Estriol (medication)
 | |
 | |
| Clinical data | |
|---|---|
| Pronunciation | /ˈɛstriɒl, -traɪɒl/[1] ESS-TREE-ohl[1] |
| Trade names | Ovestin, others[2][3] |
| Other names | Oestriol; E3; 16α-Hydroxyestradiol; Estra-1,3,5(10)-triene-3,16α,17β-triol |
| Routes of administration | By mouth, vaginal, intramuscular injection[4][5][6] |
| Drug class | Estrogen |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | Oral: ~1–2%[4][6] Vaginal: ~10–20%[5][4][6] |
| Protein binding | 92%:[4] • Albumin: 91%[4] • SHBG: 1%[4] • Free: 8%[4] |
| Metabolism | Liver, intestines (conjugation (glucuronidation, sulfation), oxidation, hydroxylation)[4] |
| Metabolites | • Estriol 16α-glucuronide[7][5] • Estriol 3-glucuronide[7][5] • Estriol 3-sulfate[7][5] • Estriol 3-sulfate 16α-gluc.[7][5] • 16α-Hydroxyestrone[4][8] • Others (minor)[4] |
| Elimination half-life | Oral: 5–10 hours[9][8] IM: 1.5–5.3 hours (as E3)[5] IV: 20 minutes (as E3)[10][11] |
| Excretion | Urine: >95% (as conjugates)[4][5] |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| Chemical and physical data | |
| Formula | C18H24O3 |
| Molar mass | 288.387 g·mol−1 |
| 3D model (JSmol) | |
| Melting point | 82 to 86 °C (180 to 187 °F) (experimental) |
| Solubility in water | 0.119 mg/mL (20 °C) |
| |
| |
| (verify) | |
Estriol (E3), sold under the brand name Ovestin among others, is an estrogen medication and naturally occurring steroid hormone which is used in menopausal hormone therapy.[12][4][6][13] It is also used in veterinary medicine as Incurin to treat urinary incontinence due to estrogen deficiency in dogs.[14][15][16][17] The medication is taken by mouth in the form of tablets, as a cream that is applied to the skin, as a cream or pessary that is applied in the vagina, and by injection into muscle.[4][5][6]
Estriol is well-tolerated and produces relatively few adverse effects.[12][18] Side effects may include breast tenderness, vaginal discomfort and discharge, and endometrial hyperplasia.[12][18] Estriol is a naturally occurring and bioidentical estrogen, or an agonist of the estrogen receptor, the biological target of estrogens like endogenous estradiol.[4] It is an atypical and relatively weak estrogen, with much lower potency than estradiol.[4][6][19] When present continuously at adequate concentrations however, estriol produces full estrogenic effects similarly to estradiol.[20][21]
Estriol was first discovered in 1930,[22][23] and was introduced for medical use shortly thereafter.[24][25] Estriol esters such as estriol succinate are also used.[4][18][3] Although it is less commonly employed than other estrogens like estradiol and conjugated estrogens, estriol is widely available for medical use in Europe and elsewhere throughout the world.[4][2][3][6]
Medical uses
[edit]Estriol is used in menopausal hormone therapy to treat menopausal symptoms, such as hot flashes, vulvovaginal atrophy, and dyspareunia (difficult or painful sexual intercourse).[12][4][13][26][18] The benefits of estriol on bone mineral density and osteoporosis prevention have been inconsistent and are less clear.[18][12] Estriol has been found to reduce the risk of urinary tract infections and other urogenital symptoms.[4][12] A combination of estriol and lactobacilli as a dual estrogen and probiotic has been marketed for the treatment of vaginal atrophy and urinary tract infections.[27]
| Route/form | Estrogen | Low | Standard | High | |||
|---|---|---|---|---|---|---|---|
| Oral | Estradiol | 0.5–1 mg/day | 1–2 mg/day | 2–4 mg/day | |||
| Estradiol valerate | 0.5–1 mg/day | 1–2 mg/day | 2–4 mg/day | ||||
| Estradiol acetate | 0.45–0.9 mg/day | 0.9–1.8 mg/day | 1.8–3.6 mg/day | ||||
| Conjugated estrogens | 0.3–0.45 mg/day | 0.625 mg/day | 0.9–1.25 mg/day | ||||
| Esterified estrogens | 0.3–0.45 mg/day | 0.625 mg/day | 0.9–1.25 mg/day | ||||
| Estropipate | 0.75 mg/day | 1.5 mg/day | 3 mg/day | ||||
| Estriol | 1–2 mg/day | 2–4 mg/day | 4–8 mg/day | ||||
| Ethinylestradiola | 2.5–10 μg/day | 5–20 μg/day | – | ||||
| Nasal spray | Estradiol | 150 μg/day | 300 μg/day | 600 μg/day | |||
| Transdermal patch | Estradiol | 25 μg/dayb | 50 μg/dayb | 100 μg/dayb | |||
| Transdermal gel | Estradiol | 0.5 mg/day | 1–1.5 mg/day | 2–3 mg/day | |||
| Vaginal | Estradiol | 25 μg/day | – | – | |||
| Estriol | 30 μg/day | 0.5 mg 2x/week | 0.5 mg/day | ||||
| IM or SC injection | Estradiol valerate | – | – | 4 mg 1x/4 weeks | |||
| Estradiol cypionate | 1 mg 1x/3–4 weeks | 3 mg 1x/3–4 weeks | 5 mg 1x/3–4 weeks | ||||
| Estradiol benzoate | 0.5 mg 1x/week | 1 mg 1x/week | 1.5 mg 1x/week | ||||
| SC implant | Estradiol | 25 mg 1x/6 months | 50 mg 1x/6 months | 100 mg 1x/6 months | |||
| Footnotes: a = No longer used or recommended, due to health concerns. b = As a single patch applied once or twice per week (worn for 3–4 days or 7 days), depending on the formulation. Note: Dosages are not necessarily equivalent. Sources: See template. | |||||||
Available forms (except USA)
[edit]Estriol is available in oral tablet, vaginal cream, and vaginal suppository forms.[13] It is also available over-the-counter or from compounding pharmacies in the form of topical creams.[28] The medication is available both as estriol and in the form of estriol ester prodrugs such as estriol succinate, estriol acetate benzoate, and estriol tripropionate, as well as the polymeric ester prodrug polyestriol phosphate.[4][18][29][2][3]
Estriol was originally marketed in the 1930s in the form of oral capsules containing 0.06, 0.12, or 0.24 mg estriol under the brand names Theelol (Parke-Davis) and Estriol (Lilly, Abbott).[30][31][32][33][34] Subsequently, many decades later, oral tablets containing 0.35, 1, or 2 mg estriol were introduced under brand names such as Gynäsan, Hormomed, Ovestin, and Ovo-Vinces.[35]
Contraindications
[edit]General contraindications of estrogens include breast cancer, endometrial cancer, and others.[19] In animals, estriol is contraindicated during pregnancy and in ferrets.[17]
Side effects
[edit]Estriol is well-tolerated and produces relatively few adverse effects.[12][18] Breast tenderness may sometimes occur as a side effect of estriol.[12] Local reactions with vaginal estriol such as discomfort (irritation, burning, itching) and discharge may occur.[12] Estriol may produce endometrial hyperplasia similarly to estradiol and other estrogens, and hence should be combined with a progestogen in women with intact uteruses to prevent this risk.[36][4] However, it appears that typical clinical dosages of vaginal estriol are not associated with an important risk of endometrial proliferation or hyperplasia.[12][26] As such, combination with a progestogen may not be needed in the case of vaginal estriol.[12][26] Some studies suggest that this may also be true for oral estriol.[18] However, dosage and frequency of administration, as well as meal consumption, may be determining factors as to whether or not estriol produces endometrial proliferation.[4]
Overdose
[edit]Estrogens and other steroids are relatively safe in acute overdose.[citation needed] Estriol has been assessed in single oral doses of up to 75 mg.[37][38] General symptoms of estrogen overdose in humans may include nausea, vomiting, vaginal bleeding, and reversible feminization.[39][16] While there are no known studies describing the acute toxicity of estrogen overdose in dogs, this species is known to be more sensitive to the toxic effects of estrogens than humans and other animals.[16] The most serious short-term adverse effect of estrogens in dogs is bone marrow suppression and consequent pancytopenia, which can be life-threatening.[16]
Interactions
[edit]Interactions with estriol might be expected to be similar to those of estradiol.[40] No interactions with estriol have been reported in animals.[17] However, it should not be used in combination with other drugs that suppress bone marrow production in dogs.[17]
Pharmacology
[edit]Pharmacodynamics
[edit]Estriol is an estrogen, or an agonist of the estrogen receptors (ERs), ERα and ERβ.[4][41][42] In terms of relative binding affinities (RBA) for the ERs compared to estradiol, it was found in one study to possess 11 to 14% of the RBA for the human ERα and 18 to 21% of the RBA for the human ERβ.[42] Its relative transactivational capacities at the ERs compared to estradiol were 11% at ERα and 17% at ERβ.[42] In addition to being a ligand of the classical nuclear ERs, estriol is an antagonist of the G protein-coupled estrogen receptor (GPER), a membrane estrogen receptor (mER), at high concentrations (~1,000–10,000 μM).[43][44][41][45] This is in contrast to estradiol, which is an agonist of this receptor.[44][41][45] Like other estrogens, estriol does not importantly interact with other steroid hormone receptors.[46][47][48][49][50]
Estriol is a much less potent estrogen than is estradiol, and is somewhat weak and atypical in its properties.[4][42][44][19] Given by subcutaneous injection in mice, estradiol is about 10-fold more potent than estrone and about 100-fold more potent than estriol.[51] With clinical use, estriol is said to be weakly estrogenic in certain tissues, such as the liver and endometrium, but produces pronounced and full estrogenic responses in the vaginal epithelium.[4] The medication has been found to reduce hot flashes, improve vaginal atrophy, reverse the postmenopausal decline in skin thickness and collagen content, suppress gonadotropin secretion, and produce proliferation of breast epithelium.[4] Conversely, estriol does not consistently affect bone resorption or fracture risk, does not seem to increase breast density, and, at oral doses of 2 to 4 mg/day, does not affect liver proteins, lipid metabolism, or hemostatic parameters.[4][18] Additionally, vaginal estriol does not appear to produce endometrial proliferation or increase the risk of endometrial hyperplasia, and some studies have found this to be the case for oral estriol as well.[4][18][52] On the other hand, it appears that estriol may be able to stimulate the growth of active breast cancer.[18][12] In rodents, estriol induces mammary gland development similar to that with estrone.[53] By the oral route in women, estriol has approximately 30% of the potency of estradiol in terms of hot flashes relief and suppression of follicle-stimulating hormone secretion, and about 20% of the potency of estradiol on stimulation of liver production of high-density lipoprotein (HDL) cholesterol.[4] A study of ovulation inhibition by estrogens in women found that prevention of ovulation occurred with 5 mg/day oral estriol in only 1 of 7 cycles.[54][55] Due to its differing effects from those of estradiol, estriol may be considered a safer estrogen in certain regards.[12]

The weak and atypical estrogenicity of estriol is thought to be related to its short duration in the body and hence the fact that it stays bound to the ER for a relatively short amount of time.[4][21] Whereas estradiol remains bound to the ER for 6 to 24 hours with a single short-acting injection, estriol dissociates from the receptor much more rapidly and stays bound for only 1 to 6 hours.[4][21][58][59] As a result, estriol can only induce estrogenic effects which require short-term interaction with the ERs.[4][21] Induction of endometrial mitoses requires the ligand to remain bound for at least 9 to 12 hours, and this is thought to be responsible for the lack of endometrial proliferation with estriol in many studies.[4][21] If estriol is delivered more continuously than a single administration per day however, for instance if it is given as a subcutaneous pellet, as a depot injection, or in multiple doses two or three times per day, this results in more sustained exposure to estriol and full estrogenic responses equivalent to those of estradiol occur.[4][21][12] For these reasons, estriol has been described as a "short-acting" estrogen and it has been said that descriptors like "weak" and "impeded" are inaccurate.[21] Consumption of food after oral administration of estriol also results in more prolonged exposure to estriol, due to enterohepatic recycling and resurgences in estriol levels.[4] As such, if avoidance of endometrial hyperplasia or other full estrogenic effects is intended, it may be preferable to take estriol in a single dose, as low as possible, once per day at night before bedtime.[4][52]
Although estriol is an estrogen, it has also been reported to have mixed agonist–antagonist or partial agonist activity at the ERs.[4][21][19] On its own, it is said to be weakly estrogenic, but in the presence of estradiol, it has been found to be antiestrogenic.[4][44] However, this is again due to the fact that estriol is a "short-acting" estrogen.[21] If estriol is present continuously with estradiol, it shows no antagonism of estradiol.[21] The co-administration of estriol with estradiol has been found not to influence the effects of the latter in women, including neither enhancing nor antagonizing the effects of estradiol.[52][60]
| Ligand | Other names | Relative binding affinities (RBA, %)a | Absolute binding affinities (Ki, nM)a | Action | ||
|---|---|---|---|---|---|---|
| ERα | ERβ | ERα | ERβ | |||
| Estradiol | E2; 17β-Estradiol | 100 | 100 | 0.115 (0.04–0.24) | 0.15 (0.10–2.08) | Estrogen |
| Estrone | E1; 17-Ketoestradiol | 16.39 (0.7–60) | 6.5 (1.36–52) | 0.445 (0.3–1.01) | 1.75 (0.35–9.24) | Estrogen |
| Estriol | E3; 16α-OH-17β-E2 | 12.65 (4.03–56) | 26 (14.0–44.6) | 0.45 (0.35–1.4) | 0.7 (0.63–0.7) | Estrogen |
| Estetrol | E4; 15α,16α-Di-OH-17β-E2 | 4.0 | 3.0 | 4.9 | 19 | Estrogen |
| Alfatradiol | 17α-Estradiol | 20.5 (7–80.1) | 8.195 (2–42) | 0.2–0.52 | 0.43–1.2 | Metabolite |
| 16-Epiestriol | 16β-Hydroxy-17β-estradiol | 7.795 (4.94–63) | 50 | ? | ? | Metabolite |
| 17-Epiestriol | 16α-Hydroxy-17α-estradiol | 55.45 (29–103) | 79–80 | ? | ? | Metabolite |
| 16,17-Epiestriol | 16β-Hydroxy-17α-estradiol | 1.0 | 13 | ? | ? | Metabolite |
| 2-Hydroxyestradiol | 2-OH-E2 | 22 (7–81) | 11–35 | 2.5 | 1.3 | Metabolite |
| 2-Methoxyestradiol | 2-MeO-E2 | 0.0027–2.0 | 1.0 | ? | ? | Metabolite |
| 4-Hydroxyestradiol | 4-OH-E2 | 13 (8–70) | 7–56 | 1.0 | 1.9 | Metabolite |
| 4-Methoxyestradiol | 4-MeO-E2 | 2.0 | 1.0 | ? | ? | Metabolite |
| 2-Hydroxyestrone | 2-OH-E1 | 2.0–4.0 | 0.2–0.4 | ? | ? | Metabolite |
| 2-Methoxyestrone | 2-MeO-E1 | <0.001–<1 | <1 | ? | ? | Metabolite |
| 4-Hydroxyestrone | 4-OH-E1 | 1.0–2.0 | 1.0 | ? | ? | Metabolite |
| 4-Methoxyestrone | 4-MeO-E1 | <1 | <1 | ? | ? | Metabolite |
| 16α-Hydroxyestrone | 16α-OH-E1; 17-Ketoestriol | 2.0–6.5 | 35 | ? | ? | Metabolite |
| 2-Hydroxyestriol | 2-OH-E3 | 2.0 | 1.0 | ? | ? | Metabolite |
| 4-Methoxyestriol | 4-MeO-E3 | 1.0 | 1.0 | ? | ? | Metabolite |
| Estradiol sulfate | E2S; Estradiol 3-sulfate | <1 | <1 | ? | ? | Metabolite |
| Estradiol disulfate | Estradiol 3,17β-disulfate | 0.0004 | ? | ? | ? | Metabolite |
| Estradiol 3-glucuronide | E2-3G | 0.0079 | ? | ? | ? | Metabolite |
| Estradiol 17β-glucuronide | E2-17G | 0.0015 | ? | ? | ? | Metabolite |
| Estradiol 3-gluc. 17β-sulfate | E2-3G-17S | 0.0001 | ? | ? | ? | Metabolite |
| Estrone sulfate | E1S; Estrone 3-sulfate | <1 | <1 | >10 | >10 | Metabolite |
| Estradiol benzoate | EB; Estradiol 3-benzoate | 10 | ? | ? | ? | Estrogen |
| Estradiol 17β-benzoate | E2-17B | 11.3 | 32.6 | ? | ? | Estrogen |
| Estrone methyl ether | Estrone 3-methyl ether | 0.145 | ? | ? | ? | Estrogen |
| ent-Estradiol | 1-Estradiol | 1.31–12.34 | 9.44–80.07 | ? | ? | Estrogen |
| Equilin | 7-Dehydroestrone | 13 (4.0–28.9) | 13.0–49 | 0.79 | 0.36 | Estrogen |
| Equilenin | 6,8-Didehydroestrone | 2.0–15 | 7.0–20 | 0.64 | 0.62 | Estrogen |
| 17β-Dihydroequilin | 7-Dehydro-17β-estradiol | 7.9–113 | 7.9–108 | 0.09 | 0.17 | Estrogen |
| 17α-Dihydroequilin | 7-Dehydro-17α-estradiol | 18.6 (18–41) | 14–32 | 0.24 | 0.57 | Estrogen |
| 17β-Dihydroequilenin | 6,8-Didehydro-17β-estradiol | 35–68 | 90–100 | 0.15 | 0.20 | Estrogen |
| 17α-Dihydroequilenin | 6,8-Didehydro-17α-estradiol | 20 | 49 | 0.50 | 0.37 | Estrogen |
| Δ8-Estradiol | 8,9-Dehydro-17β-estradiol | 68 | 72 | 0.15 | 0.25 | Estrogen |
| Δ8-Estrone | 8,9-Dehydroestrone | 19 | 32 | 0.52 | 0.57 | Estrogen |
| Ethinylestradiol | EE; 17α-Ethynyl-17β-E2 | 120.9 (68.8–480) | 44.4 (2.0–144) | 0.02–0.05 | 0.29–0.81 | Estrogen |
| Mestranol | EE 3-methyl ether | ? | 2.5 | ? | ? | Estrogen |
| Moxestrol | RU-2858; 11β-Methoxy-EE | 35–43 | 5–20 | 0.5 | 2.6 | Estrogen |
| Methylestradiol | 17α-Methyl-17β-estradiol | 70 | 44 | ? | ? | Estrogen |
| Diethylstilbestrol | DES; Stilbestrol | 129.5 (89.1–468) | 219.63 (61.2–295) | 0.04 | 0.05 | Estrogen |
| Hexestrol | Dihydrodiethylstilbestrol | 153.6 (31–302) | 60–234 | 0.06 | 0.06 | Estrogen |
| Dienestrol | Dehydrostilbestrol | 37 (20.4–223) | 56–404 | 0.05 | 0.03 | Estrogen |
| Benzestrol (B2) | – | 114 | ? | ? | ? | Estrogen |
| Chlorotrianisene | TACE | 1.74 | ? | 15.30 | ? | Estrogen |
| Triphenylethylene | TPE | 0.074 | ? | ? | ? | Estrogen |
| Triphenylbromoethylene | TPBE | 2.69 | ? | ? | ? | Estrogen |
| Tamoxifen | ICI-46,474 | 3 (0.1–47) | 3.33 (0.28–6) | 3.4–9.69 | 2.5 | SERM |
| Afimoxifene | 4-Hydroxytamoxifen; 4-OHT | 100.1 (1.7–257) | 10 (0.98–339) | 2.3 (0.1–3.61) | 0.04–4.8 | SERM |
| Toremifene | 4-Chlorotamoxifen; 4-CT | ? | ? | 7.14–20.3 | 15.4 | SERM |
| Clomifene | MRL-41 | 25 (19.2–37.2) | 12 | 0.9 | 1.2 | SERM |
| Cyclofenil | F-6066; Sexovid | 151–152 | 243 | ? | ? | SERM |
| Nafoxidine | U-11,000A | 30.9–44 | 16 | 0.3 | 0.8 | SERM |
| Raloxifene | – | 41.2 (7.8–69) | 5.34 (0.54–16) | 0.188–0.52 | 20.2 | SERM |
| Arzoxifene | LY-353,381 | ? | ? | 0.179 | ? | SERM |
| Lasofoxifene | CP-336,156 | 10.2–166 | 19.0 | 0.229 | ? | SERM |
| Ormeloxifene | Centchroman | ? | ? | 0.313 | ? | SERM |
| Levormeloxifene | 6720-CDRI; NNC-460,020 | 1.55 | 1.88 | ? | ? | SERM |
| Ospemifene | Deaminohydroxytoremifene | 0.82–2.63 | 0.59–1.22 | ? | ? | SERM |
| Bazedoxifene | – | ? | ? | 0.053 | ? | SERM |
| Etacstil | GW-5638 | 4.30 | 11.5 | ? | ? | SERM |
| ICI-164,384 | – | 63.5 (3.70–97.7) | 166 | 0.2 | 0.08 | Antiestrogen |
| Fulvestrant | ICI-182,780 | 43.5 (9.4–325) | 21.65 (2.05–40.5) | 0.42 | 1.3 | Antiestrogen |
| Propylpyrazoletriol | PPT | 49 (10.0–89.1) | 0.12 | 0.40 | 92.8 | ERα agonist |
| 16α-LE2 | 16α-Lactone-17β-estradiol | 14.6–57 | 0.089 | 0.27 | 131 | ERα agonist |
| 16α-Iodo-E2 | 16α-Iodo-17β-estradiol | 30.2 | 2.30 | ? | ? | ERα agonist |
| Methylpiperidinopyrazole | MPP | 11 | 0.05 | ? | ? | ERα antagonist |
| Diarylpropionitrile | DPN | 0.12–0.25 | 6.6–18 | 32.4 | 1.7 | ERβ agonist |
| 8β-VE2 | 8β-Vinyl-17β-estradiol | 0.35 | 22.0–83 | 12.9 | 0.50 | ERβ agonist |
| Prinaberel | ERB-041; WAY-202,041 | 0.27 | 67–72 | ? | ? | ERβ agonist |
| ERB-196 | WAY-202,196 | ? | 180 | ? | ? | ERβ agonist |
| Erteberel | SERBA-1; LY-500,307 | ? | ? | 2.68 | 0.19 | ERβ agonist |
| SERBA-2 | – | ? | ? | 14.5 | 1.54 | ERβ agonist |
| Coumestrol | – | 9.225 (0.0117–94) | 64.125 (0.41–185) | 0.14–80.0 | 0.07–27.0 | Xenoestrogen |
| Genistein | – | 0.445 (0.0012–16) | 33.42 (0.86–87) | 2.6–126 | 0.3–12.8 | Xenoestrogen |
| Equol | – | 0.2–0.287 | 0.85 (0.10–2.85) | ? | ? | Xenoestrogen |
| Daidzein | – | 0.07 (0.0018–9.3) | 0.7865 (0.04–17.1) | 2.0 | 85.3 | Xenoestrogen |
| Biochanin A | – | 0.04 (0.022–0.15) | 0.6225 (0.010–1.2) | 174 | 8.9 | Xenoestrogen |
| Kaempferol | – | 0.07 (0.029–0.10) | 2.2 (0.002–3.00) | ? | ? | Xenoestrogen |
| Naringenin | – | 0.0054 (<0.001–0.01) | 0.15 (0.11–0.33) | ? | ? | Xenoestrogen |
| 8-Prenylnaringenin | 8-PN | 4.4 | ? | ? | ? | Xenoestrogen |
| Quercetin | – | <0.001–0.01 | 0.002–0.040 | ? | ? | Xenoestrogen |
| Ipriflavone | – | <0.01 | <0.01 | ? | ? | Xenoestrogen |
| Miroestrol | – | 0.39 | ? | ? | ? | Xenoestrogen |
| Deoxymiroestrol | – | 2.0 | ? | ? | ? | Xenoestrogen |
| β-Sitosterol | – | <0.001–0.0875 | <0.001–0.016 | ? | ? | Xenoestrogen |
| Resveratrol | – | <0.001–0.0032 | ? | ? | ? | Xenoestrogen |
| α-Zearalenol | – | 48 (13–52.5) | ? | ? | ? | Xenoestrogen |
| β-Zearalenol | – | 0.6 (0.032–13) | ? | ? | ? | Xenoestrogen |
| Zeranol | α-Zearalanol | 48–111 | ? | ? | ? | Xenoestrogen |
| Taleranol | β-Zearalanol | 16 (13–17.8) | 14 | 0.8 | 0.9 | Xenoestrogen |
| Zearalenone | ZEN | 7.68 (2.04–28) | 9.45 (2.43–31.5) | ? | ? | Xenoestrogen |
| Zearalanone | ZAN | 0.51 | ? | ? | ? | Xenoestrogen |
| Bisphenol A | BPA | 0.0315 (0.008–1.0) | 0.135 (0.002–4.23) | 195 | 35 | Xenoestrogen |
| Endosulfan | EDS | <0.001–<0.01 | <0.01 | ? | ? | Xenoestrogen |
| Kepone | Chlordecone | 0.0069–0.2 | ? | ? | ? | Xenoestrogen |
| o,p'-DDT | – | 0.0073–0.4 | ? | ? | ? | Xenoestrogen |
| p,p'-DDT | – | 0.03 | ? | ? | ? | Xenoestrogen |
| Methoxychlor | p,p'-Dimethoxy-DDT | 0.01 (<0.001–0.02) | 0.01–0.13 | ? | ? | Xenoestrogen |
| HPTE | Hydroxychlor; p,p'-OH-DDT | 1.2–1.7 | ? | ? | ? | Xenoestrogen |
| Testosterone | T; 4-Androstenolone | <0.0001–<0.01 | <0.002–0.040 | >5000 | >5000 | Androgen |
| Dihydrotestosterone | DHT; 5α-Androstanolone | 0.01 (<0.001–0.05) | 0.0059–0.17 | 221–>5000 | 73–1688 | Androgen |
| Nandrolone | 19-Nortestosterone; 19-NT | 0.01 | 0.23 | 765 | 53 | Androgen |
| Dehydroepiandrosterone | DHEA; Prasterone | 0.038 (<0.001–0.04) | 0.019–0.07 | 245–1053 | 163–515 | Androgen |
| 5-Androstenediol | A5; Androstenediol | 6 | 17 | 3.6 | 0.9 | Androgen |
| 4-Androstenediol | – | 0.5 | 0.6 | 23 | 19 | Androgen |
| 4-Androstenedione | A4; Androstenedione | <0.01 | <0.01 | >10000 | >10000 | Androgen |
| 3α-Androstanediol | 3α-Adiol | 0.07 | 0.3 | 260 | 48 | Androgen |
| 3β-Androstanediol | 3β-Adiol | 3 | 7 | 6 | 2 | Androgen |
| Androstanedione | 5α-Androstanedione | <0.01 | <0.01 | >10000 | >10000 | Androgen |
| Etiocholanedione | 5β-Androstanedione | <0.01 | <0.01 | >10000 | >10000 | Androgen |
| Methyltestosterone | 17α-Methyltestosterone | <0.0001 | ? | ? | ? | Androgen |
| Ethinyl-3α-androstanediol | 17α-Ethynyl-3α-adiol | 4.0 | <0.07 | ? | ? | Estrogen |
| Ethinyl-3β-androstanediol | 17α-Ethynyl-3β-adiol | 50 | 5.6 | ? | ? | Estrogen |
| Progesterone | P4; 4-Pregnenedione | <0.001–0.6 | <0.001–0.010 | ? | ? | Progestogen |
| Norethisterone | NET; 17α-Ethynyl-19-NT | 0.085 (0.0015–<0.1) | 0.1 (0.01–0.3) | 152 | 1084 | Progestogen |
| Norethynodrel | 5(10)-Norethisterone | 0.5 (0.3–0.7) | <0.1–0.22 | 14 | 53 | Progestogen |
| Tibolone | 7α-Methylnorethynodrel | 0.5 (0.45–2.0) | 0.2–0.076 | ? | ? | Progestogen |
| Δ4-Tibolone | 7α-Methylnorethisterone | 0.069–<0.1 | 0.027–<0.1 | ? | ? | Progestogen |
| 3α-Hydroxytibolone | – | 2.5 (1.06–5.0) | 0.6–0.8 | ? | ? | Progestogen |
| 3β-Hydroxytibolone | – | 1.6 (0.75–1.9) | 0.070–0.1 | ? | ? | Progestogen |
| Footnotes: a = (1) Binding affinity values are of the format "median (range)" (# (#–#)), "range" (#–#), or "value" (#) depending on the values available. The full sets of values within the ranges can be found in the Wiki code. (2) Binding affinities were determined via displacement studies in a variety of in-vitro systems with labeled estradiol and human ERα and ERβ proteins (except the ERβ values from Kuiper et al. (1997), which are rat ERβ). Sources: See template page. | ||||||
| Estrogen | Relative binding affinities (%) | ||||||
|---|---|---|---|---|---|---|---|
| ER | AR | PR | GR | MR | SHBG | CBG | |
| Estradiol | 100 | 7.9 | 2.6 | 0.6 | 0.13 | 8.7–12 | <0.1 |
| Estradiol benzoate | ? | ? | ? | ? | ? | <0.1–0.16 | <0.1 |
| Estradiol valerate | 2 | ? | ? | ? | ? | ? | ? |
| Estrone | 11–35 | <1 | <1 | <1 | <1 | 2.7 | <0.1 |
| Estrone sulfate | 2 | 2 | ? | ? | ? | ? | ? |
| Estriol | 10–15 | <1 | <1 | <1 | <1 | <0.1 | <0.1 |
| Equilin | 40 | ? | ? | ? | ? | ? | 0 |
| Alfatradiol | 15 | <1 | <1 | <1 | <1 | ? | ? |
| Epiestriol | 20 | <1 | <1 | <1 | <1 | ? | ? |
| Ethinylestradiol | 100–112 | 1–3 | 15–25 | 1–3 | <1 | 0.18 | <0.1 |
| Mestranol | 1 | ? | ? | ? | ? | <0.1 | <0.1 |
| Methylestradiol | 67 | 1–3 | 3–25 | 1–3 | <1 | ? | ? |
| Moxestrol | 12 | <0.1 | 0.8 | 3.2 | <0.1 | <0.2 | <0.1 |
| Diethylstilbestrol | ? | ? | ? | ? | ? | <0.1 | <0.1 |
| Notes: Reference ligands (100%) were progesterone for the PR, testosterone for the AR, estradiol for the ER, dexamethasone for the GR, aldosterone for the MR, dihydrotestosterone for SHBG, and cortisol for CBG. Sources: See template. | |||||||
| Estrogen | ER RBA (%) | Uterine weight (%) | Uterotrophy | LH levels (%) | SHBG RBA (%) |
|---|---|---|---|---|---|
| Control | – | 100 | – | 100 | – |
| Estradiol (E2) | 100 | 506 ± 20 | +++ | 12–19 | 100 |
| Estrone (E1) | 11 ± 8 | 490 ± 22 | +++ | ? | 20 |
| Estriol (E3) | 10 ± 4 | 468 ± 30 | +++ | 8–18 | 3 |
| Estetrol (E4) | 0.5 ± 0.2 | ? | Inactive | ? | 1 |
| 17α-Estradiol | 4.2 ± 0.8 | ? | ? | ? | ? |
| 2-Hydroxyestradiol | 24 ± 7 | 285 ± 8 | +b | 31–61 | 28 |
| 2-Methoxyestradiol | 0.05 ± 0.04 | 101 | Inactive | ? | 130 |
| 4-Hydroxyestradiol | 45 ± 12 | ? | ? | ? | ? |
| 4-Methoxyestradiol | 1.3 ± 0.2 | 260 | ++ | ? | 9 |
| 4-Fluoroestradiola | 180 ± 43 | ? | +++ | ? | ? |
| 2-Hydroxyestrone | 1.9 ± 0.8 | 130 ± 9 | Inactive | 110–142 | 8 |
| 2-Methoxyestrone | 0.01 ± 0.00 | 103 ± 7 | Inactive | 95–100 | 120 |
| 4-Hydroxyestrone | 11 ± 4 | 351 | ++ | 21–50 | 35 |
| 4-Methoxyestrone | 0.13 ± 0.04 | 338 | ++ | 65–92 | 12 |
| 16α-Hydroxyestrone | 2.8 ± 1.0 | 552 ± 42 | +++ | 7–24 | <0.5 |
| 2-Hydroxyestriol | 0.9 ± 0.3 | 302 | +b | ? | ? |
| 2-Methoxyestriol | 0.01 ± 0.00 | ? | Inactive | ? | 4 |
| Notes: Values are mean ± SD or range. ER RBA = Relative binding affinity to estrogen receptors of rat uterine cytosol. Uterine weight = Percentage change in uterine wet weight of ovariectomized rats after 72 hours with continuous administration of 1 μg/hour via subcutaneously implanted osmotic pumps. LH levels = Luteinizing hormone levels relative to baseline of ovariectomized rats after 24 to 72 hours of continuous administration via subcutaneous implant. Footnotes: a = Synthetic (i.e., not endogenous). b = Atypical uterotrophic effect which plateaus within 48 hours (estradiol's uterotrophy continues linearly up to 72 hours). Sources: See template. | |||||
| Estrogen | HF | VE | UCa | FSH | LH | HDL-C | SHBG | CBG | AGT | Liver |
|---|---|---|---|---|---|---|---|---|---|---|
| Estradiol | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Estrone | ? | ? | ? | 0.3 | 0.3 | ? | ? | ? | ? | ? |
| Estriol | 0.3 | 0.3 | 0.1 | 0.3 | 0.3 | 0.2 | ? | ? | ? | 0.67 |
| Estrone sulfate | ? | 0.9 | 0.9 | 0.8–0.9 | 0.9 | 0.5 | 0.9 | 0.5–0.7 | 1.4–1.5 | 0.56–1.7 |
| Conjugated estrogens | 1.2 | 1.5 | 2.0 | 1.1–1.3 | 1.0 | 1.5 | 3.0–3.2 | 1.3–1.5 | 5.0 | 1.3–4.5 |
| Equilin sulfate | ? | ? | 1.0 | ? | ? | 6.0 | 7.5 | 6.0 | 7.5 | ? |
| Ethinylestradiol | 120 | 150 | 400 | 60–150 | 100 | 400 | 500–600 | 500–600 | 350 | 2.9–5.0 |
| Diethylstilbestrol | ? | ? | ? | 2.9–3.4 | ? | ? | 26–28 | 25–37 | 20 | 5.7–7.5 |
Sources and footnotes
Notes: Values are ratios, with estradiol as standard (i.e., 1.0). Abbreviations: HF = Clinical relief of hot flashes. VE = Increased proliferation of vaginal epithelium. UCa = Decrease in UCa. FSH = Suppression of FSH levels. LH = Suppression of LH levels. HDL-C, SHBG, CBG, and AGT = Increase in the serum levels of these liver proteins. Liver = Ratio of liver estrogenic effects to general/systemic estrogenic effects (hot flashes/gonadotropins). Sources: See template. | ||||||||||
| Compound | Dosage for specific uses (mg usually)[a] | ||||||
|---|---|---|---|---|---|---|---|
| ETD[b] | EPD[b] | MSD[b] | MSD[c] | OID[c] | TSD[c] | ||
| Estradiol (non-micronized) | 30 | ≥120–300 | 120 | 6 | - | - | |
| Estradiol (micronized) | 6–12 | 60–80 | 14–42 | 1–2 | >5 | >8 | |
| Estradiol valerate | 6–12 | 60–80 | 14–42 | 1–2 | - | >8 | |
| Estradiol benzoate | - | 60–140 | - | - | - | - | |
| Estriol | ≥20 | 120–150[d] | 28–126 | 1–6 | >5 | - | |
| Estriol succinate | - | 140–150[d] | 28–126 | 2–6 | - | - | |
| Estrone sulfate | 12 | 60 | 42 | 2 | - | - | |
| Conjugated estrogens | 5–12 | 60–80 | 8.4–25 | 0.625–1.25 | >3.75 | 7.5 | |
| Ethinylestradiol | 200 μg | 1–2 | 280 μg | 20–40 μg | 100 μg | 100 μg | |
| Mestranol | 300 μg | 1.5–3.0 | 300–600 μg | 25–30 μg | >80 μg | - | |
| Quinestrol | 300 μg | 2–4 | 500 μg | 25–50 μg | - | - | |
| Methylestradiol | - | 2 | - | - | - | - | |
| Diethylstilbestrol | 2.5 | 20–30 | 11 | 0.5–2.0 | >5 | 3 | |
| DES dipropionate | - | 15–30 | - | - | - | - | |
| Dienestrol | 5 | 30–40 | 42 | 0.5–4.0 | - | - | |
| Dienestrol diacetate | 3–5 | 30–60 | - | - | - | - | |
| Hexestrol | - | 70–110 | - | - | - | - | |
| Chlorotrianisene | - | >100 | - | - | >48 | - | |
| Methallenestril | - | 400 | - | - | - | - | |
| Estrogen | Form | Dose (mg) | Duration by dose (mg) | ||
|---|---|---|---|---|---|
| EPD | CICD | ||||
| Estradiol | Aq. soln. | ? | – | <1 d | |
| Oil soln. | 40–60 | – | 1–2 ≈ 1–2 d | ||
| Aq. susp. | ? | 3.5 | 0.5–2 ≈ 2–7 d; 3.5 ≈ >5 d | ||
| Microsph. | ? | – | 1 ≈ 30 d | ||
| Estradiol benzoate | Oil soln. | 25–35 | – | 1.66 ≈ 2–3 d; 5 ≈ 3–6 d | |
| Aq. susp. | 20 | – | 10 ≈ 16–21 d | ||
| Emulsion | ? | – | 10 ≈ 14–21 d | ||
| Estradiol dipropionate | Oil soln. | 25–30 | – | 5 ≈ 5–8 d | |
| Estradiol valerate | Oil soln. | 20–30 | 5 | 5 ≈ 7–8 d; 10 ≈ 10–14 d; 40 ≈ 14–21 d; 100 ≈ 21–28 d | |
| Estradiol benz. butyrate | Oil soln. | ? | 10 | 10 ≈ 21 d | |
| Estradiol cypionate | Oil soln. | 20–30 | – | 5 ≈ 11–14 d | |
| Aq. susp. | ? | 5 | 5 ≈ 14–24 d | ||
| Estradiol enanthate | Oil soln. | ? | 5–10 | 10 ≈ 20–30 d | |
| Estradiol dienanthate | Oil soln. | ? | – | 7.5 ≈ >40 d | |
| Estradiol undecylate | Oil soln. | ? | – | 10–20 ≈ 40–60 d; 25–50 ≈ 60–120 d | |
| Polyestradiol phosphate | Aq. soln. | 40–60 | – | 40 ≈ 30 d; 80 ≈ 60 d; 160 ≈ 120 d | |
| Estrone | Oil soln. | ? | – | 1–2 ≈ 2–3 d | |
| Aq. susp. | ? | – | 0.1–2 ≈ 2–7 d | ||
| Estriol | Oil soln. | ? | – | 1–2 ≈ 1–4 d | |
| Polyestriol phosphate | Aq. soln. | ? | – | 50 ≈ 30 d; 80 ≈ 60 d | |
Notes and sources
Notes: All aqueous suspensions are of microcrystalline particle size. Estradiol production during the menstrual cycle is 30–640 µg/d (6.4–8.6 mg total per month or cycle). The vaginal epithelium maturation dosage of estradiol benzoate or estradiol valerate has been reported as 5 to 7 mg/week. An effective ovulation-inhibiting dose of estradiol undecylate is 20–30 mg/month. Sources: See template. | |||||
| Class | Examples | RE complex retention | Pharmacodynamic profile | Uterine effects |
|---|---|---|---|---|
| Short-acting (a.k.a. "weak" or "impeded") |
Estriol • 16-Epiestriol • 17α-Estradiol • ent-Estradiol • 16-Ketoestradiol • Dimethylstilbestrol • meso-Butestrol | Short (1–4 hours) | Single or once-daily injections: partial agonist or antagonist | Early responsesa |
| Implant or multiple injections per day: full agonist | Early and late responsesb | |||
| Long-acting | A. Estradiol • Estrone • Ethinylestradiol • Diethylstilbestrol • Hexestrol | Intermediate (6–24 hours) | Single or once-daily injections: full agonist | Early and late responses |
| B. Clomifene • Nafoxidine • Nitromifene • Tamoxifen | Long (>24–48 hours) | Single injection: agonist Repeated injections: antagonist |
Early and late responses | |
| Footnotes: a = Early responses occur after 0–6 hours and include water imbibition, hyperemia, amino acid and nucleotide uptake, activation of RNA polymerases I and II, and stimulation of induced protein, among others. b = Late responses occur after 6–48 hours and include cellular hypertrophy and hyperplasia and sustained RNA polymerase I and II activity, among others. Sources: [80][81][82][83][84][85][86] | ||||
Pharmacokinetics
[edit]
Absorption
[edit]Estriol has significant bioavailability, but its potency is limited by rapid metabolism and excretion and its relatively weak estrogenic activity.[6][18] With oral administration, during first-pass metabolism, a considerable portion of estriol is conjugated via sulfation into estriol sulfate and rapidly excreted.[6][4][52] Only about 10 to 20% of a dose of estriol remains in the circulation, and of this, only about 1 to 2% is present in its active, unconjugated form.[4][6][52] Peak levels of estriol occur about 1 to 3 hours after an oral dose.[4][5] Similarly to the case of progesterone, taking oral estriol with food greatly enhances its absorption.[6] In addition, due to enterohepatic recycling, consuming a meal 4 hours after taking oral estriol can produce a second peak in estriol levels.[4][5] Dosages of oral estriol of 4 to 10 mg have been found to result in a fairly large range of maximal estriol levels of 80 to 340 pg/mL.[5] After a single oral dose of 8 mg estriol in postmenopausal women, maximal levels of 65 pg/mL estriol and 60 ng/mL estriol conjugates were produced within an hour.[4] With continued daily administration, this increased to peak levels of 130 pg/mL estriol, whereas maximal levels of estriol conjugates remained at 60 ng/mL.[4] Levels of estriol rapidly decreased to low levels following occurrence of peak levels.[4] Consumption of a meal 4 hours after taking an oral dose of 8 mg estriol during continuous daily administration resulted in a second estriol peak 2 hours later of 120 pg/mL, with estriol levels declining slowly thereafter to about 25 pg/mL after 24 hours.[4]
The bioavailability of estriol is markedly increased with vaginal administration compared to oral administration.[6] The relative bioavailability of oral estriol was found to be about 10% of that of vaginal estriol.[5] In accordance, a single dose of 8 mg oral estriol and of 0.5 mg vaginal estriol have been found to produce similar circulating concentrations of estriol.[4] It has been said that 0.5 to 1 mg vaginal estriol may be equivalent in clinical effect to 8 to 12 mg oral estriol.[18] The high bioavailability of vaginal estriol is due to rapid absorption and low metabolism in atrophic vaginal mucosa.[4] Vaginal estriol at typical clinical dosages results both in high local concentrations of estriol in the vagina and in systemic action.[4] Vaginal administration of low doses of 30 μg estriol and of higher doses of 0.5 and 1 mg estriol have been found to produce equivalent local effects in the vagina and improvement of vaginal symptoms, suggesting that a saturation of estrogenic effect of vaginal estriol has been reached in the vagina by a dose of only 30 μg estriol.[4] In contrast to higher doses of vaginal estriol however, 30 μg/day estriol is not associated with systemic effects.[4] Similarly, the use of 0.5 mg vaginal estriol twice a week instead of daily has been said to largely attenuate the systemic effects of estriol.[4] Whereas oral estriol results in high levels of estriol conjugates which greatly exceed those of unconjugated estriol, vaginal estriol has been found to produce levels of unconjugated estriol and estriol conjugates that are similar.[4]
The absorption of estrogens by the skin is described as low for estriol, moderate for estradiol, and high for estrone.[4] This is related to the number of hydroxyl groups in the molecules; the more hydroxyl groups, the lower the skin permeability.[4] This may account for the relative lack of use of transdermal or topical estriol.[6]
Rectal administration of estriol has been assessed in one study.[87] Administration of a rectal suppository containing 100 mg estriol resulted in estriol levels in pregnant women at term increasing by about 53%.[87] Estriol levels at term are normally between 5,000 and 20,000 pg/mL, which suggests that estriol levels may have increased following the suppository by about 5,000 to 10,000 pg/mL (precise levels were not provided).[88][89][90]
Estriol succinate is an ester prodrug of estriol which is used medically via oral and vaginal routes similarly.[4] In estriol succinate, two of the hydroxyl groups of estriol, those at the C16α and C17β positions, are esterified with succinic acid.[4] As such, when adjusted for differences in molecular weight, a dose of 2 mg estriol succinate is equivalent to 1.18 mg unconjugated estriol.[4] Unlike other estrogen esters, such as estradiol valerate, estriol succinate is hydrolyzed almost not at all in the intestinal mucosa when taken orally, and in relation to this, is absorbed more slowly than is estriol.[4] Consequently, oral estriol succinate is a longer-acting form of estriol than oral estriol.[20] Instead of in the gastrointestinal tract, oral estriol succinate is cleaved into estriol mainly in the liver.[4] After a single 8 mg oral dose of estriol succinate, maximum levels of circulating estriol of 40 pg/mL are attained within 12 hours, and this increases up to 80 pg/mL with continued daily administration.[4]
Distribution
[edit]Similarly to estradiol, but unlike estrone, estriol is accumulated in target tissues.[4][91] The plasma protein binding of estriol is approximately 92%, with about 91% bound to albumin, 1% bound to sex hormone-binding globulin (SHBG), and 8% free or unbound.[4] Estriol has very low affinity for SHBG, with only about 0.3% of the affinity of testosterone for this protein (or about 0.6% of that of estradiol).[4][92][93] Relative to estradiol, which is about 98% plasma protein-bound, a significantly greater fraction of estriol is unbound in the circulation and hence available for biological activity (2% relative to 8%, respectively).[93][4][18] This appears to account for the greater than expected biological activity of estriol relative to estradiol when considering its affinities for the estrogen receptors.[94]
Metabolism
[edit]Estriol is metabolized extensively via conjugation, including glucuronidation and sulfation.[4][6][5][7] Glucuronidation of estriol takes place mainly in the intestinal mucosa, while sulfation occurs in the liver.[4] More minor amounts of estriol can be oxidized and hydroxylated at various positions.[4] One such reaction is transformation into 16α-hydroxyestrone.[4] Estriol is an end-product of phase I estrogen metabolism and cannot be converted into estradiol or estrone.[4][52] The main metabolites of estriol are estrogen conjugates, including estriol sulfates, estriol glucuronides, and mixed estriol sulfate/glucuronide conjugates.[4] 16α-Hydroxyestrone is known to occur as a metabolite of estriol as well.[95][96][91]
The biological half-life of oral estriol has been reported to be in the range of 5 to 10 hours.[9][8][52] The elimination half-life of estriol following an intramuscular injection of 1 mg estriol has been found to be 1.5 to 5.3 hours.[5] The blood half-life of unconjugated estriol has been reported to be 20 minutes.[10][11] The metabolic clearance rate of estriol is approximately 1,110 L/day/m2, which is about twice that of estradiol.[4] Hence, estriol is eliminated from the body more rapidly than is estradiol.[4] Enterohepatic recycling may extend the duration of oral estriol.[18]
A single 1 to 2 mg dose of estriol in oil solution by intramuscular injection has a duration of about 3 or 4 days.[97] Estriol esters such as estriol dipropionate and estriol dihexanoate, when administered via intramuscular injection in an oil solution, have been found to maintain elevated levels of estriol for much longer amounts of time than oral or vaginal estriol, in the range of days to months.[5] These two estriol esters have not been marketed, but estriol acetate benzoate and estriol tripropionate are medically used estriol esters which are given via depot intramuscular injection and are long-acting similarly.[29] Polyestriol phosphate is an ester of estriol in the form of a polymer, and has a very long duration of action.[98][51]
Excretion
[edit]Estriol is excreted more than 95% in urine.[4] This is due to the fact that estriol conjugates in the colon are completely hydrolyzed via bacterial enzymes and in turn estriol in this part of the body is reabsorbed into the body.[4] The main urinary metabolites of exogenous estriol administered via intravenous injection in baboons have been found to be estriol 16α-glucuronide (65.8%), estriol 3-glucuronide (14.2%), estriol 3-sulfate (13.4%), and estriol 3-sulfate 16α-glucuronide (5.1%).[5][7] The metabolism and excretion of estriol in these animals closely resembled that which has been observed in humans.[7]
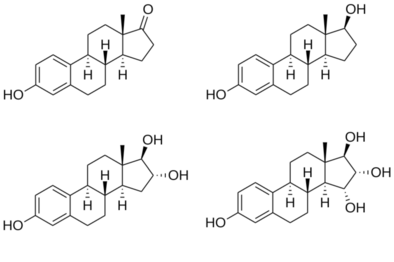
Chemistry
[edit]Estriol, also known as 16α-hydroxyestradiol or as estra-1,3,5(10)-triene-3,16α,17β-triol, is a naturally occurring estrane steroid with double bonds between the C1 and C2, C3 and C4, and C5 and C10 positions and hydroxyl groups at the C3, C16α, and C17β positions.[29][2] The name estriol and the abbreviation E3 were derived from the chemical terms estrin (estra-1,3,5(10)-triene) and triol (three hydroxyl groups).[99]
Analogues
[edit]A variety of analogues of estriol are known, including both naturally occurring isomers and synthetic substituted derivatives and esters.[29][2] 16β-Epiestriol (epiestriol), 17α-epiestriol, and 16β,17α-epiestriol are isomers of estriol that are endogenous weak estrogens.[29] Mytatrienediol (16α-methyl-16β-epiestriol 3-methyl ether) is a synthetic derivative of 16β-epiestriol that was never marketed.[29] Estriol acetate benzoate, estriol succinate, and estriol tripropionate are synthetic estriol esters that have been marketed for medical use, whereas estriol dihexanoate, estriol dipropionate, and estriol triacetate have not been introduced.[29][2] Quinestradol is the 3-cyclopentyl ether of estriol and has also been marketed.[29][2] Polyestriol phosphate, an ester of estriol in the form of a polymer, has been marketed previously as well.[98][100][51][101] These esters, ethers, and polymers are prodrugs of estriol.[4] Ethinylestriol and nilestriol are synthetic C17α ethynylated derivatives of estriol.[29][2] Ethinylestriol has not been marketed, but nilestriol, which is the 3-cyclopentyl ether of ethinylestriol and a prodrug of it, has been.[29][2]
Estetrol (E4), also known as 15α-hydroxyestriol, is a naturally occurring analogue of estriol with an additional hydroxyl group, at the C15α position.[102][103] It is closely related to estriol and has similar but non-identical pharmacological properties.[102][103] Like estriol, estetrol is a relatively weak and atypical estrogen.[102][103] Estetrol is under development for potential clinical use for a variety of indications, such as menopausal hormone therapy and hormonal birth control.[104][105]
History
[edit]Estriol was discovered in 1930.[22][23] Subsequently, it was introduced for medical use in oral and transdermal formulations under brand names such as Estriol, Oestrosalve, Theelol, and Tridestrin.[106][107][108][25][109][110][24] In addition, conjugated estriol, containing mainly estriol glucuronide, was marketed in the 1930s, under the brand names Emmenin and Progynon.[106][108][25][109][111][112] They were the first orally active estrogen preparations to be introduced in medicine.[111][112] In contrast to estrone, free estriol was never introduced for use by intramuscular injection.[113] Estriol continues to be used medically today, widely throughout the world and in a variety of different formulations and brand names.[2][3][6]
Society and culture
[edit]Generic names
[edit]Estriol is the generic name of estriol in American English and its INN, USP, BAN, DCF, and JAN.[29][2][114][3] It is pronounced /ˌɛstraɪoʊl/ ESS-TREE-ohl.[1] Estriolo is the name of estriol in Italian[3] and estriolum is its name in Latin, whereas its name remains unchanged as estriol in Spanish, Portuguese, French, and German.[3][2] Oestriol, in which the "O" is silent, was the former BAN of estriol and its name in British English,[29][114][2] but the spelling was eventually changed to estriol.[3]
Brand names
[edit]Estriol is or has been marketed under a variety of brand names throughout the world, including Aacifemine, Colpogyn, Elinol, Estriel, Estriol, Estriosalbe, Estrokad, Evalon, Gydrelle, Gynäsan, Gynest, Gynoflor (in combination with lactobacilli), Incurin (veterinary), Klimax-E, OeKolp, Oestro-Gynaedron, Orgestriol, Ortho-Gynest, Ovesterin, Ovestin, Ovestinon, Ovestrion, Ovo-Vinces, Pausanol, Physiogine, Sinapause, Synapause, Synapause-E, Trophicrème, Vago-Med, Vacidox, and Xapro.[2][3]
Estriol succinate has been marketed under the brand names Blissel, Evalon, Gelistrol, Hemostyptanon, Orgastyptin, Ovestin, Pausan, Sinapause, Styptanon, Synapsa, Synapasa, Synapausa, and Synapause.[29][2][3] Estriol diacetate benzoate has been marketed under the brand name Holin-Depot and estriol tripropionate has been marketed under the brand name Estriel.[29] Polyestriol phosphate has been marketed under the brand names Gynäsan, Klimadurin, and Triodurin.[100][115][116] Emmenin and Progynon were estriol products marketed in the 1930s which were manufactured from the urine of pregnant women and contained estriol conjugates, primarily estriol glucuronide.[111][112]
Estriol for multiple sclerosis had the tentative brand name Trimesta but did not complete development and was never marketed.[117]
Availability
[edit]Estriol is marketed widely throughout the world, including in Europe, South Africa, Australia, New Zealand, Asia, Latin America, and elsewhere.[2][3] The medication is also available in some countries in the form of estriol succinate, an ester prodrug of estriol.[2][29][118] Estriol and its esters are not approved for use in the United States or Canada, although estriol has been produced and sold by compounding pharmacies in North America for use as a component of bioidentical hormone therapy.[36][119] In addition, topical creams containing estriol are not regulated in the United States and are available over-the-counter in this country.[28]
Research
[edit]Estriol may have immunomodulatory effects and has been of investigational interest in the treatment of multiple sclerosis and a number of other conditions.[18] Estriol succinate was under development for the treatment of multiple sclerosis in the United States and worldwide, and reached phase II clinical trials for this indication, but development was discontinued due to insufficient effectiveness.[117] It had the tentative brand name Trimesta.[117]
Veterinary use
[edit]Estriol is used in veterinary medicine, under the brand name Incurin, in the treatment of urinary incontinence due to estrogen deficiency in dogs.[14][15][16][17] Certain estrogens, like estradiol, can cause bone marrow suppression in dogs, which can be fatal, but estriol appears to pose less or possibly no risk.[17][120]
References
[edit]- ^ a b c Estriol. Dictionary.com.
- ^ a b c d e f g h i j k l m n o p q Index Nominum 2000: International Drug Directory. Taylor & Francis. January 2000. pp. 407–. ISBN 978-3-88763-075-1.
- ^ a b c d e f g h i j k l "Estriol". Archived from the original on 2018-07-05. Retrieved 2018-05-20.
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac ad ae af ag ah ai aj ak al am an ao ap aq ar as at au av aw ax ay az ba bb bc bd be bf bg bh bi bj bk bl bm bn bo bp bq br bs bt bu bv bw bx by bz Kuhl H (August 2005). "Pharmacology of estrogens and progestogens: influence of different routes of administration". Climacteric. 8 (Suppl 1): 3–63. doi:10.1080/13697130500148875. PMID 16112947. S2CID 24616324.
- ^ a b c d e f g h i j k l m n o p q Oettel M, Schillinger E (6 December 2012). Estrogens and Antiestrogens II: Pharmacology and Clinical Application of Estrogens and Antiestrogen. Springer Science & Business Media. pp. 265, 273. ISBN 978-3-642-60107-1.
- ^ a b c d e f g h i j k l m n o Taylor M (December 2001). "Unconventional estrogens: estriol, biest, and triest". Clinical Obstetrics and Gynecology. 44 (4): 864–879. doi:10.1097/00003081-200112000-00024. PMID 11600867. S2CID 27098486.
- ^ a b c d e f g Musey PI, Kirdani RY, Bhanalaph T, Sandberg AA (December 1973). "Estriol metabolism in the baboon: analysis of urinary and biliary metabolites". Steroids. 22 (6): 795–817. doi:10.1016/0039-128X(73)90054-8. PMID 4203562.
- ^ a b c Dörwald FZ (4 February 2013). "Steroids". Lead Optimization for Medicinal Chemists: Pharmacokinetic Properties of Functional Groups and Organic Compounds. John Wiley & Sons. pp. 486–. ISBN 978-3-527-64565-7.
- ^ a b Wentz AC (January 1988). Gynecologic Endocrinology and Infertility for the House Officer. Williams & Wilkins. ISBN 978-0-683-08931-8.
Estriol is considered a short-acting estrogen with a half-life of 5 hours.
- ^ a b Visser M, Holinka CF, Coelingh Bennink HJ (2008). "First human exposure to exogenous single-dose oral estetrol in early postmenopausal women". Climacteric. 11 (Suppl 1): 31–40. doi:10.1080/13697130802056511. PMID 18464021. S2CID 23568599.
- ^ a b Applied Biochemistry of Clinical Disorders (2nd ed.). University of California. 1986. ISBN 978-0-397-50768-9.
Because its half-life is about 20 minutes, unconjugated estriol rapidly reflects changes in estriol production.
- ^ a b c d e f g h i j k l m n Rueda C, Osorio AM, Avellaneda AC, Pinzón CE, Restrepo OI (August 2017). "The efficacy and safety of estriol to treat vulvovaginal atrophy in postmenopausal women: a systematic literature review". Climacteric. 20 (4): 321–330. doi:10.1080/13697137.2017.1329291. PMID 28622049. S2CID 407950.
- ^ a b c Zutshi V, Rathore AM, Sharma K (1 January 2005). Hormones in Obstetrics and Gynaecology. Jaypee Brothers Publishers. pp. 101–. ISBN 978-81-8061-427-9.
- ^ a b Ettinger SJ, Feldman EC, Cote E (11 January 2017). Textbook of Veterinary Internal Medicine - eBook. Elsevier Health Sciences. pp. 6017, 6380. ISBN 978-0-323-31239-4.
- ^ a b Boothe DM (25 July 2011). Small Animal Clinical Pharmacology and Therapeutics - E-Book. Elsevier Health Sciences. pp. 2350–2351. ISBN 978-1-4377-2357-1.
- ^ a b c d e Bonagura JD, Twedt DC (10 July 2008). Kirk's Current Veterinary Therapy XIV - E-Book. Elsevier Health Sciences. pp. 772, 4442. ISBN 978-1-4377-1152-3.
- ^ a b c d e f Papich MG (1 October 2015). Saunders Handbook of Veterinary Drugs: Small and Large Animal. Elsevier Health Sciences. pp. 304–. ISBN 978-0-323-24485-5.
- ^ a b c d e f g h i j k l m n o p Ali ES, Mangold C, Peiris AN (September 2017). "Estriol: emerging clinical benefits". Menopause. 24 (9): 1081–1085. doi:10.1097/GME.0000000000000855. PMID 28375935. S2CID 41137736.
- ^ a b c d Carr BC (2001). "The maternal-fetal-placental unit.". In Becker KL (ed.). Principles and Practice of Endocrinology and Metabolism. Lippincott Williams & Wilkins. pp. 932, 989, 1061. ISBN 978-0-7817-1750-2.
- ^ a b Clark JH, Markaverich BM (1983). "The agonistic and antagonistic effects of short acting estrogens: a review". Pharmacology & Therapeutics. 21 (3): 429–453. doi:10.1016/0163-7258(83)90063-3. PMID 6356176.
- ^ a b c d e f g h i j Clark JH, Markaverich BM (April 1984). "The agonistic and antagonistic actions of estriol". Journal of Steroid Biochemistry. 20 (4B): 1005–1013. doi:10.1016/0022-4731(84)90011-6. PMID 6202959.
- ^ a b Josimovich JB (11 November 2013). Gynecologic Endocrinology. Springer Science & Business Media. pp. 31–. ISBN 978-1-4613-2157-6.
- ^ a b Sartorelli AC, Johns DG (27 November 2013). Antineoplastic and Immunosuppressive Agents. Springer Science & Business Media. pp. 104–. ISBN 978-3-642-65806-8.
- ^ a b Merrill RC (July 1958). "Estriol: a review". Physiological Reviews. 38 (3): 463–480. doi:10.1152/physrev.1958.38.3.463. PMID 13567043.
- ^ a b c Fluhmann CF (November 1938). "Estrogenic Hormones: Their Clinical Usage". California and Western Medicine. 49 (5): 362–366. PMC 1659459. PMID 18744783.
- ^ a b c Vooijs GP, Geurts TB (September 1995). "Review of the endometrial safety during intravaginal treatment with estriol". European Journal of Obstetrics, Gynecology, and Reproductive Biology. 62 (1): 101–106. doi:10.1016/0301-2115(95)02170-c. hdl:2066/21059. PMID 7493689.
- ^ "Estriol/Lactobacillus - Acerus Pharmaceuticals/Medinova -". AdisInsight. Springer Nature Switzerland AG.
- ^ a b Cirigliano M (June 2007). "Bioidentical hormone therapy: a review of the evidence". Journal of Women's Health. 16 (5): 600–631. doi:10.1089/jwh.2006.0311. PMID 17627398.
- ^ a b c d e f g h i j k l m n o Elks J (14 November 2014). The Dictionary of Drugs: Chemical Data: Chemical Data, Structures and Bibliographies. Springer. pp. 899–. ISBN 978-1-4757-2085-3.
- ^ Mazer C, Israel SL, Charny CW (1946). Diagnosis and treatment of menstrual disorders and sterility. Hoeber. p. 525.
8. PREPARATIONS OF ESTRIOL. Estriol is the least active of all commercially available natural estrogenic substances. A milligram of estriol yields approximately 350 Allen-Doisy rat units. Estriol (Abbott). Capsules containing 0.06, 0.12, and 0.24 mg. Estriol (Lilly). Puvules containing 0.06, 0.12, and 0.24 mg. Theelol (Parke-Davis). Capsules containing 0.06, 0.12, and 0.24 mg.
- ^ Barr DP (1940). Modern Medical Therapy in General Practice. William & Wilkins Company. p. 194. ISBN 978-0-598-66833-2.
Estriol. Estriol (theelol) is trihydroxyestrin. It is a crystalline estrogenic steroid obtained from the urine of pregnant women. It is less actively estrogenic than estrone. Several pharmaceutical houses supply capsules containing 0.06 or 0.12 mg. These may be obtained as Theelol (Parke-Davis), Estriol (Abbott), and Estriol (Lilly).
- ^ Sollmann TH (1948). A manual of pharmacology and its applications to therapeutics and toxicology. W. B. Saunders.
Estriol (Theelol), N.N.R.; characters and solubility as for estrone; considerably less potent. Marketed as capsules of 0.06, 0.12 and 0.24 mg. Dose, 0.06 to 0.12 mg. once to four times daily.
- ^ Council on Drugs (American Medical Association) (1950). New and Nonofficial Drugs. Lippincott. p. 322.
Abbott Laboratories Capsules Estriol: 0.12 mg. and 0.24 mg. Eli Lilly and Company Pulvules Estriol: 0.06 mg., 0.12 mg. and 0.24 mg. Parke, Davis & Company Kapseals Theelol: 0.24 mg.
- ^ New York State Journal of Medicine. Medical Society of the State of New York. 1939. p. 1760.
- ^ Lauritzen C (1988). "Natürliche und Synthetische Sexualhormone – Biologische Grundlagen und Behandlungsprinzipien" [Natural and Synthetic Sexual Hormones – Biological Basis and Medical Treatment Principles]. In Schneider HP, Lauritzen C, Nieschlag E (eds.). Grundlagen und Klinik der Menschlichen Fortpflanzung [Foundations and Clinic of Human Reproduction] (in German). Walter de Gruyter. pp. 229–306. ISBN 978-3-11-010968-9. OCLC 35483492.
- ^ a b Fugh-Berman A, Bythrow J (July 2007). "Bioidentical hormones for menopausal hormone therapy: variation on a theme". Journal of General Internal Medicine. 22 (7): 1030–1034. doi:10.1007/s11606-007-0141-4. PMC 2219716. PMID 17549577.
- ^ Greenblatt RB, Natrajan PK, Aksu MF, Tzingounis VA (January 1980). "The fate of a large bolus of exogenous estrogen administered to postmenopausal women". Maturitas. 2 (1): 29–35. doi:10.1016/0378-5122(80)90057-2. PMID 6250009.
- ^ Adlercreutz H, Martin F, Wahlroos O, Soini E (1975). "Mass spectrometric and mass fragmentographic determination of natural and synthetic steroids in biological fluids". Journal of Steroid Biochemistry. 6 (3–4): 247–259. doi:10.1016/0022-4731(75)90140-5. PMID 1186230.
- ^ Pocket Books (2005). The PDR Pocket Guide to Prescription Drugs. Simon and Schuster. pp. 1540–. ISBN 978-1-4165-1085-7.
- ^ Bratman S (2003). Mosby's Handbook of Herbs and Supplements and Their Therapeutic Uses. Mosby/Healthgate. ISBN 978-0-323-02015-2.
- ^ a b c Jaouen G, Top S, McGlinchey MJ (20 April 2015). "The Biological Target Potential of Organometallic Steroids". In Jaouen G, Salmain M (eds.). Bioorganometallic Chemistry: Applications in Drug Discovery, Biocatalysis, and Imaging. John Wiley & Sons. pp. 45–. ISBN 978-3-527-33527-5.
- ^ a b c d Escande A, Pillon A, Servant N, Cravedi JP, Larrea F, Muhn P, et al. (May 2006). "Evaluation of ligand selectivity using reporter cell lines stably expressing estrogen receptor alpha or beta". Biochemical Pharmacology. 71 (10): 1459–1469. doi:10.1016/j.bcp.2006.02.002. PMID 16554039.
- ^ Prossnitz ER, Arterburn JB (July 2015). "International Union of Basic and Clinical Pharmacology. XCVII. G Protein-Coupled Estrogen Receptor and Its Pharmacologic Modulators". Pharmacological Reviews. 67 (3): 505–540. doi:10.1124/pr.114.009712. PMC 4485017. PMID 26023144.
- ^ a b c d Lappano R, Rosano C, De Marco P, De Francesco EM, Pezzi V, Maggiolini M (May 2010). "Estriol acts as a GPR30 antagonist in estrogen receptor-negative breast cancer cells". Molecular and Cellular Endocrinology. 320 (1–2): 162–170. doi:10.1016/j.mce.2010.02.006. PMID 20138962. S2CID 24525995.
- ^ a b Girgert R, Emons G, Gründker C (December 2014). "Inhibition of GPR30 by estriol prevents growth stimulation of triple-negative breast cancer cells by 17β-estradiol". BMC Cancer. 14 (1): 935. doi:10.1186/1471-2407-14-935. PMC 4364648. PMID 25496649.
- ^ Raynaud JP, Ojasoo T, Bouton MM (1979). "Receptor Binding as a Tool in the Development of New Bioactive Steroids". Drug Design. Medicinal Chemistry: A Series of Monographs. 11: 169–214. doi:10.1016/B978-0-12-060308-4.50010-X. ISBN 978-0-12-060308-4.
- ^ Ojasoo T, Raynaud JP (November 1978). "Unique steroid congeners for receptor studies". Cancer Research. 38 (11 Pt 2): 4186–4198. PMID 359134.
- ^ Ojasoo T, Delettré J, Mornon JP, Turpin-VanDycke C, Raynaud JP (1987). "Towards the mapping of the progesterone and androgen receptors". Journal of Steroid Biochemistry. 27 (1–3): 255–269. doi:10.1016/0022-4731(87)90317-7. PMID 3695484.
- ^ Raynaud JP, Bouton MM, Moguilewsky M, Ojasoo T, Philibert D, Beck G, et al. (January 1980). "Steroid hormone receptors and pharmacology". Journal of Steroid Biochemistry. 12: 143–157. doi:10.1016/0022-4731(80)90264-2. PMID 7421203.
- ^ Dunn JF, Nisula BC, Rodbard D (July 1981). "Transport of steroid hormones: binding of 21 endogenous steroids to both testosterone-binding globulin and corticosteroid-binding globulin in human plasma". The Journal of Clinical Endocrinology and Metabolism. 53 (1): 58–68. doi:10.1210/jcem-53-1-58. PMID 7195404.
- ^ a b c Labhart A (6 December 2012). Clinical Endocrinology: Theory and Practice. Springer Science & Business Media. pp. 548, 551. ISBN 978-3-642-96158-8.
The polymer of estradiol or estriol and phosphoric acid has an excellent depot action when given intramuscularly (polyestriol phosphate or polyestradiol phosphate) (Table 16). Phosphoric acid combines with the estrogen molecule at C3 and C17 to form a macromolecule. The compound is stored in the liver and spleen where the estrogen is steadily released by splitting off of the phosphate portion due to the action of alkaline phosphatase. [...] Conjugated estrogens and polyestriol and estradiol phosphate can also be given intravenously in an aqueous solution. Intravenous administration of ovarian hormones offers no advantages, however, and therefore has no practical significance. [...] The following duarations of action have been obtained with a single administration (WlED, 1954; LAURITZEN, 1968): [...] 50 mg polyestradiol phosphate ~ 1 month; 50 mg polyestriol phosphate ~ 1 month; 80 mg polyestriol phosphate ~ 2 months.
- ^ a b c d e f g Kuhl H (September 1990). "Pharmacokinetics of oestrogens and progestogens". Maturitas. 12 (3): 171–197. doi:10.1016/0378-5122(90)90003-O. PMID 2170822.
- ^ Nelson WO (1936). "Endocrine Control of the Mammary Gland". Physiological Reviews. 16 (3): 488–526. doi:10.1152/physrev.1936.16.3.488. ISSN 0031-9333.
- ^ Martinez-Manautou J, Rudel HW (1966). "Antiovulatory Activity of Several Synthetic and Natural Estrogens". In Greenblatt RB (ed.). Ovulation: Stimulation, Suppression, and Detection. Lippincott. pp. 243–253. ISBN 978-0-397-59010-0.
- ^ Herr F, Revesz C, Manson AJ, Jewell JB (1970). "Biological Properties of Estrogen Sulfates". In Bernstein S, Solomon S (eds.). Chemical and Biological Aspects of Steroid Conjugation. Springer. pp. 368–408. doi:10.1007/978-3-642-95177-0. ISBN 978-3-642-49506-9.
- ^ a b c Clark JH, Peck EJ (1979). "Control of Steroid Receptor Levels and Steroid Antagonism". Female Sex Steroids: Receptors and Function. Monographs on Endocrinology. Vol. 14. Springer. pp. 99–134. doi:10.1007/978-3-642-81339-9_6. ISBN 978-3-642-81341-2. ISSN 0077-1015. PMID 390365.
- ^ a b c Clark JH, Paszko Z, Peck EJ (January 1977). "Nuclear binding and retention of the receptor estrogen complex: relation to the agonistic and antagonistic properties of estriol". Endocrinology. 100 (1): 91–96. doi:10.1210/endo-100-1-91. PMID 830547.
- ^ Rabe T, Runnebaum B, Kellermeier-Wittlinger S (17 April 2013). "Hormontherapie". In Runnebaum B, Rabe T (eds.). Gynäkologische Endokrinologie und Fortpflanzungsmedizin: Band 1: Gynäkologische Endokrinologie. Springer-Verlag. pp. 88–. ISBN 978-3-662-07635-4.
- ^ Kopera H (1991). "Hormone der Gonaden". Hormonelle Therapie für die Frau. Kliniktaschenbücher. Springer. pp. 59–124. doi:10.1007/978-3-642-95670-6_6. ISBN 978-3-540-54554-5. ISSN 0172-777X.
- ^ Hellberg D, Nilsson S (April 1984). "Comparison of a triphasic oestradiol/norethisterone acetate preparation with and without an oestriol component in the treatment of climacteric complaints". Maturitas. 5 (4): 233–243. doi:10.1016/0378-5122(84)90016-1. PMID 6429481.
- ^ Lauritzen C (September 1990). "Clinical use of oestrogens and progestogens". Maturitas. 12 (3): 199–214. doi:10.1016/0378-5122(90)90004-P. PMID 2215269.
- ^ Lauritzen C (June 1977). "[Estrogen thearpy in practice. 3. Estrogen preparations and combination preparations]" [Estrogen therapy in practice. 3. Estrogen preparations and combination preparations]. Fortschritte Der Medizin (in German). 95 (21): 1388–92. PMID 559617.
- ^ Wolf AS, Schneider HP (12 March 2013). Östrogene in Diagnostik und Therapie. Springer-Verlag. pp. 78–. ISBN 978-3-642-75101-1.
- ^ Göretzlehner G, Lauritzen C, Römer T, Rossmanith W (1 January 2012). Praktische Hormontherapie in der Gynäkologie. Walter de Gruyter. pp. 44–. ISBN 978-3-11-024568-4.
- ^ Knörr K, Beller FK, Lauritzen C (17 April 2013). Lehrbuch der Gynäkologie. Springer-Verlag. pp. 212–213. ISBN 978-3-662-00942-0.
- ^ Horský J, Presl J (1981). "Hormonal Treatment of Disorders of the Menstrual Cycle". In Horsky J, Presl J (eds.). Ovarian Function and its Disorders: Diagnosis and Therapy. Springer Science & Business Media. pp. 309–332. doi:10.1007/978-94-009-8195-9_11. ISBN 978-94-009-8195-9.
- ^ Pschyrembel W (1968). Praktische Gynäkologie: für Studierende und Ärzte. Walter de Gruyter. pp. 598–599. ISBN 978-3-11-150424-7.
- ^ Lauritzen CH (January 1976). "The female climacteric syndrome: significance, problems, treatment". Acta Obstetricia Et Gynecologica Scandinavica. Supplement. 51: 47–61. doi:10.3109/00016347509156433. PMID 779393.
- ^ Lauritzen C (1975). "The Female Climacteric Syndrome: Significance, Problems, Treatment". Acta Obstetricia et Gynecologica Scandinavica. 54 (s51): 48–61. doi:10.3109/00016347509156433. ISSN 0001-6349.
- ^ Kopera H (1991). "Hormone der Gonaden". Hormonelle Therapie für die Frau. Kliniktaschenbücher. pp. 59–124. doi:10.1007/978-3-642-95670-6_6. ISBN 978-3-540-54554-5. ISSN 0172-777X.
- ^ Scott WW, Menon M, Walsh PC (April 1980). "Hormonal Therapy of Prostatic Cancer". Cancer. 45 (Suppl 7): 1929–1936. doi:10.1002/cncr.1980.45.s7.1929. PMID 29603164.
- ^ Leinung MC, Feustel PJ, Joseph J (2018). "Hormonal Treatment of Transgender Women with Oral Estradiol". Transgender Health. 3 (1): 74–81. doi:10.1089/trgh.2017.0035. PMC 5944393. PMID 29756046.
- ^ Ryden AB (1950). "Natural and synthetic oestrogenic substances; their relative effectiveness when administered orally". Acta Endocrinologica. 4 (2): 121–39. doi:10.1530/acta.0.0040121. PMID 15432047.
- ^ Ryden AB (1951). "The effectiveness of natural and synthetic oestrogenic substances in women". Acta Endocrinologica. 8 (2): 175–91. doi:10.1530/acta.0.0080175. PMID 14902290.
- ^ Kottmeier HL (1947). "Ueber blutungen in der menopause: Speziell der klinischen bedeutung eines endometriums mit zeichen hormonaler beeinflussung: Part I". Acta Obstetricia et Gynecologica Scandinavica. 27 (s6): 1–121. doi:10.3109/00016344709154486. ISSN 0001-6349.
There is no doubt that the conversion of the endometrium with injections of both synthetic and native estrogenic hormone preparations succeeds, but the opinion whether native, orally administered preparations can produce a proliferation mucosa changes with different authors. PEDERSEN-BJERGAARD (1939) was able to show that 90% of the folliculin taken up in the blood of the vena portae is inactivated in the liver. Neither KAUFMANN (1933, 1935), RAUSCHER (1939, 1942) nor HERRNBERGER (1941) succeeded in bringing a castration endometrium into proliferation using large doses of orally administered preparations of estrone or estradiol. Other results are reported by NEUSTAEDTER (1939), LAUTERWEIN (1940) and FERIN (1941); they succeeded in converting an atrophic castration endometrium into an unambiguous proliferation mucosa with 120–300 oestradiol or with 380 oestrone.
- ^ Rietbrock N, Staib AH, Loew D (11 March 2013). Klinische Pharmakologie: Arzneitherapie. Springer-Verlag. pp. 426–. ISBN 978-3-642-57636-2.
- ^ Martinez-Manautou J, Rudel HW (1966). "Antiovulatory Activity of Several Synthetic and Natural Estrogens". In Robert Benjamin Greenblatt (ed.). Ovulation: Stimulation, Suppression, and Detection. Lippincott. pp. 243–253.
- ^ Herr F, Revesz C, Manson AJ, Jewell JB (1970). "Biological Properties of Estrogen Sulfates". Chemical and Biological Aspects of Steroid Conjugation. pp. 368–408. doi:10.1007/978-3-642-49793-3_8. ISBN 978-3-642-49506-9.
- ^ Duncan CJ, Kistner RW, Mansell H (October 1956). "Suppression of ovulation by trip-anisyl chloroethylene (TACE)". Obstetrics and Gynecology. 8 (4): 399–407. PMID 13370006.
- ^ Clark JH, Paszko Z, Peck EJ (January 1977). "Nuclear binding and retention of the receptor estrogen complex: relation to the agonistic and antagonistic properties of estriol". Endocrinology. 100 (1): 91–96. doi:10.1210/endo-100-1-91. PMID 830547.
- ^ Clark JH, Hardin JW, McCormack SA (1979). "Mechanism of action of estrogen agonists and antagonists". Journal of Animal Science. 49 Suppl 2: 46–65. doi:10.1093/ansci/49.supplement_ii.46. PMID 400777.
- ^ Lunan CB, Klopper A (September 1975). "Antioestrogens. A review". Clinical Endocrinology. 4 (5): 551–572. doi:10.1111/j.1365-2265.1975.tb01568.x. PMID 170029. S2CID 9628572.
- ^ Rabe T, Runnebaum B, Kellermeier-Wittlinger S (1994). "Hormontherapie" [Hormone Therapy]. In Runnebaum B, Rabe T (eds.). Gynäkologische Endokrinologie und Fortpflanzungsmedizin: Band 1: Gynäkologische Endokrinologie [Gynecological Endocrinology and Reproductive Medicine: Volume 1: Gynecological Endocrinology]. pp. 63–147. doi:10.1007/978-3-662-07635-4_3. ISBN 978-3-662-07635-4.
- ^ Clark JH, Markaverich BM (1983). "The agonistic and antagonistic effects of short acting estrogens: a review". Pharmacology & Therapeutics. 21 (3): 429–453. doi:10.1016/0163-7258(83)90063-3. PMID 6356176.
- ^ Clark JH, Markaverich BM (April 1984). "The agonistic and antagonistic actions of estriol". Journal of Steroid Biochemistry. 20 (4B): 1005–1013. doi:10.1016/0022-4731(84)90011-6. PMID 6202959.
- ^ Terenius L, Ljungkvist I (1972). "Aspects on the mode of action of antiestrogens and antiprogestogens". Gynecologic Investigation. 3 (1): 96–107. doi:10.1159/000301746. PMID 4347201.
- ^ a b Moran DJ, McGarrigle HH, Lachelin GC (January 1994). "Maternal plasma progesterone levels fall after rectal administration of estriol". The Journal of Clinical Endocrinology and Metabolism. 78 (1): 70–72. doi:10.1210/jcem.78.1.8288717. PMID 8288717.
- ^ Norman AW, Litwack G (23 October 1997). Hormones. Academic Press. pp. 398–. ISBN 978-0-08-053413-8.
- ^ Kurjak A, Chervenak FA (25 September 2006). Textbook of Perinatal Medicine, Second Edition. CRC Press. pp. 699–. ISBN 978-1-4398-1469-7.
- ^ Greene MF, Creasy RK, Resnik R, Iams JD, Lockwood CJ, Moore T (25 November 2008). Creasy and Resnik's Maternal-Fetal Medicine: Principles and Practice E-Book. Elsevier Health Sciences. pp. 115–. ISBN 978-1-4377-2135-5.
- ^ a b Wiegerinck MA, Poortman J, Donker TH, Thijssen JH (January 1983). "In vivo uptake and subcellular distribution of tritium-labeled estrogens in human endometrium, myometrium, and vagina". The Journal of Clinical Endocrinology and Metabolism. 56 (1): 76–86. doi:10.1210/jcem-56-1-76. PMID 6847874.
- ^ Buchsbaum HJ (6 December 2012). The Menopause. Springer Science & Business Media. pp. 62–. ISBN 978-1-4612-5525-3.
- ^ a b Lorenzo J, Horowitz M, Choi Y, Takayanagi H, Schett G (23 September 2015). Osteoimmunology: Interactions of the Immune and Skeletal Systems. Elsevier Science. pp. 216–. ISBN 978-0-12-800627-6.
- ^ Anderson JN, Peck EJ, Clark JH (April 1974). "Nuclear receptor-estrogen complex: in vivo and in vitro binding of estradiol and estriol as influenced by serum albumin". Journal of Steroid Biochemistry. 5 (2): 103–107. doi:10.1016/0022-4731(74)90114-9. PMID 4366454.
- ^ van Haaften M, Donker GH, Tas AA, Gramberg LG, Blankenstein MA, Thijssen JH (September 1988). "Identification of 16 alpha-hydroxy-estrone as a metabolite of estriol". Gynecological Endocrinology. 2 (3): 215–221. doi:10.3109/09513599809029346. PMID 3227988.
- ^ Thijssen JH, Blankenstein MA (1990). "Uptake and metabolism of estradiol by normal and abnormal breast tissues". Annals of the New York Academy of Sciences. 586 (1): 252–258. Bibcode:1990NYASA.586..252T. doi:10.1111/j.1749-6632.1990.tb17813.x. PMID 2357005. S2CID 35881837.
- ^ Brown JB (December 1957). "The relationship between urinary oestrogens and oestrogens produced in the body". The Journal of Endocrinology. 16 (2): 202–212. doi:10.1677/joe.0.0160202. PMID 13491750.
- ^ a b Lauritzen C, Velibese S (September 1961). "Clinical investigations of a long-acting oestriol (polyoestriol phosphate)". Acta Endocrinologica. 38 (1): 73–87. doi:10.1530/acta.0.0380073. PMID 13759555.
- ^ Cole LA, Kramer PR (13 October 2015). Human Physiology, Biochemistry and Basic Medicine. Elsevier Science. pp. 122–. ISBN 978-0-12-803717-1.
- ^ a b Bachmann FF (January 1971). "[Treatment of menopausal complants with polyoestriol-phosphate. Experiences with Gynäsan injections]" [Treatment of menopausal complants with polyoestriol-phosphate. Experiences with Gynäsan injections]. Munchener Medizinische Wochenschrift (in German). 113 (5): 166–169. PMID 5107471.
- ^ Campbell S (6 December 2012). The Management of the Menopause & Post-Menopausal Years: The Proceedings of the International Symposium held in London 24–26 November 1975 Arranged by the Institute of Obstetrics and Gynaecology, The University of London. Springer Science & Business Media. pp. 395–. ISBN 978-94-011-6165-7.
In the Federal Republic of Germany between 10 and 20% of all climacteric women are on estrogen treatment. We have the following oral estrogens for a treatment. (t) Conjugated estrogens, (2) estradiol valerate, (3) ethinyl-estradiol and its cyclopentyl-enol ether, (4) stilbestrol, (5) ethinyl-estradiol-methyltestosterone, (6) estriol and estriol succinate, most of them as coated tablets. Several long acting injectable preparations are available: several esters of combined estradiol-testosterone, one of estradiol-dehydroepiandrosterone enanthate and a prolonged polyestriol phosphate are also available. Lastly, depot injections of estradiol- and stilbestrol-esters are on the market.
- ^ a b c Coelingh Bennink HJ, Holinka CF, Diczfalusy E (2008). "Estetrol review: profile and potential clinical applications". Climacteric. 11 (Suppl 1): 47–58. doi:10.1080/13697130802073425. PMID 18464023. S2CID 24003341.
- ^ a b c Visser M, Coelingh Bennink HJ (March 2009). "Clinical applications for estetrol". The Journal of Steroid Biochemistry and Molecular Biology. 114 (1–2): 85–89. doi:10.1016/j.jsbmb.2008.12.013. PMID 19167495. S2CID 32081001.
- ^ "Estetrol - Mithra Pharmaceuticals/Pantarhei Bioscience". AdisInsight. Springer Nature Switzerland AG.
- ^ "Drospirenone/Estetrol - Mithra Pharmaceuticals". AdisInsight. Springer Nature Switzerland AG.
- ^ a b Greene RR (1941). "Endocrine Therapy for Gynecologic Disorders". Medical Clinics of North America. 25 (1): 155–168. doi:10.1016/S0025-7125(16)36624-X. ISSN 0025-7125.
- ^ Johnstone RW (November 1936). "Sex Hormone Therapy in Gynæcology". Edinburgh Medical Journal. 43 (11): 680–695. PMC 5303355. PMID 29648134.
- ^ a b Reilly WA (November 1941). "Estrogens: Their Use in Pediatrics". California and Western Medicine. 55 (5): 237–239. PMC 1634235. PMID 18746057.
- ^ a b Fluhmann CF (1944). "Clinical Use of Extracts from the Ovaries". Journal of the American Medical Association. 125 (1): 1. doi:10.1001/jama.1944.02850190003001. ISSN 0002-9955.
- ^ Macpherson AI (June 1940). "The Use of Œstrogens in Obstetrics and Gynæcology". Edinburgh Medical Journal. 47 (6): 406–424. PMC 5306594. PMID 29646930.
- ^ a b c Rooke T (1 January 2012). The Quest for Cortisone. MSU Press. pp. 54–. ISBN 978-1-60917-326-5.
- ^ a b c Grant GA, Beall D (22 October 2013). "Studies on estrogen conjugates". In Pincus G (ed.). Recent Progress in Hormone Research: The Proceedings of the Laurentian Hormone Conference. Elsevier Science. pp. 307–. ISBN 978-1-4832-1945-5.
- ^ Cantor EB (September 1956). "A survey of estrogens". Postgraduate Medicine. 20 (3): 224–231. doi:10.1080/00325481.1956.11691266. PMID 13359169.
- ^ a b Morton IK, Hall JM (6 December 2012). Concise Dictionary of Pharmacological Agents: Properties and Synonyms. Springer Science & Business Media. pp. 206, 905. ISBN 978-94-011-4439-1.
- ^ Negwer M, Scharnow HG (4 October 2001). Organic-chemical drugs and their synonyms: (an international survey). Wiley-VCH. ISBN 978-3-527-30247-5.
8075-01 (6628-01) 37452-43-0 R Polymeric ester with phosphoric acid S Klimadurin, Polyestriol phosphate, Polyostriolphosphat, Triodurin U Depot-estrogen
- ^ Martindale W, et al. (Royal Pharmaceutical Society of Great Britain. Dept. of Pharmaceutical Sciences) (1993). The Extra Pharmacopoeia. Pharmaceutical Press. p. 2258. ISBN 978-0-85369-300-0.
Polyoestriol Phosphate. [...] ingredient of Klimadurin. [...] Triodurin [...].
- ^ a b c "Estriol succinate - Synthetic Biologics". AdisInsight. Springer Nature Switzerland AG.
- ^ Platt D (6 December 2012). Geriatrics 3: Gynecology · Orthopaedics · Anesthesiology · Surgery · Otorhinolaryngology · Ophthalmology · Dermatology. Springer Science & Business Media. pp. 6–. ISBN 978-3-642-68976-5.
- ^ Files JA, Ko MG, Pruthi S (July 2011). "Bioidentical hormone therapy". Mayo Clinic Proceedings. 86 (7): 673–80, quiz 680. doi:10.4065/mcp.2010.0714. PMC 3127562. PMID 21531972.
- ^ Feldman EC, Nelson RW (1 January 2004). Canine and Feline Endocrinology and Reproduction. Elsevier Health Sciences. pp. 839–. ISBN 0-7216-9315-6.
Further reading
[edit]- Merrill RC (July 1958). "Estriol: a review". Physiological Reviews. 38 (3): 463–480. doi:10.1152/physrev.1958.38.3.463. PMID 13567043.
- Clark JH, Hardin JW, McCormack SA (1979). "Mechanism of action of estrogen agonists and antagonists". Journal of Animal Science. 49 (Suppl 2): 46–65. doi:10.1093/ansci/49.supplement_ii.46. PMID 400777.
- Clark JH, Markaverich BM (1983). "The agonistic and antagonistic effects of short acting estrogens: a review". Pharmacology & Therapeutics. 21 (3): 429–453. doi:10.1016/0163-7258(83)90063-3. PMID 6356176.
- Clark JH, Markaverich BM (April 1984). "The agonistic and antagonistic actions of estriol". Journal of Steroid Biochemistry. 20 (4B): 1005–1013. doi:10.1016/0022-4731(84)90011-6. PMID 6202959.
- Heimer GM (1987). "Estriol in the postmenopause". Acta Obstetricia et Gynecologica Scandinavica. Supplement. 139: 2–23. doi:10.3109/00016348709156470. PMID 3475930. S2CID 38712328.
- Esposito G (June 1991). "Estriol: a weak estrogen or a different hormone?". Gynecological Endocrinology. 5 (2): 131–153. doi:10.3109/09513599109028436. PMID 1927578.
- Vooijs GP, Geurts TB (September 1995). "Review of the endometrial safety during intravaginal treatment with estriol". European Journal of Obstetrics, Gynecology, and Reproductive Biology. 62 (1): 101–106. doi:10.1016/0301-2115(95)02170-c. hdl:2066/21059. PMID 7493689.
- Head KA (April 1998). "Estriol: safety and efficacy" (PDF). Alternative Medicine Review. 3 (2): 101–113. PMID 9577246.
- Taylor M (December 2001). "Unconventional estrogens: estriol, biest, and triest". Clinical Obstetrics and Gynecology. 44 (4): 864–879. doi:10.1097/00003081-200112000-00024. PMID 11600867. S2CID 27098486.
- Ciszko B, Zdrojewicz Z (July 2006). "[Compliance endogenous and exogenous estriol in clinical practice]" [Compliance endogenous and exogenous estriol in clinical practice]. Ginekologia Polska (in Polish). 77 (7): 559–565. PMID 17076208.
- Perepanova TS, Khazan PL (2007). "[The role of estriol in therapy of urogenital disorders in postmenopausal women]". Urologiia (in Russian) (3): 102–4, 107. PMID 17722629.
- Holtorf K (January 2009). "The bioidentical hormone debate: are bioidentical hormones (estradiol, estriol, and progesterone) safer or more efficacious than commonly used synthetic versions in hormone replacement therapy?". Postgraduate Medicine. 121 (1): 73–85. doi:10.3810/pgm.2009.01.1949. PMID 19179815. S2CID 2060730.
- Unlü C, Donders G (2011). "Use of lactobacilli and estriol combination in the treatment of disturbed vaginal ecosystem: a review". Journal of the Turkish German Gynecological Association. 12 (4): 239–246. doi:10.5152/jtgga.2011.57. PMC 3939257. PMID 24592002.
- Ali ES, Mangold C, Peiris AN (September 2017). "Estriol: emerging clinical benefits". Menopause. 24 (9): 1081–1085. doi:10.1097/GME.0000000000000855. PMID 28375935. S2CID 41137736.
- Rueda C, Osorio AM, Avellaneda AC, Pinzón CE, Restrepo OI (August 2017). "The efficacy and safety of estriol to treat vulvovaginal atrophy in postmenopausal women: a systematic literature review". Climacteric. 20 (4): 321–330. doi:10.1080/13697137.2017.1329291. PMID 28622049. S2CID 407950.
- Mueck AO, Ruan X, Prasauskas V, Grob P, Ortmann O (April 2018). "Treatment of vaginal atrophy with estriol and lactobacilli combination: a clinical review". Climacteric. 21 (2): 140–147. doi:10.1080/13697137.2017.1421923. PMID 29381086.
- La Rosa VL, Ciebiera M, Lin LT, Fan S, Butticè S, Sathyapalan T, et al. (June 2019). "Treatment of genitourinary syndrome of menopause: the potential effects of intravaginal ultralow-concentration oestriol and intravaginal dehydroepiandrosterone on quality of life and sexual function". Przeglad Menopauzalny = Menopause Review. 18 (2): 116–122. doi:10.5114/pm.2019.86836. PMC 6719636. PMID 31488961.