Polyestradiol phosphate
 | |
| Clinical data | |
|---|---|
| Trade names | Estradurin |
| Other names | Leo-114[1] |
| AHFS/Drugs.com | International Drug Names |
| Pregnancy category |
|
| Routes of administration | Intramuscular injection |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Protein binding | >95% (estradiol)[2] |
| Metabolism | Mainly liver |
| Elimination half-life | 70 days (320 mg i.m.)[3] |
| Excretion | Urine |
| Identifiers | |
| |
| CAS Number | |
| PubChem SID | |
| ChemSpider |
|
| UNII | |
| KEGG | |
| ChEMBL | |
| Chemical and physical data | |
| Formula | (C18H22)m(O4P)n (m, n ≈ 80)[citation needed] |
| Molar mass | Polymer: ~26 g/mol[citation needed] Repeat unit: 370.382 g/mol |
| Melting point | 195 to 202 °C (383 to 396 °F) |
| | |
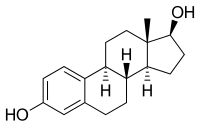
Polyestradiol phosphate (PEP) (INN, BAN) (brand name Estradurin), also known as estradiol polymer with phosphoric acid or as estradiol 17β-phosphate polymer, is a synthetic, steroidal estrogen and an estrogen ester in the form of a polymer[4] – specifically, the 17β-phosphate ester polymer of estradiol – which is used in the treatment of prostate cancer.[1][5][6][7] It is administered via intramuscular injection once a month and acts as a very long-lasting prodrug of estradiol.[8] PEP was introduced by Pfizer in 1957 and has been marketed in the United States and throughout Europe.[1][9][10][11] It is no longer available in the U.S.[9][12]
Medical uses
PEP is used as an intramuscular injection for estrogen therapy of prostate cancer. It is available in combination with mepivacaine, a local anaesthetic, to avoid a burning sensation during application. After injection, it releases the active agent estradiol over several weeks.[13]
Intramuscular PEP has been compared to combined androgen blockade (castration + flutamide) for the treatment of prostate cancer in a large randomized clinical trial of 915 patients.[14][15] At 18.5 months, there was no difference in survival or cardiovascular toxicity between the two treatment modalities.[14][15] These findings suggest that parenteral forms of estradiol may have similar effectiveness and safety relative to androgen deprivation therapy (ADT) in the treatment of prostate cancer.[14][15] In addition, estrogen may have significant advantages relative to ADT in terms of bone loss and fractures, hot flashes, and sexual function, as well as considerable cost savings with parenteral forms of estradiol compared to GnRH analogue therapy.[14][15] On the other hand, gynecomastia and breast tenderness occur at relatively high rates with estrogens, whereas incidences are low with castration or combined androgen blockade.[16]
Contraindications
The drug has the same contraindications as other forms of estradiol, including active thromboembolism (such as myocardial infarction) or high risk for thromboembolic events, asthma, and severe hepatic impairment.[7][13]
Side effects
Although systematic studies of the drug's adverse effects are missing, it is assumed that they are identical to the effects observed under therapy with estradiol and other estrogens. These include nausea, headache, sodium and water retention, gain (but sometimes loss) of body weight, impaired glucose tolerance, and mood swings (in 40% of patients). Allergic reactions of the skin include itching, erythema multiforme and, rarely, Stevens–Johnson syndrome.[7] As thromboembolic complications are associated mainly with oral estrogens and attributed to the first-pass effect, they are expected to occur less frequently under parenteral therapies such as PEP.[13]
Overdose typically manifests itself by reversible feminization.[13]
Interactions
Estradiol levels may be increased by CYP3A4 inhibitors such as erythromycin, clarithromycin, ketoconazole, itraconazole and grapefruit juice, and lowered by CYP3A4 inducers such as St John's wort, barbiturates, carbamazepine and rifampicin. The combination with COX-2 inhibitors can increase the risk for thromboembolism. Estradiol can also increase the effects of glucocorticoids.[13][17]
Pharmacology
The growth of prostate cancer is generally stimulated by dihydrotestosterone (DHT); and unless the cancer is castration resistant, it can be treated by depriving it of DHT. Estradiol inhibits the action of DHT by several mechanisms. Firstly, it acts over the hypothalamic–pituitary–gonadal axis feedback loop by blocking secretion of luteinizing hormone, which reduces testosterone synthesis in Leydig cells in the testicle. It blocks testosterone uptake into prostate cells, where it would be metabolized to DHT by the enzyme 5α-reductase. Estradiol also inhibits 5α-reductase directly, blocks binding of DHT to androgen receptors, and exhibits cytotoxicity on prostate cancer cells.[7][13]
Antigonadotropic activity
PEP is antigonadotropic due to its estrogenic activity.[18] It has been found to suppress testosterone levels in men by 55, 75, and 85% at intramuscular dosages of 80, 160, and 240 mg every 4 weeks, respectively.[19] A single intramuscular dose of 320 mg PEP in men has been found to suppress testosterone levels into the castrate range within 3 weeks.[3]
Pharmacokinetics
Dosage Time |
160 mg | 240 mg | 320 mg |
|---|---|---|---|
| Day 2 | 55 pg/mL | 89 pg/mL | 204 pg/mL |
| Day 28 | 136 pg/mL | 163 pg/mL | 218 pg/mL |
| Day 90 | 272 pg/mL | 409 pg/mL | 518 pg/mL |
| Day 180 | 409 pg/mL | 477 pg/mL | 681 pg/mL |
and Day 28 is prior to the second injection. | |||
PEP reaches the bloodstream within hours after the injection (90% after 24 hours), and is accumulated in the reticuloendothelial system.[7] Estradiol is then cleaved from the polymer by phosphatases, although slowly because PEP acts as a phosphatase inhibitor.[21] With monthly injections, stable estradiol concentrations are reached after six to twelve months.[7] Estradiol is metabolized primarily in the liver by CYP3A4 and other cytochrome enzymes, and to a lesser extent in extrahepatic tissues.[13] The metabolites are mainly excreted via the kidneys.
PEP has a very long duration and is given by intramuscular injection once-monthly.[20] In men, an initial intramuscular injection of PEP results in a rapid rise in estradiol levels measured at 24 hours followed by a slow and gradual further increase in levels up until at least day 28 (the time of the next injection).[20] Subsequent injections result in a progressive and considerable accumulation in estradiol levels up to at least 6 months.[20] The mean terminal half-life of PEP has been found to be 70 days with a single 320 mg intramuscular dose of the drug.[3]
In light of the fact that phosphatases, which cleave PEP into estradiol and phosphoric acid, are present in most tissues in the body, it has been said that the long terminal half-life and slow release of PEP are somewhat surprising.[19] Research has found that PEP acts as an inhibitor of alkaline phosphatase in vitro, and it has been proposed that PEP may inhibit its own metabolism.[19]
Chemistry
PEP is a polymer of estradiol and phosphoric acid.[19] It has been determined via ultracentrifugation that the mean molecular weight of PEP corresponds to a chain length of approximately 13 repeat units of estradiol 17β-phosphate.[19]
Solubility
PEP is of very low solubility in water, acetone, chloroform, dioxane, and ethanol, but solves readily in bases, especially in aqueous pyridine.[7]
Synthesis
Like polyphosphates of polyphenols, PEP can be prepared from the monomer (in this case estradiol) and phosphoryl chloride. The latter reacts with both the phenolic hydroxyl group in position 3 and the aliphatic one in position 17. The molecular mass of the resulting polymer can be controlled by interrupting the reaction after a given time: the longer the reaction is allowed to continue, the higher the mass.[21][22]
History
Pharmacological experiments on estradiol phosphates conducted around 1950 gave rise to the hypothesis that estradiol 3,17β-diphosphate acted as an inhibitor of kidney alkaline phosphatase.[21] When the same scientists wanted to synthesize simple phosphates of phloretin, a compound found in apple tree leaves,[23] they accidentally created a polymer instead.[22] This was later shown to exhibit the same anti-phosphatase properties as estradiol diphosphate, and so it was hypothesized that the original finding was due to contamination with estradiol phosphate polymers.[21] Consequently, these polymers were studied in more detail, which resulted in the development of PEP as early as 1953[8] and its subsequent introduction in 1957 in the United States.[9][10]
Society and culture
Availability
PEP has been marketed in the United States and throughout Europe, including in Austria, Denmark, Finland, Germany, the Netherlands, Norway, Spain, Sweden, and Switzerland.[1] It is no longer available in the U.S.,[9][12] but it is still reported to be marketed in Denmark, Sweden, and Switzerland.[24]
References
- ^ a b c d Index Nominum 2000: International Drug Directory. Taylor & Francis. January 2000. pp. 856–. ISBN 978-3-88763-075-1.
- ^ "Estradurin" (in German). Arzneimittel-Kompendium der Schweiz. August 2008. Retrieved 22 April 2012.
- ^ a b c Stege R, Gunnarsson PO, Johansson CJ, Olsson P, Pousette A, Carlström K (1996). "Pharmacokinetics and testosterone suppression of a single dose of polyestradiol phosphate (Estradurin) in prostatic cancer patients". Prostate. 28 (5): 307–10. doi:10.1002/(SICI)1097-0045(199605)28:5<307::AID-PROS6>3.0.CO;2-8. PMID 8610057.
- ^ Johansson, CJ; Gunnarsson, PO (June 2000). "Pharmacodynamic model of testosterone suppression after intramuscular depot estrogen therapy in prostate cancer". Prostate. 44 (1): 26–30. doi:10.1002/1097-0045(20000615)44:1<26::AID-PROS4>3.0.CO;2-P. PMID 10861754.
- ^ S. Gangolli (1999). The Dictionary of Substances and Their Effects: O-S. Royal Society of Chemistry. pp. 425–. ISBN 978-0-85404-833-5.
- ^ Mikkola, A; Aro, J; Rannikko, S; Ruutu, M; Finnprostate, Group (March 2007). "Ten-year survival and cardiovascular mortality in patients with advanced prostate cancer primarily treated by intramuscular polyestradiol phosphate or orchiectomy". Prostate. 67 (4): 447–55. doi:10.1002/pros.20547. PMID 17219379.
{{cite journal}}:|first5=has generic name (help) - ^ a b c d e f g Dinnendahl, V; Fricke, U, eds. (2010). Arzneistoff-Profile (in German). Vol. 4 (23 ed.). Eschborn, Germany: Govi Pharmazeutischer Verlag. ISBN 978-3-7741-98-46-3.
- ^ a b Steinbach T, Wurm FR (2015). "Poly(phosphoester)s: A New Platform for Degradable Polymers". Angew. Chem. Int. Ed. Engl. 54 (21): 6098–108. doi:10.1002/anie.201500147. PMID 25951459.
- ^ a b c d "Drugs@FDA: FDA Approved Drug Products: Estradurin" (HTML). United States Food and Drug Administration. Retrieved 12 October 2016.
- ^ a b William Andrew Publishing (22 October 2013). Pharmaceutical Manufacturing Encyclopedia. Elsevier. pp. 2935–. ISBN 978-0-8155-1856-3.
- ^ "Produktresumé for Estradurin" (PDF) (in Danish). 29 January 2010. Retrieved 21 April 2012.
{{cite web}}: Unknown parameter|trans_title=ignored (|trans-title=suggested) (help) - ^ a b Mosby (11 February 2009). Mosby's Pocket Dictionary of Medicine, Nursing & Health Professions. Elsevier Health Sciences. pp. 3672–. ISBN 0-323-06604-6.
- ^ a b c d e f g W, Jasek, ed. (2007). Austria-Codex (in German) (62nd ed.). Vienna: Österreichischer Apothekerverlag. pp. 2992–4. ISBN 978-3-85200-181-4.
- ^ a b c d Sayed Y, Taxel P (2003). "The use of estrogen therapy in men". Curr Opin Pharmacol. 3 (6): 650–4. PMID 14644018.
- ^ a b c d Hedlund PO, Henriksson P (2000). "Parenteral estrogen versus total androgen ablation in the treatment of advanced prostate carcinoma: effects on overall survival and cardiovascular mortality. The Scandinavian Prostatic Cancer Group (SPCG)-5 Trial Study". Urology. 55 (3): 328–33. PMID 10699602.
- ^ Deepinder F, Braunstein GD (2012). "Drug-induced gynecomastia: an evidence-based review". Expert Opinion on Drug Safety. 11 (5): 779–95. doi:10.1517/14740338.2012.712109. PMID 22862307.
Treatment with estrogen has the highest incidence of gynecomastia, at 40 – 80%, anti-androgens, including flutamide, bicalutamide and nilutamide, are next, with a 40 – 70% incidence, followed by GnRH analogs (goserelin, leuprorelin) and combined androgen deprivation, both with incidences of 13% each.
- ^ Klopp, T, ed. (2011). Arzneimittel-Interaktionen (in German) (2011/2012 ed.). Arbeitsgemeinschaft für Pharmazeutische Information. ISBN 978-3-85200-214-9.
- ^ Waun Ki Hong; James F. Holland (2010). Holland-Frei Cancer Medicine 8. PMPH-USA. pp. 753–. ISBN 978-1-60795-014-1.
- ^ a b c d e Gunnarsson PO, Norlén BJ (1988). "Clinical pharmacology of polyestradiol phosphate". Prostate. 13 (4): 299–304. PMID 3217277.
- ^ a b c d Stege R, Carlström K, Collste L, Eriksson A, Henriksson P, Pousette A (1988). "Single drug polyestradiol phosphate therapy in prostatic cancer". Am. J. Clin. Oncol. 11 Suppl 2: S101–3. PMID 3242384.
- ^ a b c d Diczfalusy, E (April 1954). "Poly-estradiol phosphate (PEP); a long-acting water soluble estrogen". Endocrinology. 54 (4): 471–7. doi:10.1210/endo-54-4-471. PMID 13151143.
- ^ a b Diczfalusy, E; Fernö, O; Fex, H; Högberg, B; Linderot, T; Rosenberg, Th (1953). "Synthetic high molecular weight enzyme inhibitors. I. Polymeric phosphates of phloretin and related compounds" (PDF). Acta Chem Scand. 7 (6): 921–7. doi:10.3891/acta.chem.scand.07-0913.
- ^ Picinelli, A; Dapena, E; Mangas, JJ (1995). "Polyphenolic pattern in apple tree leaves in relation to scab resistance. A preliminary study". Journal of Agricultural and Food Chemistry. 43 (8): 2273–78. doi:10.1021/jf00056a057.
- ^ Drugs.com: International Drug Names