health Organization. 27 June 2022. Retrieved 5 August 2022.
- ^ "Protecting you from mpox (monkeypox): information on the smallpox vaccination". GOV.UK. Archived from the original on 28 May 2023. Retrieved 28 May 2023.
- ^ "Mpox (Monkeypox) awareness campaign: Communications toolkit for stakeholders". Western Australia Department of Health. 10 June 2022. Archived from the original on 28 May 2023. Retrieved 28 May 2023.
- ^ "Multi-country outbreak of mpox - External Situation Report 21" (PDF). World Health Organization. 27 April 2023. Retrieved 21 June 2023.
- ^ "Total confirmed cases of COVID-19 per million people". Our World in Data. Archived from the original on 19 March 2020. Retrieved 10 April 2020.
- ^ "WHO Statement Regarding Cluster of Pneumonia Cases in Wuhan, China". WHO. 31 December 2019. Retrieved 12 March 2020.
- ^ "Covid-19 Coronavirus Pandemic (Live statistics)". Worldometer. 2020. Retrieved 3 April 2020.
- ^ "Coronavirus COVID-19 Global Cases by Johns Hopkins CSSE". gisanddata.maps.arcgis.com. Retrieved 8 March 2020.
- ^ "WHO Director-General's opening remarks at the media briefing on COVID-19—11 March 2020". WHO. 11 March 2020. Retrieved 12 March 2020.
- ^ "WHO - Statement on the fifteenth meeting of the IHR (2005) Emergency Committee on the COVID-19 pandemic". World Health Organisation. Retrieved 10 May 2023.
- ^ "WHO Coronavirus (COVID-19) Dashboard". World Health Organization. 19 June 2023. Retrieved 19 June 2023.
- ^ a b Antia R, Halloran ME (October 2021). "Transition to endemicity: Understanding COVID-19". Immunity (Review). 54 (10): 2172–2176. doi:10.1016/j.immuni.2021.09.019. PMC 8461290. PMID 34626549.
- ^ Markov PV, Ghafari M, Beer M, Lythgoe K, Simmonds P, Stilianakis NI, Katzourakis A (June 2023). "The evolution of SARS-CoV-2". Nat Rev Microbiol (Review). 21 (6): 361–379. doi:10.1038/s41579-023-00878-2. PMID 37020110. S2CID 257983412.
In the absence of eradication, the virus will likely become endemic, a process that could take years to decades. We will be able to establish that endemic persistence has been reached if the virus shows repeatable patterns in prevalence year on year, for example, regular seasonal fluctuations and no out-of-season peaks. The form this endemic persistence will take remains to be determined, and the eventual infection prevalence and disease burden will depend on the rate of emergence of antigenically distinct lineages, our ability to roll out and update vaccines, and the future trajectory of virulence (Fig. 4c)....Meanwhile, focusing on the epidemiology of the pathogen, it is important to bear in mind that the transition from a pandemic to future endemic existence of SARS-CoV-2 is likely to be long and erratic, rather than a short and distinct switch, and that endemic SARS-CoV-2 is by far not a synonym for safe infections, mild COVID-19 or a low population mortality and morbidity burden.
- ^ Steere-Williams J (May 2022). "Endemic fatalism and why it will not resolve COVID-19". Public Health. 206: 29–30. doi:10.1016/j.puhe.2022.02.011. ISSN 0033-3506. PMC 8841151. PMID 35316742.
- ^ "WHO HIV/AIDS Data and Statistics". Retrieved 12 April 2020.
- ^ Cohen MS, Hellmann N, Levy JA, DeCock K, Lange J (April 2008). "The spread, treatment, and prevention of HIV-1: evolution of a global pandemic". The Journal of Clinical Investigation. 118 (4): 1244–1254. doi:10.1172/JCI34706. PMC 2276790. PMID 18382737.
- ^ Chong JR (30 October 2007). "Analysis clarifies route of AIDS". Los Angeles Times. Retrieved 6 July 2014.
- ^ "The South African Department of Health Study". Avert.org. 2006. Retrieved 26 August 2010.
- ^ "Global HIV & AIDS statistics — 2021 fact sheet". www.unaids.org. UNAIDS. Retrieved 1 July 2021.
- ^ Hauck G (22 November 2020). "We're celebrating Thanksgiving amid a pandemic. Here's how we did it in 1918 – and what happened next". USA Today. Graphics by Karl Gelles. Archived from the original on 21 November 2020.
- ^ "Ancient Athenian Plague Proves to Be Typhoid". Scientific American. 25 January 2006.
- ^ Past pandemics that ravaged Europe. BBC News, 7 November. 2005
- ^ "Modern lab reaches across the ages to resolve plague DNA debate". phys.org. 20 May 2013.
- ^ "Cambridge Catalogue page 'Plague and the End of Antiquity'". Cambridge.org. Retrieved 26 August 2010.
- ^ Quotes from book "Plague and the End of Antiquity" Archived 16 July 2011 at the Wayback Machine Lester K. Little, ed., Plague and the End of Antiquity: The Pandemic of 541–750, Cambridge, 2006. ISBN 0-521-84639-0
- ^ Death on a Grand Scale. MedHunters.
- ^ Stéphane Barry and Norbert Gualde, in L'Histoire No. 310, June 2006, pp. 45–46, say "between one-third and two-thirds"; Robert Gottfried (1983). "Black Death" in Dictionary of the Middle Ages, volume 2, pp. 257–267, says "between 25 and 45 percent".
- ^ Chisholm, Hugh, ed. (1911). . Encyclopædia Britannica. Vol. 21 (11th ed.). Cambridge University Press. pp. 693–705.
- ^ "A List of National Epidemics of Plague in England 1348–1665". Urbanrim.org.uk. 4 August 2010. Archived from the original on 8 May 2009. Retrieved 26 August 2010.
- ^ Revill J (16 May 2004). "Black Death blamed on man, not rats". The Observer. London. Retrieved 3 November 2008.
- ^ The Great Plague of London, 1665. The Harvard University Library, Open Collections Program: Contagion.
- ^ G. William Beardslee. "The 1832 Cholera Epidemic in New York State". Earlyamerica.com. Retrieved 26 August 2010.
- ^ "Zoonotic Infections: Plague". World Health Organization. Archived from the original on 20 April 2009. Retrieved 5 July 2014.
- ^ Bubonic plague hits San Francisco 1900–1909. A Science Odyssey. Public Broadcasting Service (PBS).
- ^ "Human Plague—United States, 1993–1994". cdc.gov.
- ^ a b c d Taubenberger JK, Morens DM (January 2006). "1918 Influenza: the mother of all pandemics". Emerging Infectious Diseases. 12 (1): 15–22. doi:10.3201/eid1201.050979. PMC 3291398. PMID 16494711. Archived from the original on 6 October 2009. Retrieved 7 September 2017.
- ^ "Historical Estimates of World Population". Archived from the original on 9 July 2012. Retrieved 29 March 2013.
- ^ Gagnon A, Miller MS, Hallman SA, Bourbeau R, Herring DA, Earn DJ, Madrenas J (2013). "Age-specific mortality during the 1918 influenza pandemic: unravelling the mystery of high young adult mortality". PLOS ONE. 8 (8): e69586. Bibcode:2013PLoSO...869586G. doi:10.1371/journal.pone.0069586. PMC 3734171. PMID 23940526.
- ^ "The 1918 Influenza Pandemic". virus.stanford.edu.
- ^ Spanish flu facts by Channel 4 News.
- ^ Qureshi AI (2016). Ebola Virus Disease: From Origin to Outbreak. Academic Press. p. 42. ISBN 978-0128042427.
- ^ Spanish flu strikes during World War I, 14 January 2010
- ^ "Smallpox: Eradicating the Scourge". Bbc.co.uk. 5 November 2009. Retrieved 26 August 2010.
- ^ Smallpox The Fight to Eradicate a Global Scourge Archived 7 September 2008 at the Wayback Machine, David A. Koplow
- ^ Greg Lange,"Smallpox epidemic ravages Native Americans on the northwest coast of North America in the 1770s", 23 January 2003, HistoryLink.org, Online Encyclopedia of Washington State History, accessed 2 June 2008
- ^ Houston CS, Houston S (March 2000). "The first smallpox epidemic on the Canadian Plains: In the fur-traders' words". The Canadian Journal of Infectious Diseases. 11 (2): 112–115. doi:10.1155/2000/782978. PMC 2094753. PMID 18159275.
- ^ "The Story Of ... Smallpox—and other Deadly Eurasian Germs". Pbs.org. Retrieved 26 August 2010.
- ^ "Stacy Goodling, "Effects of European Diseases on the Inhabitants of the New World"". Archived from the original on 10 May 2008.
- ^ Smallpox Through History Archived 29 October 2009 at the Wayback Machine
- ^ "New Zealand Historical Perspective". Canr.msu.edu. 31 March 1998. Archived from the original on 12 June 2010. Retrieved 26 August 2010.
- ^ How did Easter Island's ancient statues lead to the destruction of an entire ecosystem?, The Independent
- ^ Fiji School of Medicine Archived 20 October 2014 at the Wayback Machine
- ^ Measles hits rare Andaman tribe. BBC News. 16 May 2006.
- ^ Meeting the First Inhabitants, TIMEasia.com, 21 August 2000
- ^ Genetic Study Bolsters Columbus Link to Syphilis, New York Times, 15 January 2008
- ^ Columbus May Have Brought Syphilis to Europe, LiveScience
- ^ Nomination VOC archives for Memory of the World Register (English)
- ^ "Sahib: The British Soldier in India, 1750–1914 by Richard Holmes". Asianreviewofbooks.com. 27 October 2005. Archived from the original on 26 March 2009. Retrieved 26 August 2010.
- ^ "Dr. Francisco de Balmis and his Mission of Mercy, Society of Philippine Health History". Archived from the original on 19 October 2013.
- ^ "Lewis Cass and the Politics of Disease: The Indian Vaccination Act of 1832". Muse.jhu.edu. Archived from the original on 5 February 2008. Retrieved 26 August 2010.
- ^ Conquest and Disease or Colonialism and Health? Archived 7 December 2008 at the Wayback Machine, Gresham College | Lectures and Events
- ^ WHO Media centre (2001). "Fact sheet No. 259: African trypanosomiasis or sleeping sickness".
- ^ Iliffe J (1989). "The Origins of African Population Growth". The Journal of African History. 30 (1): 165–169. doi:10.1017/S0021853700030942. JSTOR 182701. S2CID 59931797.
- ^ "World Population Clock—U.S. Census Bureau". U.S. Census Bureau. Archived from the original on 18 November 2011. Retrieved 18 November 2011.
- ^ "Prioritizing diseases for research and development in emergency contexts (Published 2018, revision in progress 2023)". World Health Organization. Retrieved 23 June 2023.
- ^ "Targeting diseases with epidemic and pandemic potential". CEPI, Coalition for Epidemic Preparedness Innovations. 23 June 2023. Retrieved 23 June 2023.
- ^ "10 infectious diseases that could be the next pandemic | Gavi, the Vaccine Alliance". Gavi, the Vaccine Alliance. 7 May 2020. Retrieved 23 June 2023.
- ^ Sonnevend J (December 2020). Alexander JC, Jacobs RN, Smith P (eds.). "A virus as an icon: the 2020 pandemic in images". American Journal of Cultural Sociology. 8 (3). Palgrave Macmillan: 451–461. doi:10.1057/s41290-020-00118-7. eISSN 2049-7121. PMC 7537773. PMID 33042541.
- ^ McArdle M. "When a danger is growing exponentially, everything looks fine until it doesn't". Washington Post. Retrieved 15 March 2020.
- ^ "50 Years of Influenza Surveillance". World Health Organization. Archived from the original on 1 May 2009.
- ^ "Pandemic Flu". Department of Health and Social Security. Archived from the original on 7 January 2012.
- ^ Beveridge WI (1977). Influenza: The Last Great Plague: An Unfinished Story of Discovery. New York: Prodist. ISBN 0-88202-118-4.
Return of the Germs: For more than a century drugs and vaccines made astounding progress against infectious diseases. Now our best defenses may be social changes
{{cite book}}: CS1 maint: location missing publisher (link) - ^ Potter CW (October 2001). "A history of influenza". Journal of Applied Microbiology. 91 (4): 572–579. doi:10.1046/j.1365-2672.2001.01492.x. PMID 11576290. S2CID 26392163.
- ^ "Pandemic Influenza". CIDRAP. 16 June 2011.
- ^ Chandra S, Christensen J, Likhtman S (November 2020). "Connectivity and seasonality: the 1918 influenza and COVID-19 pandemics in global perspective". Journal of Global History. 15 (3): 413–414. doi:10.1017/S1740022820000261. S2CID 228988279.
- ^ "Spanish flu". ScienceDaily. Archived from the original on 25 March 2015.
- ^ "The Great Pandemic: The United States in 1918–1919". U.S. Department of Health & Human Services. Archived from the original on 26 November 2011.
- ^ Vilensky JA, Foley P, Gilman S (August 2007). "Children and encephalitis lethargica: a historical review". Pediatric Neurology. 37 (2): 79–84. doi:10.1016/j.pediatrneurol.2007.04.012. PMID 17675021.
- ^ Harmon K. "H1N1 shares key similar structures to 1918 flu, providing research avenues for better vaccines". Scientific American Blog Network.
- ^ a b "Symposium on the Asian Influenza Epidemic, 1957". Proceedings of the Royal Society of Medicine. 51 (12): 1009–1018. 1 December 1958. doi:10.1177/003591575805101205. ISSN 0035-9157.
- ^ Murray R (1969). "Production and testing in the USA of influenza virus vaccine made from the Hong Kong variant in 1968-69". Bulletin of the World Health Organization. 41 (3): 495–496. hdl:10665/262478. PMC 2427701. PMID 5309463.
- ^ "Q&A: Swine flu". BBC News. 27 April 2009.
- ^ a b c Viboud C, Grais RF, Lafont BA, Miller MA, Simonsen L (July 2005). "Multinational impact of the 1968 Hong Kong influenza pandemic: evidence for a smoldering pandemic". The Journal of Infectious Diseases. 192 (2): 233–248. doi:10.1086/431150. PMID 15962218.
- ^ a b Cockburn WC, Delon PJ, Ferreira W (1969). "Origin and progress of the 1968-69 Hong Kong influenza epidemic". Bulletin of the World Health Organization. 41 (3): 345–348. PMC 2427756. PMID 5309437.
- ^ Dumar AM (2009). Swine Flu: What You Need to Know. Wildside Press LLC. p. 20. ISBN 978-1434458322.
- ^ Michaelis M, Doerr HW, Cinatl J (August 2009). "Novel swine-origin influenza A virus in humans: another pandemic knocking at the door". Medical Microbiology and Immunology. 198 (3): 175–183. doi:10.1007/s00430-009-0118-5. PMID 19543913. S2CID 20496301.
- ^ Petrovski BÉ, Lumi X, Znaor L, Ivastinović D, Confalonieri F, Petrovič MG, Petrovski G (July 2020). "Reorganize and survive-a recommendation for healthcare services affected by COVID-19-the ophthalmology experience". Eye. 34 (7): 1177–1179. doi:10.1038/s41433-020-0871-7. PMC 7169374. PMID 32313170.
- ^ Rozo M, Gronvall GK (August 2015). "The Reemergent 1977 H1N1 Strain and the Gain-of-Function Debate". mBio. 6 (4). doi:10.1128/mBio.01013-15. PMC 4542197. PMID 26286690.
- ^ Trifonov V, Khiabanian H, Rabadan R (July 2009). "Geographic dependence, surveillance, and origins of the 2009 influenza A (H1N1) virus". The New England Journal of Medicine. 361 (2): 115–119. doi:10.1056/NEJMp0904572. PMID 19474418. S2CID 205105276.
- ^ "2009 H1N1 Pandemic". Centers for Disease Control and Prevention. 11 June 2019.
- ^ "Swine flu has killed up to 17,000 in U.S.: report". Reuters. 12 February 2010.
- ^ Klenk; et al. (2008). "Avian Influenza: Molecular Mechanisms of Pathogenesis and Host Range". Animal Viruses: Molecular Biology. Caister Academic Press. ISBN 978-1-904455-22-6.
- ^ Kawaoka Y, ed. (2006). Influenza Virology: Current Topics. Caister Academic Press. ISBN 978-1-904455-06-6.
- ^ Leprosy 'could pose new threat'. BBC News. 3 April 2007.
- ^ "Leprosy". WHO. Retrieved 22 August 2007.
- ^ Miller TS, Smith-Savage R (2006). "Medieval Leprosy Reconsidered". International Social Science Review. 81 (1/2): 16–28. JSTOR 41887256.
- ^ Boldsen JL (February 2005). "Leprosy and mortality in the Medieval Danish village of Tirup". American Journal of Physical Anthropology. 126 (2): 159–168. doi:10.1002/ajpa.20085. PMID 15386293.
- ^ Herbermann, Charles, ed. (1913). . Catholic Encyclopedia. New York: Robert Appleton Company.
- ^ "Malaria Facts". Archived from the original on 29 December 2012. Retrieved 7 September 2017.
- ^ White NJ (April 2004). "Antimalarial drug resistance". The Journal of Clinical Investigation. 113 (8): 1084–1092. doi:10.1172/JCI21682. PMC 385418. PMID 15085184.
- ^ Vector- and Rodent-Borne Diseases in Europe and North America. Norman G. Gratz. World Health Organization, Geneva.
- ^ DNA clues to malaria in ancient Rome. BBC News. 20 February 2001.
- ^ "Malaria and Rome" Archived 11 May 2011 at the Wayback Machine. Robert Sallares. ABC.net.au. 29 January 2003.
- ^ "The Changing World of Pacific Northwest Indians". Center for the Study of the Pacific Northwest, University of Washington.
- ^ "A Brief History of Malaria". Infoplease.com. Retrieved 26 August 2010.
- ^ Malaria. By Michael Finkel. National Geographic Magazine.
- ^ Orenstein WA, Papania MJ, Wharton ME (May 2004). "Measles elimination in the United States". The Journal of Infectious Diseases. 189 (Supplement_1): S1–S3. doi:10.1086/377693. PMID 15106120.
- ^ Center for Disease Control & National Immunization Program. Measles History, article online 2001. Available from https://www.cdc.gov/measles/about/history.html
- ^ a b Torrey, EF; Yolken, RH (3 April 2005). "Their bugs are worse than their bite". Birdflubook.com. p. B01. Archived from the original on 26 June 2013. Retrieved 26 August 2010.
- ^ Stein CE, Birmingham M, Kurian M, Duclos P, Strebel P (May 2003). "The global burden of measles in the year 2000--a model that uses country-specific indicators". The Journal of Infectious Diseases. 187 (Suppl 1): S8-14. doi:10.1086/368114. PMID 12721886.
- ^ Man and Microbes: Disease and Plagues in History and Modern Times; by Arno Karlen
- ^ "Measles and Small Pox as an Allied Army of the Conquistadors of America" Archived 2 May 2009 at the Wayback Machine by Carlos Ruvalcaba, translated by Theresa M. Betz in "Encounters" (Double Issue No. 5–6, pp. 44–45)
- ^ "WHO | SARS outbreak contained worldwide". WHO. Archived from the original on 25 August 2004. be safe be active
- ^ War and Pestilence. Time. 29 April 1940
- ^ The Historical Impact of Epidemic Typhus Archived 11 June 2010 at the Wayback Machine. Joseph M. Conlon.
- ^ War and Pestilence. Time.
- ^ a b Conlon JM. "The historical impact of epidemic typhus" (PDF). Archived from the original (PDF) on 11 June 2010. Retrieved 21 April 2009.
- ^ Soviet Prisoners of War: Forgotten Nazi Victims of World War II By Jonathan Nor, TheHistoryNet
- ^ Smallpox and Vaccinia Archived 1 June 2009 at the Wayback Machine. National Center for Biotechnology Information.
- ^ "UC Davis Magazine, Summer 2006: Epidemics on the Horizon". Archived from the original on 11 December 2008. Retrieved 3 January 2008.
- ^ How Poxviruses Such As Smallpox Evade The Immune System, ScienceDaily, 1 February 2008
- ^ "Smallpox" Archived 21 September 2007 at the Wayback Machine. WHO Factsheet. Retrieved on 22 September 2007.
- ^ De Cock KM (2001). "(Book Review) The Eradication of Smallpox: Edward Jenner and The First and Only Eradication of a Human Infectious Disease". Nature Medicine. 7 (1): 15–16. doi:10.1038/83283.
- ^ "Rinderpest: OIE—World Organisation for Animal Health". oie.int.
- ^ World Health Organization (WHO). Tuberculosis Fact sheet No. 104—Global and regional incidence. March 2006, Retrieved on 6 October 2006.
- ^ Centers for Disease Control. Fact Sheet: Tuberculosis in the United States. Archived 23 April 2009 at the Wayback Machine 17 March 2005, Retrieved on 6 October 2006.
- ^ "Multidrug-Resistant Tuberculosis". Archived from the original on 9 March 2010. Retrieved 7 September 2017.
- ^ Rook GA, Dheda K, Zumla A (August 2005). "Immune responses to tuberculosis in developing countries: implications for new vaccines". Nature Reviews. Immunology. 5 (8): 661–667. doi:10.1038/nri1666. PMID 16056257. S2CID 9004625.
- ^ "Tuberculosis". WHO. 24 March 2020. Retrieved 31 May 2020.
- ^ Chisholm, Hugh, ed. (1911). . Encyclopædia Britannica. Vol. 28 (11th ed.). Cambridge University Press. pp. 910–911..
- ^ Arnebeck B (30 January 2008). "A Short History of Yellow Fever in the US". Benjamin Rush, Yellow Fever and the Birth of Modern Medicine. Archived from the original on 7 November 2007. Retrieved 4 December 2008.
- ^ Africa's Nations Start to Be Their Brothers' Keepers. The New York Times, 15 October 1995.
- ^ "Zika virus could become 'explosive pandemic'". bbc.co.uk. 28 January 2016.
- ^ Sikka V, Chattu VK, Popli RK, Galwankar SC, Kelkar D, Sawicki SG, et al. (2016). "The Emergence of Zika Virus as a Global Health Security Threat: A Review and a Consensus Statement of the INDUSEM Joint working Group (JWG)". Journal of Global Infectious Diseases. 8 (1): 3–15. doi:10.4103/0974-777X.176140. PMC 4785754. PMID 27013839.
- ^ "Selecting Viruses for the Seasonal Flu Vaccine". Centers for Disease Control and Prevention. 3 November 2022. Retrieved 30 June 2023.
- ^ "WHO official: 'Next pandemic may be more severe'". Arab News. 29 December 2020. Retrieved 30 December 2020.
- ^ Carrington D (9 March 2021). "Inaction leaves world playing 'Russian roulette' with pandemics, say experts". The Guardian. Retrieved 10 March 2021.
- ^ Woolaston K, Fisher JL (29 October 2020). "UN report says up to 850,000 animal viruses could be caught by humans, unless we protect nature". The Conversation. Retrieved 1 December 2020.
- ^ Carrington D (29 October 2020). "Protecting nature is vital to escape 'era of pandemics' – report". The Guardian. Retrieved 1 December 2020.
- ^ "Escaping the 'Era of Pandemics': experts warn worse crises to come; offer options to reduce risk". EurekAlert!. 29 October 2020. Retrieved 1 December 2020.
- ^ Carrington D (4 June 2021). "World leaders 'ignoring' role of the destruction of nature in causing pandemics". The Guardian. Retrieved 4 June 2021.
- ^ Researchers sound the alarm: the multidrug resistance of the plague bacillus could spread Archived 14 October 2007 at the Wayback Machine. Pasteur.fr
- ^ Health ministers to accelerate efforts against drug-resistant TB. World Health Organization.
- ^ Bill Gates joins Chinese government in tackling TB 'timebomb'. Guardian.co.uk. 1 April 2009
- ^ "Global Tuberculosis Report". World Health Organisation. Retrieved 30 June 2023.
- ^ Murray CJ, Ikuta KS, Sharara F, Swetschinski L, Aguilar GR, Gray A, et al. (Antimicrobial Resistance Collaborators) (February 2022). "Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis". Lancet. 399 (10325): 629–655. doi:10.1016/S0140-6736(21)02724-0. PMC 8841637. PMID 35065702. S2CID 246077406.
- ^ Park ES, Shimojima M, Nagata N, Ami Y, Yoshikawa T, Iwata-Yoshikawa N, et al. (August 2019). "Severe Fever with Thrombocytopenia Syndrome Phlebovirus causes lethal viral hemorrhagic fever in cats". Scientific Reports. 9 (1): 11990. Bibcode:2019NatSR...911990P. doi:10.1038/s41598-019-48317-8. PMC 6700174. PMID 31427690.
- ^ "Fears of Ebola pandemic if violent attacks continue in DR Congo". Al-Jazeera. 23 May 2019.
- ^ Wojda TR, Valenza PL, Cornejo K, McGinley T, Galwankar SC, Kelkar D, et al. (2015). "The Ebola Outbreak of 2014-2015: From Coordinated Multilateral Action to Effective Disease Containment, Vaccine Development, and Beyond". Journal of Global Infectious Diseases. 7 (4): 127–138. doi:10.4103/0974-777X.170495. PMC 4693303. PMID 26752867.
- ^ "Global Health Risk Framework—The Neglected Dimension of Global Security: A Framework to Counter Infectious Disease Crises" (PDF). National Academy of Medicine. 16 January 2016. Retrieved 2 August 2016.
- ^ World Bank Group (September 2019). Pandemic Preparedness Financing. Status Update (PDF). Washington: World Bank Group. Archived from the original (PDF) on 1 March 2020.
- ^ Pueyo S (12 May 2020). "Jevons' paradox and a tax on aviation to prevent the next pandemic". SocArXiv. doi:10.31235/osf.io/vb5q3. S2CID 219809283.
- ^ Wang L, Wu JT (January 2018). "Characterizing the dynamics underlying global spread of epidemics". Nature Communications. 9 (1): 218. Bibcode:2018NatCo...9..218W. doi:10.1038/s41467-017-02344-z. PMC 5768765. PMID 29335536.
- ^ Le Quéré C, Jackson RB, Jones MW, Smith AJ, Abernethy S, Andrew RM, et al. (2020). "Temporary reduction in daily global CO2 emissions during the COVID-19 forced confinement". Nature Climate Change. 10 (7): 647–653. Bibcode:2020NatCC..10..647L. doi:10.1038/s41558-020-0797-x.
- ^ "Pollution made COVID-19 worse. Now, lockdowns are clearing the air". National Geographic Magazine. 8 April 2020. Retrieved 22 June 2020.
- ^ Bauwens M, Compernolle S, Stavrakou T, Müller JF, van Gent J, Eskes H, et al. (June 2020). "Impact of Coronavirus Outbreak on NO2 Pollution Assessed Using TROPOMI and OMI Observations". Geophysical Research Letters. 47 (11): e2020GL087978. Bibcode:2020GeoRL..4787978B. doi:10.1029/2020GL087978. PMC 7261997. PMID 32836515.
- ^ "Probing the Black Death for lead pollution insights". Harvard University Gazette. 30 May 2017. Retrieved 22 June 2020.
- ^ More AF, Spaulding NE, Bohleber P, Handley MJ, Hoffmann H, Korotkikh EV, et al. (June 2017). "Next-generation ice core technology reveals true minimum natural levels of lead (Pb) in the atmosphere: Insights from the Black Death". GeoHealth. 1 (4): 211–219. doi:10.1002/2017GH000064. PMC 7007106. PMID 32158988.
- ^ "The Black Death helped reveal how long humans have polluted the planet". Popular Science Magazine. 25 September 2017. Retrieved 22 June 2020.
- ^ "Humans Polluted the Air Much Earlier Than Previously Thought". Smithsonian Magazine. 2 June 2017. Retrieved 22 June 2020.
- ^ "'We have been poisoning ourselves': has ice analysis revealed the truth about lead?". The Guardian. 30 May 2017. Retrieved 22 June 2020.
Further reading
- American Lung Association (April 2007). "Multidrug Resistant Tuberculosis Fact Sheet". Archived from the original on 30 November 2006. Retrieved 29 November 2007.
- Bancroft EA (October 2007). "Antimicrobial resistance: it's not just for hospitals". JAMA. 298 (15): 1803–1804. doi:10.1001/jama.298.15.1803. PMC 2536104. PMID 17940239.
- Brilliant L, Smolinski M, Danzig L, Lipkin WI (January–February 2023). "Inevitable Outbreaks: How to Stop an Age of Spillovers from Becoming an Age of Pandemics". Foreign Affairs. 102 (1): 126–130, 132–140.
- Brook T (November 2020). "Comparative pandemics: the Tudor–Stuart and Wanli–Chongzhen years of pestilence, 1567–1666". Journal of Global History. 15 (3): 363–379. doi:10.1017/S174002282000025X. S2CID 228979855.
- Eisenberg M, Mordechai L (December 2020). "The Justinianic plague and global pandemics: The making of the plague concept". The American Historical Review. 125 (5): 1632–1667. doi:10.1093/ahr/rhaa510.
- Honigsbaum M (18 October 2020). "How do pandemics end? In different ways, but it's never quick and never neat". The Guardian. ISSN 0261-3077. Retrieved 28 October 2020.
- Larson E (2007). "Community factors in the development of antibiotic resistance". Annual Review of Public Health. 28: 435–447. doi:10.1146/annurev.publhealth.28.021406.144020. PMID 17094768.
- Lietaert Peerbolte BJ (September 2021). "The Book of Revelation: Plagues as Part of the Eschatological Human Condition". Journal for the Study of the New Testament. 44 (1). SAGE Publications: 75–92. doi:10.1177/0142064X211025496. ISSN 1745-5294. S2CID 237332665.
- McKenna N (September 2020). "Return of the Germs: For more than a century drugs and vaccines made astounding progress against infectious diseases. Now our best defenses may be social changes". Scientific American. 323 (3): 50–56.
What might prevent or lessen [the] possibility [of a virus emerging and finding a favorable human host] is more prosperity more equally distributed – enough that villagers in South Asia need not trap and sell bats to supplement their incomes and that, low-wage workers in the U.S. need not go to work while ill because they have no sick leave
- Quammen D (24 August 202). "Did Pangolin Trafficking Cause the Coronavirus Pandemic". The New Yorker. pp. 26–31 (31).
More field research is needed [...]. More sampling of wild animals. More scrutiny of genomes. More cognizance of the fact that animal infections can become human infections because humans are animals. We live in a world of viruses, and we have scarcely begun to understand this one. [ COVID-19
- "Escaping the 'Era of Pandemics': Experts Warn Worse Crises to Come Options Offered to Reduce Risk". Intergovernmental Science-Policy Platform on Biodiversity and Ecosystem Services. 2020.









