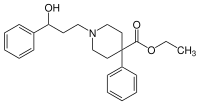
Phenoperidine
 | |
| Clinical data | |
|---|---|
| Routes of administration | Intravenous |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Metabolism | Liver |
| Excretion | Bile and Urine |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| ChemSpider | |
| UNII | |
| KEGG | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.008.391 |
| Chemical and physical data | |
| Formula | C23H29NO3 |
| Molar mass | 367.481 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| | |
Phenoperidine was discovered by Janssen Pharmaceutica 1960.[1] Marketed as its hydrochloride as Operidine or Lealgin, is an opioid used as a general anesthetic. It is a derivative of isonipecotic acid, like pethidine, and is metabolized in part to norpethidine. It is 20-200 times as potent as pethidine as an analgesic. The greatly increased potency essentially eliminates the toxic effects of norpethidine accumulation which are seen when pethidine is administered in high doses or for long periods of time.
In humans 1 milligram is equipotent with 10 mg morphine. It has less effect on the circulatory system and is less hypnotic than morphine, but it has about the same emetic effect. The nausea can be prevented by giving droperidol or haloperidol. After an intravenous dose the analgesia sets in after 3–5 minutes.[2]
Phenoperidine shares structural similarities with both pethidine and haloperidol (and related butyrophenone antipsychotics, e.g. droperidol). While not commonly used today in clinical practice, it is of historical interest as a precursor in the development of some of the most widely used neuroleptic drugs on the market today.
Introduction
Phenoperidine behaves in a similar way to morphine and is classified as a narcotic analgesic. It can be used as a neuroleptanalgesia, with droperidol for instance. [3] It is also known for its “high potency, rapid onset of action, the intensity of its peak effect and short duration of pharmacological effects." [4]
History and Synthesis
Phenoperidine was developed in 1957 through modifications of an existing drug. To begin, two key analgesic compounds, pethidine (meperidine) and methadone, were both synthesized by Otto Eisleb. Methadone preluded the synthesis of pethidine in 1939. Analogues of both of these drugs were investigated during World War II and years after, with the primary focus being on methadone. Janssen Pharmaceutica located in Belgium synthesized dextromoramide from methadone in 1954 and afterwards the company pursued pethidine analogues due in part to the less complicated chemistry of the compound. In doing so, the methyl group attached to the pethidine nitrogen was replaced by a propiophenone group. With this modification, phenoperidine was synthesized in 1957. Phenoperidine was determined to have decreased stability and enhanced lipophilicity compared to pethidine. Soon after, studies in mice showed that phenoperidine was over 100 times more potent than pethidine. [5] At the time, phenoperidine was the “most potent opioid in the world” and was used extensively in the European market but not in the United States. Through further advances, Janssen Pharmaceutica created fentanyl in 1960, which proved to be ten times more potent than phenoperidine. [6] Interestingly, additional modifications led to the discovery of one of the World Health Organization’s essential medicines, claimed to be “one of the greatest advances of the 20th century psychiatry”—haloperidol. [7]
Historical Uses
In 1980, pethidine, morphine, diamorphine, and phenoperidine were the most prevalent analgesics used. Phenoperidine was only used in surgery and intensive care units. [8] At this time there was also a transition to sedatives, such as phenoperidine, from muscle relaxants. In fact, 66% of patients receiving ventilated intensive therapy were given phenoperidine in a district general hospital, where phenoperidine was used in Great Britain for 20 years. Because of its respiratory depression, phenoperidine was useful in controlled ventilation cases. [9] Then, in 2000, phenoperidine was listed as a common narcotic epidural product. [10]
Regulations
Phenoperidine is classified as a schedule 1 opiate and is categorized as a Drug Enforcement Agency (DEA) controlled substance with a corresponding code 9641. [11]
Opioid Market
Opioid sales have more than doubled since 2001. In 2001, $3.97 billion were spent on opioids. In 2012, it rose to $8.34 billion and 240.9 million prescriptions. [12] In 2011, the total global morphine equivalent opioid consumption per person was 61.66 mg/capita. While in the Americas, the total morphine equivalent opioid consumption was roughly 750 mg/capita. [13]
Pharmacokinetics
Phenoperidine is cleared through both renal and hepatic mechanisms. It is primarily elminated by the liver. [14] The liver metabolizes the drug and produces active metabolites, meperidine and norpethidine, that are then renally eliminated in the urine. The elimination half-life is approximately 193 minutes while the clearance is 1.32 L/hr/kg. Although in the presence of chronic hepatic disease, the elimination half-life increases and the clearance decreases. [15]
The plasma concentration time profile of phenoperidine oftentimes has a secondary peak. Several other drug products have a similar secondary peak. It is believed that upon absorption into the GI tract, the drug is then reabsorbed into the plasma. Due to studies with antacid administration with phenoperidine, it appears that this secondary peak is heavily dependent upon the difference in pH of the stomach (pH 7.4) and plasma (pH 2.3). Antacid resulted in partial or complete elimination of the secondary peak. [16] This phenomenon is further investigated in Clinical Studies section when discussing the article, “Effect of Antacids on the Plasma Concentration of Phenoperidine.”
Interestingly, determining the concentration of the starting drug can be challenging and may have been responsible for the variability in reports of clearance and other pharmacokinetic parameters, as was the case in the differing reports of Fischer and Calvey. Calvey suggested that this may be due to the much greater metabolite concentration (5-10 times greater) that can then potentially cross react with phenoperidine, resulting in a greater detected concentration than the actual concentration of the unconjugated drug which leads to greater elimination half-lives. [17]
There have been reports of cardiovascular collapse, increased intracranial pressure, and decreased arterial pressure upon administration of phenoperidine in the past. [9]
According to a review article, the genotoxicity and carcinogenicity of phenoperidine was not available. [18]
Animal Studies
One animal study demonstrated that phenoperidine is 75 times more potent than morphine and 275 times more potent than pethidine. [4] Then, a synergistic analgesic effect was evident when in rats when phenoperidine was administered with clonidine. [19] Another study showed that phenoperidine decreased oxidation of rat liver mitochondria. [20]
Clinical Studies
During one study, the pharmacokinetics of phenoperidine were analyzed in patients with liver disease, having only minimal to moderate hepatic impairment. It was found that the plasma concentration is roughly 2 times greater when hepatic function is impaired. In addition, the secondary peak was much more profound in these patients. Compared to patients without any hepatic impairment, the elimination of the metabolites decreased while the elimination of the unchanged phenoperidine increased, as was expected with a liver that is not able to metabolize compounds as well. The volume of distribution was almost identical for hepatically impaired and stable patients. The elimination half-life was increased by 50% since the clearance decreased. Regardless, it was concluded that the pharmacokinetics of phenoperidine were not altered significantly with minimal to moderate hepatic impairment. [21]
One clinical study evaluated the pharmacokinetics of phenoperidine with and without antacid. Six healthy volunteers between the ages of 22 and 47 and weights of 55 and 90 kg were administered phenoperidine orally or intravenously in the presence or absence of Anduril, an antacid. The intravenous dosage was 15 µg/kg. Between 20 to 50 minutes, there was a secondary peak in the control group, but this peak was completely absent from 4 of the 6 patients with Andursil and decreased significantly in the other two. The plasma concentration was greater during the first 20 minutes when administered with Andursil. In fact for the control, at 2.5 minutes the plasma concentration was 9.1±1.6 ng/mL which decreased to 5.6±1 ng/mL at 20 minutes; for the antacid group, the plasma concentrations at the same time points were 14.7±2.5 and 6.1±0.7 ng/mL. In addition, the area under the curve (AUC) for the initial 20 minutes was 193.1±4.2 ng min/mL with antacid and 131.5±20.4 ng min/mL. Analyzing the AUCs from 0 to 180 minutes shows that these quantities are not significantly different (Control-617.9±73.3 ng min/mL and Antacid-588.9±38.9 ng min/mL). The total plasma clearance was very similar as well (Control-24±3.3 mL/min kg and Antacid-23.7±1.6 mL/min kg). In addition to intravenous studies, the pharmacokinetics of an oral formulation were also analyzed in two patients. The relative bioavailability was 9.9 and 13.5% (AUCs of 82 ng min/mL and 97.8 ng min/mL) for the two patients, illustrating the significant effect of first pass metabolism. [14]
There were some interesting findings in a study done in the early 1980s where 5 patients underwent general anaesthesia (abdominal surgery) and were administered 2 mg of phenoperidine intravenously. First, it was confirmed that phenoperidine, pethidine, and norpethidine are excreted in the urine. It was also seen that the greatest effects on respiration were evident between 5 to 15 minutes after delivery and maintained these respiratory levels for less than 60 minutes. In other words, the pharmacological effects last approximately 45 to 60 minutes, correlating to a required concentration greater than or equal to 5 ng/mL. In this study, the distribution half life varied from 3.19 to 14.23 minutes while the elimination half life ranged from 47.31 to 162.23 minutes. The phenoperidine was detected in the plasma for over 3 hours. [22]
Another surgery study was done in 30 patients undergoing minor surgery (predominantly genito-urinary). These patients received 0.077 mg/kg of phenoperidine intravenously. A constant pulse and blood pressure indicated that there were no signs of cardiovascular effects. Roughly 66.7% of the patients had vertical nystagmus, 16.7% nausea and vomiting, 16.7% had to have a larger dosage, 10% respiratory depression, 10% apnoea, 3.33% experienced unconsciousness. This study found that the administration of nalorphine following the surgery led to fewer implications. [4]
References
- ^ BE Patent 576331
- ^ Farmacevtiska specialiteter i Sverige (FASS) (in Swedish). Stockholm: Linfo. 1983. ISBN 91-85314-44-7.
- ^ "Phenoperidine". University of Rochester Medical Center. University of Rochester Medical Center. Retrieved 3 December 2014.
- ^ a b c Rollason, W.N. (1963). "Phenoperidine (R1406): A New Analgesic". Anaesthesia. 18 (1): 16-22.
{{cite journal}}:|access-date=requires|url=(help) - ^ Lopez-Munoz, Francisco; Alamo, Cecilio (2009). "The Consolidation of Neuroleptic Therapy: Janssen, the Discovery of Haloperidol and Its Introduction into Clinical Practice". Brain Research Bulletin. 79: 130-141.
{{cite journal}}:|access-date=requires|url=(help) - ^ Stanley, Theodore (2014). "The Fentanyl Story". The Journal of Pain. 15 (12): 1215-1226.
{{cite journal}}:|access-date=requires|url=(help) - ^ Lopez-Munoz, Francisco; Alamo, Cecilio (2009). "The Consolidation of Neuroleptic Therapy: Janssen, the Discovery of Haloperidol and Its Introduction into Clinical Practice". Brain Research Bulletin. 79: 130-141.
{{cite journal}}:|access-date=requires|url=(help) - ^ Chan, K.; Murray, G.R.; Rostron, C.; Calvey, T.N.; Williams, N.E. (1981). "Quantitative Gas-Liquid Chromatographic Method for Determination of Phenoperidine in Human Plasma". Journal of Chromatography. 223: 213-218.
{{cite journal}}:|access-date=requires|url=(help) - ^ a b Grummitt, R.M.; Goat, V.A. (1984). "Intracranial Pressure after Phenoperidine". Anaesthesia. 39: 565-567.
- ^ Aranda, Margaret; Hanson III, C. William (June 2000). "Anesthetics, Sedatives, and Paralytics: Understanding Their Use in the Intensive Care Unit". Surgical Clinics of North America. 80 (3).
{{cite journal}}:|access-date=requires|url=(help) - ^ "Dextromethorphan" (PDF). U.S. Food and Drug Administration. U.S. Food and Drug Administration. Retrieved 22 November 2014.
- ^ Meier, Barry; Marsh, Bill (22 June 2013). "The Soaring Cost of the Opioid Economy". The New York Times Company. The New York Times.
{{cite news}}:|access-date=requires|url=(help) - ^ "Regional". Pain & Policy Studies Group. Pain & Policy Studies, University of Wisconsin—Madison. Retrieved 2014-11-24.
- ^ a b Calvey, T.N.; Milne, L.A.; Williams, N.E.; Chan, K.; Murray, G.R. (1983). "Effect of Antacids on the Plasma Concentration of Phenoperidine". British Journal of Anaesthesia. 55 (1): 535-539.
- ^ Woerlee, G.M. (1992). Kinetics and Dynamics of Intravenous Anesthetics. Netherlands: Kluwer Academic Publishers.
{{cite book}}:|access-date=requires|url=(help) - ^ Davies, N.M.; Takemoto, J.K.; Brocks, D.R.; Yanez, J.A. (2010). "Multiple Peaking Phenomena in Pharmacokinetic Disposition". Clinical Pharmacokinetics. 49 (6): 351-377.
{{cite journal}}:|access-date=requires|url=(help) - ^ Calvey, T.N.; Williams, N.E. (1986). "Pharmacokinetics of Phenoperidine". British Journal of Anaesthesia. 58: 821-822.
- ^ Brambilla, Giovanni; Martelli, Antonietta (2009). "Update on Genotoxicity and Carcinogenicity Testing of 472 Marketed Pharmaceuticals". Mutation Research/Reviews in Mutation Research. 681: 200-229.
- ^ Yang, J.P.; Jiang, H.; Wu, J. (1990). "Synergic Antinociceptive Effects of Clonidine and Phenoperidine". Pain. S 112.
- ^ Kim, Leng EA; Cros, Jean (1979). "Effects of Phenoperidine on Rat Liver Mitochondrial Respiration". Biochemical Pharmacology. 28: 361-366.
{{cite journal}}:|access-date=requires|url=(help) - ^ Isherwood, C.N.; Calvey, T.N.; Williams, N.E.; Chan, K.; Murray, G.R. (1984). "Elimination of Phenoperidine in Liver Disease". British Journal of Anaesthesia. 56: 843-847.
- ^ Milne, L.; Williams, N.E.; Calvey, T.N.; Murray, G.R.; Chan, K. (1980). "Plasma Concentration and Metabolism of Phenoperidine in Man". British Journal of Anaesthesia. 52: 537-540.
External links
- Kintz, P.; Godelar, B.; Mangin, P.; Lugnier, A.; Chaumont, A. (1989). "Simultaneous Determination of Pethidine (Meperidine), Phenoperidine, and Norpethidine (Normeperidine), their Common Metabolite, by Gas Chromatography with Selective Nitrogen Detection". Forensic Science International. 43 (3): 267–273. doi:10.1016/0379-0738(89)90154-0. PMID 2613140.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Claris, O.; Bertrix, L. (1988). "Phenoperidine: Pharmacology and Use in Pediatric Resuscitation". Pédiatrie (in French). 43 (6): 509–513. PMID 3186421.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - "Antipsychotics - Reference pathway". Kyoto Encyclopedia of Genes and Genomes. Kanehisa Laboratories, Kyoto University, University of Tokyo. Retrieved 2007-01-16.
