Interleukin 13
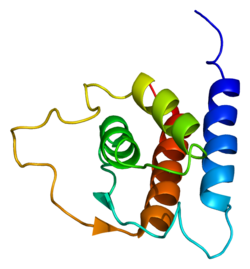
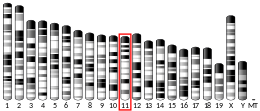
Interleukin 13 (IL-13) is a protein that in humans is encoded by the IL13 gene.[4][5][6] IL-13 was first cloned in 1993 and is located on chromosome 5q31 with a length of 1.4kb.[4] It has a mass of 13 kDa and folds into 4 alpha helical bundles.[7] The secondary structural features of IL-13 are similar to that of Interleukin 4 (IL-4); however it only has 25% sequence homology to IL-4 and is capable of IL-4 independent signaling.[7][4][8] IL-13 is a cytokine secreted by T helper type 2 (Th2) cells, CD4 cells, natural killer T cell, mast cells, basophils, eosinophils and nuocytes.[7] Interleukin-13 is a central regulator in IgE synthesis, goblet cell hyperplasia, mucus hypersecretion, airway hyperresponsiveness, fibrosis and chitinase up-regulation.[7] It is a mediator of allergic inflammation and different diseases including asthma.[7]
Functions
IL-13 has effects on immune cells that are similar to those of the closely related cytokine IL-4.[4] However, IL-13 is suspected to be the central mediator of the physiologic changes induced by allergic inflammation in many tissues.[4]
Although IL-13 is associated primarily with the induction of airway disease, it also has anti-inflammatory properties.[4] IL-13 induces a class of protein-degrading enzymes, known as matrix metalloproteinases (MMPs), in the airways.[4] These enzymes are required to induce aggression of parenchymal inflammatory cells into the airway lumen, where they are then cleared.[4] Among other factors, IL-13 induces these MMPs as part of a mechanism that protects against excessive allergic inflammation that predisposes to asphyxiation.[4]
IL-13 is known to induce changes in hematopoietic cells, but these effects are probably less important than that of IL-4.[4] Furthermore, IL-13 can induce immunoglobulin E (IgE) secretion from activated human B cells.[4][7] Deletion of IL-13 from mice does not markedly affect either Th2 cell development or antigen-specific IgE responses induced by potent allergens.[4] In comparison, deletion of IL-4 deactivates these responses. Thus, rather than a lymphoid cytokine, IL-13 acts more prominently as a molecular bridge linking allergic inflammatory cell to the non-immune cells in contact with them, thereby altering physiological function.[4]
The signaling of IL-13 begins through a shared multi-subunit receptor with IL-4.[7] This receptor is a heterodimer receptor complex consisting of alpha IL-4 receptor (IL-4Rα) and alpha Interleukin-13 receptor (IL-13R1).[7] The high affinity of IL-13 to the IL-13R1 leads to their bond formation which further increase the probability of a heterodimer formation to IL-4R1 and the production of the type 2 IL-4 receptor. Heterodimerization activates both the STAT6 and the IRS.[7] STAT6 signaling is important in initiation of the allergic response.[7] Most of the biological effects of IL-13, like those of IL-4, are linked to a single transcription factor, signal transducer and activator of transcription 6 (STAT6).[7] Interleukin-13 and its associated receptors with α subunit of the IL-4 receptor (IL-4Rα) allows for the downstream activation of STAT6.[9] The JAK Janus kinase proteins on the cytoplasmic end of the receptors allows for the phosphorylation of STAT6, which then forms an activated homodimer and are transported to the nucleus.[9] Once, in the nucleus, STAT6 heterodimer molecule regulates gene expression of cell types critical to the balance between host immune defense and allergic inflammatory responses such as the development of Th2.[9] This can be resulted from an allergic reaction brought about when facing an Ala gene. IL-13 also binds to another receptor known as IL-13Rα2.[10] IL-13Rα2 (which is labelled as a decoy receptor) is derived from Th2 cells and is a pleotropic immune regulatory cytokine.[10] IL-13 has greater affinity (50-times) to IL-13Rα2 than to IL-13Ra1.[10] The IL-13Rα2 subunit binds only to IL-13 and it exists in both membrane-bound and soluble forms in mice.[10] A soluble form of IL-13Rα2 has not been detected in human subjects.[10] Studies of IL-13 transgenic mice lungs with IL-13Rα2 null loci indicated that IL-13Rα2 deficiency significantly augmented IL-13 or ovalbumin-induced pulmonary inflammation and remodeling.[10] Most normal cells, such as immune cells or endothelial cells, express very low or undetectable levels of IL-13 receptors.[10] Research has shown that cell-surface expression of IL-13Rα2 on human asthmatic airway fibroblasts was reduced compared with expression on normal control airway fibroblasts.[10] This supported the hypothesis that IL-13Rα2 is a negative regulator of IL-13–induced response and illustrated significantly reduced production of TGF-β1 and deposition of collagen in the lungs of mice.[10]
Interleukin-13 has a critical role in the Goblet cell metaplasia.[11] Goblet cells are filled with mucin (MUC).[11] MUC5AC Mucin 5AC is a gel-like mucin product of goblet cells.[11] Interleukin-13 induces goblet cell differentiation and allows for the production of MUC5AC in tracheal epithelium.[11] 15-Lipoxygenase-1 (15LO1) which is an enzyme in the fatty acid metabolism and its metabolite, 15-HETE, are highly expressed in asthma (which lead to the overexpression of MUC5AC) and are induced by IL-13 in human airway epithelial cells. With the increasing number of goblet cells, there is the production of excessive mucus within the bronchi.[11] The functional consequences of the changes in MUC storation and secretion contributes to the pathophysiologic mechanisms for various clinical abnormalities in asthmatic patients including sputum production, airway narrowing, exacerbation and accelerated loss in lung function.[11]
Additionally, IL-13 has been shown to induce a potent fibrogenic program during the course of diverse diseases marked by elevated Type 2 cytokines such as chronic schistosomiasis and atopic dermatitis among others. It has been suggested that this fibrogenic program is critically dependent on direct IL-13 signaling through IL-4Rα on PDGFRβ+ fibroblasts.[12]
Clinical significance
IL-13 specifically induces physiological changes in parasitized organs that are required to expel the offending organisms or their products. For example, expulsion from the gut of a variety of mouse helminths requires IL-13 secreted by Th2 cells. IL-13 induces several changes in the gut that create an environment hostile to the parasite, including enhanced contractions and glycoprotein hyper-secretion from gut epithelial cells, that ultimately lead to detachment of the organism from the gut wall and their removal.[13]
The eggs of the parasite Schistosoma mansoni may lodge in a variety of organs including the gut wall, liver, lung and even central nervous system, inducing the formation of granulomas under the control of IL-13. Here, however, the eventual result is organ damage and often profound or even fatal disease, not resolution of the infection. An emerging concept is that IL-13 may antagonize Th1 responses that are required to resolve intracellular infections. In this immune dysregulated context, marked by the recruitment of aberrantly large numbers of Th2 cells, IL-13 inhibits the ability of host immune cells to destroy intracellular pathogens.
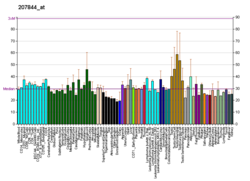
IL-13 expression has demonstrated to be increased in bronchoalveolar lavage (BAL) fluid and cells in patients with atopic mild asthma after allergen challenge.[14] Genome-wide association studies have identified multiple polymorphisms of IL-13 and genes encoding the IL-13 receptors as associated with asthma susceptibility, bronchial hyperresponsiveness, and increased IgE levels.[14] The overexpression of IL-13 induces many features of allergic lung disease, including airway hyperresponsiveness, goblet cell metaplasia, mucus hypersecretion and airway remodelling which all contribute to airway obstruction.[15] murine studies demonstrated that IL-13 was both necessary and sufficient to generate asthma-like Th2 responses in the mouse lung.[7] IL-13 is mainly overexpressed in sputum, bronchial submucosa, peripheral blood and mast cells in the airway smooth muscle bundle.[7] IL-4 contributes to these physiologic changes, but is less important than IL-13. IL-13 also induces secretion of chemokines that are required for recruitment of allergic effector cells to the lung. Studies of STAT6 transgenic mice suggest the possibility that IL-13 signaling occurring only through the airway epithelium is required for most of these effects. While no studies have yet directly implicated IL-13 in the control of human diseases, many polymorphisms in the IL-13 gene have been shown to confer an enhanced risk of atopic respiratory diseases such as asthma.[13] In a study conducted with knockout mice model for asthma, air resistance, mucus production and profibrogenic mediator induction were solely found to be dependent on the presence of IL-13R1 and not IL-13Rα2.[7] Studies on transgenic mouse in vivo demonstrate that lung over-expression of IL-13 induces subepithelial airway fibrosis.[7] IL-13 is the dominant effector in toxin, infection, allergic, and post-transplant bronchiolitis obliterans models of fibrosis.[7]
Other research suggests that IL-13 is responsible for the promotion of the survival and the migration of epithelial cells, production of inducible nitric oxide synthase by airway epithelial cells, activation of macrophages, permeability of the epithelial cells, and transformation of airway fibroblasts to myofibroblasts leading to collagen deposition.[14] The deposition then influences the airway remodelling in asthmatic patients.[14]
Dupilumab is a monoclonal antibody IL-13 and IL-4 modulator that targets the shared receptor of IL-4 and IL-13, IL4Rα.[16] Since IL-4 and IL-13 have similar biological activities, dupilumab may be an effective form of treatment for asthmatic patients.[16]
See also
- Interleukin-13 receptor, the IL-13 receptor
References
- ^ a b c GRCm38: Ensembl release 89: ENSMUSG00000020383 – Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ a b c d e f g h i j k l m Minty A, Chalon P, Derocq JM, Dumont X, Guillemot JC, Kaghad M, Labit C, Leplatois P, Liauzun P, Miloux B (March 1993). "Interleukin-13 is a new human lymphokine regulating inflammatory and immune responses". Nature. 362 (6417): 248–50. Bibcode:1993Natur.362..248M. doi:10.1038/362248a0. PMID 8096327. S2CID 4368915.
- ^ McKenzie AN, Culpepper JA, de Waal Malefyt R, Brière F, Punnonen J, Aversa G, Sato A, Dang W, Cocks BG, Menon S (April 1993). "Interleukin 13, a T-cell-derived cytokine that regulates human monocyte and B-cell function". Proceedings of the National Academy of Sciences of the United States of America. 90 (8): 3735–9. Bibcode:1993PNAS...90.3735M. doi:10.1073/pnas.90.8.3735. PMC 46376. PMID 8097324.
- ^ Morgan JG, Dolganov GM, Robbins SE, Hinton LM, Lovett M (October 1992). "The selective isolation of novel cDNAs encoded by the regions surrounding the human interleukin 4 and 5 genes". Nucleic Acids Res. 20 (19): 5173–9. doi:10.1093/nar/20.19.5173. PMC 334302. PMID 1408833.
- ^ a b c d e f g h i j k l m n o p Rael EL, Lockey RF (2011). "Interleukin-13 signaling and its role in asthma". The World Allergy Organization Journal. 4 (3): 54–64. doi:10.1097/WOX.0b013e31821188e0. PMC 3651056. PMID 23283176.
- ^ Zurawski G, de Vries JE (January 1994). "Interleukin 13, an interleukin 4-like cytokine that acts on monocytes and B cells, but not on T cells". Immunol. Today. 15 (1): 19–26. doi:10.1016/0167-5699(94)90021-3. PMID 7907877.
- ^ a b c Walford HH, Doherty TA (2013). "STAT6 and lung inflammation". JAK-STAT. 2 (4): e25301. doi:10.4161/jkst.25301. PMC 3876430. PMID 24416647.
- ^ a b c d e f g h i Tu M, Wange W, Cai L, Zhu P, Gao Z, Zheng W (2016). "IL-13 receptor α2 stimulates human glioma cell growth and metastasis through the Src/PI3K/Akt/mTOR signaling pathway". Tumour Biology. 37 (11): 14701–14709. doi:10.1007/s13277-016-5346-x. PMID 27623944. S2CID 30389002.
- ^ a b c d e f Fahy JV (2002). "Goblet cell and mucin gene abnormalities in asthma". Chest. 122 (6 Suppl): 320S–326S. doi:10.1378/chest.122.6_suppl.320S. PMID 12475809. S2CID 23113468.
- ^ Gieseck RL, Ramalingam TR, Hart KM, Vannella KM, Cantu DA, Lu WY, Ferreira-González S, Forbes SJ, Vallier L, Wynn TA (2016). "Interleukin-13 Activates Distinct Cellular Pathways Leading to Ductular Reaction, Steatosis, and Fibrosis". Immunity. 45 (1): 145–58. doi:10.1016/j.immuni.2016.06.009. PMC 4956513. PMID 27421703.
- ^ a b Seyfizadeh N, Seyfizadeh N, Babaloo Z (2014). "Interleukin-13 as an Important Mediator: A Review on its Roles in Some Human Diseases". Iranian Journal of Allergy, Asthma and Immunology. In Press.
- ^ a b c d Ingram JL, Kraft M (2012). "IL-13 in asthma and allergic disease: asthma phenotypes and targeted therapies". The Journal of Allergy and Clinical Immunology. 130 (4): 829–42, quiz 843–4. doi:10.1016/j.jaci.2012.06.034. PMID 22951057.
- ^ Wills-Karp M, Luyimbazi J, Xu X, Schofield B, Neben TY, Karp CL, Donaldson DD (December 1998). "Interleukin-13: central mediator of allergic asthma". Science. 282 (5397): 2258–61. Bibcode:1998Sci...282.2258W. doi:10.1126/science.282.5397.2258. PMID 9856949.
- ^ a b Vatrella A, Fabozzi I, Calabrese C, Maselli R, Pelaia G (2014). "Dupilumab: a novel treatment for asthma". Journal of Asthma and Allergy. 7: 123–30. doi:10.2147/JAA.S52387. PMC 4159398. PMID 25214796.
{{cite journal}}: CS1 maint: unflagged free DOI (link)
Further reading
- Marone G, Florio G, Petraroli A, de Paulis A (2001). "Dysregulation of the IgE/Fc epsilon RI network in HIV-1 infection". J. Allergy Clin. Immunol. 107 (1): 22–30. doi:10.1067/mai.2001.111589. PMID 11149986.
- Marone G, Florio G, Triggiani M, Petraroli A, de Paulis A (2001). "Mechanisms of IgE elevation in HIV-1 infection". Crit. Rev. Immunol. 20 (6): 477–96. doi:10.1615/critrevimmunol.v20.i6.40. PMID 11396683.
- Skinnider BF, Kapp U, Mak TW (2003). "The role of interleukin 13 in classical Hodgkin lymphoma". Leuk. Lymphoma. 43 (6): 1203–10. doi:10.1080/10428190290026259. PMID 12152987. S2CID 21083414.
- Izuhara K, Arima K, Yasunaga S (2003). "IL-4 and IL-13: their pathological roles in allergic diseases and their potential in developing new therapies". Current Drug Targets. Inflammation and Allergy. 1 (3): 263–9. doi:10.2174/1568010023344661. PMID 14561191.
- Dessein A, Kouriba B, Eboumbou C, Dessein H, Argiro L, Marquet S, Elwali NE, Rodrigues V, Li Y, Doumbo O, Chevillard C (2005). "Interleukin-13 in the skin and interferon-gamma in the liver are key players in immune protection in human schistosomiasis". Immunol. Rev. 201: 180–90. doi:10.1111/j.0105-2896.2004.00195.x. PMID 15361241. S2CID 25378236.
- Copeland KF (2006). "Modulation of HIV-1 transcription by cytokines and chemokines". Mini Reviews in Medicinal Chemistry. 5 (12): 1093–101. doi:10.2174/138955705774933383. PMID 16375755.