Interleukin 26
Interleukin-26 (IL-26) is a protein that in humans is encoded by the IL26 gene.[3][4][5]
IL-26 is the most recently identified member of the IL-20 cytokine subfamily,[6] which was formed according to the usage of common receptor subunits and similarities in target-cell profiles and functions. All cytokines belonging to this subfamily are members of the larger IL-10 family. IL-26 is expressed in certain herpesvirus-transformed T cells but not in primary stimulated T cells.[4] IL-26 signals through a receptor complex comprising two distinct proteins called IL-20 receptor 1 and IL-10 receptor 2.[7] By signaling through this receptor complex, IL-26 induces rapid phosphorylation of the transcription factors STAT1 and STAT3, which enhance IL-10 and IL-8 secretion and as expression of the CD54 molecule on the surface of epithelial cells.[8]
Gene organization and protein structure
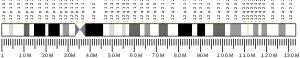
The IL26 gene is conserved in various vertebrates, but it is curiously absent in mice and rats. Paralogs of this gene have been identified in several non-mammalian species.[9] The human gene is located on chromosome 12 (12q15), between the genes encoding IL-22 and IFNγ,[10] and composed of five exons separated by three introns. This genomic cluster of genes encoding IL-22, IL-26, and IFNγ is present among all vertebrates.[11]
IL-26 is a 171-amino acid protein that exhibits six alpha helices connected by loops and four conserved cysteine residues. Endogenous IL-26 is expressed as a 36 kDa homodimer.[4] Originally named AK155, IL-26 was categorized in the IL-10 cytokine family due to sequence homology and secondary structure similarities.
Expression
The IL-26 expression was initially discovered in human HVS-transformed T cells.[6] Since then it was confirmed that T helper 1 cells and Th17 memory CD4+ cells are the major sources of IL-26. More accurately, IL-26 is expressed by pro-inflammatory IL-17 producing T cells in chronically inflamed tissues.[12][13][14] Co-expression of IL-17, IL-22, and IL-26 de facto defines the phenotype of human Th17 cells. Furthermore, CD26+ CD4+ T cells produce IL-26 in a model of graft-versus-host disease (GvHD).[15] CD4+ T cells polarized toward a regulatory phenotype (Treg), naïve CD4+ T cells, and T helper 2 cells show low or no expression of IL-26.[16]
It remains unclear whether IL-26 monocytes and macrophages express IL-26. Some studies showed there is no expression,[16] whereas other studies inconsistently reported constitutive expression at a low level in monocytes,[17] and the secretion of IL-26 by lung alveolar macrophages locally exposed to endotoxin.[18] The IL-26 expression is also present in NK cells,[16] especially NKp44+ human NK cell subset localized in mucosa-associated lymphoid tissue express substantial amounts of IL-26.[19] Very low IL-26 expression was reported in human herpesvirus 8-transformed B cells.[4]
Regarding non-immune cells, IL-26 expression was detected in primary bronchial epithelial cells from healthy individuals.[16] Pathologically, fibroblasts harvested from the inflamed synovia of patients with rheumatoid arthritis constituted the main source of IL-26.[14]
Receptors
IL-26R heterodimer, a conventional receptor for IL-26, consists of two chains – IL-10R2, and IL-20R1.[7] The IL-20R1 subunit contains the IL-26-binding site, whereas the IL-10R2 subunit acts as a second chain completing the assembly. Experiments performed with epithelial cells suggested both receptor subunits are required for the IL-26-dependent signal transduction.[8] According to some observations,[20] there is a possibility that additional IL-26 receptors exist.
Ligand binding by functional IL-26 receptor complex results in the initiation of a signal transduction pathway involving receptor-associated Janus tyrosine kinases Jak1 and Tyk2. IL-20R1 interacts with Jak1, and IL-10R2 is associated with Tyk2. Ligand-induced heterodimerization of receptor chains promotes cross-activation of Janus kinases, which phosphorylate receptor intracellular domains, leading to the activation of STAT protein family intracellular transcription factors STAT1 and STAT3. In addition, IL-26 activates extracellular signal-regulated kinases (ERK)-1/2, c-Jun N-terminal kinase (JNK), mitogen-activated protein kinases (MAPKs), and protein kinase B (PKB).[7]
While IL-10R2 is expressed on a wide variety of tissues, the expression of IL-20R1 is limited only to some tissues.[21] Thus, the ability to respond to IL-26 is restricted by the expression of IL-20R1 subunit.
Role
Interleukin 26 (IL-26) is an inflammatory mediator and a driver of chronic inflammation due to its ability to act as a carrier of extracellular DNA,[22] and as an antimicrobial molecule through its capacity to form pores in bacterial membranes. These properties suggest that IL-26 can be categorized as a kinocidin.
IL-26 is a natural human antimicrobial that promotes immune sensing of bacterial and host cell death. IL-26 is a cationic amphipathic protein that kills extracellular bacteria via membrane-pore formation. Furthermore, Th17 cell–derived IL-26 formed complexes with bacterial DNA and self-DNA released by dying bacteria and host cells. The IL-26–DNA complexes triggered the production of type I interferon by plasmacytoid dendritic cells via activation of Toll-like receptor 9, but independently of the IL-26 receptor.[22] Monocytes infected with intracellular bacterium M. tuberculosis reacted by decreasing IL-26 production, and IL-26 serum concentrations were lower in tuberculosis patients.[17] These data indicate that IL-26 may be involved in host defense against bacteria in more ways.
Concerning host defense to viruses, the role of IL-26 appears to be related to the expression of IL-26R by epithelial cells as these constitute the first barrier against many viruses. Elevated serum levels of IL-26 were detected in patients with chronic infection by hepatitis C virus. Moreover, the sensitivity of NK cells to IL-26 might trigger the ability to kill the virus-infected host cells.[23]
So far, the role of IL-6 in acute inflammation has not been properly studied, and most biological functions of IL-26 have been identified in pathological situations that feature chronic inflammation. The expression of IL-26 is elevated in the inflamed colonic mucosa of patients with Crohn's disease and it was reported that IL-26 induces the expression of IL-8 and TNFα as well as IL-10 in human gut epithelial cells. This activation of epithelial cells involves STAT1 and/or STAT3.[12] IL26 gene is also over-expressed in the joints of patients with spondyloarthritis[24] and rheumatoid arthritis,[14] in the sera and lesional skin tissues of psoriasis patients,[25] and in the sera of multiple sclerosis patients.[26]
A novel effect of IL-26 produced by donor-derived CD26+ CD4+ T cells on the pathophysiology of pulmonary chronic GVHD was observed in a murine model.[15]
The roles of IL-26 in normal physiology remain unknown. By contrast to other IL-10 cytokine family members, no induction of primary human keratinocyte proliferation in response to IL-26 has been detected.
References
- ^ a b c GRCh38: Ensembl release 89: ENSG00000111536 – Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Entrez Gene: interleukin 26".
- ^ a b c d Knappe A, Hör S, Wittmann S, Fickenscher H (April 2000). "Induction of a novel cellular homolog of interleukin-10, AK155, by transformation of T lymphocytes with herpesvirus saimiri". Journal of Virology. 74 (8): 3881–7. doi:10.1128/JVI.74.8.3881-3887.2000. PMC 111897. PMID 10729163.
- ^ Goris A, Marrosu MG, Vandenbroeck K (August 2001). "Novel polymorphisms in the IL-10 related AK155 gene (chromosome 12q15)". Genes and Immunity. 2 (5): 284–6. doi:10.1038/sj.gene.6363772. PMID 11528524.
- ^ a b Larochette V, Miot C, Poli C, Beaumont E, Roingeard P, Fickenscher H, et al. (2019-02-12). "IL-26, a Cytokine With Roles in Extracellular DNA-Induced Inflammation and Microbial Defense". Frontiers in Immunology. 10: 204. doi:10.3389/fimmu.2019.00204. PMC 6379347. PMID 30809226.
- ^ a b c Sheikh F, Baurin VV, Lewis-Antes A, Shah NK, Smirnov SV, Anantha S, et al. (February 2004). "Cutting edge: IL-26 signals through a novel receptor complex composed of IL-20 receptor 1 and IL-10 receptor 2". Journal of Immunology. 172 (4): 2006–10. doi:10.4049/jimmunol.172.4.2006. PMID 14764663.
- ^ a b Hör S, Pirzer H, Dumoutier L, Bauer F, Wittmann S, Sticht H, et al. (August 2004). "The T-cell lymphokine interleukin-26 targets epithelial cells through the interleukin-20 receptor 1 and interleukin-10 receptor 2 chains". The Journal of Biological Chemistry. 279 (32): 33343–51. doi:10.1074/jbc.M405000200. PMID 15178681.
- ^ Igawa D, Sakai M, Savan R (March 2006). "An unexpected discovery of two interferon gamma-like genes along with interleukin (IL)-22 and -26 from teleost: IL-22 and -26 genes have been described for the first time outside mammals". Molecular Immunology. 43 (7): 999–1009. doi:10.1016/j.molimm.2005.05.009. PMID 16005068.
- ^ Donnelly RP, Sheikh F, Dickensheets H, Savan R, Young HA, Walter MR (October 2010). "Interleukin-26: an IL-10-related cytokine produced by Th17 cells". Cytokine & Growth Factor Reviews. IL-10 Family of Cytokines. 21 (5): 393–401. doi:10.1016/j.cytogfr.2010.09.001. PMC 2997847. PMID 20947410.
- ^ Qi ZT, Nie P (November 2008). "Comparative study and expression analysis of the interferon gamma gene locus cytokines in Xenopus tropicalis". Immunogenetics. 60 (11): 699–710. doi:10.1007/s00251-008-0326-y. PMID 18726591. S2CID 25613652.
- ^ a b Dambacher J, Beigel F, Zitzmann K, De Toni EN, Göke B, Diepolder HM, et al. (September 2009). "The role of the novel Th17 cytokine IL-26 in intestinal inflammation". Gut. 58 (9): 1207–17. doi:10.1136/gut.2007.130112. PMID 18483078. S2CID 3186117.
- ^ Pène J, Chevalier S, Preisser L, Vénéreau E, Guilleux MH, Ghannam S, et al. (June 2008). "Chronically inflamed human tissues are infiltrated by highly differentiated Th17 lymphocytes". Journal of Immunology. 180 (11): 7423–30. doi:10.4049/jimmunol.180.11.7423. PMID 18490742.
- ^ a b c Corvaisier M, Delneste Y, Jeanvoine H, Preisser L, Blanchard S, Garo E, et al. (2012-09-25). Marrack P (ed.). "IL-26 is overexpressed in rheumatoid arthritis and induces proinflammatory cytokine production and Th17 cell generation". PLOS Biology. 10 (9): e1001395. doi:10.1371/journal.pbio.1001395. PMC 3463509. PMID 23055831.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ a b Ohnuma K, Hatano R, Aune TM, Otsuka H, Iwata S, Dang NH, et al. (April 2015). "Regulation of pulmonary graft-versus-host disease by IL-26+CD26+CD4 T lymphocytes". Journal of Immunology. 194 (8): 3697–712. doi:10.4049/jimmunol.1402785. PMC 4568737. PMID 25786689.
- ^ a b c d Wolk K, Kunz S, Asadullah K, Sabat R (June 2002). "Cutting edge: immune cells as sources and targets of the IL-10 family members?". Journal of Immunology. 168 (11): 5397–402. doi:10.4049/jimmunol.168.11.5397. PMID 12023331.
- ^ a b Guerra-Laso JM, Raposo-García S, García-García S, Diez-Tascón C, Rivero-Lezcano OM (February 2015). "Microarray analysis of Mycobacterium tuberculosis-infected monocytes reveals IL26 as a new candidate gene for tuberculosis susceptibility". Immunology. 144 (2): 291–301. doi:10.1111/imm.12371. PMC 4298423. PMID 25157980.
- ^ Che KF, Tengvall S, Levänen B, Silverpil E, Smith ME, Awad M, et al. (November 2014). "Interleukin-26 in antibacterial host defense of human lungs. Effects on neutrophil mobilization". American Journal of Respiratory and Critical Care Medicine. 190 (9): 1022–31. doi:10.1164/rccm.201404-0689OC. PMID 25291379.
- ^ Cella M, Fuchs A, Vermi W, Facchetti F, Otero K, Lennerz JK, et al. (February 2009). "A human natural killer cell subset provides an innate source of IL-22 for mucosal immunity". Nature. 457 (7230): 722–5. Bibcode:2009Natur.457..722C. doi:10.1038/nature07537. PMC 3772687. PMID 18978771.
- ^ Hummelshoj L, Ryder LP, Poulsen LK (July 2006). "The role of the interleukin-10 subfamily members in immunoglobulin production by human B cells". Scandinavian Journal of Immunology. 64 (1): 40–7. doi:10.1111/j.1365-3083.2006.01773.x. PMID 16784489. S2CID 46419911.
- ^ Nagalakshmi ML, Murphy E, McClanahan T, de Waal Malefyt R (May 2004). "Expression patterns of IL-10 ligand and receptor gene families provide leads for biological characterization". International Immunopharmacology. IL-Teenagers; the family of the IL-10 homologue comes of age. 4 (5): 577–92. doi:10.1016/j.intimp.2004.01.007. PMID 15120644.
- ^ a b Meller S, Di Domizio J, Voo KS, Friedrich HC, Chamilos G, Ganguly D, et al. (September 2015). "T(H)17 cells promote microbial killing and innate immune sensing of DNA via interleukin 26". Nature Immunology. 16 (9): 970–9. doi:10.1038/ni.3211. PMC 4776746. PMID 26168081.
- ^ Miot C, Beaumont E, Duluc D, Le Guillou-Guillemette H, Preisser L, Garo E, et al. (September 2015). "IL-26 is overexpressed in chronically HCV-infected patients and enhances TRAIL-mediated cytotoxicity and interferon production by human NK cells". Gut. 64 (9): 1466–75. doi:10.1136/gutjnl-2013-306604. PMID 25183206. S2CID 8052342.
- ^ Heftdal LD, Andersen T, Jæhger D, Woetmann A, Østgård R, Kenngott EE, et al. (July 2017). "Synovial cell production of IL-26 induces bone mineralization in spondyloarthritis". Journal of Molecular Medicine. 95 (7): 779–787. doi:10.1007/s00109-017-1528-2. PMID 28365787. S2CID 3932106.
- ^ Michalak-Stoma A, Pietrzak A, Szepietowski JC, Zalewska-Janowska A, Paszkowski T, Chodorowska G (December 2011). "Cytokine network in psoriasis revisited". European Cytokine Network. 22 (4): 160–8. doi:10.1684/ecn.2011.0294. PMID 22236965.
- ^ Esendagli G, Kurne AT, Sayat G, Kilic AK, Guc D, Karabudak R (February 2013). "Evaluation of Th17-related cytokines and receptors in multiple sclerosis patients under interferon β-1 therapy". Journal of Neuroimmunology. 255 (1–2): 81–4. doi:10.1016/j.jneuroim.2012.10.009. PMID 23177721. S2CID 11325105.
Further reading
- Davila S, Froeling FE, Tan A, Bonnard C, Boland GJ, Snippe H, et al. (April 2010). "New genetic associations detected in a host response study to hepatitis B vaccine". Genes and Immunity. 11 (3): 232–8. doi:10.1038/gene.2010.1. PMID 20237496.
- Silverberg MS, Cho JH, Rioux JD, McGovern DP, Wu J, Annese V, et al. (February 2009). "Ulcerative colitis-risk loci on chromosomes 1p36 and 12q15 found by genome-wide association study". Nature Genetics. 41 (2): 216–20. doi:10.1038/ng.275. PMC 2652837. PMID 19122664.
- Dambacher J, Beigel F, Zitzmann K, De Toni EN, Göke B, Diepolder HM, et al. (September 2009). "The role of the novel Th17 cytokine IL-26 in intestinal inflammation". Gut. 58 (9): 1207–17. doi:10.1136/gut.2007.130112. PMID 18483078. S2CID 3186117.
- Rose JE, Behm FM, Drgon T, Johnson C, Uhl GR (2010). "Personalized smoking cessation: interactions between nicotine dose, dependence and quit-success genotype score". Molecular Medicine. 16 (7–8): 247–53. doi:10.2119/molmed.2009.00159. PMC 2896464. PMID 20379614.
- Sheikh F, Baurin VV, Lewis-Antes A, Shah NK, Smirnov SV, Anantha S, et al. (February 2004). "Cutting edge: IL-26 signals through a novel receptor complex composed of IL-20 receptor 1 and IL-10 receptor 2". Journal of Immunology. 172 (4): 2006–10. doi:10.4049/jimmunol.172.4.2006. PMID 14764663.
- Siezen CL, Bont L, Hodemaekers HM, Ermers MJ, Doornbos G, Van't Slot R, et al. (April 2009). "Genetic susceptibility to respiratory syncytial virus bronchiolitis in preterm children is associated with airway remodeling genes and innate immune genes". The Pediatric Infectious Disease Journal. 28 (4): 333–5. doi:10.1097/INF.0b013e31818e2aa9. PMID 19258923. S2CID 25601837.
- Vandenbroeck K, Cunningham S, Goris A, Alloza I, Heggarty S, Graham C, et al. (October 2003). "Polymorphisms in the interferon-gamma/interleukin-26 gene region contribute to sex bias in susceptibility to rheumatoid arthritis". Arthritis and Rheumatism. 48 (10): 2773–8. doi:10.1002/art.11236. PMID 14558082.
- Dumoutier L, Van Roost E, Ameye G, Michaux L, Renauld JC (December 2000). "IL-TIF/IL-22: genomic organization and mapping of the human and mouse genes". Genes and Immunity. 1 (8): 488–94. doi:10.1038/sj.gene.6363716. PMID 11197690.
- Kantarci OH, Hebrink DD, Schaefer-Klein J, Sun Y, Achenbach S, Atkinson EJ, et al. (March 2008). "Interferon gamma allelic variants: sex-biased multiple sclerosis susceptibility and gene expression". Archives of Neurology. 65 (3): 349–57. doi:10.1001/archneurol.2007.66. PMID 18332247.
- Janssen R, Bont L, Siezen CL, Hodemaekers HM, Ermers MJ, Doornbos G, et al. (September 2007). "Genetic susceptibility to respiratory syncytial virus bronchiolitis is predominantly associated with innate immune genes". The Journal of Infectious Diseases. 196 (6): 826–34. doi:10.1086/520886. PMID 17703412.
- Wang K, Baldassano R, Zhang H, Qu HQ, Imielinski M, Kugathasan S, et al. (May 2010). "Comparative genetic analysis of inflammatory bowel disease and type 1 diabetes implicates multiple loci with opposite effects". Human Molecular Genetics. 19 (10): 2059–67. doi:10.1093/hmg/ddq078. PMC 2860894. PMID 20176734.
- Schuurhof A, Bont L, Siezen CL, Hodemaekers H, van Houwelingen HC, Kimman TG, et al. (June 2010). "Interleukin-9 polymorphism in infants with respiratory syncytial virus infection: an opposite effect in boys and girls". Pediatric Pulmonology. 45 (6): 608–13. doi:10.1002/ppul.21229. PMID 20503287. S2CID 24678182.