User:I enjoy sandwiches/h
Hormone replacement therapy (HRT), also known as menopausal hormone therapy (MHT) or postmenopausal hormone therapy (PHT, PMHT), is a form of hormone therapy used to treat symptoms associated with female menopause.[1][2] These symptoms can include hot flashes, vaginal atrophy, accelerated skin aging, vaginal dryness, decreased muscle mass, sexual dysfunction, and bone loss. They are in large part related to the diminished levels of sex hormones that occur during this time.[1][2]
The main hormonal medications used in HRT for menopausal symptoms are estrogens and progestogens.[3] Though both can have symptomatic benefits, progestogen is specifically added to estrogen regimens when the uterus is still present. Unopposed estrogen therapy promotes endometrial thickening and can lead to cancer, while progestogen reduces this risk.[3][4][5] Androgens like testosterone are sometimes used as well.[6] HRT is available through a variety of different routes.[3]
The long-term effects of HRT on most organ systems vary by age and time since last physiologic exposure to hormones, and there can be large differences in individual regimens, factors which have made analyzing effect difficult.[7] There have been several large trials on hormone replacement in women, with the Women's Health Initiative (WHI) of the National Institutes of Health being the largest prospective study to date, and in particular having a significant impact since its inception. The WHI was a massive study of over 27,000 women conducted beginning in 1991 and taking place over 15 years, with multiple subsequent publications since that time analyzing its data.
The results of the WHI have been complex, and suggest both potential risks and benefits across different organ systems. Long term follow up of the WHI participants, however, has found no difference in all-cause, cardiovascular, or cancer mortality with HRT.[7] Later studies have suggested that risk can differ depending on route of administration.[8] Bioidentical hormone replacement is a more recent development, and while some early data suggests an improved risk profile, there have been no large prospective studies to date.[9]
The current indications for use from the United States Food and Drug Administration (FDA) include short-term treatment of menopausal symptoms, such as vasomotor hot flashes or vaginal atrophy, and prevention of osteoporosis.[10]
Indications[edit]
Women receiving this treatment are usually post-, peri-, or surgically menopausal. Menopause is the permanent cessation of menstruation resulting from loss of ovarian follicular activity, defined as beginning twelve months after the final natural menstrual cycle. This twelve month time point divides menopause into early and late transition periods known as 'perimenopause' and 'postmenopause'.[5] Premature menopause can occur if the ovaries are surgically removed, as can be done to treat ovarian or uterine cancer.
Potential menopausal symptoms include:[1][2]
- Hot flashes - vasomotor symptoms
- Vulvovaginal atrophy - atrophic vaginitis and dryness
- Dyspareunia - painful sexual intercourse due to vaginal atrophy and lack of lubrication
- Bone loss - decreased bone mineral density, which can eventually lead to osteopenia, osteoporosis, and associated fractures
- Decreased sexual desire
- Defeminization - diminished feminine fat distribution and accelerated skin aging[11][12]
- Sleep disturbances and joint pain
The most common of these are are loss of sexual drive and vaginal dryness.[5][13]
HRT may impact diseases like breast cancer, colorectal cancer, endometrial cancer, cardiovascular disease and dementia, though there is much debate in the medical community as to magnitude of effect and whether positive or negative.
HRT is often given as a short-term relief from menopausal symptoms during perimenopause.[14]
Long term health effects[edit]
The effects of HRT on most organ systems vary by age and time since last physiologic exposure to hormones, and there can be large differences in individual regimens, factors which have made analyzing effect difficult.[7] Demographically, the vast majority of data available is in postmenopausal American women with concurrent pre-existing conditions, and with a mean age of over 60 years.[15]
The Women's Health Initiative (WHI) of the National Institutes of Health (NIH) is a massive study of over 27,000 women beginning in 1991 and has been the largest prospective analysis of HRT effects in menopause to date. Successive analyses have found sometimes contradictory results, with the most recent publication in 2017 finding no difference for all cause mortality with HRT.[7]
Potential benefits[edit]
Bone density[edit]

There is a large and significant reduction in hip fracture rates with HRT in menopause. This protective effect persists after the cessation of therapy, though to a lesser degree.[16][17] Estrogen prevents the activity of osteoclasts, and improves bone mineral density. It also helps collagen formation, which in turn improves texture of the intervertebral discs and bone matrix.[18]
Cardiovascular disease[edit]

The risks of coronary heart disease with HRT vary by age and years since onset of menopause. Women aged 50 to 59 using HRT have a lower risk of coronary heart disease,[19] as do women who are within five years of the onset of menopause.[20] There may be an increase in heart disease in older patients taking HRT, though this is only statistically significant in individuals twenty years post menopause.[16] There is no actual difference in long-term mortality from HRT, regardless of age.[7]
A Cochrane review suggested that women starting HRT less than 10 years after menopause had lower mortality and coronary heart disease, without any strong effect on the risk of stroke. Those starting therapy more than 10 years after menopause had little effect on mortality and coronary heart disease, but an increased risk of stroke. Taking the increased risk of venous thromboembolism into account, the reviewers came to the conclusion that HRT had little benefit in cardiovascular disease.[21]
HRT also improves cholesterol levels. With menopause, HDL decreases, while LDL, triglycerides and lipoprotein a increase, patterns that reverse with estrogen. Beyond this, HRT improves heart contraction, coronary blood flow, sugar metabolism, and decreases platelet aggregation and plaque formation. HRT may promote reverse cholesterol transport through induction of cholesterol ABC transporters.[22]
Endometrial cancer[edit]

In postmenopausal women, continuous combined estrogen plus progestin decreases endometrial cancer incidence.[23] The duration of progestogen therapy should be at least 14 days per cycle to prevent endometrial disease.[24]
Endometrial cancer has been grouped into two forms in the context of hormone replacement. Type 1 is the most common, can be associated with estrogen therapy, and is usually low grade. Type 2 is not related to estrogen stimulation and usually higher grade and poorer prognosis.[25] The endometrial hyperplasia that leads to endometrial cancer with estrogen therapy can be prevented by concomitant administration of progestogen.[25] The extensive use of high-dose estrogens for birth control in the 1970s is thought to have resulted in a significant increase in the incidence of type 1 endometrial cancer.[26]
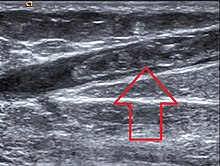
Paradoxically, progestogens do promote the growth of uterine fibroids, and a pelvic ultrasound can be performed before beginning HRT to make sure there are no underlying uterine or endometrial lesions.[25]
Muscle mass[edit]
Hormone replacement therapy in the form of estrogen and androgen can be effective at reversing the effects of aging on muscle.[27]
Neurodegenerative disorders[edit]
HRT may increase risk of dementia if initiated after 65 years of age, but have a neutral outcome or be neuroprotective for those between 50-55 years.[16] HRT can also improve executive and attention processes outside of the context of dementia in postmenopausal women.[28]
Sexual function[edit]
It is commonly misunderstood that as women complete their reproductive years, sexual activity stops altogether. Epidemiological surveys suggest that this is not true for most, with a recent study amongst women aged 40–69 revealing that 75% of women remain sexually active.[5] With increasing life spans, women today are living one third or more of their lives in a postmenopausal state, a period during which healthy sexuality can be integral to their quality of life.[29]
A major complaint among postmenopausal women is decreased libido and sexual function, and many may seek medical consultation.[6][30] Several hormonal changes take place during this period, including a decrease in estrogen and an increase in follicle-stimulating hormone. For most women, the majority of change occurs during the late perimenopausal and postmenopausal stages.[5] Decrease in sex hormone-binding globulin (SHBG) and inhibin (A and B) also occurs. Testosterone, a hormone more commonly associated with males, is also present in women at a lower level. It peaks at age 30, but declines gradually with age, so there is little variation across the lifetime and during the menopausal transition.[5] With surgical menopause, testosterone declines more sharply and can result in more severe symptoms.[5] HRT can help with sexual difficulties related to pain and lubrication.[6]

Not all women are responsive, especially those with preexisting sexual difficulties.[13] Estrogen replacement can restore vaginal cells, pH levels, and blood flow to the vagina, all of which tend to deteriorate at the onset of menopause. Pain or discomfort with sex appears to be the most responsive component to estrogen.[13] It also has been shown to have positive effects on the urinary tract.[13] Reduced vaginal atrophy and increased sexual arousal, frequency and orgasm have also been noted.[13]
The effectiveness of hormone replacement can decline in some women after long-term use.[13] A number of studies have also found that the combined effects of estrogen/androgen replacement therapy can increase libido and arousal over estrogen alone.[13] Findings on a relatively new form of HRT called tibolone, a synthetic steroid with estrogenic, androgenic, and progestogenic properties, suggest that it has the ability to improve mood, libido, and physical symptoms of surgically menopausal women to a greater degree than ERT. In various placebo-controlled studies, improvements in vasomotor symptoms, emotional response, sleep disturbances, physical symptoms, and sexual desire have been observed.[6] Tibolone has been used in Europe for almost two decades but is not available North America at this point.[6]
Skin[edit]
Estrogen replacement promotes collagen formation, which in turn improves texture and appearance of the skin and fingernails.[18] There is no association of HRT, either positive of negative, with skin cancer.[31]
Potential risks[edit]
Breast cancer[edit]
There is a non-statistically significant increased incidence of breast cancer for hormone replacement therapy with synthetic progesterone.[7] The risk may be reduced with bioidentical progesterone, though research is still very early, with no prospective studies or randomized controlled trials to date.[32] The relative risk of breast cancer also varies depending on the interval between menopause and HRT and route of administration.[33]

The WHI also found a non-significant trend in the estrogen-alone clinical trial towards a reduced risk of breast cancer, though estrogen is usually only given alone in the setting of a hysterectomy due to the effect of unopposed estrogen on the uterus.[19][34]
HRT has been more strongly associated with risk of breast cancer in women with a lower range body mass indices (BMIs). No breast cancer association has been found with BMIs of over 25.[35] It has been suggested by some that the absence of significant effect in some of these studies could be due to selective prescription to overweight women who have higher baseline estrone, or to the very low progesterone serum levels after oral administration leading to a high tumor inactivation rate.[36]
For women who previously have had breast cancer, it is recommended to first consider other options for menopausal effects, such as bisphosphonates or selective estrogen receptor modulators (SERMs) for osteoporosis, cholesterol-lowering agents and aspirin for cardiovascular disease, and vaginal estrogen for local symptoms. Observational studies of systemic HRT after breast cancer are generally reassuring. If HRT is necessary after breast cancer, estrogen-only therapy or estrogen therapy with a progestogen may be safer options than combined systemic therapy.[37]
Colorectal cancer[edit]
In the WHI study, results were mixed. Women who took combined estrogen-progesterone therapy had a lower risk of getting colorectal cancer, but the cancers they did have were more likely to have spread to lymph nodes or distant sites than colorectal cancer in women not taking hormones.[31]
Ovarian cancer[edit]
A 2015 meta-analysis found that HRT was associated with an increased risk of ovarian cancer, with women using HRT having about one additional case of ovarian cancer per 1,000 users.[38] This risk is decreased when progestogen therapy is given concomitantly, as opposed to estrogen alone, and also decreases with increasing time since stopping HRT.[39] Regarding the specific subtype, there may be a higher risk of serous cancer, but no association with clear cell, endometrioid, or mucinous ovarian cancer.[39]
Pulmonary embolism and venous clotting[edit]
Comparisons between routes of administration suggest that when estrogens are taken orally the risk of a venous clot forming and traveling to the lungs is increased, an effect which is not seen with estrogen applied to the skin or vagina.[40] Transdermal and transvaginal administration are not subject to first pass metabolism, and so lack the anabolic effects that oral therapy has on liver synthesis of Vitamin K dependent clotting factors.[41] Taking progesterone at the same time can decrease this risk.[40]
Stroke[edit]
Multiple studies suggest that the possibility of HRT related stroke is absent if therapy is started within five years of menopause,[42] and that the association is absent or even preventative when given by non-oral routes.[8] Ischemic stroke risk was increased during the time of intervention in the WHI, with no significant effect after the cessation of therapy[16] and no difference in mortality at long term follow up.[7] When oral synthetic estrogen or combined estrogen-progestogen treatment is delayed until 5 years from menopause, cohort studies in Swedish women have suggested an association with hemorrhagic and ischemic stroke.[42] Another large cohort of Danish women suggested that the specific route of administration was important, finding that although oral estrogen increased risk of stroke, transdermal application had no impact, and vaginal estrogen actually had a decreased risk.[8]
Available forms[edit]
There are five major human steroid hormones: estrogens, progestogens, androgens, mineralocorticoids, and glucocorticoids. Estrogens and progestogens are the two most often used in menopause. They are available in a wide variety of FDA approved and non–FDA-approved formulations.[9]
In women with intact uteruses, estrogens are almost always given in combination with progestogens, as long-term unopposed estrogen therapy is associated with a markedly increased risk of endometrial hyperplasia and endometrial cancer.[3] Conversely, in women who have undergone a hysterectomy or do not have a uterus, a progestogen is not required, and estrogen can be used alone. There are many combined formulations which include both estrogen and progestogen.
Specific types of hormone replacement include:[3]
- Estrogens – bioidentical estrogens like estradiol and estriol, animal-derived estrogens like conjugated estrogens (CEEs), and synthetic estrogens like ethinylestradiol
- Progestogens – bioidentical progesterone, and progestins (synthetic progestogens) like medroxyprogesterone acetate (MPA), norethisterone, and dydrogesterone
- Androgens – bioidentical testosterone and dehydroepiandrosterone (DHEA), and synthetic anabolic steroids like methyltestosterone and nandrolone decanoate[43][44]
Tibolone is a synthetic derivative of Mexican yam whose metabolites have estrogenic, progestogenic, and androgenic effects.[3]
Vaginal estrogen can improve local atrophy and dryness, with fewer systemic effects than estrogens delivered by other routes.[45] Sometimes an androgen, generally testosterone, is added to treat diminished libido. It may also treat reduced energy and help reduce osteoporosis after menopause.
Continuous versus cyclic[edit]
Dosage is often varied cyclically to more closely mimic the ovarian hormone cycle, with estrogens taken daily and progestogens taken for about two weeks every month or every other month, a schedule referred to as 'cyclic' or 'sequentially combined'. Alternatively, 'continuous combined' HRT can be given with a constant daily hormonal dosage.
| Route/form | Estrogen | Low | Standard | High | |||
|---|---|---|---|---|---|---|---|
| Oral | Estradiol | 0.5–1 mg/day | 1–2 mg/day | 2–4 mg/day | |||
| Estradiol valerate | 0.5–1 mg/day | 1–2 mg/day | 2–4 mg/day | ||||
| Estradiol acetate | 0.45–0.9 mg/day | 0.9–1.8 mg/day | 1.8–3.6 mg/day | ||||
| Conjugated estrogens | 0.3–0.45 mg/day | 0.625 mg/day | 0.9–1.25 mg/day | ||||
| Esterified estrogens | 0.3–0.45 mg/day | 0.625 mg/day | 0.9–1.25 mg/day | ||||
| Estropipate | 0.75 mg/day | 1.5 mg/day | 3 mg/day | ||||
| Estriol | 1–2 mg/day | 2–4 mg/day | 4–8 mg/day | ||||
| Ethinylestradiola | 2.5–10 μg/day | 5–20 μg/day | – | ||||
| Nasal spray | Estradiol | 150 μg/day | 300 μg/day | 600 μg/day | |||
| Transdermal patch | Estradiol | 25 μg/dayb | 50 μg/dayb | 100 μg/dayb | |||
| Transdermal gel | Estradiol | 0.5 mg/day | 1–1.5 mg/day | 2–3 mg/day | |||
| Vaginal | Estradiol | 25 μg/day | – | – | |||
| Estriol | 30 μg/day | 0.5 mg 2x/week | 0.5 mg/day | ||||
| IM or SC injection | Estradiol valerate | – | – | 4 mg 1x/4 weeks | |||
| Estradiol cypionate | 1 mg 1x/3–4 weeks | 3 mg 1x/3–4 weeks | 5 mg 1x/3–4 weeks | ||||
| Estradiol benzoate | 0.5 mg 1x/week | 1 mg 1x/week | 1.5 mg 1x/week | ||||
| SC implant | Estradiol | 25 mg 1x/6 months | 50 mg 1x/6 months | 100 mg 1x/6 months | |||
| Footnotes: a = No longer used or recommended, due to health concerns. b = As a single patch applied once or twice per week (worn for 3–4 days or 7 days), depending on the formulation. Note: Dosages are not necessarily equivalent. Sources: See template. | |||||||
Route of administration[edit]

The medications used in menopausal HRT are available in numerous different formulations for use by a variety of different routes of administration:[3]
- Oral administration – tablets, capsules
- Transdermal administration – patches, gels, creams
- Vaginal administration – tablets, creams, suppositories, rings
- Intramuscular or subcutaneous injection – solutions in vials or ampoules
- Subcutaneous implant – surgically-inserted pellets placed into fat tissue
- Less commonly sublingual, buccal, intranasal, and rectal administration, as well as intrauterine devices
More recently developed forms of drug delivery are alleged to have increased local effect lower dosing, fewer side effects, and constant rather than cyclical serum hormone levels.[46] Transdermal and transvaginal estrogen, in particular, avoid first pass metabolism through the liver. This in turn prevents an increase in clotting factors and accumulation of anti-estrogenic metabolites, resulting in fewer adverse side effects, particularly with regard to cardiovascular disease and stroke.[47]
Bioidentical hormone therapy[edit]
Bioidentical hormone therapy (BHT) is the usage of hormones that are chemically identical to those produced in the body. Although proponents of BHT claim advantages over non-bioidentical or conventional hormone therapy, the FDA does not recognize the term 'bioidentical hormone', stating there is no scientific evidence that these hormones are identical to their naturally occurring counterparts.[48][49] There are, however, FDA approved products containing hormones classified as 'bioidentical'.[9]
Bioidentical hormones can be used in either pharmaceutical or compounded preparations, with the latter generally not recommended by regulatory bodies due to their lack of standardization and regulatory oversight.[48] Most classifications of bioidentical hormones do not take into account manufacturing, source, or delivery method of the products, and so describe both non-FDA approved compounded products and FDA approved pharmaceuticals as 'bioidentical'.[9]
Bioidentical hormones in pharmaceuticals may have health benefits over their animal derived counterparts, including a potentially decreased risk of venous thromboembolism, cardiovascular disease, and breast cancer.[48] As of 2012, guidelines from the North American Menopause Society, the Endocrine Society, the International Menopause Society, and the European Menopause and Andropause Society endorsed the reduced risk of bioidentical pharmaceuticals for those with increased clotting risk.[48][50]
Compounding[edit]
Compounding for HRT is generally discouraged by the FDA and medical industry in the United States due to a lack of regulation and standardized dosing.[48][49]c The U. S. Congress did grant the FDA explicit but limited oversight of compounded drugs in a 1997 amendment to the Federal Food, Drug, and Cosmetic Act (FDCA), but they have encountered obstacles in this role since that time. After 64 patient deaths and 750 harmed patients from a 2012 meningitis outbreak due to contaminated steroid injections, Congress passed the 2013 Drug Quality and Security Act, authorizing creation by the FDA of a voluntary registration for facilities that manufactured compounded drugs, and reinforcing FDCA regulations for traditional compounding.[51]
In the United Kingdom, on the other hand, compounding is a regulated activity. The Medicines and Healthcare products Regulatory Agency regulates compounding performed under a Manufacturing Specials license and the General Pharmaceutical Council regulates compounding performed within a pharmacy. All testosterone prescribed in the United Kingdom is bioidentical, with its use supported by the National Health Service. There is also marketing authorisation for male testosterone products. National Institute for Health and Care Excellence guideline 1.4.8 states: "consider testosterone supplementation for menopausal women with low sexual desire if HRT alone is not effective". The footnote adds: "at the time of publication (November 2015), testosterone did not have a United Kingdom marketing authorisation for this indication in women. Bio-identical progesterone is used in IVF treatment and for pregnant women who are at risk of premature labour."
Side effects[edit]
Some common and uncommon side effects include:[52]
Common[edit]
- Headache
- Upset stomach, stomach cramps or bloating
- Diarrhea
- Appetite and weight changes
- Changes in sex drive or performance
- Nervousness
- Brown or black patches on the skin
- Acne
- Swelling of hands, feet, or lower legs due to fluid retention
- Changes in menstrual flow
- Breast tenderness, enlargement, or discharge
- Sudden difficulty wearing contact lenses
Uncommon[edit]
- Double vision
- Severe abdominal pain
- Yellowing of skin or eyes
- Severe depression
- Unusual bleeding
- Loss of appetite
- Skin rash
- Lassitude
- Fever
- Dark-colored urine
- Light colored stool
- Chorea[53]
Contraindications[edit]
The following are absolute and relative contraindications to HRT:[54]
Absolute contraindications[edit]
- Undiagnosed vaginal bleeding
- Severe liver disease
- Pregnancy
- Severe coronary artery disease
- Aggressive breast, uterine or ovarian cancer
Relative contraindications[edit]
- Migraine headaches
- History of breast cancer
- History of ovarian cancer
- Venous thrombosis
- History of uterine fibroids
- Atypical ductal hyperplasia of the breast
- Active gallbladder disease (cholangitis, cholecystitis)
- Well-differentiated and early endometrial cancer - once treatment for the malignancy is complete, is no longer an absolute contraindication.
Medical and regulatory body statements[edit]
Current indications for HRT from the FDA include short-term treatment of menopausal symptoms such as hot flashes and vaginal atrophy, and prevention of osteoporosis.[10]
The American College of Obstetrics and Gynecology (ACOG) approves of HRT for symptomatic relief of menopausal symptoms,[55] and advocates its usage beyond the age of 65 in appropriate clinical scenarios.[56]
The North American Menopause Society (NAMS) 2016 annual meeting mentioned that HRT may have more benefits than risks in women before the age of 60.[57] A consensus expert opinion published by The Endocrine Society stated that when taken during perimenopause or the initial years of menopause, HRT carries significantly fewer risks than previously published, and reduces all cause mortality in most patient scenarios.[58]
The American Association of Clinical Endocrinologists (AACE) has also released multiple position statements approving of HRT in appropriate clinical scenarios.[59]
History and research[edit]
The extraction of CEEs from the urine of pregnant mares led to the marketing in 1942 of Premarin, one of the earlier forms of estrogen to be introduced.[60][61] From that time until the mid-1970s, estrogen was administered without a supplemental progestogen. Beginning in 1975, studies began to show that without a progestogen, unopposed estrogen therapy with Premarin resulted in an 8-fold increased risk of endometrial cancer, eventually causing sales of Premarin to plummet.[60] It was recognized in the early 1980s that the addition of a progestogen to estrogen reduced this risk to the endometrium.[60] This led to the development of combined estrogen–progestogen therapy, most commonly with a combination of conjugated equine estrogen (Premarin) and medroxyprogesterone (Provera).[60]
Women's Health Initiative and other trials[edit]
The WHI results were both positive and negative, suggesting that during the time of hormone therapy itself, there are increases in invasive breast cancer, stroke and lung clots. Other risks include increased endometrial cancer, gallbladder disease, and urinary incontinence, while benefits include decreased hip fractures, decreased incidence of diabetes, and improvement of vasomotor symptoms. There also is an increased risk of dementia with HRT in women over 65, though when given earlier it appears to be neuroprotective. After the cessation of HRT, the WHI continued observe its participants, and found that most of these risks and benefits dissipated, though some elevation in breast cancer risk did persist.[16] Other studies have also suggested an increased risk of ovarian cancer.[39]
The actual trials were intended to be conducted between 1991 and 2006.[60] However, the arm of the WHI receiving combined estrogen and progestin therapy was closed prematurely in 2002 by its Data Monitoring Committee (DMC) due to perceived health risks, although the trial arm was stopped only a full year after the data suggesting increased risk became manifest. In 2004, the arm of the WHI in which post-hysterectomy patients were being treated with estrogen alone was also closed by the DMC. Clinical medical practice changed based upon two parallel Women's Health Initiative (WHI) studies of HRT. Prior studies were smaller, and many were of women who electively took hormonal therapy. The WHI studies were the first large, double-blind, placebo-controlled clinical trials of HRT in healthy women. One portion of the parallel studies followed over 16,000 women for an average of 5.2 years, half of whom took placebo, while the other half took a combination of CEEs and MPA (Prempro). This WHI estrogen-plus-progestin trial was stopped prematurely in 2002 because preliminary results suggested risks of combined CEEs and progestins exceeded their benefits. The first report on the halted WHI estrogen-plus-progestin study came out in July 2002.[62]
Initial data from the WHI in 2002 suggested mortality to be lower when HRT was begun earlier, between age 50 to 59, but higher when begun after age 60. In older patients, there was an apparent increased incidence of breast cancer, heart attacks, venous thrombosis, and stroke, although a reduced incidence of colorectal cancer and bone fracture. At the time, The WHI recommended that women with non-surgical menopause take the lowest feasible dose of HRT for the shortest possible time to minimize associated risks.[62] Some of the WHI findings were again found in a larger national study done in the United Kingdom, known as the Million Women Study (MWS). As a result of these findings, the number of women taking HRT dropped precipitously.[63] In 2012, the United States Preventive Task Force (USPSTF) concluded that the harmful effects of combined estrogen and progestin therapy likely exceeded their chronic disease prevention benefits.[64][65]
In 2002 when the first WHI follow up study was published, with HRT in post menopausal women, both older and younger age groups had a slightly higher incidence of breast cancer, and both heart attack and stroke were increased in older patients, although not in younger participants. Breast cancer was increased in women treated with estrogen and a progestin, but not with estrogen and progesterone or estrogen alone. Treatment with unopposed estrogen (i.e., an estrogen alone without a progestogen) is contraindicated if the uterus is still present, due to its proliferative effect on the endometrium. The WHI also found a reduced incidence of colorectal cancer when estrogen and a progestogen were used together, and most importantly, a reduced incidence of bone fractures. Ultimately, the study found disparate results for all cause mortality with HRT, finding it to be lower when HRT was begun during ages 50–59, but higher when begun after age 60. The authors of the study recommended that women with non-surgical menopause take the lowest feasible dose of hormones for the shortest time to minimize risk.[62]
The data published by the WHI suggested supplemental estrogen increased risk of venous thromboembolism and breast cancer but was protective against osteoporosis and colorectal cancer, while the impact on cardiovascular disease was mixed.[66] These results were later supported in trials from the United Kingdom, but not in more recent studies from France and China. Genetic polymorphism appears to be associated with inter-individual variability in metabolic response to HRT in postmenopausal women.[67][68]
Neither the WHI nor the MWS differentiated the results for different types of progestogens used. MPA – the type most commonly used in the United States – was the only one examined by the WHI, which in its analysis and conclusions extrapolated the benefits versus risks of MPA to all progestins. This conclusion has since been challenged by several researchers as unjustified and misleading, resulting in unreasonable, unnecessary avoidance by many women of HRT. In addition, subsequent findings released by the WHI showed that all cause mortality was not dramatically different between the groups receiving CEEs, those receiving estrogen and a progestogen, and those not on therapy.[69] In addition, the WHI trial was limited by low adherence, high attrition, inadequate power to detect risks for some outcomes, and evaluation of few regimens.[65] The double blinding limited validity of study results due to its effects on patient exclusion criteria. Patients who were experiencing symptoms of the menopausal transition were excluded from the study, meaning that younger women who had only recently experienced menopause were not significantly represented. As a result, while the average age of menopause is age 51, study participants were on average 62 years of age. Demographically, the vast majority were Caucasian, and tended to be slightly overweight and former smokers.
| Clinical outcome | Hypothesized effect on risk |
Estrogen and progestogen (CEs 0.625 mg/day p.o. + MPA 2.5 mg/day p.o.) (n = 16,608, with uterus, 5.2–5.6 years follow up) |
Estrogen alone (CEs 0.625 mg/day p.o.) (n = 10,739, no uterus, 6.8–7.1 years follow up) | ||||
|---|---|---|---|---|---|---|---|
| HR | 95% CI | AR | HR | 95% CI | AR | ||
| Coronary heart disease | Decreased | 1.24 | 1.00–1.54 | +6 / 10,000 PYs | 0.95 | 0.79–1.15 | −3 / 10,000 PYs |
| Stroke | Decreased | 1.31 | 1.02–1.68 | +8 / 10,000 PYs | 1.37 | 1.09–1.73 | +12 / 10,000 PYs |
| Pulmonary embolism | Increased | 2.13 | 1.45–3.11 | +10 / 10,000 PYs | 1.37 | 0.90–2.07 | +4 / 10,000 PYs |
| Venous thromboembolism | Increased | 2.06 | 1.57–2.70 | +18 / 10,000 PYs | 1.32 | 0.99–1.75 | +8 / 10,000 PYs |
| Breast cancer | Increased | 1.24 | 1.02–1.50 | +8 / 10,000 PYs | 0.80 | 0.62–1.04 | −6 / 10,000 PYs |
| Colorectal cancer | Decreased | 0.56 | 0.38–0.81 | −7 / 10,000 PYs | 1.08 | 0.75–1.55 | +1 / 10,000 PYs |
| Endometrial cancer | – | 0.81 | 0.48–1.36 | −1 / 10,000 PYs | – | – | – |
| Hip fractures | Decreased | 0.67 | 0.47–0.96 | −5 / 10,000 PYs | 0.65 | 0.45–0.94 | −7 / 10,000 PYs |
| Total fractures | Decreased | 0.76 | 0.69–0.83 | −47 / 10,000 PYs | 0.71 | 0.64–0.80 | −53 / 10,000 PYs |
| Total mortality | Decreased | 0.98 | 0.82–1.18 | −1 / 10,000 PYs | 1.04 | 0.91–1.12 | +3 / 10,000 PYs |
| Global index | – | 1.15 | 1.03–1.28 | +19 / 10,000 PYs | 1.01 | 1.09–1.12 | +2 / 10,000 PYs |
| Diabetes | – | 0.79 | 0.67–0.93 | 0.88 | 0.77–1.01 | ||
| Gallbladder disease | Increased | 1.59 | 1.28–1.97 | 1.67 | 1.35–2.06 | ||
| Stress incontinence | – | 1.87 | 1.61–2.18 | 2.15 | 1.77–2.82 | ||
| Urge incontinence | – | 1.15 | 0.99–1.34 | 1.32 | 1.10–1.58 | ||
| Peripheral artery disease | – | 0.89 | 0.63–1.25 | 1.32 | 0.99–1.77 | ||
| Probable dementia | Decreased | 2.05 | 1.21–3.48 | 1.49 | 0.83–2.66 | ||
| Abbreviations: CEs = conjugated estrogens. MPA = medroxyprogesterone acetate. p.o. = per oral. HR = hazard ratio. AR = attributable risk. PYs = person–years. CI = confidence interval. Notes: Sample sizes (n) include placebo recipients, which were about half of patients. "Global index" is defined for each woman as the time to earliest diagnosis for coronary heart disease, stroke, pulmonary embolism, breast cancer, colorectal cancer, endometrial cancer (estrogen plus progestogen group only), hip fractures, and death from other causes. Sources: See template. | |||||||
The WHI reported statistically significant increases in rates of breast cancer, coronary heart disease, strokes and pulmonary emboli. The study also found statistically significant decreases in rates of hip fracture and colorectal cancer. "A year after the study was stopped in 2002, an article was published indicating that estrogen plus progestin also increases the risks of dementia."[70] The conclusion of the study was that the HRT combination presented risks that outweighed its measured benefits. The results were almost universally reported as risks and problems associated with HRT in general, rather than with Prempro, the specific proprietary combination of CEEs and MPA studied.
After the increased clotting found in the first WHI results was reported in 2002, the number of Prempro prescriptions filled reduced by almost half. Following the WHI results, a large percentage of HRT users opted out of them, which was quickly followed by a sharp drop in breast cancer rates. The decrease in breast cancer rates has continued in subsequent years.[71] An unknown number of women started taking alternatives to Prempro, such as compounded bioidentical hormones, though researchers have asserted that compounded hormones are not significantly different from conventional hormone therapy.[72]
The other portion of the parallel studies featured women who were post hysterectomy and so received either placebo progestogen or CEEs alone. This group did not show the risks demonstrated in the combination hormone study, and the estrogen-only study was not halted in 2002. However, in February 2004 it, too, was halted. While there was a 23% decreased incidence of breast cancer in the estrogen-only study participants, risks of stroke and pulmonary embolism were increased slightly, predominantly in patients who began HRT over the age of 60.[73]
Several other large studies and meta-analyses have reported reduced mortality for HRT in women younger than age 60 or within 10 years of menopause, and a debatable or absent effect on mortality in women over 60.[74][75][76][77][58][78]
Though research thus far has been substantial, further investigation is needed to fully understand differences in effect for different types of HRT and lengths of time since menopause.[79][80][18]
Society and public perception[edit]
Wyeth controversy[edit]
Wyeth, now a subsidiary of Pfizer, was a pharmaceutical company that marketed the HRT products Premarin (CEEs) and Prempro (CEEs + MPA).[81][82] In 2009, litigation involving Wyeth resulted in the release of 1,500 documents that revealed practices concerning its promotion of these medications.[81][82][83] The documents showed that Wyeth commissioned dozens of ghostwritten reviews and commentaries that were published in medical journals in order to promote unproven benefits of its HRT products, downplay their harms and risks, and cast competing therapies in a negative light.[81][82][83] Starting in the mid-1990s and continuing for over a decade, Wyeth pursued an aggressive "publication plan" strategy to promote its HRT products through the use of ghostwritten publications.[83] It worked mainly with DesignWrite, a medical writing firm.[83] Between 1998 and 2005, Wyeth had 26 papers promoting its HRT products published in scientific journals.[81]
These favorable publications emphasized the benefits and downplayed the risks of its HRT products, especially the "misconception" of the association of its products with breast cancer.[83] The publications defended unsupported cardiovascular "benefits" of its products, downplayed risks such as breast cancer, and promoted off-label and unproven uses like prevention of dementia, Parkinson's disease, vision problems, and wrinkles.[82] In addition, Wyeth emphasized negative messages against the SERM raloxifene for osteoporosis, instructed writers to stress the fact that "alternative therapies have increased in usage since the WHI even though there is little evidence that they are effective or safe...", called into question the quality and therapeutic equivalence of approved generic CEE products, and made efforts to spread the notion that the unique risks of CEEs and MPA were a class effect of all forms of menopausal HRT: "Overall, these data indicate that the benefit/risk analysis that was reported in the Women's Health Initiative can be generalized to all postmenopausal hormone replacement therapy products."[82]
Following the publication of the WHI data in 2002, the stock prices for the pharmaceutical industry plummeted, and huge numbers of women stopped using HRT.[84] The stocks of Wyeth, which supplied the Premarin and Prempro that were used in the WHI trials, decreased by more than 50%, and never fully recovered.[84] Some of their articles in response promoted themes such as the following: "the WHI was flawed; the WHI was a controversial trial; the population studied in the WHI was inappropriate or was not representative of the general population of menopausal women; results of clinical trials should not guide treatment for individuals; observational studies are as good as or better than randomized clinical trials; animal studies can guide clinical decision-making; the risks associated with hormone therapy have been exaggerated; the benefits of hormone therapy have been or will be proven, and the recent studies are an aberration."[60] Similar findings were observed in a 2010 analysis of 114 editorials, reviews, guidelines, and letters by five industry-paid authors.[60] These publications promoted positive themes and challenged and criticized unfavorable trials such as the WHI and MWS.[60] In 2009, Wyeth was acquired by Pfizer in a deal valued at US$68 billion.[85][86] Pfizer, a company that produces Provera and Depo-Provera (MPA) and has also engaged in medical ghostwriting, continues to market Premarin and Prempro, which remain best-selling medications.[60][83]
According to Fugh-Berman (2010), "Today, despite definitive scientific data to the contrary, many gynecologists still believe that the benefits of [HRT] outweigh the risks in asymptomatic women. This non-evidence–based perception may be the result of decades of carefully orchestrated corporate influence on medical literature."[82] As many as 50% of physicians have expressed skepticism about large trials like the WHI and HERS.[87] The positive perceptions of many physicians of HRT in spite of large trials showing risks that potentially outweigh any benefits may be due to the efforts of pharmaceutical companies like Wyeth.[83][60]
Popularity[edit]
The 1990s showed a dramatic decline in prescription rates, though more recently they have begun to rise again.[88][89]
See also[edit]
- Androgen replacement therapy
- Hormonal contraception
- Menopause
- Pharmacodynamics of progesterone
- Pharmacodynamics of estradiol
- Transgender hormone therapy (male-to-female)
References[edit]
- ^ a b c Stuenkel CA, Davis SR, Gompel A, Lumsden MA, Murad MH, Pinkerton JV, Santen RJ (November 2015). "Treatment of Symptoms of the Menopause: An Endocrine Society Clinical Practice Guideline". J. Clin. Endocrinol. Metab. 100 (11): 3975–4011. doi:10.1210/jc.2015-2236. PMID 26444994. S2CID 29118146.
- ^ a b c Santen RJ, Allred DC, Ardoin SP, Archer DF, Boyd N, Braunstein GD, Burger HG, Colditz GA, Davis SR, Gambacciani M, Gower BA, Henderson VW, Jarjour WN, Karas RH, Kleerekoper M, Lobo RA, Manson JE, Marsden J, Martin KA, Martin L, Pinkerton JV, Rubinow DR, Teede H, Thiboutot DM, Utian WH (July 2010). "Postmenopausal hormone therapy: an Endocrine Society scientific statement". J. Clin. Endocrinol. Metab. 95 (7 Suppl 1): s1–s66. doi:10.1210/jc.2009-2509. PMID 20566620.
- ^ a b c d e f g Kuhl H (2005). "Pharmacology of estrogens and progestogens: influence of different routes of administration" (PDF). Climacteric. 8 Suppl 1: 3–63. doi:10.1080/13697130500148875. PMID 16112947. S2CID 24616324.
- ^ Shuster, Lynne T.; Rhodes, Deborah J.; Gostout, Bobbie S.; Grossardt, Brandon R.; Rocca, Walter A. (2010). "Premature menopause or early menopause: Long-term health consequences". Maturitas. 65 (2): 161–166. doi:10.1016/j.maturitas.2009.08.003. ISSN 0378-5122. PMC 2815011. PMID 19733988.
- ^ a b c d e f g Eden, K.J., & Wylie, K.R. (2009). Quality of sexual life and menopause. Women’s Health, 5 (4), 385-396. doi:10.2217/whe.09.24
- ^ a b c d e Ziaei, S., Moghasemi, M., & Faghihzadeh, S. (2010). Comparative effects of conventional hormone replacement therapy and tibolone on climacteric symptoms and sexual dysfunction in postmenopausal women. Climateric, 13, 147-156. doi:10.1016/j.maturitas.2006.04.014
- ^ a b c d e f g Manson, JE; Aragaki, AK; Rossouw, JE; Anderson, GL; Prentice, RL; LaCroix, AZ; Chlebowski, RT; Howard, BV; Thomson, CA; Margolis, KL; Lewis, CE; Stefanick, ML; Jackson, RD; Johnson, KC; Martin, LW; Shumaker, SA; Espeland, MA; Wactawski-Wende, J; WHI, Investigators. (12 September 2017). "Menopausal Hormone Therapy and Long-term All-Cause and Cause-Specific Mortality: The Women's Health Initiative Randomized Trials". JAMA. 318 (10): 927–938. doi:10.1001/jama.2017.11217. PMID 28898378. S2CID 3427944.
- ^ a b c Løkkegaard, E; Nielsen, LH; Keiding, N (August 2017). "Risk of Stroke With Various Types of Menopausal Hormone Therapies: A National Cohort Study". Stroke. 48 (8): 2266–2269. doi:10.1161/STROKEAHA.117.017132. PMID 28626058. S2CID 207579406.
- ^ a b c d Files, JA; Ko, MG; Pruthi, S (July 2011). "Bioidentical hormone therapy". Mayo Clinic Proceedings. 86 (7): 673–80, quiz 680. doi:10.4065/mcp.2010.0714. PMID 21531972.
- ^ a b "USPTF Consensus Statement". 2012.
- ^ Raine-Fenning NJ, Brincat MP, Muscat-Baron Y (2003). "Skin aging and menopause : implications for treatment". Am J Clin Dermatol. 4 (6): 371–8. doi:10.2165/00128071-200304060-00001. PMID 12762829. S2CID 20392538.
- ^ Zouboulis CC, Makrantonaki E (June 2012). "Hormonal therapy of intrinsic aging". Rejuvenation Res. 15 (3): 302–12. doi:10.1089/rej.2011.1249. PMID 22533363.
- ^ a b c d e f g Sarrel, P.M. (2000). Effects of hormone replacement therapy on sexual psychophysiology and behavior in postmenopause. Journal of Women’s Health and Gender-Based Medicine, 9, 25-32
- ^ "Menopause treatments". NHS. Retrieved 2018-02-23.
- ^ Marjoribanks, Jane; Farquhar, Cindy; Roberts, Helen; Lethaby, Anne; Lee, Jasmine (17 Jan 2017). "Long-term hormone therapy for perimenopausal and postmenopausal women". The Cochrane Database of Systematic Reviews. 1: CD004143. doi:10.1002/14651858.CD004143.pub5. ISSN 1469-493X. PMID 28093732.
- ^ a b c d e Manson, JE; Chlebowski, RT; Stefanick, ML; Aragaki, AK; Rossouw, JE; Prentice, RL; Anderson, G; Howard, BV; Thomson, CA; LaCroix, AZ; Wactawski-Wende, J; Jackson, RD; Limacher, M; Margolis, KL; Wassertheil-Smoller, S; Beresford, SA; Cauley, JA; Eaton, CB; Gass, M; Hsia, J; Johnson, KC; Kooperberg, C; Kuller, LH; Lewis, CE; Liu, S; Martin, LW; Ockene, JK; O'Sullivan, MJ; Powell, LH; Simon, MS; Van Horn, L; Vitolins, MZ; Wallace, RB (2 October 2013). "Menopausal hormone therapy and health outcomes during the intervention and extended poststopping phases of the Women's Health Initiative randomized trials". JAMA. 310 (13): 1353–68. doi:10.1001/jama.2013.278040. PMID 24084921.
- ^ Zhu, L; Jiang, X; Sun, Y; Shu, W (April 2016). "Effect of hormone therapy on the risk of bone fractures: a systematic review and meta-analysis of randomized controlled trials". Menopause (New York, N.Y.). 23 (4): 461–70. doi:10.1097/GME.0000000000000519. PMID 26529613. S2CID 26110755.
- ^ a b c Studd J (March 2010). "Ten reasons to be happy about hormone replacement therapy: a guide for patients". Menopause Int. 16 (1): 44–6. doi:10.1258/mi.2010.010001. PMID 20424287. S2CID 33414205.
- ^ a b Anderson, G. L.; Limacher, M.; Assaf, A. R.; Bassford, T.; Beresford, S. A.; Black, H.; Bonds, D.; Brunner, R.; Brzyski, R.; Caan, B.; Chlebowski, R.; Curb, D.; Gass, M.; Hays, J.; Heiss, G.; Hendrix, S.; Howard, B. V.; Hsia, J.; Hubbell, A.; Jackson, R.; Johnson, K. C.; Judd, H.; Kotchen, J. M.; Kuller, L.; Lacroix, A. Z.; Lane, D.; Langer, R. D.; Lasser, N.; Lewis, C. E.; Manson, J. (2004). "Effects of Conjugated Equine Estrogen in Postmenopausal Women with Hysterectomy: The Women's Health Initiative Randomized Controlled Trial". JAMA: The Journal of the American Medical Association. 291 (14): 1701–1712. doi:10.1001/jama.291.14.1701. PMID 15082697. S2CID 38249709.
- ^ Manson, J. E.; Hsia, J.; Johnson, K. C.; Rossouw, J. E.; Assaf, A. R.; Lasser, N. L.; Trevisan, M.; Black, H. R.; Heckbert, S. R.; Detrano, R.; Strickland, O. L.; Wong, N. D.; Crouse, J. R.; Stein, E.; Cushman, M.; Women's Health Initiative Investigators (2003). "Estrogen plus Progestin and the Risk of Coronary Heart Disease". New England Journal of Medicine. 349 (6): 523–534. doi:10.1056/NEJMoa030808. PMID 12904517.
- ^ Boardman, Henry MP; Hartley, Louise; Eisinga, Anne; Main, Caroline; Roqué i Figuls, Marta; Bonfill Cosp, Xavier; Gabriel Sanchez, Rafael; Knight, Beatrice; Boardman, Henry MP (2015). "Hormone therapy for preventing cardiovascular disease in post-menopausal women". Reviews (3): CD002229. doi:10.1002/14651858.CD002229.pub4. PMID 25754617.
- ^ Darabi, M.; Rabbani, M.; Ani, M.; Zarean, E.; Panjehpour, M.; Movahedian, A. (2011). "Increased leukocyte ABCA1 gene expression in post-menopausal women on hormone replacement therapy". Gynecological Endocrinology. 27 (9): 701–705. doi:10.3109/09513590.2010.507826. PMID 20807164. S2CID 203464.
- ^ Chlebowski, RT; Anderson, GL; Sarto, GE; Haque, R; Runowicz, CD; Aragaki, AK; Thomson, CA; Howard, BV; Wactawski-Wende, J; Chen, C; Rohan, TE; Simon, MS; Reed, SD; Manson, JE (March 2016). "Continuous Combined Estrogen Plus Progestin and Endometrial Cancer: The Women's Health Initiative Randomized Trial". Journal of the National Cancer Institute. 108 (3): djv350. doi:10.1093/jnci/djv350. PMID 26668177.
- ^ Archer, DF (2001). "The effect of the duration of progestin use on the occurrence of endometrial cancer in postmenopausal women". Menopause (New York, N.Y.). 8 (4): 245–51. doi:10.1097/00042192-200107000-00005. PMID 11449081. S2CID 38526018.
- ^ a b c Kim, JJ; Kurita, T; Bulun, SE (February 2013). "Progesterone action in endometrial cancer, endometriosis, uterine fibroids, and breast cancer". Endocrine Reviews. 34 (1): 130–62. doi:10.1210/er.2012-1043. PMID 23303565.
- ^ Young, Robert; Arlan F., Jr Fuller; Fuller, Arlan F.; Michael V. Seiden (2004). Uterine cancer. Hamilton, Ont: B.C. Decker. ISBN 1-55009-163-8.
- ^ Tiidus, PM (August 2011). "Benefits of estrogen replacement for skeletal muscle mass and function in post-menopausal females: evidence from human and animal studies". The Eurasian Journal of Medicine. 43 (2): 109–14. doi:10.5152/eajm.2011.24. PMID 25610174.
- ^ Schmidt R, Fazekas F, Reinhart B, Kapeller P, Fazekas G, Offenbacher H, Eber B, Schumacher M, Freidl W (November 1996). "Estrogen replacement therapy in older women: a neuropsychological and brain MRI study". Journal of the American Geriatrics Society. 44 (11): 1307–13. doi:10.1111/j.1532-5415.1996.tb01400.x. PMID 8909345. S2CID 22921797.
- ^ Miller M.M.; Franklin K.B.J. (1999). "Theoretical basis for the benefit of postmenopausal estrogen substitution". Experimental Gerontology. 34 (5): 587–604. doi:10.1016/S0531-5565(99)00032-7. PMID 10530785. S2CID 43031351.
- ^ Gonzalez, M., Viagara, G., Caba, F., & Molina, E. (2004). Sexual function, menopause and hormone replacement therapy (HRT). The European Menopause Journal, 48, 411-420. doi:10.1016/j.maturitas.2003.10.005
- ^ a b "Menopausal Hormone Therapy and Cancer Risk". www.cancer.org. Retrieved 4 March 2019.
- ^ Fournier, A. S.; Berrino, F.; Clavel-Chapelon, F. O. (2007). "Unequal risks for breast cancer associated with different hormone replacement therapies: Results from the E3N cohort study". Breast Cancer Research and Treatment. 107 (1): 103–111. doi:10.1007/s10549-007-9523-x. PMC 2211383. PMID 17333341.
- ^ Letendre, I.; Lopes, P. (2012). "Ménopause et risques carcinologiques". Journal de Gynécologie Obstétrique et Biologie de la Reproduction. 41 (7): F33–F37. doi:10.1016/j.jgyn.2012.09.006. PMID 23062839.
- ^ Stefanick ML; Anderson GL; Margolis KL; et al. (2006). "Effects of conjugated equine estrogens on breast cancer and mammography screening in postmenopausal women with hysterectomy". JAMA. 295 (14): 1647–57. doi:10.1001/jama.295.14.1647. PMID 16609086. S2CID 3956784.
- ^ "Association between hormone replacement therapy use and breast cancer risk varies by race/ethnicity, body mass index, and breast density". JNCI Journal of the National Cancer Institute. 105 (18). 2013. doi:10.1093/jnci/djt264. ISSN 0027-8874.
- In turn citing: Hou, N.; Hong, S.; Wang, W.; Olopade, O. I.; Dignam, J. J.; Huo, D. (2013). "Hormone Replacement Therapy and Breast Cancer: Heterogeneous Risks by Race, Weight, and Breast Density". JNCI Journal of the National Cancer Institute. 105 (18): 1365–1372. doi:10.1093/jnci/djt207. ISSN 0027-8874. PMC 3776262. PMID 24003037.
- ^ Kuhl, H.; Schneider, H. P. G. (2013). "Progesterone – promoter or inhibitor of breast cancer". Climacteric. 16 Suppl 1: 54–68. doi:10.3109/13697137.2013.768806. PMID 23336704. S2CID 20808536.
- ^ Management of the menopause after breast cancer Archived 2016-04-07 at archive.today, from The Royal Australian and New Zealand College of Obstetricians and Gynaecologists. College Statement C-Gyn 15. 1st Endorsed: February 2003. Current: November 2011. Review: November 2014
- ^ Collaborative Group on Epidemiological Studies of Ovarian Cancer (12 February 2015). "Menopausal hormone use and ovarian cancer risk: individual participant meta-analysis of 52 epidemiological studies". The Lancet. 385 (9980): 1835–1842. doi:10.1016/S0140-6736(14)61687-1.
- ^ a b c Shi, LF; Wu, Y; Li, CY (April 2016). "Hormone therapy and risk of ovarian cancer in postmenopausal women: a systematic review and meta-analysis". Menopause (New York, N.Y.). 23 (4): 417–24. doi:10.1097/GME.0000000000000550. PMID 26506499. S2CID 32195397.
- ^ a b Scarabin, P.-Y. (August 2018). "Progestogens and venous thromboembolism in menopausal women: an updated oral versus transdermal estrogen meta-analysis". Climacteric. 21 (4): 341–345. doi:10.1080/13697137.2018.1446931. ISSN 1473-0804. PMID 29570359. S2CID 4229701.
- ^ Olié, V. R.; Canonico, M.; Scarabin, P. Y. (2010). "Risk of venous thrombosis with oral versus transdermal estrogen therapy among postmenopausal women". Current Opinion in Hematology. 17 (5): 457–463. doi:10.1097/MOH.0b013e32833c07bc. PMID 20601871. S2CID 205827003.
- ^ a b Carrasquilla GD, Frumento P, Berglund A, Borgfeldt C, Bottai M, Chiavenna C, Eliasson M, Engström G, Hallmans G, Jansson JH, Magnusson PK, Nilsson PM, Pedersen NL, Wolk A, Leander K (November 2017). "Postmenopausal hormone therapy and risk of stroke: A pooled analysis of data from population-based cohort studies". PLOS Med. 14 (11): e1002445. doi:10.1371/journal.pmed.1002445. PMC 5693286. PMID 29149179.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Morley JE, Perry HM (May 2003). "Androgens and women at the menopause and beyond". J. Gerontol. A Biol. Sci. Med. Sci. 58 (5): M409–16. doi:10.1093/gerona/58.5.M409. PMID 12730248.
- ^ Garefalakis M, Hickey M (2008). "Role of androgens, progestins and tibolone in the treatment of menopausal symptoms: a review of the clinical evidence". Clin Interv Aging. 3 (1): 1–8. doi:10.2147/CIA.S1043. PMC 2544356. PMID 18488873.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Estrogen (Vaginal Route) from Mayo Clinic / Thomson Healthcare Inc. Portions of this document last updated: Nov. 1, 2011
- ^ Fraser IS, Mansour D (March 2006). "Delivery systems for hormone replacement therapy". Expert Opin Drug Deliv. 3 (2): 191–204. doi:10.1517/17425247.3.2.191. PMID 16506947. S2CID 29446836.
- ^ Beck, KL; Anderson, MC; Kirk, JK (August 2017). "Transdermal estrogens in the changing landscape of hormone replacement therapy". Postgraduate Medicine. 129 (6): 632–636. doi:10.1080/00325481.2017.1334507. PMID 28540770. S2CID 205452835.
- ^ a b c d e Conaway E (March 2011). "Bioidentical hormones: an evidence-based review for primary care providers". J Am Osteopath Assoc. 111 (3): 153–64. PMID 21464264.
- ^ a b "FDA Takes Action Against Compounded Menopause Hormone Therapy Drugs". FDA. 2008-01-09. Retrieved 2009-02-17.
- ^ Simon JA (July 2014). "What if the Women's Health Initiative had used transdermal estradiol and oral progesterone instead?". Menopause. 21 (7): 769–83. doi:10.1097/GME.0000000000000169. PMID 24398406. S2CID 30292136.
- ^ Pinkerton, JV; Pickar, JH (February 2016). "Update on medical and regulatory issues pertaining to compounded and FDA-approved drugs, including hormone therapy". Menopause (New York, N.Y.). 23 (2): 215–23. doi:10.1097/GME.0000000000000523. PMID 26418479. S2CID 30612542.
- ^ Deleruyelle, LJ (2017). "Menopausal Symptom Relief and Side Effects Experienced by Women Using Compounded Bioidentical Hormone Replacement Therapy and Synthetic Conjugated Equine Estrogen and/or Progestin Hormone Replacement Therapy, Part 3". International Journal of Pharmaceutical Compounding. 21 (1): 6–16. PMID 28346192.
- ^ Suchowersky O, Muthipeedika J (December 2005). "A case of late-onset chorea". Nat Clin Pract Neurol. 1 (2): 113–6. doi:10.1038/ncpneuro0052. PMID 16932507. S2CID 11410333.
- ^ MacLennan, AH (August 2011). "HRT in difficult circumstances: are there any absolute contraindications?". Climacteric : The Journal of the International Menopause Society. 14 (4): 409–17. doi:10.3109/13697137.2010.543496. PMID 21355685. S2CID 25426141.
- ^ Lewis, Ricki. "ACOG Revises Guidelines on Treating Menopause Symptoms". login.medscape.com. Medscape. Retrieved 4 March 2019.
- ^ "Hormone Therapy and Heart Disease - ACOG". www.acog.org. Committee on Gynecologic Practice. Retrieved 4 March 2019.
- ^ "Medscape". www.medscape.com.
- ^ a b Santen, RJ; Utian, WH (2010). "Executive Summary: Postmenopausal Hormone Therapy: An Endocrine Society Scientific Statement". J Clin Endocrinol Metab. 95 S1–S66 (Supplement 1): s1–s66. doi:10.1210/jc.2009-2509. Retrieved Jan 16, 2015.
- ^ Cobin, RH; Goodman, NF; AACE Reproductive Endocrinology Scientific, Committee. (July 2017). "American Association of Clinical Endocrinologists and American College of Endocrinology Position Statement on Menopause–2017 Update" (PDF). Endocrine Practice : Official Journal of the American College of Endocrinology and the American Association of Clinical Endocrinologists. 23 (7): 869–880. doi:10.4158/EP171828.PS. PMID 28703650. Retrieved 1 March 2019.
- ^ a b c d e f g h i j Fugh-Berman, Adriane (2015). "The Science of Marketing: How Pharmaceutical Companies Manipulated Medical Discourse on Menopause". Women's Reproductive Health. 2 (1): 18–23. doi:10.1080/23293691.2015.1039448. ISSN 2329-3691.
- ^ IARC Working Group on the Evaluation of Carcinogenic Risks to Humans; World Health Organization; International Agency for Research on Cancer (2007). Combined Estrogen-progestogen Contraceptives and Combined Estrogen-progestogen Menopausal Therapy. World Health Organization. pp. 205–. ISBN 978-92-832-1291-1.
- ^ a b c Writing Group for the Women's Health Initiative Investigators (2002). "Risks and Benefits of Estrogen Plus Progestin in Healthy Postmenopausal Women: Principal Results From the Women's Health Initiative Randomized Controlled Trial". JAMA. 288 (3): 321–333. doi:10.1001/jama.288.3.321. PMID 12117397. S2CID 20149703.
- ^ Chlebowski RT, Kuller LH, Prentice RL, Stefanick ML, Manson JE, Gass M, et al. (February 2009). "Breast cancer after use of estrogen plus progestin in postmenopausal women". The New England Journal of Medicine. 360 (6): 573–87. doi:10.1056/NEJMoa0807684. PMC 3963492. PMID 19196674.
- ^ Kreatsoulas, C.; Anand, S. S. (2013). "Menopausal hormone therapy for the primary prevention of chronic conditions. U.S. Preventive Services Task Force Recommendation Statement" (PDF). Polskie Archiwum Medycyny Wewnetrznej. 123 (3): 112–117. PMID 23396275.
- ^ a b Nelson, H. D.; Walker, M.; Zakher, B.; Mitchell, J. (2012). "Menopausal hormone therapy for the primary prevention of chronic conditions: A systematic review to update the U.S. Preventive Services Task Force recommendations". Annals of Internal Medicine. 157 (2): 104–113. doi:10.7326/0003-4819-157-2-201207170-00466. PMID 22786830. S2CID 25829459.
- ^ George, James L.; Colman, Robert W.; Goldhaber, Samuel Z.; Victor J. Marder (2006). Hemostasis and thrombosis: basic principles and clinical practice. Hagerstwon, MD: Lippincott Williams & Wilkins. pp. 1239. ISBN 0-7817-4996-4.
- ^ Darabi M, Ani M, Panjehpour M, Rabbani M, Movahedian A, Zarean E (2011). "Effect of estrogen receptor β A1730G polymorphism on ABCA1 gene expression response to postmenopausal hormone replacement therapy". Genetic Testing and Molecular Biomarkers. 15 (1–2): 11–5. doi:10.1089/gtmb.2010.0106. PMID 21117950.
- ^ Chlebowski, R. T.; Anderson, G. L. (2015). "Menopausal hormone therapy and breast cancer mortality: clinical implications". Therapeutic Advances in Drug Safety. 6 (2): 45–56. doi:10.1177/2042098614568300. ISSN 2042-0986. PMC 4406918. PMID 25922653.
- ^ Rossouw, J. E.; Prentice, R. L.; Manson, J. E.; Wu, L.; Barad, D.; Barnabei, V. M.; Ko, M.; Lacroix, A. Z.; Margolis, K. L.; Stefanick, M. L. (2007). "Postmenopausal Hormone Therapy and Risk of Cardiovascular Disease by Age and Years Since Menopause". JAMA: The Journal of the American Medical Association. 297 (13): 1465–1477. doi:10.1001/jama.297.13.1465. PMID 17405972. S2CID 16529377.
- ^ Mazzucco AE, Santoro E, DeSoto M, Lee JH (December 2010). "Hormone Therapy and Menopause". National Research Center for Women and Families.
- ^ Gina Kolata (2007-04-19). "Sharp Drop in Rates of Breast Cancer Holds". New York Times.
- ^ Roni Caryn Rabin (2007-08-28). "For a Low-Dose Hormone, Take Your Pick". New York Times.
Many women seeking natural remedies have turned to compounding pharmacies, which use bioidentical hormones that are chemically synthesized but with the same molecular structure as hormones produced by a woman's body.
- ^ John Gever (2011-04-05). "New WHI Estrogen Analysis Shows Lower Breast Ca Risk". MedPageToday.
- ^ Salpeter, S. R.; Cheng, J.; Thabane, L.; Buckley, N. S.; Salpeter, E. E. (2009). "Bayesian Meta-analysis of Hormone Therapy and Mortality in Younger Postmenopausal Women". The American Journal of Medicine. 122 (11): 1016–1022.e1. doi:10.1016/j.amjmed.2009.05.021. PMID 19854329.
- ^ Anderson, G. L.; Chlebowski, R. T.; Rossouw, J. E.; Rodabough, R. J.; McTiernan, A.; Margolis, K. L.; Aggerwal, A.; David Curb, J. D.; Hendrix, S. L.; Allan Hubbell, F. A.; Khandekar, J.; Lane, D. S.; Lasser, N.; Lopez, A. M.; Potter, J.; Ritenbaugh, C. (2006). "Prior hormone therapy and breast cancer risk in the Women's Health Initiative randomized trial of estrogen plus progestin". Maturitas. 55 (2): 103–115. doi:10.1016/j.maturitas.2006.05.004. PMID 16815651.
- ^ Hulley, S.; Grady, D.; Bush, T.; Furberg, C.; Herrington, D.; Riggs, B.; Vittinghoff, E. (1998). "Randomized trial of estrogen plus progestin for secondary prevention of coronary heart disease in postmenopausal women. Heart and Estrogen/progestin Replacement Study (HERS) Research Group". JAMA: The Journal of the American Medical Association. 280 (7): 605–613. doi:10.1001/jama.280.7.605. PMID 9718051.
- ^ Salpeter, S. R.; Walsh, J. M. E.; Greyber, E.; Ormiston, T. M.; Salpeter, E. E. (2004). "Mortality associated with hormone replacement therapy in younger and older women". Journal of General Internal Medicine. 19 (7): 791–804. doi:10.1111/j.1525-1497.2004.30281.x. PMC 1492478. PMID 15209595.
- ^ Grodstein, F.; Stampfer, M. J.; Colditz, G. A.; Willett, W. C.; Manson, J. E.; Joffe, M.; Rosner, B.; Fuchs, C.; Hankinson, S. E.; Hunter, D. J.; Hennekens, C. H.; Speizer, F. E. (1997). "Postmenopausal Hormone Therapy and Mortality". New England Journal of Medicine. 336 (25): 1769–1775. doi:10.1056/NEJM199706193362501. PMID 9187066.
- ^ Bethea CL (Feb 2011). "MPA: Medroxy-Progesterone Acetate Contributes to Much Poor Advice for Women". Endocrinology. 152 (2): 343–345. doi:10.1210/en.2010-1376. PMC 3037166. PMID 21252179.
- ^ Harman SM, Brinton EA, Cedars M, Lobo R, Manson JE, Merriam GR, Miller VM, Naftolin F, Santoro N (March 2005). "KEEPS: The Kronos Early Estrogen Prevention Study". Climacteric. 8 (1): 3–12. doi:10.1080/13697130500042417. PMID 15804727. S2CID 37219662.
- ^ a b c d Singer, Natasha (4 August 2009). "Medical Papers by Ghostwriters Pushed Therapy". The New York Times. Retrieved 13 July 2018.
- ^ a b c d e f Fugh-Berman AJ (September 2010). "The haunting of medical journals: how ghostwriting sold "HRT"". PLOS Med. 7 (9): e1000335. doi:10.1371/journal.pmed.1000335. PMC 2935455. PMID 20838656.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ a b c d e f g Steve Kent May; Steve May (20 January 2012). Case Studies in Organizational Communication: Ethical Perspectives and Practices: Ethical Perspectives and Practices. SAGE. pp. 197–. ISBN 978-1-4129-8309-9.
- ^ a b Miller VM, Harman SM (November 2017). "An update on hormone therapy in postmenopausal women: mini-review for the basic scientist". Am. J. Physiol. Heart Circ. Physiol. 313 (5): H1013–H1021. doi:10.1152/ajpheart.00383.2017. PMID 28801526. S2CID 207650230.
- ^ https://www.nytimes.com/2009/01/26/business/26drug.html
- ^ https://www.cnbc.com/id/33384753
- ^ Tao M, Teng Y, Shao H, Wu P, Mills EJ (2011). "Knowledge, perceptions and information about hormone therapy (HT) among menopausal women: a systematic review and meta-synthesis". PLOS ONE. 6 (9): e24661. doi:10.1371/journal.pone.0024661. PMC 3174976. PMID 21949743.
- ^ Beck, KL; Anderson, MC; Kirk, JK (August 2017). "Transdermal estrogens in the changing landscape of hormone replacement therapy". Postgraduate Medicine. 129 (6): 632–636. doi:10.1080/00325481.2017.1334507. PMID 28540770. S2CID 205452835.
- ^ "Hormone therapy for brain performance: No effect, whether started early or late". www.sciencedaily.com.
External links[edit]
Category:Endocrine procedures Category:Life sciences industry Category:Menopause
