Methylphenidate: Difference between revisions
mNo edit summary |
|||
| Line 44: | Line 44: | ||
===Attention deficit hyperactivity disorder=== |
===Attention deficit hyperactivity disorder=== |
||
Methylphenidate is approved by the FDA for the treatment of [[attention-deficit hyperactivity disorder]]<ref>{{cite journal | author = Fone KC | coauthors = Nutt DJ. | year = 2005 | month = February | title = Stimulants: use and abuse in the treatment of attention deficit disorder. | journal = Current opinion in pharmacology. | volume = 5 | issue = 1 | pages = 87–93 | pmid = 15661631 | doi = 10.1016/j.coph.2004.10.001}}</ref> The addition of [[behavioural modification therapy]] (e.g. [[CBT]]) has additional benefits on treatment outcome.<ref>{{cite journal |author=Capp PK, Pearl PL, Conlon C |title=Methylphenidate HCl: therapy for attention deficit hyperactivity disorder |journal=Expert Rev Neurother |volume=5 |issue=3 |pages=325–31 |year=2005 |month=May |pmid=15938665 |doi=10.1586/14737175.5.3.325 |url=http://www.expert-reviews.com/doi/abs/10.1586/14737175.5.3.325?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dncbi.nlm.nih.gov}}</ref><ref>{{cite journal |author=Greenfield B, Hechman L |title=Treatment of attention deficit hyperactivity disorder in adults |journal=Expert Rev Neurother |volume=5 |issue=1 |pages=107–21 |year=2005 |month=January |pmid=15853481 |doi=10.1586/14737175.5.1.107 |url=http://www.expert-reviews.com/doi/abs/10.1586/14737175.5.1.107?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dncbi.nlm.nih.gov}}</ref> There is a lack of evidence of the effectiveness in the long term of beneficial effects of methylphenidate with regard to learning and academic performance.<ref>{{cite journal |author=Swanson JM, Cantwell D, Lerner M, McBurnett K, Hanna G |title=Effects of stimulant medication on learning in children with ADHD |journal=J Learn Disabil |volume=24 |issue=4 |pages=219–30, 255 |year=1991 |month=April |pmid=1875157 |doi= |url=}}</ref> A [[meta analysis]] of the literature concluded that methylphenidate quickly and effectively reduces the signs and symptoms of ADHD in children under the age of 18 in the short term but found that this conclusion may be be biased due to the high number of low quality clinical trials in the literature. There have been no placebo controlled trials investigating the long term effectiveness of methylphenidate beyond 4 weeks thus the long term effectiveness of methylphenidate has not been scientifically demonstrated. Serious concerns of [[publication bias]] regarding the use of methylphenidate for ADHD has also been noted.<ref name="pmid11762571">{{cite journal |author=Schachter HM, Pham B, King J, Langford S, Moher D |title=How efficacious and safe is short-acting methylphenidate for the treatment of attention-deficit disorder in children and adolescents? A meta-analysis |journal=CMAJ |volume=165 |issue=11 |pages=1475–88 |year=2001 |month=November |pmid=11762571 |pmc=81663 |doi= |url=http://www.cmaj.ca/cgi/pmidlookup?view=long&pmid=11762571}}</ref> A diagnosis of ADHD must be confirmed and the benefits and risks and proper use of stimulants as well as alternative treatments should be discussed with the parent before [[stimulants]] are prescribed.<ref>{{cite journal |author=Morgan AM |title=Use of stimulant medications in children |journal=Am Fam Physician |volume=38 |issue=4 |pages=197–202 |year=1988 |month=October |pmid=3051976 |doi= |url=}}</ref> The dosage used can vary quite significantly from individual child to individual child with some children responding to quite low doses whereas other children require the higher dose range. The dose therefore should be titrated to an optimal level which achieves therapeutic benefit and minimal side effects.<ref>{{cite journal |author=Stevenson RD, Wolraich ML |title=Stimulant medication therapy in the treatment of children with attention deficit hyperactivity disorder |journal=Pediatr. Clin. North Am. |volume=36 |issue=5 |pages=1183–97 |year=1989 |month=October |pmid=2677938 |doi= |url=}}</ref> Therapy with methylphenidate does not and should not be indefinite. Weaning off periods to assess symptoms are recommended.<ref name="pmid11056411">{{cite journal |author=Kidd PM |title=Attention deficit/hyperactivity disorder (ADHD) in children: rationale for its integrative management |journal=Altern Med Rev |volume=5 |issue=5 |pages=402–28 |year=2000 |month=October |pmid=11056411 |doi= |url=http://www.thorne.com/altmedrev/.fulltext/5/5/402.pdf |format=PDF}}</ref> |
Methylphenidate is approved by the FDA for the treatment of [[attention-deficit hyperactivity disorder]]<ref>{{cite journal | author = Fone KC | coauthors = Nutt DJ. | year = 2005 | month = February | title = Stimulants: use and abuse in the treatment of attention deficit disorder. | journal = Current opinion in pharmacology. | volume = 5 | issue = 1 | pages = 87–93 | pmid = 15661631 | doi = 10.1016/j.coph.2004.10.001}}</ref> The addition of [[behavioural modification therapy]] (e.g. [[CBT]]) has additional benefits on treatment outcome.<ref>{{cite journal |author=Capp PK, Pearl PL, Conlon C |title=Methylphenidate HCl: therapy for attention deficit hyperactivity disorder |journal=Expert Rev Neurother |volume=5 |issue=3 |pages=325–31 |year=2005 |month=May |pmid=15938665 |doi=10.1586/14737175.5.3.325 |url=http://www.expert-reviews.com/doi/abs/10.1586/14737175.5.3.325?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dncbi.nlm.nih.gov}}</ref><ref>{{cite journal |author=Greenfield B, Hechman L |title=Treatment of attention deficit hyperactivity disorder in adults |journal=Expert Rev Neurother |volume=5 |issue=1 |pages=107–21 |year=2005 |month=January |pmid=15853481 |doi=10.1586/14737175.5.1.107 |url=http://www.expert-reviews.com/doi/abs/10.1586/14737175.5.1.107?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dncbi.nlm.nih.gov}}</ref> There is a lack of evidence of the effectiveness in the long term of beneficial effects of methylphenidate with regard to learning and academic performance.<ref>{{cite journal |author=Swanson JM, Cantwell D, Lerner M, McBurnett K, Hanna G |title=Effects of stimulant medication on learning in children with ADHD |journal=J Learn Disabil |volume=24 |issue=4 |pages=219–30, 255 |year=1991 |month=April |pmid=1875157 |doi= |url=}}</ref> A [[meta analysis]] of the literature concluded that methylphenidate quickly and effectively reduces the signs and symptoms of ADHD in children under the age of 18 in the short term but found that this conclusion may be be biased due to the high number of low quality clinical trials in the literature. There have been no placebo controlled trials investigating the long term effectiveness of methylphenidate beyond 4 weeks thus the long term effectiveness of methylphenidate has not been scientifically demonstrated. Serious concerns of [[publication bias]] regarding the use of methylphenidate for ADHD has also been noted.<ref name="pmid11762571">{{cite journal |author=Schachter HM, Pham B, King J, Langford S, Moher D |title=How efficacious and safe is short-acting methylphenidate for the treatment of attention-deficit disorder in children and adolescents? A meta-analysis |journal=CMAJ |volume=165 |issue=11 |pages=1475–88 |year=2001 |month=November |pmid=11762571 |pmc=81663 |doi= |url=http://www.cmaj.ca/cgi/pmidlookup?view=long&pmid=11762571}}</ref> A diagnosis of ADHD must be confirmed and the benefits and risks and proper use of stimulants as well as alternative treatments should be discussed with the parent before [[stimulants]] are prescribed.<ref>{{cite journal |author=Morgan AM |title=Use of stimulant medications in children |journal=Am Fam Physician |volume=38 |issue=4 |pages=197–202 |year=1988 |month=October |pmid=3051976 |doi= |url=}}</ref> The dosage used can vary quite significantly from individual child to individual child with some children responding to quite low doses whereas other children require the higher dose range. The dose therefore should be titrated to an optimal level which achieves therapeutic benefit and minimal side effects.<ref>{{cite journal |author=Stevenson RD, Wolraich ML |title=Stimulant medication therapy in the treatment of children with attention deficit hyperactivity disorder |journal=Pediatr. Clin. North Am. |volume=36 |issue=5 |pages=1183–97 |year=1989 |month=October |pmid=2677938 |doi= |url=}}</ref> Therapy with methylphenidate does not and should not be indefinite. Weaning off periods to assess symptoms are recommended.<ref name="pmid11056411">{{cite journal |author=Kidd PM |title=Attention deficit/hyperactivity disorder (ADHD) in children: rationale for its integrative management |journal=Altern Med Rev |volume=5 |issue=5 |pages=402–28 |year=2000 |month=October |pmid=11056411 |doi= |url=http://www.thorne.com/altmedrev/.fulltext/5/5/402.pdf |format=PDF}}</ref> It is viewed by many governing bodies of major sporting associations that methylphenidate can combine with Claritin D ''in vivo'' to form substances similar in both structure and pharmacological effect to amphetamines. Case in point: Nascar's indefinate suspension and recent reinstatement of little known driver Jeremy Mayfield in the Sprint Cup series. |
||
===Narcolepsy=== |
===Narcolepsy=== |
||
Revision as of 04:46, 31 May 2009
 | |
 | |
| Clinical data | |
|---|---|
| Pregnancy category |
|
| Routes of administration | Oral, Transdermal, IV, Nasal |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | 11–52% |
| Protein binding | 30% |
| Metabolism | Liver |
| Elimination half-life | 2–4 hours |
| Excretion | Urine |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.003.662 |
| Chemical and physical data | |
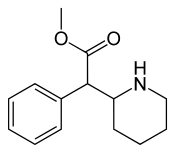
| Formula | C14H19NO2 |
| Molar mass | 233.31 g/mol g·mol−1 |
| 3D model (JSmol) | |
| |
Methylphenidate[2] (MPH) is the most commonly prescribed psychostimulant and is indicated in the treatment of attention-deficit hyperactivity disorder, Postural Orthostatic Tachycardia Syndrome and narcolepsy, although off-label uses include treating lethargy, depression, neural insult and obesity. In North America it is most commonly known as the brand name Ritalin, which is an instant-release racemic mixture, although a variety of brand names and formulations exist.[3] Methylphenidate is a potent central nervous system stimulant derived from amphetamine thought to exert its effect by enhancing dopaminergic transmission in the brain.[4][5][6][7]
History
Methylphenidate was patented in 1954 by the CIBA pharmaceutical company (now Novartis) as a potential cure for Mohr's disease.[citation needed] Beginning in the 1960s, it was used to treat children with ADHD or ADD, known at the time as hyperactivity or minimal brain dysfunction (MBD). Today methylphenidate is the most commonly prescribed medication to treat ADHD around the world.[citation needed] Production and prescription of methylphenidate rose significantly in the 1990s, especially in the United States, as the ADHD diagnosis came to be better understood and more generally accepted within the medical and mental health communities.[8]
Most brand-name Ritalin is produced in the United States, and methylphenidate is produced in the United States, Mexico, Argentina and Pakistan. Other generic forms, such as "methylin", are produced by several U.S. pharmaceutical companies. Ritalin is also sold in the United Kingdom, Germany and other European countries (although in much lower volumes than in the United States). These generic versions of methylphenidate tend to outsell brand-name Ritalin four to one.[citation needed] In Belgium the product is sold under the name "Rilatine" and in Portugal as "Ritalina".
Another medicine is Concerta, a once-daily extended-release form of methylphenidate, which was approved in April 2000. Studies have demonstrated that long-acting methylphenidate preparations such as Concerta are just as effective, if not more effective, than IR (instant release) formulas.[9][10][11][12] Time-release medications are also less prone to misuse[citation needed]
In April 2006, the U.S. Food and Drug Administration (FDA) approved a transdermal patch for the treatment of ADHD called Daytrana.[13]
Therapeutic uses

Methylphenidate is the most commonly prescribed psychostimulant and works by increasing the activity of the central nervous system.[14] It produces such effects as increasing or maintaining alertness, combating fatigue, and improving attention.[9] The benefits and cost effectiveness of methylphenidate long term are unknown due to a lack of research.[15][16] The long term effects of methylphenidate on the developing brain are unknown. Methylphenidate is not approved for children under six years of age.[17][18]
Attention deficit hyperactivity disorder
Methylphenidate is approved by the FDA for the treatment of attention-deficit hyperactivity disorder[19] The addition of behavioural modification therapy (e.g. CBT) has additional benefits on treatment outcome.[20][21] There is a lack of evidence of the effectiveness in the long term of beneficial effects of methylphenidate with regard to learning and academic performance.[22] A meta analysis of the literature concluded that methylphenidate quickly and effectively reduces the signs and symptoms of ADHD in children under the age of 18 in the short term but found that this conclusion may be be biased due to the high number of low quality clinical trials in the literature. There have been no placebo controlled trials investigating the long term effectiveness of methylphenidate beyond 4 weeks thus the long term effectiveness of methylphenidate has not been scientifically demonstrated. Serious concerns of publication bias regarding the use of methylphenidate for ADHD has also been noted.[23] A diagnosis of ADHD must be confirmed and the benefits and risks and proper use of stimulants as well as alternative treatments should be discussed with the parent before stimulants are prescribed.[24] The dosage used can vary quite significantly from individual child to individual child with some children responding to quite low doses whereas other children require the higher dose range. The dose therefore should be titrated to an optimal level which achieves therapeutic benefit and minimal side effects.[25] Therapy with methylphenidate does not and should not be indefinite. Weaning off periods to assess symptoms are recommended.[26] It is viewed by many governing bodies of major sporting associations that methylphenidate can combine with Claritin D in vivo to form substances similar in both structure and pharmacological effect to amphetamines. Case in point: Nascar's indefinate suspension and recent reinstatement of little known driver Jeremy Mayfield in the Sprint Cup series.
Narcolepsy
Narcolepsy, a chronic sleep disorder characterized by overwhelming daytime drowsiness and sudden attacks of sleep, is treated primarily with stimulants. Methylphenidate is considered effective in increasing wakefulness, vigilance, and performance.[27] Methylphenidate improves measures of somnolence on standardized tests, such as the Multiple Sleep Latency Test, but performance does not improve to levels comparable to healthy controls.[28]
Adjunctive
Use of stimulants such as methylphenidate in cases of refractory depression is controversial.[29] In individuals with cancer, methylphenidate is commonly used to counteract opioid-induced somnolence, to increase the analgesic effects of opioids, to treat depression, and to improve cognitive function.[30] Methylphenidate may be used in addition to an antidepressant for treatment-refractory major depressive disorder. It can also improve depression in several groups including stroke, cancer, HIV-positive patients.[31] However, benefits tend to be only partial with stimulants being generally less effective than traditional antidepressants and there is some suggestive evidence of a risk of habituation. Stimulants may however, have fewer side effects than tricyclic antidepressants in the elderly and medically ill.[32] A review of the literature found that methylphenidate was ineffective for refractory cases of major depression.[33]
Substance dependence
Methylphenidate has shown some benefits as a replacement therapy for methamphetamine addicts.[34] Methylphenidate and amphetamine have been investigated as a chemical replacement for the treatment of cocaine dependence[35][36][37] in the same way that methadone is used as a replacement for heroin. Its effectiveness in treatment of cocaine or other psychostimulant dependence has not been proven and further research is needed.[38]
Early research began in 2007-8 in some countries on the effectiveness of methylphenidate as a substitute agent in refractory cases of cocaine dependence; the fact that it can satisfy cravings for cocaine in a way which is subjectively and pharmacologically equivalent but longer-lasting as well as easier on the body and somewhat safer and easier to manage has long been part of the 'street lore' associated with stimulants in many parts of the world in much the same way that other substitutionmittel drugs such as methadone, buprenorphine, LAAM, butorphanol, extended-release oral morphine, dihydrocodeine, and clonidine were amongst opioid users in various times over the past century.[clarification needed]
Pervasive developmental disorders
Given the high co-morbidity between ADHD and autism, a few studies have examined the efficacy and effectiveness of methylphenidate in the treatment of autism. However, most of these studies examined the effects of methylphenidate on attention and hyperactivity symptoms among kids with autism spectrum disorders. Aman and Langworthy (2000) attempted to examine the effects of methylphenidate on social-communication and self-regulation behaviors among kids with ASDs.[39]
The sample included 33 children with pervasive developmental disorder (29 boys) with a mean age of 6.93 years (range 5-13). This was a 4-week randomized, double-blind, cross-over placebo study, with treatment changing each week between 4 conditions: placebo, low dose, medium dose, and high dose. In this design, neither the experimenters nor the families know which of the 4 treatments the child is receiving at any given time. In addition, the treatment condition changes randomly each week, without anyone knowing the nature of the old or new condition. This allows the experimenters to assume that consistent changes in behaviors that occur during a particular treatment is truly due to the effect of that treatment and not to the expectation of the treatment (placebo effect).
The results indicate that children showed significantly more joint attention behaviors when receiving methylphenidate than when receiving the placebo (although the most effective dosage varied by individual). Furthermore, at a group level, the low dose of methylphenidate resulted in significantly improved joint attention behaviors when compared to the placebo, but no differences were noted between the low, medium, and high doses. Low and medium doses of methylphenidate also resulted in improved self-regulation behavior when compared to placebo.
The study presents compelling preliminary evidence suggesting that methylphenidate is effective in improving some social behaviors among children with autism spectrum disorders.[40]
Investigational
Animal studies using rats with ADHD like behaviours were used to assess the safety of methylphenidate on the developing brain and found that psychomotor impairments, structural and functional parameters of the dopaminergic system were improved with treatment. This animal data suggests that methylphenidate supports brain development and hyperactivity in children diagnosed with ADHD. However, in normal control animals methylphenidate caused long lasting changes to the dopaminergic system suggesting that if a child is misdiagnosed with ADHD they may be at risk of long lasting adverse effects to brain development. Animal tests found that rats given methylphenidate grew up to be more stressful and emotional. It is unclear due to lack of followup study whether this occurs in ADHD like animals and whether it occurs in humans.[41] However, long lasting benefits of stimulant drugs have not been found in humans.[42]
Methylphenidate may reduce the risk of falls in older adults by treating cognitive deficits associated with aging and disease.[43]
Delivery formulations

All media are in milligrams.
Tablet
- Ritalin: 5, 10 or 20 mg tablets.
- Ritalin SR: 20 mg controlled-release tablets.
- Attenta: 10 mg tablets.
- Methylin: 5, 10 or 20 mg tablets.
- Methylin ER: 10 and 20 mg controlled-release tablets.
- Metadate ER: 10 and 20 mg controlled-release tablets.
- Equasym: 5, 10, 20 or 30 mg tablets.
- Rubifen: 5, 10 or 20 mg tablets.
Capsules
- Ritalin LA: 10, 20, 30 or 40 mg controlled-release capsules.
- Metadate CD: 10, 20, 30, 40, 50 or 60 mg controlled-release capsules.
- Biphentin: 10, 15, 30, 40, or 60 mg suspended release capsules.
Patches
- Daytrana 10, 15, 20 or 30 mg controlled-release patches (1.1, 1.6, 2.2 or 3.3 mg/hour for 9 hours).
Adverse effects
Some adverse effects may emerge during chronic use of methylphenidate so a constant watch for adverse effects is recommended.[46] Some adverse effects of stimulant therapy may emerge during long term therapy but there is very little research of the long term effects of stimulants.[47][48] The most common side effects of taking methylphenidate are nervousness and insomnia. Other reactions include pupil dilation[49], hypersensitivity (including skin rash, urticaria, fever, arthralgia, exfoliative dermatitis, erythema multiforme with histopathological findings of necrotizing vasculitis, and thrombocytopenic purpura); anorexia; nausea; dizziness; palpitations; growth retardation, headache; dyskinesia; drowsiness; blood pressure and pulse changes, both up and down; tachycardia; angina; cardiac arrhythmia; abdominal pain; addiction and drug dependence, suicidal thoughts, personality changes, and weight loss during prolonged therapy. Very rare effects include reports of Tourette's syndrome, seizures, toxic psychosis, and neuroleptic malignant syndrome.[26][50][51] Sudden death due to cardiotoxicity occurs in between 1.3 to 8.5 per 100,000 person-year.[52]
Known or suspected risks to health
Researchers have also looked into the role of methylphenidate in affecting stature, with some studies finding slight decreases in height acceleration.[53] Other studies indicate height may normalize by adolescence.[54][55] In a 2005 study, only "minimal effects on growth in height and weight were observed" after 2 years of treatment. "No clinically significant effects on vital signs or laboratory test parameters were observed."[56]
A 2003 study tested the effects of dextromethylphenidate (Focalin), levomethylphenidate, and (racemic) detro-, levomethylphenidate (Ritalin) on mice to search for any carcinogenic effects. The researchers found that all three preparations were non-genotoxic and non-clastogenic; d-MPH, d, l-MPH, and l-MPH did not cause mutations or chromosomal aberrations. They concluded that none of the compounds present a carcinogenic risk to humans.[57] Current scientific evidence supports that long-term methylphenidate treatment does not increase the risk of developing cancer in humans.[58]
The use of ADHD medication in children under the age of 6 has not been studied. Severe hallucinations may occur. ADHD symptoms include hyperactivity and difficulty holding still and following directions; these are also characteristics of a typical child under the age of 6. For this reason it may be more difficult to diagnose young children, and caution should be used with this age group.[citation needed]
However, it was documented in 2000, by Zito et al. [59][60]“that at least 1.5% of children between the ages of two and four are medicated with stimulants, anti-depressants and anti-psychotic drugs, despite the paucity of controlled scientific trials confirming safety and long-term effects with preschool children.”
On March 22, 2006 the FDA Pediatric Advisory Committee decided that medications using methylphenidate ingredients do not need black box warnings about their risks, noting that "for normal children, these drugs do not appear to pose an obvious cardiovascular risk."[61] Previously, 19 possible cases had been reported of Cardiac arrest linked to children taking methylphenidate[62] and the Drug Safety and Risk Management Advisory Committee to the FDA recommend a "black-box" warning in 2006 for stimulant drugs used to treat attention deficit/hyperactivity disorder.[63]
Doses prescribed of stimulants above the recommended dose level is associated with higher levels of psychosis, substance misuse and psychiatric admissions.[64]
Long term effects
The effects of long-term methylphenidate treatment on the developing brains of children with ADHD is the subject of study and debate.[65][66] Although the safety profile of short-term methylphenidate therapy in clinical trials has been well established, repeated use of psychostimulants such as methylphenidate is less clear. The long term effects of methylphenidate such as drug addiction, withdrawal reactions, psychosis and depression and effects in pregnancy has received very little research and thus the long term effects of using stimulants for ADHD are largely unknown. There are no well defined withdrawal schedules for discontinuing long term use of stimulants.[67] There is limited data which suggests that there may be modest benefits in correctly diagnosed children with ADHD but there are also overall modest risks.[68] Short term clinical trials lasting a few weeks show an incidence of psychosis of about 0.1%.[50] A small study of just under 100 children which assessed long term outcome of stimulant use found that 6% of children became psychotic often months or years of stimulant therapy. Typically psychosis would abate soon after stopping stimulant therapy. As the study size was small larger studies have been recommended.[69] The long term effects on mental health disorders in later life of chronic use of methylphenidate is unknown.[70] Concerns have been raised that long-term therapy might cause drug dependence, paranoia, schizophrenia and behavioral sensitisation, similar to other stimulants.[71] Psychotic symptoms from methylphenidate can include, hearing voices, visual hallucinations, urges to harm oneself, severe anxiety, euphoria, grandiosity, paranoid delusions, confusion, increased aggression and irritability. Methylphenidate psychosis is unpredictable in who it will occur. Family history of mental illness does not predict the incidence of stimulant toxicosis in ADHD children. High rates of childhood stimulant use is found in patients with a diagnosis of schizophrenia and bipolar disorder independent of ADHD. Individuals with a diagnosis of bipolar or schizophrenia who were prescribed stimulants during childhood typically have a significantly earlier onset of the psychotic disorder and suffer a more severe clinical course of psychotic disorder.[72][73][74] Knowledge of the effects of chronic use of methylphenidate is poorly understood with regard to persisting behavioral and neuroadaptational effects.[75]
Tolerance and behavioural sensitisation may occur with long term use of methylphenidate.[76] There is also cross tolerance with other stimulants such as amphetamines and cocaine.[77] Stimulant withdrawal or rebound reactions can occur and should be minimised in intensity, i.e. via a gradual tapering off of medication over a period of weeks or months.[78][79][80] A very small study of abrupt withdrawal of stimulants did suggest that withdrawal reactions are not typical. Nonetheless withdrawal reactions may still occur in susceptible individuals.[81] The withdrawal or rebound symptoms of methylphenidate can include psychosis, depression, irritability and a temporary worsening of the original ADHD symptoms. Methylphenidate due to its very short elimination half life may be more prone to rebound effects than d-amphetamine.[26][82][83] Up to a third of ADHD children experience a rebound effect when methylphenidate dose wears off.[84]
Contraindications
Methylphenidate should not be prescribed concomitantly with tricyclic antidepressants, such as desipramine, or monoamine oxidase inhibitors, such as phenelzine or tranylcypromine, as methylphenidate may dangerously increase plasma concentrations, leading to potential toxic reactions (mainly, cardiovascular effects). Methylphenidate should not be prescribed to patients who suffer from severe arrhythmia, hypertension or liver damage. It shouldn't be prescribed to patients who demonstrate drug-seeking behaviour, pronounced agitation or nervousness.[26] Care should be taken while prescribing methylphenidate to children with a family history of Paroxysmal Supraventricular Tachycardia(PSVT).
Special precautions
Special precaution is recommended in individuals with epilepsy with additional caution in individuals with uncontrolled epilepsy due to the potential for methylphenidate to lower the seizure threshold..[85]
Interactions
Intake of adrenergic agonist drugs or pemoline with methylphenidate increases the risk of liver toxicity.[86][87] Antidepressants taken in conjunction with methylphenidate may cause hypertension, hypothermia and convulsions.[26] When methylphenidate is coingested with ethanol, a metabolite called ethylphenidate is formed via hepatic transesterification.[88][89] Coinjestion of alcohol (ethanol) also increases the blood plasma levels of d-methylphenidate by up to 40%.[76] It is more selective to the dopamine transporter (DAT) than methylphenidate, having approximately the same efficacy as the parent compound,[90] but has significantly less activity on the norepinephrine transporter (NET).[91]
Pregnancy
Use of methylphenidate during pregnancy is not recommended as there is some evidence of developmental effects, particularly neurobehavioral alterations.[92]
Overdose
In 2004, over 8000 methylphenidate ingestions were reported in US poison center data.[93] The most common reasons for intentional exposure were drug abuse and suicide attempts.[94] An overdose manifests in agitation, hallucinations, psychosis, lethargy, seizures, tachycardia, dysrhythmias, hypertension, and hyperthermia.[95] Benzodiazepines may be used as treatment if agitation, dystonia, or convulsions are present.[93]
Pharmacology
Methylphenidate is a ring-subsituted amphetamine derivative which exerts its pharmacological effects via stimulating the release and blocking the reuptake of catecholamines.[96][97] Methylphenidate is most active in effecting levels of the catecholamine called dopamine and to a lesser extent noradrenaline.[98][99]
Pharmacokinetics
Methylphenidate has binding affinity for both the dopamine transporter and norepinephrine transporter, with the dextromethylphenidate enantiomers displaying a prominent affinity for the norepinephrine transporter. Both the dextro- and levorotary enantiomers displayed receptor affinity for the serotonergic 5HT1A and 5HT2B subtypes, though direct binding to the serotonin transporter was not observed.[100]
The enantiomers and the relative psychoactive effects and CNS stimulation of dextro- and levo-methylphenidate is analogous to what is found in amphetamine, where dextro-amphetamine is considered to have a greater psychoactive and CNS stimulatory effect than levo-amphetamine.
Pharmacodynamics
Methylphenidate exerts its therapeutic effects via blocking the reuptake of dopamine into nerve terminals as well as stimulating the release of dopamine from dopamine nerve terminals resulting in increased dopamine levels in the synapse. Actually, Methylphenidate blocks reuptake, but does not help release dopamine, which is a property of amphetamines.[101] The onset of central nervous system effects occurs rapidly after intake of methylphenidate and persist for about 4 hours.[102] The mechanism of action and chemical structure of methylphenidate is extremely similar to cocaine with usual doses of both drugs occupy 50% of dopamine transporters. However, cocaine effects such as euphoria are rare at doses prescribed clinically.[103][104][105][106]
The means by which methylphenidate affects people diagnosed with ADHD are not well understood. Some researchers have theorized that ADHD is caused by a dopamine imbalance in the brains of those affected. Methylphenidate is a norepinephrine and dopamine reuptake inhibitor, which means that it increases the level of the dopamine neurotransmitter in the brain by partially blocking the dopamine transporter (DAT) that removes dopamine from the synapses.[107] This inhibition of DAT blocks the reuptake of dopamine and norepinephrine into the presynaptic neuron, increasing the amount of dopamine in the synapse. It also stimulates the release of dopamine and norepinephrine into the synapse [citation needed]. Finally, it increases the magnitude of dopamine release after a stimulus, increasing the salience of stimulus. An alternate explanation which has been explored is that the methylphenidate affects the action of serotonin in the brain.[108] However, benefits with other stimulants which have a different mechanism of action indicates that support for a deficit in specific neurotransmitters is unsupported and unproven by the evidence and remains a speculative hypothesis.[109]
It is commonly asked why a stimulant should be used to treat hyperactivity, which seems paradoxical. However, MRIs of ADHD brains show decreased activity in the brain centers critical to concentration and goal-directed activities.[110] Treatment with methylphenidate (etc.) results in increased activity in those regions, in ADHD patients, and in healthy controls as well. Thus the model explanation is that hyperactive children (and adults) have underactive concentration centers, and stimulating them reduces hyperactivity. Thus the stimulants do not work paradoxically. They stimulate portions of the brain that are underactive by increasing dopamine and norepinephrine in the striatum and prefontal cortex.
One study finds that methylphenidate reduces the increases in brain glucose metabolism during performance of a cognitive task by about 50%. This suggests that, similar to increasing dopamine and norepinephrine in the striatum and prefrontal cortex, methylphenidate may focus activation of certain regions and make the brain more efficient. This is consistent with the observation that stimulant drugs can enhance attention and performance in some individuals. If brain resources are not optimally distributed (for example, in individuals with ADHD or sleep deprivation), improved performance could be achieved by reducing task-induced regional activation. Stimulant delivery when brain resources are already optimally distributed may then adversely affect performance.[111]
A paper published in Biological Psychiatry reports that methylphenidate fine-tunes the functioning of neurons in the prefrontal cortex - a brain region involved in attention, decision-making and impulse control - while having few effects outside it. The team studied PFC neurons in rats under a variety of methylphenidate doses, including one that improved the animals' performance in a working memory task of the type that ADHD patients have trouble completing. Using microelectrodes, the scientists observed both the random, spontaneous firings of PFC neurons and their response to stimulation of the hippocampus. When they listened to individual PFC neurons, the scientists found that while cognition-enhancing doses of methylphenidate had little effect on spontaneous activity, the neurons' sensitivity to signals coming from the hippocampus increased dramatically. Under higher, stimulatory doses, on the other hand, PFC neurons stopped responding to incoming information.[112]
Abuse potential
Methylphenidate is a drug of abuse.[113] Methylphenidate like other stimulants increases dopamine levels but at therapeutic doses the increase is slow and thus euphoria does not typically occur except in rare instances. The abuse potential is increased when methylphenidate is crushed and snorted or when it is injected producing effects almost identical to cocaine. Cocaine like effects can also occur with very large doses taken orally. The dose however, which produces euphoric effects varies between individuals. Methylphenidate is actually more potent than cocaine in its effect on dopamine transporters. Methylphenidate should not be viewed as a weak stimulant as has previously been hypothesised.[114] The primary source for methylphenidate for abuse is diversion from legitimate prescriptions rather than illicit synthesis. Those who use to stay awake do so by taking it orally, while intranasal and intravenous are the preferred means for inducing euphoria.[95] IV users tend to be adults whose use may cause panlobular pulmonary emphysema.[94] Methylphenidate has a high potential for drug dependence and addictive abuse due to its similarity pharmaologically to cocaine and amphetamines.[26] Abuse of prescription stimulants is higher amongst college students than non-college attending young adults. College students misuse methylphenidate either as a study aid or to stay awake longer The increased alcohol consumption due to stimulant misuse has additional negative effects on health.[115]
Methylphenidate pharmacological effect on the central nervous system is almost identical to that of cocaine. Studies have shown that the two drugs are nearly indistinguishable when administered intravenously to cocaine addicts.[116][117] However, cocaine has a slightly higher affinity for the dopamine receptor in comparison to methylphenidate, which is thought to be the mechanism of the euphoria associated with the relatively short-lived cocaine high.[118] Controversy has surrounded whether methylphenidate is as commonly abused as other stimulants with many believing that its rate of abuse is much lower than other stimulants. However, the majority of studies assessing its abuse potential and drug liking scores have determined that it has a similar abuse potential as cocaine and d-amphetamine.[119] Reports of users experimenting with mixing methylphenidate with caffeine and benzocaine to produce a powder for insufflation for an even more cocaine-like effect began to appear in the middle 1970s; this is apparently an incrementation upon a mixture known as Toot containing phenylpropanolamine, caffeine, and benzocaine in the search for legal highs. As moderate doses of cocaine have caffeine-like effects and benzocaine produces a slight stimulant effect of its own perhaps 5 per cent the strength of cocaine with a ceiling in that range, the mixture is reported to have at least some of the sought effects.
Legal status
In the United States, methylphenidate is classified as a Schedule II controlled substance, the designation used for substances that have a recognized medical value but present a high likelihood for abuse because of their addictive potential. Internationally, methylphenidate is a Schedule II drug under the Convention on Psychotropic Substances.[120]
Controversy
Methylphenidate, usually referred to as the brand name Ritalin, has been related to controversy regarding the treatment of ADHD. Criticism generally revolves around alleged or established side effects, concerns of illicit use and abuse, and the ethics of giving psychotropic drugs to children to reduce ADHD symptoms.[121] There is growing concern of the widespread use of methylphenidate and its long term effects, which include concerns of life threatening effects. Calls have been made that methylphenidate be severely restricted in its use.[26] The pharmacological effects of methylphenidate, a schedule II drug are almost identical to cocaine and the amphetamines. The abuse pattern of methylphenidate is very similar to cocaine and amphetamines.[26] In 2002, a study showed that rats treated with methylphenidate are more receptive to the reinforcing effects of cocaine,[118] which seeded doubts if the medication is a gateway drug to substance abuse. However, this contention has since been discredited by multiple sources,[122][123] although uncertainity continues to exist.[124]
Controversy also surrounds whether ADHD is a disorder or a personality trait with some in the medical profession believing that it is a myth that hyperactivity is a disorder. They further point out that as a group ADHD children have in general healthy brains with no gross neurological deficits.[125]
Richard Bromfield claims that Ritalin is often prescribed not because of an underlying neurological disorder, but as an easy way to calm down children whose misbehavior actually results from ordinary causes such as bad parenting.[126]
Treatment of ADHD has led to legal actions including malpractice suits regarding informed consent, inadequate information on side effects, over or misdiagnosis and coersive use of medications by school systems.[127]
See also
- Ethylphenidate
- O-2172
- Psychoactive drug
- Steroid
- Amphetamine
- Methamphetamine
- Benzedrine
- Controversy about ADHD
- Pemoline
References
- ^ "FDA-sourced list of all drugs with black box warnings (Use Download Full Results and View Query links.)". nctr-crs.fda.gov. FDA. Retrieved 22 Oct 2023.
- ^ Pronunciation
- ^ Brand names also include Ritalina, Rilatine, Attenta (in Australia), Methylin, Penid, and Rubifen; and the sustained release tablets Concerta, Metadate CD, Methylin ER, Ritalin LA, and Ritalin-SR. Focalin is a preparation containing only dextro-methylphenidate, rather than the usual racemic dextro- and levo-methylphenidate mixture of other formulations. A newer way of taking methylphenidate is by using a transdermal patch (under the brand name Daytrana), similar to those used for nicotine replacement therapy.
- ^ Sharma RP, Javaid JI, Pandey GN, Easton M, Davis JM (1990). "Pharmacological effects of methylphenidate on plasma homovanillic acid and growth hormone". Psychiatry Res. 32 (1): 9–17. PMID 2190251.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Seifert J, Scheuerpflug P, Zillessen KE, Fallgatter A, Warnke A (2003). "Electrophysiological investigation of the effectiveness of methylphenidate in children with and without ADHD". J Neural Transm. 110 (7): 821–9. doi:10.1007/s00702-003-0818-8. PMID 12811642.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Auriel E, Hausdorff JM, Giladi N (2008). "Methylphenidate for the Treatment of Parkinson Disease and Other Neurological Disorders". Clin Neuropharmacol. doi:10.1097/WNF.0B013E318170576C. PMID 18978488.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Dadfarmay S, Dixon J (2009). "A case of acute cardiomyopathy and pericarditis associated with methylphenidate". Cardiovasc. Toxicol. 9 (1): 49–52. doi:10.1007/s12012-009-9033-7. PMID 19296063.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ "News from DEA, Congressional Testimony, 05/16/00". Retrieved 2007-11-02.
- ^ a b Steele, M., et al. (2006). "Template:PDFlink". Can J Clin Pharmacol. 2006 Winter;13(1):e50-62.
- ^ Pelham, W.E., et al. (2001). "Once-a-day Concerta methylphenidate versus three-times-daily methylphenidate in laboratory and natural settings". Pediatrics. 2001 Jun;107(6):E105.
- ^ Keating, G.M., McClellan, K., Jarvis, B. (2001). "Methylphenidate (OROS formulation)". CNS Drugs. 2001;15(6):495-500; discussion 501-3.
- ^ Hoare, P., et al. (2005). "Template:PDFlink". Eur Child Adolesc Psychiatry. 2005 Sep;14(6):305-9.
- ^ Peck, P. (2006, 7 April). FDA Approves Daytrana Transdermal Patch for ADHD. MedPage today. Retrieved April 7, 2006, from http://www.medpagetoday.com/ProductAlert/Prescriptions/tb/3027.
- ^ Markowitz JS, Logan BK, Diamond F, Patrick KS (1999). "Detection of the novel metabolite ethylphenidate after methylphenidate overdose with alcohol coingestion". J Clin Psychopharmacol. 19 (4): 362–6. doi:10.1097/00004714-199908000-00013. PMID 10440465.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Gilmore A, Milne R (2001). "Methylphenidate in children with hyperactivity: review and cost-utility analysis". Pharmacoepidemiol Drug Saf. 10 (2): 85–94. doi:10.1002/pds.564. PMID 11499858.
- ^ Mott TF, Leach L, Johnson L (2004). "Clinical inquiries. Is methylphenidate useful for treating adolescents with ADHD?". J Fam Pract. 53 (8): 659–61. PMID 15298843.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Vitiello B (2001). "Psychopharmacology for young children: clinical needs and research opportunities". Pediatrics. 108 (4): 983–9. PMID 11581454.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Hermens DF, Rowe DL, Gordon E, Williams LM (2006). "Integrative neuroscience approach to predict ADHD stimulant response". Expert Rev Neurother. 6 (5): 753–63. doi:10.1586/14737175.6.5.753. PMID 16734523.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Fone KC (2005). "Stimulants: use and abuse in the treatment of attention deficit disorder". Current opinion in pharmacology. 5 (1): 87–93. doi:10.1016/j.coph.2004.10.001. PMID 15661631.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ^ Capp PK, Pearl PL, Conlon C (2005). "Methylphenidate HCl: therapy for attention deficit hyperactivity disorder". Expert Rev Neurother. 5 (3): 325–31. doi:10.1586/14737175.5.3.325. PMID 15938665.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Greenfield B, Hechman L (2005). "Treatment of attention deficit hyperactivity disorder in adults". Expert Rev Neurother. 5 (1): 107–21. doi:10.1586/14737175.5.1.107. PMID 15853481.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Swanson JM, Cantwell D, Lerner M, McBurnett K, Hanna G (1991). "Effects of stimulant medication on learning in children with ADHD". J Learn Disabil. 24 (4): 219–30, 255. PMID 1875157.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Schachter HM, Pham B, King J, Langford S, Moher D (2001). "How efficacious and safe is short-acting methylphenidate for the treatment of attention-deficit disorder in children and adolescents? A meta-analysis". CMAJ. 165 (11): 1475–88. PMC 81663. PMID 11762571.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Morgan AM (1988). "Use of stimulant medications in children". Am Fam Physician. 38 (4): 197–202. PMID 3051976.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Stevenson RD, Wolraich ML (1989). "Stimulant medication therapy in the treatment of children with attention deficit hyperactivity disorder". Pediatr. Clin. North Am. 36 (5): 1183–97. PMID 2677938.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ a b c d e f g h Kidd PM (2000). "Attention deficit/hyperactivity disorder (ADHD) in children: rationale for its integrative management" (PDF). Altern Med Rev. 5 (5): 402–28. PMID 11056411.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Fry JM (1998). "Treatment modalities for narcolepsy". Neurology. 50 (2 Suppl 1): S43–8. PMID 9484423.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Mitler MM (1994). "Evaluation of treatment with stimulants in narcolepsy". Sleep. 17 (8 Suppl): S103–6. PMID 7701190.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Kraus MF, Burch EA (1992). "Methylphenidate hydrochloride as an antidepressant: controversy, case studies, and review". South. Med. J. 85 (10): 985–91. PMID 1411740.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Rozans M, Dreisbach A, Lertora JJ, Kahn MJ (2002). "Palliative uses of methylphenidate in patients with cancer: a review". J. Clin. Oncol. 20 (1): 335–9. doi:10.1200/JCO.20.1.335. PMID 11773187.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Leonard BE, McCartan D, White J, King DJ (2004). "Methylphenidate: a review of its neuropharmacological, neuropsychological and adverse clinical effects". Hum Psychopharmacol. 19 (3): 151–80. doi:10.1002/hup.579. PMID 15079851.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Satel SL, Nelson JC (1989). "Stimulants in the treatment of depression: a critical overview". J Clin Psychiatry. 50 (7): 241–9. PMID 2567730.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Schweitzer I, Tuckwell V, Johnson G (1997). "A review of the use of augmentation therapy for the treatment of resistant depression: implications for the clinician". Aust N Z J Psychiatry. 31 (3): 340–52. PMID 9226079.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Elkashef A, Vocci F, Hanson G, White J, Wickes W, Tiihonen J (2008). "Pharmacotherapy of methamphetamine addiction: an update" (PDF). Subst Abus. 29 (3): 31–49. PMC 2597382. PMID 19042205.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Grabowski J, Roache JD, Schmitz JM, Rhoades H, Creson D, Korszun A (1997). "Replacement medication for cocaine dependence: methylphenidate". J Clin Psychopharmacol. 17 (6): 485–8. doi:10.1097/00004714-199712000-00008. PMID 9408812.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Gorelick DA, Gardner EL, Xi ZX (2004). "Agents in development for the management of cocaine abuse". Drugs. 64 (14): 1547–73. PMID 15233592.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Karila L, Gorelick D, Weinstein A; et al. (2008). "New treatments for cocaine dependence: a focused review". Int. J. Neuropsychopharmacol. 11 (3): 425–38. doi:10.1017/S1461145707008097. PMID 17927843.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Shearer J (2008). "The principles of agonist pharmacotherapy for psychostimulant dependence". Drug Alcohol Rev. 27 (3): 301–8. doi:10.1080/09595230801927372. PMID 18368612.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Aman MG, Langworthy KS (2000). "Pharmacotherapy for hyperactivity in children with autism and other pervasive developmental disorders" (PDF). J Autism Dev Disord. 30 (5): 451–9. doi:10.1023/A:1005559725475. PMID 11098883.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ A review of: Laudan B. Jahromi, Connie L. Kasari, James T. McCracken, Lisa S-Y. Lee, Michael G. Aman, Christopher J. McDougle, Lawrence Scahill, Elaine Tierney, L. Eugene Arnold, Benedetto Vitiello, Louise Ritz, Andrea Witwer, Erin Kustan, Jaswinder Ghuman, David J. Posey (2008). Positive Effects of Methylphenidate on Social Communication and Self-Regulation in Children with Pervasive Developmental Disorders and Hyperactivity Journal of Autism and Developmental Disorders DOI: 10.1007/s10803-008-0636-9
- ^ Grund T., et al. "Influence of methylphenidate on brain development - an update of recent animal experiments", Behav Brain Funct. 2006 January 10;2:2.
- ^ Sagvolden T, Sergeant JA (1998). "Attention deficit/hyperactivity disorder--from brain dysfunctions to behaviour". Behav. Brain Res. 94 (1): 1–10. PMID 9708834.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ [1]
- ^ Full Prescribing Information for Concerta. (215 KiB)
- ^ Generic Concerta
- ^ Gordon N (1999). "Attention deficit hyperactivity disorder: possible causes and treatment". Int. J. Clin. Pract. 53 (7): 524–8. PMID 10692738.
- ^ King S, Griffin S, Hodges Z; et al. (2006). "A systematic review and economic model of the effectiveness and cost-effectiveness of methylphenidate, dexamfetamine and atomoxetine for the treatment of attention deficit hyperactivity disorder in children and adolescents". Health Technol Assess. 10 (23): iii–iv, xiii–146. PMID 16796929.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Gonzalez de Dios J, Cardó E, Servera M (2006). "[Methylphenidate in the treatment of attention-deficit/hyperactivity disorder: are we achieving an adequate clinical practice?]". Rev Neurol (in Spanish; Castilian). 43 (12): 705–14. PMID 17160919.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: unrecognized language (link) - ^ Jaanus SD (1992). "Ocular side effects of selected systemic drugs". Optom Clin. 2 (4): 73–96. PMID 1363080.
- ^ a b "Ritalin & Ritalin-SR Prescribing Information" (PDF). Novartis. 2007.
{{cite web}}: Unknown parameter|month=ignored (help) - ^ Matsudaira T (2007). "Attention deficit disorders--drugs or nutrition?". Nutr Health. 19 (1–2): 57–60. PMID 18309764.
- ^ Vitiello B (2008). "Understanding the risk of using medications for attention deficit hyperactivity disorder with respect to physical growth and cardiovascular function" (PDF). Child Adolesc Psychiatr Clin N Am. 17 (2): 459–74, xi. doi:10.1016/j.chc.2007.11.010. PMC 2408826. PMID 18295156.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Rao J.K., Julius J.R., Breen T.J., Blethen S.L. (1996). "Response to growth hormone in attention deficit hyperactivity disorder: effects of methylphenidate and pemoline therapy". Pediatrics. 1998 Aug;102 (2 Pt 3):497-500.
- ^ Spencer, T.J., et al. (1996)."Growth deficits in ADHD children revisited: evidence for disorder-associated growth delays?". J Am Acad Child Adolesc Psychiatry. 1996 Nov;35(11):1460-9.
- ^ Klein R.G. & Mannuzza S. (1988). "Hyperactive boys almost grown up. III. Methylphenidate effects on ultimate height". Arch Gen Psychiatry. 1988 Dec;45(12):1131-4.
- ^ Wilens, T., et al. (2005). ADHD treatment with once-daily OROS methylphenidate: final results from a long-term open-label study". J Am Acad Child Adolesc Psychiatry. 2005 Oct;44(10):1015-23.
- ^ Teo, S.K., et al. (2003). "D-Methylphenidate is non-genotoxic in vitro and in vivo assays". Mutat Res. 2003 May 9;537(1):67-79.
- ^ Walitza, Susanne (2007). "Does Methylphenidate Cause a Cytogenetic Effect in Children with Attention Deficit Hyperactivity Disorder?". Environmental Health Perspectives. 115 (6): 936–940. doi:10.1289/ehp.9866.
{{cite journal}}: Unknown parameter|authors=ignored (help); Unknown parameter|month=ignored (help) - ^ Brattler, Thomas Edward (2007). The Myth of ADHD and the Scandal of Ritalin: Helping John Dewey Students Succeed in Medicine-Free College Preparatory and Therapeutic High School. International Journal of Reality Therapy, XXVII (1), 4-13.
- ^ Zito, Julie Magno; Safer, Daniel J.; dos Reis, Susan; et al. (2000). Trends in the Prescribing of Psychotropic Medications to Preschoolers. Journal of American Medical Association, 283 (8),1025-1030.
- ^ Minutes of the FDA Pediatric Advisory Committee. March 22, 2006.
- ^ New Scientist 18 February 2006
- ^ Minutes of the FDA Pediatric Advisory Committee, March 22, 2006
- ^ Auger RR, Goodman SH, Silber MH, Krahn LE, Pankratz VS, Slocumb NL (2005). "Risks of high-dose stimulants in the treatment of disorders of excessive somnolence: a case-control study". Sleep. 28 (6): 667–72. PMID 16477952.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ "ADHD & Women's Health - Attention-deficit hyperactivity disorder National Women's Health Report". 2003. Retrieved 2007-11-03.
Although methylphenidate is perhaps one of the best-studied drugs available, with thousands of studies attesting to its longterm safety over the past 50 years, that hasn't stopped critics from raising alarms about the drug's long-term use on children's developing brains, particularly given research that finds the numbers of children taking the drug skyrocketing in recent years.
{{cite journal}}: Cite journal requires|journal=(help); Unknown parameter|month=ignored (help) - ^ Edmund J. S. Sonuga-Barke, Margaret Thompson, Howard Abikoff, Rachel Klein, Laurie Miller Brotman. "Nonpharmacological Interventions for Preschoolers With ADHD: The Case for Specialized Parent Training" (PDF). Infants & Young Children. 19 (2): 142–153. Retrieved 2008-12-30.
While most recent studies suggest that methylphenidate is relatively well-tolerated by young children, some suggest that side effects might be more marked in preschoolers than in school-aged children (Firestone, Musten, Pisterman, Mercer, & Bennett, 1998). Furthermore, some researchers have argued that there is the potential for negative long-term effects on the developing brains of young children chronically medicated (Moll, Rothenberger, Ruther, & Huther, 2002).
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Ashton H, Gallagher P, Moore B (2006). "The adult psychiatrist's dilemma: psychostimulant use in attention deficit/hyperactivity disorder". J. Psychopharmacol. (Oxford). 20 (5): 602–10. doi:10.1177/0269881106061710. PMID 16478756.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Kociancic T, Reed MD, Findling RL (2004). "Evaluation of risks associated with short- and long-term psychostimulant therapy for treatment of ADHD in children". Expert Opin Drug Saf. 3 (2): 93–100. doi:10.1517/eods.3.2.93.27337. PMID 15006715.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Cherland E, Fitzpatrick R (1999). "Psychotic side effects of psychostimulants: a 5-year review" (PDF). Can J Psychiatry. 44 (8): 811–3. PMID 10566114.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Kimko HC, Cross JT, Abernethy DR (1999). "Pharmacokinetics and clinical effectiveness of methylphenidate". Clin Pharmacokinet. 37 (6): 457–70. PMID 10628897.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Dafny N (15). "The role of age, genotype, sex, and route of acute and chronic administration of methylphenidate: A review of its locomotor effects". Brain research bulletin. 68 (6): 393–405. PMID 16459193.
{{cite journal}}: Check date values in:|date=and|year=/|date=mismatch (help); Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ^ Ross RG (2006). "Psychotic and manic-like symptoms during stimulant treatment of attention deficit hyperactivity disorder". Am J Psychiatry. 163 (7): 1149–52. doi:10.1176/appi.ajp.163.7.1149. PMID 16816217.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ DelBello MP, Soutullo CA, Hendricks W, Niemeier RT, McElroy SL, Strakowski SM (2001). "Prior stimulant treatment in adolescents with bipolar disorder: association with age at onset". Bipolar Disord. 3 (2): 53–7. PMID 11333062.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Soutullo CA, DelBello MP, Ochsner JE; et al. (2002). "Severity of bipolarity in hospitalized manic adolescents with history of stimulant or antidepressant treatment". J Affect Disord. 70 (3): 323–7. PMID 12128245.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Kuczenski R, Segal DS (2005). "Stimulant actions in rodents: implications for attention-deficit/hyperactivity disorder treatment and potential substance abuse". Biol. Psychiatry. 57 (11): 1391–6. doi:10.1016/j.biopsych.2004.12.036. PMID 15950013.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ a b Patrick KS, Straughn AB, Perkins JS, González MA (2009). "Evolution of stimulants to treat ADHD: transdermal methylphenidate" (PDF). Hum Psychopharmacol. 24 (1): 1–17. doi:10.1002/hup.992. PMC 2629554. PMID 19051222.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Leith NJ, Barrett RJ (1981). "Self-stimulation and amphetamine: tolerance to d and l isomers and cross tolerance to cocaine and methylphenidate". Psychopharmacology (Berl.). 74 (1): 23–8. PMID 6791199.
- ^ Cohen D, Leo J, Stanton T; et al. (2002). "A boy who stops taking stimulants for "ADHD": commentaries on a Pediatrics case study". Ethical Hum Sci Serv. 4 (3): 189–209. PMID 15278983.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Schwartz RH, Rushton HG (2004). "Stuttering priapism associated with withdrawal from sustained-release methylphenidate". J. Pediatr. 144 (5): 675–6. doi:10.1016/j.jpeds.2003.12.039. PMID 15127013.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Garland EJ (1998). "Pharmacotherapy of adolescent attention deficit hyperactivity disorder: challenges, choices and caveats". J. Psychopharmacol. (Oxford). 12 (4): 385–95. PMID 10065914.
- ^ Nolan EE, Gadow KD, Sprafkin J (1999). "Stimulant medication withdrawal during long-term therapy in children with comorbid attention-deficit hyperactivity disorder and chronic multiple tic disorder". Pediatrics. 103 (4 Pt 1): 730–7. PMID 10103294.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Smucker WD, Hedayat M (2001). "Evaluation and treatment of ADHD". Am Fam Physician. 64 (5): 817–29. PMID 11563573.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Rosenfeld AA (1979). "Depression and psychotic regression following prolonged methylphenidate use and withdrawal: case report". Am J Psychiatry. 136 (2): 226–8. PMID 760559.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Riccio CA, Waldrop JJ, Reynolds CR, Lowe P (2001). "Effects of stimulants on the continuous performance test (CPT): implications for CPT use and interpretation". J Neuropsychiatry Clin Neurosci. 13 (3): 326–35. PMID 11514638.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Tan M, Appleton R (2005). "Attention deficit and hyperactivity disorder, methylphenidate, and epilepsy" (PDF). Arch. Dis. Child. 90 (1): 57–9. doi:10.1136/adc.2003.048504. PMC 1720074. PMID 15613514.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Roberts SM, DeMott RP, James RC (1997). "Adrenergic modulation of hepatotoxicity". Drug Metab. Rev. 29 (1–2): 329–53. PMID 9187524.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Marotta PJ, Roberts EA (1998). "Pemoline hepatotoxicity in children". J. Pediatr. 132 (5): 894–7. PMID 9602211.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Patrick KS, González MA, Straughn AB, Markowitz JS (2005). "New methylphenidate formulations for the treatment of attention-deficit/hyperactivity disorder". Expert Opin Drug Deliv. 2 (1): 121–43. doi:10.1517/17425247.2.1.121. PMID 16296740.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Markowitz JS, DeVane CL, Boulton DW, Nahas Z, Risch SC, Diamond F, Patrick KS. Ethylphenidate formation in human subjects after the administration of a single dose of methylphenidate and ethanol. Drug Metabolism and Disposition. 2000 Jun;28(6):620-4.
- ^ Patrick KS, Williard RL, VanWert AL, Dowd JJ, Oatis JE Jr, Middaugh LD. Synthesis and pharmacology of ethylphenidate enantiomers: the human transesterification metabolite of methylphenidate and ethanol. Journal of Medicinal Chemistry. 2005 Apr 21;48(8):2876-81.
- ^ Williard RL, Middaugh LD, Zhu HJ, Patrick KS. Methylphenidate and its ethanol transesterification metabolite ethylphenidate: brain disposition, monoamine transporters and motor activity. Behavioural Pharmacology. 2007 Feb;18(1):39-51.
- ^ "NTP-CERHR monograph on the potential human reproductive and developmental effects of amphetamines". NTP CERHR MON (16): vii–III1. 2005. PMID 16130031.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ a b Scharman EJ, Erdman AR, Cobaugh DJ; et al. (2007). "Methylphenidate poisoning: an evidence-based consensus guideline for out-of-hospital management". Clin Toxicol (Phila). 45 (7): 737–52. doi:10.1080/15563650701665175. PMID 18058301.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ a b Stern EJ, Frank MS, Schmutz JF, Glenny RW, Schmidt R, Godwin JD (1994). "[[Panlobular pulmonary emphysema]] caused by i.v. injection of methylphenidate (Ritalin): findings on chest radiographs and CT scans". AJR Am J Roentgenol. 162 (3): 555–60. PMID 8109495.
{{cite journal}}: URL–wikilink conflict (help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ a b Klein-Schwartz W (2002). "Abuse and toxicity of methylphenidate". Curr. Opin. Pediatr. 14 (2): 219–23. doi:10.1097/00008480-200204000-00013. PMID 11981294.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Sulzer D, Sonders MS, Poulsen NW, Galli A (2005). "Mechanisms of neurotransmitter release by amphetamines: a review". Prog. Neurobiol. 75 (6): 406–33. doi:10.1016/j.pneurobio.2005.04.003. PMID 15955613.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Prakash S (1977). "Further studies on gene polymorphism in the mainbody and geographically isolated populations of Drosophila pseudoobscura". Genetics. 85 (4): 713–9. PMC 1213652. PMID 863242.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Iversen L (2006). "Neurotransmitter transporters and their impact on the development of psychopharmacology" (PDF). Br. J. Pharmacol. 147 Suppl 1: S82–8. doi:10.1038/sj.bjp.0706428. PMC 1760736. PMID 16402124.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Heal DJ, Pierce DM (2006). "Methylphenidate and its isomers: their role in the treatment of attention-deficit hyperactivity disorder using a transdermal delivery system". CNS Drugs. 20 (9): 713–38. PMID 16953648.
- ^ Markowitz JS, DeVane CL, Pestreich LK, Patrick KS, Muniz R (2006). "A comprehensive in vitro screening of d-, l-, and dl-threo-methylphenidate: an exploratory study". J Child Adolesc Psychopharmacol. 16 (6): 687–98. doi:10.1089/cap.2006.16.687. PMID 17201613.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Volkow ND, Wang GJ, Fowler JS, Ding YS (2005). "Imaging the effects of methylphenidate on brain dopamine: new model on its therapeutic actions for attention-deficit/hyperactivity disorder". Biol. Psychiatry. 57 (11): 1410–5. doi:10.1016/j.biopsych.2004.11.006. PMID 15950015.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Wolraich ML, Doffing MA (2004). "Pharmacokinetic considerations in the treatment of attention-deficit hyperactivity disorder with methylphenidate". CNS Drugs. 18 (4): 243–50. PMID 15015904.
- ^ Talbot PS, Laruelle M (2002). "The role of in vivo molecular imaging with PET and SPECT in the elucidation of psychiatric drug action and new drug development". Eur Neuropsychopharmacol. 12 (6): 503–11. PMID 12468013.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Swanson JM, Volkow ND (2003). "Serum and brain concentrations of methylphenidate: implications for use and abuse". Neurosci Biobehav Rev. 27 (7): 615–21. PMID 14624806.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Dutta AK, Zhang S, Kolhatkar R, Reith ME (2003). "Dopamine transporter as target for drug development of cocaine dependence medications". Eur. J. Pharmacol. 479 (1–3): 93–106. PMID 14612141.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Viggiano D, Vallone D, Sadile A (2004). "Dysfunctions in dopamine systems and ADHD: evidence from animals and modeling" (PDF). Neural Plast. 11 (1–2): 97–114. doi:10.1155/NP.2004.97. PMC 2565441. PMID 15303308.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - ^ Volkow N., et al. (1998). "Dopamine Transporter Occupancies in the Human Brain Induced by Therapeutic Doses of Oral Methylphenidate". Am J Psychiatry 155:1325-1331, October 1998.
- ^ Gainetdinov, Raul R. (2001). "Genetics of Childhood Disorders: XXIV. ADHD, Part 8: Hyperdopaminergic Mice as an Animal Model of ADHD". Journal of the American Academy of Child & Adolescent Psychiatry. 40 (3): 380–382. doi:10.1097/00004583-200103000-00020. Retrieved 2006-11-11.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ^ Koelega HS (1993). "Stimulant drugs and vigilance performance: a review". Psychopharmacology (Berl.). 111 (1): 1–16. PMID 7870923.
- ^ Rosack Jim (2004). "Brain Scans Reveal Physiology of ADHD". Psychiatric News. 39 (1): 26.
{{cite journal}}: More than one of|pages=and|page=specified (help); Unknown parameter|day=ignored (help); Unknown parameter|month=ignored (help) - ^ Volkow, ND (2008). "Methylphenidate decreased the amount of glucose needed by the brain to perform a cognitive task". 'PLoS ONE'. 3 (4): e2017. doi:10.1371/journal.pone.0002017. PMID 18414677. Retrieved 2008-11-26.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help)CS1 maint: unflagged free DOI (link) - ^ Devilbiss DM, Berridge CW (2008). "Cognition-enhancing doses of methylphenidate preferentially increase prefrontal cortex neuronal responsiveness". Biol. Psychiatry. 64 (7): 626–35. doi:10.1016/j.biopsych.2008.04.037. PMID 18585681.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Zhu J, Reith ME (2008). "Role of the dopamine transporter in the action of psychostimulants, nicotine, and other drugs of abuse". CNS Neurol Disord Drug Targets. 7 (5): 393–409. PMID 19128199.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Volkow ND, Swanson JM (2003). "Variables that affect the clinical use and abuse of methylphenidate in the treatment of ADHD". Am J Psychiatry. 160 (11): 1909–18. PMID 14594733.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Arria AM, Wish ED (2006). "Nonmedical use of prescription stimulants among students". Pediatr Ann. 35 (8): 565–71. PMID 16986451.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ http://jpet.aspetjournals.org/cgi/content/full/288/1/14#Introduction "Almost indistinguishable from that [high] induced by i.v. cocaine"
- ^ Fowler JS, Volkow ND, Wang GJ, Gatley SJ, Logan J (2001). "[(11)]Cocaine: PET studies of cocaine pharmacokinetics, dopamine transporter availability and dopamine transporter occupancy". Nucl. Med. Biol. 28 (5): 561–72. PMID 11516700.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ a b http://www.udel.edu/chemo/teaching/CHEM465/SitesF02/Prop26b/Rit%20Page4.html Pretreatment with methylphenidate sensitizes rats to the reinforcing effects of cocaine
- ^ Kollins SH, MacDonald EK, Rush CR (2001). "Assessing the abuse potential of methylphenidate in nonhuman and human subjects: a review". Pharmacol. Biochem. Behav. 68 (3): 611–27. PMID 11325419.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Template:PDFlink 23rd edition. August 2003. International Narcotics Board, Vienna International Centre. Retrieved 2 March 2006
- ^ Lakhan SE, Hagger-Johnson GE (2007). "The impact of prescribed psychotropics on youth". Clin Pract Epidemol Ment Health. 3: 21. doi:10.1186/1745-0179-3-21. PMC 2100041. PMID 17949504.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Wilens, T.E.., et al. (2003). "Does Stimulant Therapy of Attention-Deficit/Hyperactivity Disorder Beget Later Substance Abuse? A Meta-analytic Review of the Literature". PEDIATRICS. 2003 Vol. 111 No. 1:pp. 179-185
- ^ Russell A. Barkley, PhD,et al. (2003). "Does the Treatment of Attention-Deficit/Hyperactivity Disorder With Stimulants Contribute to Drug Use/Abuse? A 13-Year Prospective Study". PEDIATRICS. 2003 Vol. 111 No. 1: pp. 97-109
- ^ Fone KC, Nutt DJ (2005). "Stimulants: use and abuse in the treatment of attention deficit hyperactivity disorder". Curr Opin Pharmacol. 5 (1): 87–93. doi:10.1016/j.coph.2004.10.001. PMID 15661631.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Weinberg WA, Brumback RA (1992). "The myth of attention deficit-hyperactivity disorder: symptoms resulting from multiple causes". J. Child Neurol. 7 (4): 431–45, discussion 446–61. PMID 1469255.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Richard, Bromfield (July 1, 1996). "The Debate of Ritalin: Point & Counterpoint". Priorities. 8 (3). Retrieved 2009-02-28.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Ouellette EM (1991). "Legal issues in the treatment of children with attention deficit hyperactivity disorder". J. Child Neurol. 6 Suppl: S68–75. PMID 2002217.
External links
- Methylphenidate at Curlie
- Department of Energy 1998 September 29 press release on Ritalin at Brookhaven National Laboratory
- Erowid methylphenidate vault
