Thiazide

Thiazide (/ˈθaɪəzaɪd/) is a type of molecule[1] and a class of diuretics[2] often used to treat hypertension (high blood pressure) and edema (such as that caused by heart failure, liver failure, or kidney failure).
The thiazides and thiazide-like diuretics reduce the risk of death, stroke, heart attack, and heart failure due to hypertension.[3][needs update] The class was discovered and developed at Merck and Co. in the 1950s, and the first approved drug of this class, chlorothiazide, was marketed under the trade name Diuril beginning in 1958.[4] In most countries, the thiazides are the cheapest antihypertensive drugs available.[5]
Medical uses
Hypertension
Regarding effectiveness in the treatment of hypertension, a systematic review by the Cochrane Collaboration found:[6]
- Chlorthalidone reduces systolic and diastolic blood pressure by 12.0/4 mmHg and the reduction is not dose related when tested at a range of doses from 12.5 mg to 75 mg/day.
- Hydrochlorothiazide's effect is dose related and at a maximum dose of 50 mg/day, the reduction is 11 mmHg/5 mmHg.
Thiazides and thiazide-like diuretics have been in constant use since their introduction in 1958. They "have remained a cornerstone in the management of hypertension for more than half a century since their introduction [...] Very few agents used for the treatment of any disease can boast such staying power, which is a testament both to the efficacy and safety of these compounds." [7]
Several clinical practice guidelines address the use of thiazides. They are the recommended first-line treatment in the US (JNC VIII)[8] guidelines for hypertension and a recommended treatment in the European (ESC/ESH)[9] guidelines. However, the recent 2011 UK National Institute for Health and Clinical Excellence (NICE) guideline on the management of primary hypertension in adults (CG127)[10] recommend calcium channel blockers (CCBs) as first line agents in hypertension and advise that thiazide-like diuretics should only be used first line if CCBs are not suitable or if the patient has oedema or has a high risk of developing heart failure. Thiazides have also been replaced by angiotensin converting enzyme (ACE) inhibitors in Australia due to their propensity to increase risk of diabetes mellitus type 2.[11]
The mechanism of action of thiazides in lowering blood pressure in the long term is not fully understood. When administered acutely thiazides lower blood pressure by causing diuresis, a fall in plasma volume and a reduction in cardiac output. However, after chronic use thiazides cause a reduction in blood pressure by lowering peripheral resistance (i.e. vasodilation). The mechanism of this effect is uncertain but it may involve effects on 'whole body' or renal autoregulation, or direct vasodilator actions either through inhibition of carbonic anhydrase[12] or by desensitizing the vascular smooth muscle cells to the rise in intracellular calcium induced by norepinephrine.[13]
Other
Thiazides also lower urinary calcium excretion, making them useful in preventing calcium-containing kidney stones. This effect is associated with positive calcium balance and is associated with an increase in bone mineral density and reductions in fracture rates attributable to osteoporosis.[14] By a lesser understood mechanism, thiazides directly stimulate osteoblast differentiation and bone mineral formation, further slowing the course of osteoporosis.[15]
Because of their promotion of calcium retention, thiazides are used in the treatment of
- Dent's disease
- Hypocalcemia
- Nephrolithiasis (idiopathic hypercalciuria)
- Bromide intoxication
- Nephrogenic diabetes insipidus
Contraindications
Contraindications include:
- Hypotension
- Allergy to sulphur-containing medications
- Gout
- Renal failure
- Lithium therapy
- Hypokalemia
- May worsen diabetes
Thiazides reduce the clearance of uric acid since they compete for the same transporter, and therefore raise the levels of uric acid in the blood. Hence they are prescribed with caution in patients with gout or hyperuricemia.[16][17]
Chronic administration is associated with hyperglycemia.
Thiazides cause loss of blood potassium, while conserving blood calcium.
Thiazides can decrease placental perfusion and adversely affect the fetus so should be avoided in pregnancy.[17][18]
Adverse effects
- Hypokalemia - Thiazide diuretics reduces potassium concentration in blood through two indirect mechanisms: inhibition of sodium-chloride symporter at distal convoluted tubule of a nephron and stimulation of aldosterone that activates Na+/K+-ATPase at collecting duct. Inhibition of sodium-chloride symporter increases availability of sodium and chloride in urine. When the urine reaches the collecting duct, the increase in sodium and chloride availability activates Na+/K+-ATPase, which increases the absorption of sodium and excretion of potassium into the urine. Long term administration of thiazide diuretics reduces total body blood volume. This activates the renin–angiotensin system, stimulates the secretion of aldosterone, thus activating Na+/K+-ATPase, increasing excretion of potassium in urine.[19] Therefore, ACE inhibitor and thiazide combination is used to prevent hypokalemia.
- Hyperglycemia
- Hyperlipidemia
- Hyperuricemia
- Hypercalcemia
- Hyponatremia
- Hypomagnesemia
- Hypocalciuria
Mechanism of action
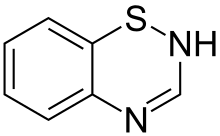
The members of this class of diuretics are derived from benzothiadiazine. They control hypertension in part by inhibiting reabsorption of sodium (Na+) and chloride (Cl−) ions from the distal convoluted tubules in the kidneys by blocking the thiazide-sensitive Na+-Cl− symporter.[20] The term "thiazide" is also often used for drugs with a similar action that do not have the thiazide chemical structure, such as chlorthalidone and metolazone. These agents are more properly termed thiazide-like diuretics.
Thiazide diuretics also increase calcium reabsorption at the distal tubule. By lowering the sodium concentration in the tubule epithelial cells, thiazides indirectly increase the activity of the basolateral Na+/Ca2+ antiporter to maintain intracellular Na+ level, facilitating Ca2+ to leave the epithelial cells into the renal interstitium. Thus, intracellular Ca2+ concentration is decreased, which allows more Ca2+ from the lumen of the tubules to enter epithelial cells via apical Ca2+-selective channels (TRPV5). In other words, less Ca2+ in the cell increases the driving force for reabsorption from the lumen.[21]
Thiazides are also thought to increase the reabsorption of Ca2+ by a mechanism involving the reabsorption of sodium and calcium in the proximal tubule in response to sodium depletion. Some of this response is due to augmentation of the action of parathyroid hormone.[22]
Denomination
Thiazide refers to both the type of molecule[23] and the medication.[24] This can lead to confusion, because some molecules (thiazide-like diuretics) are often considered as thiazide diuretics, although they are not thiazides from a chemical perspective. In this context, "thiazide" refers to a drug which acts at a "thiazide receptor",[25] which is a sodium-chloride symporter.
Breast milk
Thiazides pass into breast milk, and can decrease the flow of breast milk.[26] Thiazides are classed as 'Drugs That Have Been Associated With Significant Effects on Some Nursing Infants and Should Be Given to Nursing Mothers With Caution' by the American Academy of Pediatrics Committee on Drugs.[27]
History
The thiazide diuretics were developed by scientists Karl H. Beyer, James M. Sprague, John E. Baer, and Frederick C. Novello of Merck and Co. in the 1950s,[4] and led to the marketing of the first drug of this class, chlorothiazide, under the trade name Diuril in 1958.[28] The research leading to the discovery of chlorothiazide, leading to "the saving of untold thousands of lives and the alleviation of the suffering of millions of victims of hypertension" was recognized by a special Public Health Award from the Lasker Foundation in 1975.[29]
References
- ^ Thiazides at the U.S. National Library of Medicine Medical Subject Headings (MeSH)
- ^ Thiazide+Diuretics at the U.S. National Library of Medicine Medical Subject Headings (MeSH)
- ^ Wright JM, Musini VM (July 2009). Wright, James M (ed.). "First-line drugs for hypertension". Cochrane Database Syst Rev. 8 (3): CD001841. doi:10.1002/14651858.CD001841.pub2. PMID 19588327.
- ^ a b Beyer KH (1993). "Chlorothiazide. How the thiazides evolved as antihypertensive therapy" (PDF). Hypertension. 22 (3): 388–91. doi:10.1161/01.hyp.22.3.388. PMID 8349332.
- ^ Whitworth JA, World Health Organization, International Society of Hypertension Writing Group (November 2003). "2003 World Health Organization (WHO)/International Society of Hypertension (ISH) statement on management of hypertension". J Hypertens. 21 (11): 1983–92. doi:10.1097/00004872-200311000-00002. PMID 14597836.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Musini VM, Nazer M, Bassett K, Wright JM (2014). "Blood pressure-lowering efficacy of monotherapy with thiazide diuretics for primary hypertension". Cochrane Database Syst Rev. 5: CD003824. doi:10.1002/14651858.CD003824.pub2. PMID 24869750.
- ^ Moser, Marvin; Feig, Peter U. (2009). "Symbiotic Fifty Years of Thiazide Diuretic Therapy for Hypertension". Arch Intern Med. 169 (20). JAMA: 1851–1856. doi:10.1001/archinternmed.2009.342. Retrieved August 14, 2014.
- ^ "2014 Evidence-Based Guideline for the Management of High Blood Pressure in Adults - Report From the Panel Members Appointed to the Eighth Joint National Committee (JNC 8)". Retrieved 4 November 2017.
- ^ "escardio.org". Archived from the original on 2008-05-17. Retrieved 2007-08-30.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ National Institute for Health and Clinical Excellence (NICE) guideline on the management of primary hypertension in adults (CG127) accessed 5/3/2012 at "Archived copy". Archived from the original on 2012-01-31. Retrieved 2012-03-05.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help)CS1 maint: archived copy as title (link) - ^ Guide to management of hypertension 2008. National Heart Foundation Australia. 2008. accessed online at "Archived copy" (PDF). Archived from the original (PDF) on 2013-05-15. Retrieved 2013-07-10.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help)CS1 maint: archived copy as title (link) - ^ Hughes AD (2004). "How do thiazide and thiazide-like diuretics lower blood pressure?". J Renin Angiotensin Aldosterone Syst. 5 (4): 155–60. doi:10.3317/jraas.2004.034. PMID 15803433.
- ^ Zhu Z, Zhu S, Liu D, Cao T, Wang L, Tepel M (2005). "Thiazide-like diuretics attenuate agonist-induced vasoconstriction by calcium desensitisation linked to Rho kinase". Hypertension. 45 (2): 233–9. doi:10.1161/01.HYP.0000152701.97426.5f. PMID 15611360.
- ^ Aung K, Htay T. Thiazide diuretics and the risk of hip fracture. Cochrane Database of Systematic Reviews 2011, Issue 10. Art. No.: CD005185. DOI: 10.1002/14651858.CD005185.pub2.
- ^ Dvorak MM, De Joussineau C, Carter DH, et al. (2007). "Thiazide diuretics directly induce osteoblast differentiation and mineralized nodule formation by interacting with a sodium chloride co-transporter in bone". J. Am. Soc. Nephrol. 18 (9): 2509–16. doi:10.1681/ASN.2007030348. PMC 2216427. PMID 17656470.
- ^ http://www.medscape.com/viewarticle/421426
- ^ a b "Archived copy". Archived from the original on 2010-10-09. Retrieved 2010-05-14.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help)CS1 maint: archived copy as title (link) - ^ http://www.merck.com/mmpe/sec18/ch261/ch261k.html
- ^ Dowd, Frank J; Johnson, Bart; Mariotti, Angelo (3 September 2016). Pharmacology and Therapeutics for Dentistry - E-Book. Elsevier Health Sciences. pp. 324–326. ISBN 9780323445955. Retrieved 4 November 2017.
- ^ Duarte JD, Cooper-DeHoff RM (June 2010). "Mechanisms for blood pressure lowering and metabolic effects of thiazide and thiazide-like diuretics". Expert Rev Cardiovasc Ther. 8 (6): 793–802. doi:10.1586/erc.10.27. PMC 2904515. PMID 20528637.
- ^ Longo, Dan L; et al. (2012). Harrison's Principals of Internal Medicine, Vol. 2. New York: McGraw-Hill. p. 2285. ISBN 978-0-07-174887-2.
- ^ Longo, Dan L; et al. (2012). Harrison's Principals of Internal Medicine, Vol. 2. New York: McGraw-Hill. p. 3109. ISBN 978-0-07-174887-2.
- ^ Thiazides at the U.S. National Library of Medicine Medical Subject Headings (MeSH)
- ^ Thiazide+Diuretics at the U.S. National Library of Medicine Medical Subject Headings (MeSH)
- ^ thiazide+receptor at the U.S. National Library of Medicine Medical Subject Headings (MeSH)
- ^ Gerald G. Briggs; Roger K. Freeman; Sumner J. Yaffe (2011). Drugs in Pregnancy and Lactation: A Reference Guide to Fetal and Neonatal Risk. Lippincott Williams & Wilkins. pp. 257–. ISBN 978-1-60831-708-0.
- ^ "Transfer of drugs and other chemicals into human milk". Pediatrics. 108 (3): 776–89. September 2001. PMID 11533352.
- ^ "Drugs@FDA: FDA Approved Drug Products".
- ^ "The Lasker Foundation - Awards".
