Oxymorphone: Difference between revisions
No edit summary |
→Illicit Use: PP1: 1. oxymorphone is an opioid, not an opiate. 2. Addiction and dependence are not medically interchangeable terms, and using them as such perpetuates a general misunderstanding of this class of medications. |
||
| Line 145: | Line 145: | ||
==Illicit Use== |
==Illicit Use== |
||
Like other effective centrally acting analgesics, some of the additional effects of oxymorphone can include euphoria, anxiolysis, promotion of sociability, and other similar effects that can cause psychological addiction to the drug. Also, like |
Like other effective centrally acting analgesics, some of the additional effects of oxymorphone can include euphoria, anxiolysis, promotion of sociability, and other similar effects that can cause psychological addiction to the drug. Also, like other opioids, oxymorphone use can result in physical dependence accompanied by potential withdrawal symptoms with abrupt discontinuation. |
||
Opana ''does'' have euphoric effects, and they are short-lived. This is one of the crucial elements of a drug that can generate a serious narcotic habit rather quickly in those who take it for recreation and require more doses to maintain a stable level of euphoria. These effects however, barring enhancement with alcohol or other substances or means of administration other than oral, are less pronounced than that of morphine, fentanyl or dilaudid however, as mentioned previously, when taken intranasally the euphoric effects are far more pronounced. |
Opana ''does'' have euphoric effects, and they are short-lived. This is one of the crucial elements of a drug that can generate a serious narcotic habit rather quickly in those who take it for recreation and require more doses to maintain a stable level of euphoria. These effects however, barring enhancement with alcohol or other substances or means of administration other than oral, are less pronounced than that of morphine, fentanyl or dilaudid however, as mentioned previously, when taken intranasally the euphoric effects are far more pronounced. |
||
Revision as of 19:49, 21 February 2013
This article's lead section may be too long. (April 2010) |
This article needs additional citations for verification. (December 2010) |
 | |
| Clinical data | |
|---|---|
| Trade names | Opana |
| Other names | 14-Hydroxydihydromorphinone |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a610022 |
| Dependence liability | High |
| Routes of administration | intravenous, intramusucular, subcutaneous, oral, rectal, intranasal. |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | 10% (oral) 40% (Intranasal) 100% (IV, IM) |
| Metabolism | hepatic |
| Elimination half-life | 1.3 +/- 0.7 hrs (with parenteral admin);[1] 7.25-9.43 hr (with oral admin)[2] |
| Excretion | 35% urine, 65% feces |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.000.873 |
| Chemical and physical data | |
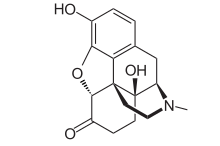
| Formula | C17H19NO4 |
| Molar mass | 301.33706 g/mol g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| (verify) | |
Oxymorphone (Opana, Numorphan, Numorphone) or 14-Hydroxydihydromorphinone is a powerful semi-synthetic opioid analgesic first developed in Germany in 1914,[3] patented in the USA by Endo Pharmaceuticals in 1955[4] and introduced to the United States market in January 1959 and other countries around the same time. It (along with hydromorphone) was designed to have less incidence of side effects than morphine and heroin. It was a success as it differs from morphine and heroin in its effects in that it generates less euphoria[citation needed], sedation, itching and other histamine effects at equianalgesic doses. This also means a lower dependence liability[dubious – discuss].
The brand name Numorphan is derived by analogy to the Nucodan name for an oxycodone product (or vice versa) as well as Paramorphan/Paramorfan for dihydromorphine and Paracodin (dihydrocodeine). The only commercially available salt of oxymorphone in most of the world at this time is the hydrochloride, which has a free base conversion ratio of 0.891.
In some countries, hydromorphinol is distributed under the trade names Numorphan and Numorphan Oral. This is a relatively rare exception and the two drugs, whilst both being strong opioid analgesics, are notably different from one another.
Oxymorphone is administered as its hydrochloride salt via injection, or suppository; typically in dosages of 1 mg (injected) to 5 mg (suppository). Endo has been the major distributor of oxymorphone throughout the world and currently markets oxymorphone in the United States and elsewhere as Opana and Opana ER.
Opana is available as 5 mg and 10 mg tablets; Opana ER, an extended-release form of oxymorphone, is available as tablets in strengths of 5 mg,10 mg, 20 mg, 30 mg, and 40 mg. As of July 21, 2011 generic strengths equivalent to Opana ER 7½ mg and 15 mg are available.[5] Some resources assert that 2, 12 and/or 15 mg IR tablets and 25, 36 and 50 mg extended release tablets will be introduced although apparently the timeline on that is not known to the public at this time. Opana Extended-Release tablets are based on the TIMERx system developed by a consortium led by Endo and Penwest. Some of these strengths (notably not the 7.5 mg) are available in an Opana IR–immediate release–form for breakthrough pain to be used by patients already on 24/7 opioid care such as fentanyl patches and sustained-relief morphine drugs like Avinza.
In addition to the sustained-release version for Opana, other versions of TIMERx are available and being developed for other protocols such as increasing, decreasing, stepwise increasing, and stepwise decreasing dose delivery over time, single and multiple bursts of medication, and combinations of the above. Opana ER was changed to the INTAC platform of extended release and abuse deterent as of 2012. Similar to the changed Oxycontin platform , both developed by Grunenthal using Polyethylenoxide under pressure and heat for extruding pills.
Specifically, the apparent extension of the duration of effect of the IR tablets (all other things being equal, oxymorphone has a duration of action of 5 to 8 hours in most patients) versus similar drugs in commonly used immediate-release forms—for example Dilaudid (hydromorphone), morphine, Vilan (nicomorphine), Paramorfan (dihydromorphine) as well as prodrugs for this group such as hydrocodone, nicocodeine, codeine, dihydrocodeine and others—is often attributed to a marginal extended-release effect from various excipients, particularly those that are hydrophilic and form a gel-like substance at the pH levels in the stomach and duodenum.
Both as the result of this and the pharmacokinetics of oxymorphone, the IR tablets have a de facto duration of action of 5 to 13 hours (the mean would seem to be around 7 hours with a moderately small standard deviation and a left-skewed and leptokurtic frequency distribution) in patients with normal kidney and liver function. As a result, patients rotated on to extended release oxymorphone preparations from other opioids may very well need the Opana IR tablets, Numorphan ampoules or phials with hypodermic needles and/or a PCA pump, or immediate-release formulations of hydromorphone, dihydromorphine, high dose oxycodone, hydromorphinol, nicomorphine, diamorphine, or morphine for breakthrough pain incidents already in progress. An oxymorphone nasal spray is reportedly in development, along with a possible hydromorphone nasal spray and implantable osmotic pumps for both drugs.
The duration of action and metabolic half-life of oxymorphone mean that immediate-release tablets are more similar to analgesic preparations of methadone, levorphanol, piritramide, and existing extended-release forms of morphine, oxycodone, ketobemidone and so on. The extended-release Opana tablets can provide detectable analgesia for anywhere from 6 to 36+ hours (the mean appears to be very close to the lower end of the continuum), largely contingent on things that can alter the drug's liberation, absorption, distribution, metabolism, and elimination profile. One cause is unusual conditions in the upper and middle GI tract, such as created by misoprostol and Arthrotec (misoprostol plus diclofenac). Among other things, misoprostol is a smooth muscle agent with both a contact and systemic mucousagogue that coats the stomach and adjacent areas with increasing amounts of mucus. This can result in everything from even slower onset of action to intact tablets being passed with stool.
Oxymorphone is also produced within the human body when the liver metabolises oxycodone by means of O demethylation catalysed by the CYP2D6 enzyme. Approximately 10% of the dose is processed by the endocrine system in this respect; this can vary widely from person to person. The codeine-hydrocodone group and morphinans exhibit the same characteristics.
Consuming alcohol with Opana extended-release tablets can be an extremely dangerous situation. The absorption of oxymorphone can vary wildly in the presence of alcohol. Plasma concentrations were found to be as low as -50% of expected to as much as 270% more than expected. Elevated plasma levels could result in overdose. Opana ER does not cause "dose dumping", which creates a blast of drug release that plagues other long acting opioids.
Uses
Oxymorphone is indicated for the relief of moderate to severe pain and also as a preoperative medication to alleviate apprehension, maintain anesthesia, and as an obstetric analgesic. Additionally, it can be used for the alleviation of pain in patients with dyspnea associated with acute left ventricular failure and pulmonary oedema.
Opana extended-release tablets are indicated for the management of chronic pain of all or most aetiologies and are indicated only for patients already on a regular schedule of strong opioids for a prolonged period. The immediate-release Opana tablets are recommended for management of breakthrough pain for patients on the extended-release version. Some protocols for chronic pain conditions characterised by severe breakthrough pain incidents add Numorphan ampoules as a third form of the drug for use when a breakthrough pain incident is in progress. An oxymorphone nasal spray is being developed for this purpose but the release date is unknown; some practitioners prefer fentanyl immediate-release formulations such as Actiq or Fentora for this purpose although some patients have severe side effects from fentanyl.
Oxymorphone is used in veterinary medicine in many of the same uses as for humans, with induction and maintenance of anaesthetia and sometimes tranquillisation of small and medium-sized animals being the most common use. Morphine, hydromorphone, fentanyl and butorphanol are also common in veterinary settings and tramadol is now often used as an analgesic for cats, dogs, ferrets, rats and other small animals.
Oxymorphone is mentioned, along with buprenorphine, oxycodone, dihydrocodeine, morphine and other opioids as a possible means of mitigating refractory depression.[6][7][8] Opioids were commonly used for this indication up until the introduction of the tricyclic antidepressants in the 1950s, even though the latter appear to work in a smaller percentage of cases and are generally more toxic than most chemical classes of opioids. Conversely, tricyclic anti-depressants and chemically related drugs are the most commonly used adjuvants and atypical analgesics used with opioids for pain, especially neuropathic pain.
Physical characteristics
Oxymorphone HCl occurs as odorless white crystals or white to off-white powder. It darkens in color with prolonged exposure to light, though this does not affect potency. One gram of oxymorphone is soluble in 4 ml of water, and it is sparingly soluble in alcohol and ether. The commercially available injection has a pH of 2.7–4.5.
Toxicity
In common with other opioids, oxymorphone overdosage is characterized by respiratory depression, extreme somnolence progressing to stupor or coma, skeletal muscle flaccidity, cold and clammy skin, and sometimes bradycardia and hypotension. In a severe case of overdose, apnea, circulatory collapse, cardiac arrest, and death may occur.
At equianalgesic doses oxymorphone is marginally more toxic than morphine but less so than fully synthetic opioids such as methadone and pethidine[citation needed]. At therapeutic doses, toxicity is primarily manifested as miosis, nausea, and possibly occasional mild involuntary muscle movements especially in the distal portions of the extremities and the shoulder area in some cases. This is most common in patients taking a number of other drugs for their condition, especially muscle relaxants and some adjuvant analgesics, and also appears to happen most often during and immediately after a significant upward titration in the single-dose and per 24 hour doses.
Instances of the body suddenly jerking bolt upright from a more relaxed sitting position is a sign of high and/or rapidly increasing serum levels of opioids and all of the above movements are likely due to the anticholinergic or anticholinergic-like effects of opioids and/or other medications prescribed at the same time, as they manifest in patients on atropine-like drugs as well. The primary risk here involves dropping objects, spilling liquids, striking body parts against walls, and potentially losing footing on flat ice surfaces.
While all this can be frightening at first, more than 85 percent of patients do not experience it at any time during treatment, and oxymorphone does not appear to induce seizures in neurologically healthy patients as does the pethidine series of opioids (pethidine, anileridine, alphaprodine, piminodine and others) nor does it have toxic metabolites that accumulate in the system as do pethdine synthetic opioids. There is also no real evidence that oxymorphone significantly lowers the seizure threshold like tramadol and some of the other synthetics mentioned above.
Brand Names
- Numorphan (suppository and injectable solution)
- Opana ER (extended-release tablet)
- Opana IR (immediate-release tablet)
Other manufacturers and Endo themselves have also, according to reports in the mass media and professional journals over the last few years, considered and/or are currently developing a Duragesic-style oxymorphone skin plasters and oxymorphone and hydromorphone nasal sprays.
Illicit Use
Like other effective centrally acting analgesics, some of the additional effects of oxymorphone can include euphoria, anxiolysis, promotion of sociability, and other similar effects that can cause psychological addiction to the drug. Also, like other opioids, oxymorphone use can result in physical dependence accompanied by potential withdrawal symptoms with abrupt discontinuation.
Opana does have euphoric effects, and they are short-lived. This is one of the crucial elements of a drug that can generate a serious narcotic habit rather quickly in those who take it for recreation and require more doses to maintain a stable level of euphoria. These effects however, barring enhancement with alcohol or other substances or means of administration other than oral, are less pronounced than that of morphine, fentanyl or dilaudid however, as mentioned previously, when taken intranasally the euphoric effects are far more pronounced.
The significant antidepressant and empathogenic properties of oxymorphone and other dihydromorphinone class semi-synthetic opioids is currently of interest to both the underground and the medical establishment, the latter of whom are "re-discovering" the anti-depressant effect and its relatively low ratio of toxic effects and lack of association with patient suicide attempts (see the oxycodone discussion for further information and footnotes) and Opana ER has been proposed as an alternative to methadone and other extended-release and/or long lasting drugs like Morphine, extended-release dihydrocodeine, buprenorphine, and 24-hour hydromorphone tablets for opioid detoxification and maintenance.
Endo withdrew the original Numorphan tablets from the market in 1972 as the result of regulatory and market pressures and other considerations as it was passionately sought, by any means necessary, by some narcotics addicts. Until its removal from the United States market at that point, oxymorphone in the form of Numorphan 10 mg instant-release tablets was one of the most sought-after and well-regarded opioids of the IV drug using community. Because of its low bioavailability, 10% when taken orally, a 10 mg tablet represents 10 times the average IV dose in a single tablet. Known popularly as "blues" or "Nu- Blues" for their light blue color, the tablets contained very few insoluble binders—making them easy to inject—and were extremely potent when used intravenously. "Blues" were also considered to be especially euphoric; comparable to or better than heroin. Numorphan tablets, and the oxymorphone they contained, are the "blues" referred to in the film Drugstore Cowboy.
Slang terms for oxymorphone include: blues, biscuits, blue heaven, new blues (although the immediate-release tablets are pink and off-white), octagons (extended release), [strength] octagons, stop signs, pink, pink heaven, biscuits (could also be Dilaudid tablets, meprobamate tablets, or formerly Quaaludes), pandas, pancakes, pink heaven, pink lady, Mrs O, Orgasna IR, OM, Pink O, The O Bomb (by analogy to the slang term for hydromorphone "H Bomb") and others.
Oxymorphone is not a component of "T's and blues", 1970s slang for a combination of pentazocine ("T's") and pyribenzamine ("blues"). Nor are "blues" 10 mg Valium tablets, which are known as Blue Bombers and BBs.
Rare cases of users baking their own at home by extracting oxycodone from pharmaceuticals and converting it to oxymorphone have been reported in a number of countries. In some cases, codeine is the starting material with morphine, or more rarely thebaine, being the intermediate. In those cases, the more common end products sought are morphine salts, morphine base, heroin, dihydromorphine, desomorphine, and hydromorphone.
The low bioavailability of oxymorphone after oral administration requires Opana extended-release to contain up to 40 mg of oxymorphone per tablet—almost as much as an entire case of Numorphan ampoules; attempts to circumvent the extended-release mechanism by injecting or snorting the tablets are therefore particularly dangerous. However, chewing the tablets and/or taking with alcohol for the 70 per cent bioavailability boost from the latter appear to be the only means successful Opana ER misuse aside from insufflation—the TIMERx system appears to be making the extended release tablets useless for preparing for injection, but injection is possible using a two-stage extraction/cooking process involving alcohol and water or a temperature independent water-only extraction process if prepared 12 – 24 hours prior to injection.
Chemistry
Oxymorphone is commercially produced from thebaine, which is a minor constituent of the opium poppy (Papaver somniferum) but thebaine is found in greater abundance (3%) in the roots of the oriental poppy (Papaver orientale). Oxymorphone can also be synthesized from morphine or oxycodone, and is an active metabolite of the latter drug. The structure-activity relationship of oxymorphone and its derivatives has been well-examined. Esterification of the hydroxyl groups yields stronger compounds. Another derivative of oxymorphone is the opioid antagonist naloxone (Narcan).
As reported in the July 1993 issue of Applied Environmental Bacteriology (PDF available at http://aem.asm.org/cgi/reprint/61/10/3645.pdf), the bacterium Pseudomonas putida, serotype M10 turns oxymorphone into oxymorphol by means of a one-step conversion involving morphine dehydrogenase and a naturally occurring NADH-dependent morphinone reductase that can work on unsaturated 7,8 bonds.
German patents from the middle 1930s indicate that oxymorphone as well as hydromorphone, hydrocodone, oxycodone, and acetylmorphone can be prepared—without the need for hydrogen gas—from solutions of codeine, morphine, and dionine by refluxing an acidic aqueous solution, or the precursor drug dissolved in ethanol, in the presence of Column 7 metals, namely palladium and platinum in fine powder or colloidal form or platina black. It is unclear from information available if aluminium or nickel can be used as a catalyst in these reactions as well.[9]
However, the aforementioned patents deal specifically with hydrogenation reactions producing dihydrocodeinone (hydrocodone), dihydromorphinone (hydromorphone), and ethyldihydromorphinone as final products. Hence it is unclear at best and rather unlikely that these particular procedures can be applied for the synthesis of oxycodone or oxymorphone, as they are not typically synthesized in this manner.
The rare practise of making homebake oxymorphone generally uses oxycodone and pyridine amongst others, and the production of homebake hydromorphone (Dilaudid) from hydrocodone does also exist but is extremely rare. This is similar to a method especially common in New Zealand to make morphine out of codeine. The resultant morphine base is used as is, made into a salt (usually citrate, although ascorbate, acetate, hydrochloride, nitrate, phosphate, and sulphate are also possible) by dissolving the base in a solution containing the relevant acid, or treated with acetic anhydride or rarely other chemicals capable of acetylating compounds to produce what is usually a mixture of heroin, morphine, 3-monoacetylmorphine and 6-monoacetylmorphine. Depending on the method, this can also contain acetylcodeine and leftover codeine.
See also
- Opioids
- Oxymorphone hydrazone
- Oxymorphol - a metabolite of oxymorphone and an intermediate in the creation of hydromorphone
- Hydromorphone
- Oxycodone
- Drug addiction
References
- ^ rxlist.com
- ^ Adams MP, Ahdieh H (2005). "Single- and multiple-dose pharmacokinetic and dose-proportionality study of oxymorphone immediate-release tablets". Drugs R D. 6 (2): 91–9. doi:10.2165/00126839-200506020-00004. PMID 15777102.
- ^ Sinatra, Raymond (2010). The Essence of Analgesia and Analgesics. MA, USA: Cambridge University Press; 1 edition. p. 123. ISBN 978-0521144506.
- ^ US patent 2806033, Mozes Juda Leweustein, "Morphine derivative", published 1955-03-08, issued 1957-10-09
- ^ "Actavis US launches Oxymorphone Extended-Release". Actavis.com. 2011-07-21. Retrieved 2012-11-03.
- ^ Stoll AL, Rueter S (December 1, 1999). "Treatment augmentation with opiates in severe and refractory major depression". Am J Psychiatry. 156 (12): 2017. PMID 10588427. Retrieved 2009-03-03.
- ^ Schürks M, Overlack M, Bonnet U (2005). "Naltrexone treatment of combined alcohol and opioid dependence: deterioration of co-morbid major depression". Pharmacopoeia. 38 (2): 100–2. doi:10.1055/s-2005-837812. PMID 15744636.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Tejedor-Real P, Mico JA, Maldonado R, Roques BP, Gibert-Rahola J (1995). "Implication of endogenous opioid system in the learned helplessness model of depression". Pharmacol Biochem Behav. 52 (1): 145–52. doi:10.1016/0091-3057(95)00067-7. PMID 7501657.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ "Dihydromorphinones from Morphine and Analogs - [www.rhodium.ws]". Erowid.org. Retrieved 2012-11-03.
