Levosalbutamol
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Xopenex, other |
| Other names | evalbuterol |
| AHFS/Drugs.com | International Drug Names |
| License data |
|
| Pregnancy category |
|
| Routes of administration | By mouth (tablets), inhalational (MDI) |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Metabolism | Hepatic |
| Elimination half-life | 3.3–4 hours |
| Excretion | Urinary |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.113.688 |
| Chemical and physical data | |
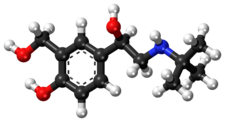
| Formula | C13H21NO3 |
| Molar mass | 239.315 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| | |
Levosalbutamol, also known as levalbuterol, is a short-acting β2 adrenergic receptor agonist used in the treatment of asthma and chronic obstructive pulmonary disease (COPD). Evidence is inconclusive regarding the efficacy of levosalbutamol versus salbutamol or salbutamol-levosalbutamol combinations, though levosalbutamol is believed to have a better safety profile due to its more selective binding to β2 receptors (primarily in the lungs) versus β1 (primarily in heart muscle).[2][3]
The drug is the (R)-(−)-enantiomer of its prototype drug salbutamol. It is available in some countries in generic formulations from pharmaceutical companies including Cipla, Teva, and Dey, among others.
Medical use
[edit]Levosalbutamol's bronchodilator properties give it indications in treatment of COPD (chronic obstructive pulmonary disease, also known as chronic obstructive lung disease) and asthma. Like other bronchodilators, it acts by relaxing smooth muscle in the bronchial tubes, and thus shortening or reversing an acute "attack" of shortness of breath or difficulty breathing. Unlike some slower-acting bronchodilators, it is not indicated as a preventative of chronic bronchial constriction.
Comparison to salbutamol
[edit]A 2013 systematic review of the drug's use as a treatment for acute asthma found that it "was not superior to albuterol regarding efficacy and safety in subjects with acute asthma." The review concluded: "We suggest that levalbuterol should not be used over albuterol for acute asthma."[2] Levalbuterol is notably more costly.[4][5]
Adverse effects
[edit]Generally, levosalbutamol is well tolerated. Common mild side-effects include an elevated heart rate, muscle cramps, and gastric upset (including heartburn and diarrhea).[6]
Symptoms of overdose in particular include: collapse into a seizure; chest pain (possible precursor of a heart attack); fast, pounding heartbeat, which may cause raised blood pressure (hypertension); irregular heartbeat (cardiac arrhythmia), which may cause paradoxical lowered blood pressure (hypotension); nervousness and tremor; headache; dizziness and nausea/vomiting; weakness or exhaustion (medical fatigue); dry mouth; and insomnia.[6]
Rarer side effects may indicate a dangerous allergic reaction. These include: paradoxical bronchospasm (shortness of breath and difficulty breathing); skin itching, rash, or hives (urticaria); swelling (angioedema) of any part of the face or throat (which can lead to voice hoarseness), or swelling of the extremities.[6]
Pharmacology
[edit]Mechanism of action
[edit]Activation of β2 adrenergic receptors on airway smooth muscle leads to the activation of adenylate cyclase and to an increase in the intracellular concentration of 3',5'-cyclic adenosine monophosphate (cyclic AMP). The increase in cyclic AMP is associated with the activation of protein kinase A, which in turn, inhibits the phosphorylation of myosin and lowers intracellular ionic calcium concentrations, resulting in muscle relaxation.
Levosalbutamol relaxes the smooth muscles of all airways, from the trachea to the terminal bronchioles. Increased cyclic AMP concentrations are also associated with the inhibition of the release of mediators from mast cells in the airways. Levosalbutamol acts as a functional agonist that relaxes the airway irrespective of the spasmogen involved, thereby protecting against all bronchoconstrictor challenges.
While it is recognized that β2 adrenergic receptors are the predominant receptors on bronchial smooth muscle, data indicate that there are beta receptors in the human heart, 10–50% of which are β2 adrenergic receptors. The precise function of these receptors has not been established. However, all β adrenergic agonist drugs can produce a significant cardiovascular effect in some patients, as measured by pulse rate, blood pressure, and restlessness symptoms, and/or electrocardiographic (ECG).
Approval and names
[edit]Levosalbutamol is the INN while levalbuterol is the USAN.
Levalbuterol was approved in the United States as a solution to be used with a nebulizer device in March 1999[7] and in March 2015 became available in a formulation with a metered-dose inhaler under the trade name Xopenex HFA (levalbuterol tartrate inhalation aerosol).[8]
See also
[edit]- Salbutamol — the racemic mixture containing both (R)-(−)- and (S)-(+)-enantiomers
References
[edit]- ^ "FDA-sourced list of all drugs with black box warnings (Use Download Full Results and View Query links.)". nctr-crs.fda.gov. FDA. Retrieved 22 Oct 2023.
- ^ a b Jat KR, Khairwa A (April 2013). "Levalbuterol versus albuterol for acute asthma: a systematic review and meta-analysis". Pulmonary Pharmacology & Therapeutics. 26 (2): 239–248. doi:10.1016/j.pupt.2012.11.003. PMID 23207739.
- ^ Punj A, Prakash A, Bhasin A (November 2009). "Levosalbutamol vs racemic salbutamol in the treatment of acute exacerbation of asthma". Indian Journal of Pediatrics. 76 (11): 1131–1135. doi:10.1007/s12098-009-0245-4. PMID 20012785. S2CID 11566782.
- ^ Schreck DM, Babin S (November 2005). "Comparison of racemic albuterol and levalbuterol in the treatment of acute asthma in the ED". Am J Emerg Med. 23 (7): 842–7. doi:10.1016/j.ajem.2005.04.003. PMID 16291438.
- ^ Hendeles L, Hartzema A (September 2003). "Levalbuterol is not more cost-effective than albuterol for COPD". Chest. 124 (3): 1176, author reply 1176–8. doi:10.1378/chest.124.3.1176. PMID 12970057.
- ^ a b c American Society of Health-System Pharmacists (1 September 2010). "Levalbuterol Oral Inhalation". MedlinePlus. Bethesda, Maryland: U.S. National Library of Medicine, National Institutes of Health. Retrieved 7 January 2015.
- ^ "US label: levalbuterol hydrochloride Inhalation Solution" (PDF). FDA. January 2015. For updates and past labels, see FDA index page for NDA 020837.
- ^ "US label: levalbuterol tartrate inhalation aerosol" (PDF). FDA. February 2017. For updates and past labels, see FDA index page for NDA 021730.
External links
[edit]- "Levalbuterol". Drug Information Portal. U.S. National Library of Medicine.
