Zolpidem: Difference between revisions
m →Recreational use: cite repair; |
→Adverse effects: state more simply; WP:REFPUNCT |
||
| Line 94: | Line 94: | ||
A 2009 meta-analysis found a 44% higher rate of mild [[infection]]s, such as [[pharyngitis]] or [[sinusitis]], in people taking zolpidem or other hypnotic drugs compared to those taking a placebo.<ref>{{cite journal|pmc=2725260|year=2009|author1=Joya|first1=FL|title=Meta-Analyses of Hypnotics and Infections: Eszopiclone, Ramelteon, Zaleplon, and Zolpidem|journal=Journal of Clinical Sleep Medicine|volume=5|issue=4|pages=377–383|last2=Kripke|first2=DF|last3=Loving|first3=RT|last4=Dawson|first4=A|last5=Kline|first5=LE}}</ref> |
A 2009 meta-analysis found a 44% higher rate of mild [[infection]]s, such as [[pharyngitis]] or [[sinusitis]], in people taking zolpidem or other hypnotic drugs compared to those taking a placebo.<ref>{{cite journal|pmc=2725260|year=2009|author1=Joya|first1=FL|title=Meta-Analyses of Hypnotics and Infections: Eszopiclone, Ramelteon, Zaleplon, and Zolpidem|journal=Journal of Clinical Sleep Medicine|volume=5|issue=4|pages=377–383|last2=Kripke|first2=DF|last3=Loving|first3=RT|last4=Dawson|first4=A|last5=Kline|first5=LE}}</ref> |
||
A 2018 meta-analysis of [[Observational study|observational studies]] found that use of hypnotics, including Zolpidem, was "significantly associated with an increased risk" of some types of cancer.<ref name="pmid29973038">{{cite journal |vauthors=Kim DH, Kim HB, Kim YH, Kim JY |title=Use of Hypnotics and Risk of Cancer: A Meta-Analysis of Observational Studies |journal=Korean Journal of Family Medicine |volume=39 |issue=4 |pages=211-218 |date=July 2018 |pmid=29973038 |doi=10.4082/kjfm.17.0025 |doi-access=free |pmc=6056405}}</ref> |
|||
===Tolerance, dependence, and withdrawal=== |
===Tolerance, dependence, and withdrawal=== |
||
Revision as of 16:54, 17 August 2018
 | |
 | |
| Clinical data | |
|---|---|
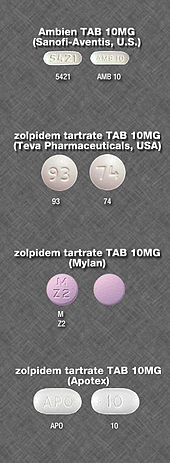
| Trade names | Ambien, Stilnoct, others[1] |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a693025 |
| Pregnancy category |
|
| Dependence liability | High |
| Routes of administration | By mouth (tablet), sublingual, oromucosal (spray), rectal |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | 70% (by mouth) |
| Protein binding | 92% |
| Metabolism | Liver through CYP3A4 |
| Elimination half-life | 2–3 hours[3] |
| Duration of action | 3 hours |
| Excretion | Kidney (56%) fecal (34%) |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.115.604 |
| Chemical and physical data | |
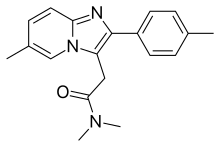
| Formula | C19H21N3O |
| Molar mass | 307.395 g/mol g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| | |
Zolpidem, sold under the brand name Ambien, among others,[1] is a sedative primarily used for the treatment of sleeping problems.[3] It is typically only recommended if sleep hygiene is not effective.[2] It decreases the time to sleep onset by about 15 minutes and at larger doses helps people stay asleep longer.[2] It is taken by mouth and is available in a long acting formulation.[3]
Common side effects include daytime sleepiness, headache, nausea, and diarrhea.[3] Other side effects include memory problems, hallucinations, and abuse.[2] The recommended dose was decreased in 2013 due to next-morning impairment.[4] Additionally driving the next morning is not recommended with either higher doses or the long acting formulation.[4] While flumazenil can reverse zolpidem's effects, usually supportive care is all that is recommended in overdose.[5]
Zolpidem is a nonbenzodiazepine of the imidazopyridine class.[3] It works by increasing GABA effects in the central nervous system by binding to GABAA receptors at the same location as benzodiazepines.[3] It generally has a half-life of two to three hours.[3] This, however, is increased in those with liver problems.[3]
Zolpidem was approved for medical use in the United States in 1992.[3] It became available as a generic medication in 2007.[6] In the United States it has a monthly cost of about US$8 for immediate release and US$66 for controlled release medication, as of 2017.[2] In that country more than 10 million prescriptions are filled a year, making it one of the most commonly used treatments for sleeping problems.[7][8]
Medical uses

Sleep
Zolpidem is typically only recommended for short-term (usually about two to six weeks) treatment of insomnia.[9] It may be used for both improving sleep onset and staying asleep.[2] Also, a 2012 review found that zolpidem's effectiveness is nearly as much due to psychological effects as to the medication itself, so "increased attention should be directed at psychological intervention of insomnia."[10] A lower-dose version (3.5 mg for men and 1.75 mg for women) is administered as a sub-lingual tablet and used for middle-of-the night awakenings. It can be taken if there is at least 4 hours between the time of administration and when the person must be awake.[11]
Other
Zolpidem has some muscle relaxant and anticonvulsant properties, but has not been approved for use in muscle relaxation or seizure prevention. This is because the dosage of drug needed to cause muscle relaxation is 10 times the sedating dose, while early studies indicated that the dosage needed for preventing seizures is 20 times the sedating dose.[12]
Adverse effects
The most common side effects for short-term use include headache (reported by 7% of people in clinical trials) drowsiness (2%), dizziness (1%), and diarrhea (1%); the most common side effects of long-term use included dry mouth (3%), allergy (4%), back pain (3%), flu-like symptoms (1%), chest pain (1%), heart palpitations (2%), drowsiness (8%), dizziness (5%), lethargy (3%), drugged feeling (3%), lightheadedness (2%), depression (1%), abnormal dreams (1%), amnesia (1%), sleep disorder (1%), diarrhea (3%), abdominal pain (2%), constipation (2%), sinusitis (4%), sore throat (3%), and rash (2%).[13]
Sleeping pills, including zolpidem, have been associated with an increased risk of death.[14]
Some users have reported unexplained sleepwalking[15] while using zolpidem, as well as sleep driving,[15] night eating syndrome while asleep, and performing other daily tasks while sleeping. Research by Australia's National Prescribing Service found these events occur mostly after the first dose taken, or within a few days of starting therapy.[16] Rare reports of sexual parasomnia (sleep sex) episodes related to zolpidem intake have also been reported.[17] Sleepwalkers can sometimes perform these tasks as normally as they might if they were awake.
Residual 'hangover' effects, such as sleepiness and impaired psychomotor and cognitive function, may persist into the day following nighttime administration. Such effects may impair the ability of users to drive safely and increase risks of falls and hip fractures.[15][18]
In February 2008, the Australian Therapeutic Goods Administration attached a boxed warning, stating that "Zolpidem may be associated with potentially dangerous complex sleep-related behaviours that may include sleep walking, sleep driving, and other bizarre behaviours... Limit use to four weeks maximum under close medical supervision."[19]
A 2009 meta-analysis found a 44% higher rate of mild infections, such as pharyngitis or sinusitis, in people taking zolpidem or other hypnotic drugs compared to those taking a placebo.[20]
A 2018 meta-analysis of observational studies found that use of hypnotics, including Zolpidem, was "significantly associated with an increased risk" of some types of cancer.[21]
Tolerance, dependence, and withdrawal

A review medical publication found long-term use of zolpidem is associated with drug tolerance, substance dependence, rebound insomnia, and CNS-related adverse effects. It was recommended that zolpidem be used for short periods of time using the lowest effective dose. Zolpidem 10 mg is effective in treating insomnia when used intermittently no fewer than three and no more than five pills per week for a period of 12 weeks.[22]
Nonpharmacological treatment options (e.g. cognitive behavioral therapy for insomnia), however, were found to have sustained improvements in sleep quality.[23] Animal studies of the tolerance-inducing properties have shown that in rodents, zolpidem has less tolerance-producing potential than benzodiazepines, but in primates the tolerance-producing potential of zolpidem was the same as that of benzodiazepines.[24] Tolerance to the effects of zolpidem can develop in some people in just a few weeks. Abrupt withdrawal may cause delirium, seizures, or other severe effects, especially if used for prolonged periods and at high dosages.[25][26][27]
When drug tolerance and physical dependence to zolpidem has developed, treatment usually entails a gradual dose reduction over a period of months to minimise withdrawal symptoms, which can resemble those seen during benzodiazepine withdrawal. Failing that, an alternative method may be necessary for some patients, such as a switch to a benzodiazepine equivalent dose of a longer-acting benzodiazepine drug, such as diazepam or chlordiazepoxide, followed by a gradual reduction in dosage of the long-acting benzodiazepine. Sometimes for difficult-to-treat patients, an inpatient flumazenil rapid detoxification program can be used to detoxify from a zolpidem drug dependence or addiction.[28]
Alcohol has cross tolerance with GABAA receptor positive modulators such as the benzodiazepines and the nonbenzodiazepine drugs. For this reason, alcoholics or recovering alcoholics may be at increased risk of physical dependency on zolpidem. Also, alcoholics and recreational drug users may have an increased likelihood of abuse and or becoming psychologically dependent on zolpidem.[29][30][31] It is not typically prescribed in those with a history of alcoholism, recreational drug use, physical dependency, or psychological dependency on sedative-hypnotic drugs. Zolpidem has rarely been associated with drug-seeking behavior,[citation needed] the likelihood of which is amplified in patients with a history of recreational use of drugs or alcohol.
Overdose
An overdose of zolpidem may cause excessive sedation, pin-point pupils, or depressed respiratory function, which may progress to coma, and possibly death. Combined with alcohol, opiates, or other CNS depressants, it may be even more likely to lead to fatal overdoses. Zolpidem overdosage can be treated with the benzodiazepine receptor antagonist flumazenil, which displaces zolpidem from its binding site on the benzodiazepine receptor to rapidly reverse the effects of the zolpidem.[32]
Detection in body fluids
Zolpidem may be quantitated in blood or plasma to confirm a diagnosis of poisoning in hospitalized patients, provide evidence in an impaired driving arrest, or to assist in a medicolegal death investigation. Blood or plasma zolpidem concentrations are usually in a range of 30–300 μg/l in persons receiving the drug therapeutically, 100–700 μg/l in those arrested for impaired driving, and 1000–7000 μg/l in victims of acute overdosage. Analytical techniques, in general, involve gas or liquid chromatography.[33][34][35]
Special precautions
Driving
Use of zolpidem may impair driving skills with a resultant increased risk of road traffic accidents. This adverse effect is not unique to zolpidem but also occurs with other hypnotic drugs. Caution should be exercised by motor vehicle drivers.[36] Studies showed that eight hours after a bedtime dose of 10 mg, 15% of women and 3% of men would have blood levels that produce impaired driving skills; for an extended-release dose of 12.5 mg, the risk increased to 33% and 25%, respectively. As a consequence, the FDA recommended the dose for women be reduced and that prescribers should consider lower doses for men.[37][38]
Elderly
The elderly are more sensitive to the effects of hypnotics including zolpidem. Zolpidem causes an increased risk of falls and may induce adverse cognitive effects.[39]
In 2015, the American Geriatrics Society recommended that zolpidem should "be avoided without consideration of duration of use because of 'its' association with harms balanced with 'its' minimal efficacy in treating insomnia."[40] This was a change from the 2012 recommendation, which suggested limiting use to 90 days or less.[40]
An extensive review of the medical literature regarding the management of insomnia and the elderly found that there is considerable evidence of the effectiveness and durability of nondrug treatments for insomnia in adults of all ages, and these interventions are underused. Compared with the benzodiazepines, the nonbenzodiazepine (including zolpidem) sedative-hypnotics appeared to offer few, if any, significant clinical advantages in efficacy or tolerability in elderly persons. Newer agents with novel mechanisms of action and improved safety profiles, such as the melatonin receptor agonists, were found to hold promise for the management of chronic insomnia in elderly people.
Long-term use of sedative-hypnotics for insomnia lacks an evidence base and has traditionally been discouraged for reasons that include concerns about such potential adverse drug effects as cognitive impairment (anterograde amnesia), daytime sedation, motor incoordination, and increased risk of motor vehicle accidents and falls. In addition, the effectiveness and safety of long-term use of these agents remain to be determined. More research is needed to evaluate the long-term effects of treatment and the most appropriate management strategy for elderly persons with chronic insomnia.[41]
Gastroesophageal reflux disease
Patients suffering from gastroesophageal reflux disease (GERD) had reflux events measured to be significantly longer when taking zolpidem than on placebo. The same trend was found for reflux events in patients without GERD. This is assumed to be due to suppression of arousal during the reflux event, which would normally result in a swallowing reflex to clear gastric acid from the esophagus. Patients with GERD experience significantly higher esophageal exposure to gastric acid, which increases the likelihood of their developing esophageal cancer.[42]
Pregnancy
Zolpidem has been assigned to pregnancy category C by the FDA. Animal studies have revealed evidence of incomplete ossification and increased postimplantation fetal loss at doses greater than seven times the maximum recommended human dose or higher; however, teratogenicity was not observed at any dose level. There are no controlled data in human pregnancy. In one case report, zolpidem was found in cord blood at delivery. Zolpidem is recommended for use during pregnancy only when benefits outweigh risks. [43]
Mechanism of action

Zolpidem is a high-affinity positive modulator of GABAA receptors. It selectively binds to α1 subunits of this pentameric ion channel. Accordingly, it has strong hypnotic properties and weak anxiolytic, myorelaxant, and anticonvulsant properties.[44] Opposed to diazepam, zolpidem is able to bind to binary αβ GABA receptors, where it was shown to bind to the α1–α1 subunit interface.[45] Zolpidem has about 10-fold lower affinity for the α2- and α3- subunits than for α1, and no appreciable affinity for α5 subunit-containing receptors.[46][47] ω1 type GABAA receptors are the α1-containing GABAA receptors and are found primarily in the brain, the ω2 receptors are those that contain the α2-, α3-, α4-, α5-, or α6 subunits, and are found primarily in the spine. Thus, zolpidem favours binding to GABAA receptors located in the brain rather the spine.[48] Zolpidem has no affinity for γ1 and γ3 subunit-containing receptors and, like the vast majority of benzodiazepine-like drugs, it lacks affinity for receptors containing α4 and α6.[49] Zolpidem modulates the receptor presumably by inducing a receptor conformation that enables an increased binding strength of the orthosteric agonist GABA towards its cognate receptor without affecting desensitization or peak currents.[50]
Like zaleplon, zolpidem may increase slow wave sleep but cause no effect on stage 2 sleep.[51] A meta-analysis that compared benzodiazepines against nonbenzodiazepines has shown few consistent differences between zolpidem and benzodiazepines in terms of sleep onset latency, total sleep duration, number of awakenings, quality of sleep, adverse events, tolerance, rebound insomnia, and daytime alertness.[52]
Chemistry
Three syntheses of zolpidem are common. 4-methylacetophenone is used as a common precursor. This is brominated and reacted with 2-amino-5-methylpyridine to give the imidazopyridine. From here the reactions use a variety of reagents to complete the synthesis, either involving thionyl chloride or sodium cyanide. These reagents are challenging to handle and require thorough safety assessments.[53][54][55] Though such safety procedures are common in industry, they make clandestine manufacture difficult.
A number of major side-products of the sodium cyanide reaction have been characterised and include dimers and mannich products.[56]
Drug–drug interactions
Notable drug–drug interactions with the pharmacokinetics of zolpidem include chlorpromazine, fluconazole, imipramine, itraconazole, ketoconazole, rifampicin, and ritonavir. Interactions with carbamazepine and phenytoin can be expected based on their metabolic pathways, but have not yet been studied. There does not appear to be any interaction between zolpidem and cimetidine or ranitidine.[57][58] However, it was noted in the same study that cimetidine did appear to prolong the hypnotic effects of Zolpidem beyond its typical 3 hour duration, which is indicative of some sort of metabolic interaction.[57]
Usage
Zolpidem is one of the most common GABA-potentiating sleeping medications prescribed in the Netherlands, with a total of 582,660 prescriptions dispensed in 2008.[59]
The United States Air Force uses zolpidem as one of the hypnotics approved as a "no-go pill" (with a 6-hour restriction on subsequent flight operation) to help aviators and special duty personnel sleep in support of mission readiness. (The other hypnotics used are temazepam and zaleplon.) "Ground tests" are required prior to authorization issued to use the medication in an operational situation.[60]
Society and culture
Recreational use
Zolpidem has potential for either medical misuse when the drug is continued long term without or against medical advice, or for recreational use when the drug is taken to achieve a "high".[61][62] The transition from medical use of zolpidem to high-dose addiction or drug dependence can occur with use, but some believe it may be more likely when used without a doctor's recommendation to continue using it, when physiological drug tolerance leads to higher doses than the usual 5 mg or 10 mg, when consumed through inhalation or injection, or when taken for purposes other than as a sleep aid.[61] Recreational use is more prevalent in those having been dependent on other drugs in the past, but tolerance and drug dependence can still sometimes occur in those without a history of drug dependence. Chronic users of high doses are more likely to develop physical dependence on the drug, which may cause severe withdrawal symptoms, including seizures, if abrupt withdrawal from zolpidem occurs.[63]
Other drugs, including the benzodiazepines and zopiclone, are also found in high numbers of suspected drugged drivers.[64] Many drivers have blood levels far exceeding the therapeutic dose range suggesting a high degree of excessive-use potential for benzodiazepines, zolpidem and zopiclone.[65] U.S. Congressman Patrick J. Kennedy says that he was using Zolpidem (Ambien) and Phenergan when caught driving erratically at 3 am.[66] "I simply do not remember getting out of bed, being pulled over by the police, or being cited for three driving infractions," Kennedy said.
Nonmedical use of zolpidem is increasingly common in the U.S., Canada, and the UK. Some users have reported decreased anxiety, mild euphoria, perceptual changes, visual distortions, and hallucinations.[67] Zolpidem was used by Australian Olympic swimmers at the London Olympics in 2012, leading to controversy.[68]
Regulation
For the stated reason of its potential for recreational use and dependence, zolpidem (along with the other benzodiazepine-like Z-drugs) is a Schedule IV substance under the Controlled Substances Act in the U.S. The United States patent for zolpidem was held by the French pharmaceutical corporation Sanofi-Aventis.[69]
Date rape drug
Zolpidem has become one of many date rape drugs.[70][71] Unlike Rohypnol ("roofies"), which was banned in 1996, zolpidem is available legally by prescription, and unlike gamma-hydroxybutyrate, which is used to treat a rare form of narcolepsy, zolpidem was prescribed 43.8 million times in the U.S. in 2012.[70] It dissolves readily in liquids such as wine,[70] and can typically be detected in bodily fluids for only 36 hours, though it may be possible to detect it by hair testing much later;[70] this is due to the short elimination half-life of 2.5–3 hours.[72] This application of the drug was highlighted during proceedings against Darren Sharper, who was accused of using the tablets he was prescribed to facilitate a series of rapes.[70][71]
Sleepwalking
Zolpidem received widespread media coverage in Australia after the death of a student who fell 20 m from the Sydney Harbour Bridge while under the influence of zolpidem.[73]
Research
While cases of zolpidem improving aphasia in people with stroke have been described, use for this purpose has unclear benefit.[74] Zolpidem has also been studied in persistent vegetative states with unclear effect.[75] A 2017 systematic review concluded that while there is preliminary evidence of benefit for treating disorders of movement and consciousness other than insomnia (including Parkinson's disease), more research is needed.[76]
References
- ^ a b "Zolpidem - Drugs.com". Drugs.com. Retrieved 15 March 2018.
- ^ a b c d e f Matheson, E; Hainer, BL (1 July 2017). "Insomnia: Pharmacologic Therapy". American Family Physician. 96 (1): 29–35. PMID 28671376.
- ^ a b c d e f g h i "Zolpidem Tartrate". The American Society of Health-System Pharmacists. Retrieved 15 March 2018.
- ^ a b "Drug Safety and Availability - FDA Drug Safety Communication: FDA approves new label changes and dosing for zolpidem products and a recommendation to avoid driving the day after using Ambien CR". www.fda.gov.
- ^ Gunja, N (June 2013). "The clinical and forensic toxicology of Z-drugs". Journal of medical toxicology : official journal of the American College of Medical Toxicology. 9 (2): 155–62. doi:10.1007/s13181-013-0292-0. PMC 3657020. PMID 23404347.
- ^ "FDA Approves First Generic Versions of Ambien (Zolpidem Tartrate) for the Treatment of Insomnia". Retrieved 2010-01-24.
- ^ "Zolpidem". LiverTox. Retrieved 15 March 2018.
- ^ "Consumer Updates - Some Sleep Drugs Can Impair Driving". www.fda.gov. 13 June 2013. Retrieved 15 March 2018.
- ^ "Ambien". The American Society of Health-System Pharmacists. Retrieved 3 April 2011.
- ^ Huedo-Medina TB, Kirsch I, Middlemass J, Klonizakis M, Siriwardena AN (Dec 17, 2012). "Effectiveness of non-benzodiazepine hypnotics in treatment of adult insomnia: meta-analysis of data submitted to the Food and Drug Administration". BMJ (Clinical research ed.). 345: e8343. doi:10.1136/bmj.e8343. PMC 3544552. PMID 23248080.
- ^ "Intermezzo (Zolpidem Tartarate)". rxlist.com. Retrieved 5 February 2018.
- ^ Depoortere H, Zivkovic B, Lloyd KG, Sanger DJ, Perrault G, Langer SZ, Bartholini G (1986). "Zolpidem, a novel nonbenzodiazepine hypnotic. I. Neuropharmacological and behavioral effects". J. Pharmacol. Exp. Ther. 237 (2): 649–58. PMID 2871178.
- ^ "US Label" (PDF). FDA. August 2016. Retrieved 2016-09-30. See FDA label index page for updates
- ^ Kripke, DF (February 2016). "Mortality Risk of Hypnotics: Strengths and Limits of Evidence". Drug safety. 39 (2): 93–107. doi:10.1007/s40264-015-0362-0. PMID 26563222.
- ^ a b c Gunja N (2013). "In the Zzz zone: the effects of Z-drugs on human performance and driving". J Med Toxicol. 9 (2): 163–71. doi:10.1007/s13181-013-0294-y. PMC 3657033. PMID 23456542.
- ^ "Zolpidem and sleep-related behaviours" (PDF). NPS Position Statement. National Prescribing Service Limited. July 2008. Archived from the original (PDF) on 2012-04-10.
- ^ Schenck CH, Arnulf I, Mahowald MW (2007). "Sleep and sex: what can go wrong? A review of the literature on sleep related disorders and abnormal sexual behaviors and experiences". Sleep. 30 (6): 683–702. PMC 1978350. PMID 17580590.
- ^ Vermeeren A (2004). "Residual effects of hypnotics: epidemiology and clinical implications". CNS Drugs. 18 (5): 297–328. doi:10.2165/00023210-200418050-00003. PMID 15089115.
- ^ Australian Government. "Zolpidem ("Stilnox") – updated information – February 2008". www.tga.gov.au. Archived from the original on 2007-08-12. Retrieved 2009-06-22.
- ^ Joya, FL; Kripke, DF; Loving, RT; Dawson, A; Kline, LE (2009). "Meta-Analyses of Hypnotics and Infections: Eszopiclone, Ramelteon, Zaleplon, and Zolpidem". Journal of Clinical Sleep Medicine. 5 (4): 377–383. PMC 2725260.
- ^ Kim DH, Kim HB, Kim YH, Kim JY (July 2018). "Use of Hypnotics and Risk of Cancer: A Meta-Analysis of Observational Studies". Korean Journal of Family Medicine. 39 (4): 211–218. doi:10.4082/kjfm.17.0025. PMC 6056405. PMID 29973038.
- ^ Perlis ML, McCall WV, Krystal AD, Walsh JK (2004). "Long-term, non-nightly administration of zolpidem in the treatment of patients with primary insomnia". The Journal of Clinical Psychiatry. 65 (8): 1128–1137. doi:10.4088/jcp.v65n0816. PMID 15323600.
- ^ Kirkwood CK (1999). "Management of insomnia". J Am Pharm Assoc (Wash). 39 (5): 688–96, quiz 713–4. PMID 10533351.
- ^ Petroski RE, Pomeroy JE, Das R, Bowman H, Yang W, Chen AP, Foster AC (April 2006). "Indiplon is a high-affinity positive allosteric modulator with selectivity for alpha1 subunit-containing GABAA receptors" (PDF). J. Pharmacol. Exp. Ther. 317 (1): 369–77. doi:10.1124/jpet.105.096701. PMID 16399882.
- ^ Harter C, Piffl-Boniolo E, Rave-Schwank M (November 1999). "[Development of drug withdrawal delirium after dependence on zolpidem and zoplicone]" [Development of drug withdrawal delirium after dependence on zolpidem and zoplicone]. Psychiatr Prax (in German). 26 (6): 309. PMID 10627964.
- ^ "Hypnotic dependence: zolpidem and zopiclone too". Prescrire Int. 10 (51): 15. February 2001. PMID 11503851.
- ^ Sethi PK, Khandelwal DC (February 2005). "Zolpidem at supratherapeutic doses can cause drug abuse, dependence and withdrawal seizure" (PDF). J Assoc Physicians India. 53: 139–40. PMID 15847035.
- ^ Quaglio G, Lugoboni F, Fornasiero A, Lechi A, Gerra G, Mezzelani P (September 2005). "Dependence on zolpidem: two case reports of detoxification with flumazenil infusion". Int Clin Psychopharmacol. 20 (5): 285–7. doi:10.1097/01.yic.0000166404.41850.b4. PMID 16096519.
- ^ Victorri-Vigneau, Caroline; Gérardin, Marie; Rousselet, Morgane; Guerlais, Marylène; Grall-Bronnec, Marie; Jolliet, Pascale (2014). "An Update on Zolpidem Abuse and Dependence". Journal of Addictive Diseases. 33 (1): 15–23. doi:10.1080/10550887.2014.882725. PMID 24467433.
- ^ Victorri-Vigneau, Caroline; Dailly, Eric; Veyrac, Gwenaëlle; Jolliet, Pascale (2007). "Evidence of zolpidem abuse and dependence: Results of the French Centre for Evaluation and Information on Pharmacodependence (CEIP) network survey". British Journal of Clinical Pharmacology. 64 (2): 198–209. doi:10.1111/j.1365-2125.2007.02861.x. PMC 2000636. PMID 17324242.
- ^ "Zolpidem Abuse".
- ^ Lheureux P, Debailleul G, De Witte O, Askenasi R (1990). "Zolpidem intoxication mimicking narcotic overdose: response to flumazenil". Human & Experimental Toxicology. 9 (2): 105–7. doi:10.1177/096032719000900209. PMID 2111156.
- ^ Jones AW, Holmgren A, Kugelberg FC (2007). "Concentrations of scheduled prescription drugs in blood of impaired drivers: considerations for interpreting the results". Ther. Drug Monit. 29 (2): 248–260. doi:10.1097/FTD.0b013e31803d3c04. PMID 17417081.
- ^ Gock SB, Wong SH, Nuwayhid N, Venuti SE, Kelley PD, Teggatz JR, Jentzen JM (1999). "Acute zolpidem overdose—report of two cases". J. Anal. Toxicol. 23 (6): 559–562. doi:10.1093/jat/23.6.559. PMID 10517569.
- ^ R. Baselt (2011). Disposition of Toxic Drugs and Chemicals in Man (9th ed.). Seal Beach, CA: Biomedical Publications. pp. 1836–1838.
- ^ Gustavsen I, Bramness JG, Skurtveit S, Engeland A, Neutel I, Mørland J (December 2008). "Road traffic accident risk related to prescriptions of the hypnotics zopiclone, zolpidem, flunitrazepam and nitrazepam". Sleep Med. 9 (8): 818–22. doi:10.1016/j.sleep.2007.11.011. PMID 18226959.
- ^ "FDA Requires Lower Dosing of Zolpidem". The Medical Letter on Drugs and Therapeutics. 55 (1408). The Medical Letter: 5. January 21, 2013. Retrieved April 14, 2013.
- ^ "FDA Drug Safety Communication: Risk of next-morning impairment after use of insomnia drugs; FDA requires lower recommended doses for certain drugs containing zolpidem (Ambien, Ambien CR, Edluar, and Zolpimist)". FDA. January 10, 2013. Retrieved April 14, 2013.
{{cite journal}}: Cite journal requires|journal=(help) - ^ Antai-Otong D (August 2006). "The art of prescribing. Risks and benefits of non-benzodiazepine receptor agonists in the treatment of acute primary insomnia in older adults". Perspect Psychiatr Care. 42 (3): 196–200. doi:10.1111/j.1744-6163.2006.00070.x. PMID 16916422.
- ^ a b Fick DM, Semla TP, Beizer J, Brandt N (2015). "American Geriatrics Society 2015 Updated Beers Criteria for Potentially Inappropriate Medication Use in Older Adults" (PDF). Journal of the American Geriatrics Society. 63 (11): 2227–2246. doi:10.1111/jgs.13702. PMID 26446832.
- ^ Bain KT (June 2006). "Management of chronic insomnia in elderly persons". Am J Geriatr Pharmacother. 4 (2): 168–92. doi:10.1016/j.amjopharm.2006.06.006. PMID 16860264.
- ^ Gagliardi GS, Shah AP, Goldstein M, Denua-Rivera S, Doghramji K, Cohen S, Dimarino AJ (September 2009). "Effect of zolpidem on the sleep arousal response to nocturnal esophageal acid exposure". Clin. Gastroenterol. Hepatol. 7 (9): 948–52. doi:10.1016/j.cgh.2009.04.026. PMID 19426833.
- ^ Drugsdb.eu. "Zolpidem Pregnancy Warnings". Retrieved 2014-02-01.
- ^ Salvà P, Costa J (September 1995). "Clinical pharmacokinetics and pharmacodynamics of zolpidem. Therapeutic implications". Clin Pharmacokinet. 29 (3): 142–53. doi:10.2165/00003088-199529030-00002. PMID 8521677.
- ^ Che Has AT, Absalom N, van Nieuwenhuijzen PS, Clarkson AN, Ahring PK, Chebib M (2016). "Zolpidem is a potent stoichiometry-selective modulator of α1β3 GABAA receptors: evidence of a novel benzodiazepine site in the α1-α1 interface". Sci Rep. 6: 28674. doi:10.1038/srep28674. PMC 4921915. PMID 27346730.
- ^ Pritchett DB, Seeburg PH (1990). "Gamma-aminobutyric acidA receptor alpha 5-subunit creates novel type II benzodiazepine receptor pharmacology". J. Neurochem. 54 (5): 1802–4. doi:10.1111/j.1471-4159.1990.tb01237.x. PMID 2157817.
- ^ Smith AJ, Alder L, Silk J, Adkins C, Fletcher AE, Scales T, Kerby J, Marshall G, Wafford KA, McKernan RM, Atack JR (2001). "Effect of alpha subunit on allosteric modulation of ion channel function in stably expressed human recombinant gamma-aminobutyric acid(A) receptors determined using (36)Cl ion flux" (PDF). Mol. Pharmacol. 59 (5): 1108–18. PMID 11306694.
- ^ Rowlett JK, Woolverton WL (November 1996). "Assessment of benzodiazepine receptor heterogeneity in vivo: apparent pA2 and pKB analyses from behavioral studies". Psychopharmacology. 128 (1): 1–16. doi:10.1007/s002130050103. PMID 8944400. Archived from the original on January 12, 2002.
{{cite journal}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Wafford KA, Thompson SA, Thomas D, Sikela J, Wilcox AS, Whiting PJ (1996). "Functional characterization of human gamma-aminobutyric acidA receptors containing the alpha 4 subunit". Mol. Pharmacol. 50 (3): 670–8. PMID 8794909.
- ^ Perrais D, Ropert N (1999). "Effect of zolpidem on miniature IPSCs and occupancy of postsynaptic GABAA receptors in central synapses". J. Neurosci. 19 (2): 578–88. PMID 9880578.
- ^ Noguchi H, Kitazumi K, Mori M, Shiba T (2004). "Electroencephalographic properties of zaleplon, a non-benzodiazepine sedative/hypnotic, in rats". J. Pharmacol. Sci. 94 (3): 246–51. doi:10.1254/jphs.94.246. PMID 15037809.
WARNING: The reference indicates that zaleplon-Sonata, not zolpidem, increases Slow-wave sleep
- ^ Dündar Y, Dodd S, Strobl J, Boland A, Dickson R, Walley T (2004). "Comparative efficacy of newer hypnotic drugs for the short-term management of insomnia: a systematic review and meta-analysis". Human psychopharmacology. 19 (5): 305–22. doi:10.1002/hup.594. PMID 15252823.
- ^ Johnson DS, Li JJ (2007). The art of drug synthesis. Hoboken, N.J.: Wiley-Interscience. pp. Chapter 15, Section 2. ISBN 9780471752158.
- ^ IN 246080, Rawalnath, Sakhardande Rajiv; Crasta Santosh, Richard & SAXENA, ALOK, "Process for the preparation of zolpidem", published 21 Dec 2005, issued 14-Feb-2011
- ^ Sumalatha, Y. (2009). "A simple and efficient synthesis of hypnotic agent, zolpidem and its related substances". Arkivoc. 2009 (2): 315–320. doi:10.3998/ark.5550190.0010.230.
- ^ Sumalatha, Y. (2009). "Synthesis and spectral characterization of zolpidem related substances - hypnotic agent". Arkivoc. 2009 (7): 143–149. doi:10.3998/ark.5550190.0010.714.
- ^ a b Hulhoven R, Desager JP, Harvengt C, Hermann P, Guillet P, Thiercelin JF (1988). "Lack of interaction between zolpidem and H2 antagonists, cimetidine and ranitidine". International journal of clinical pharmacology research. 8 (6): 471–476. PMID 3253224.
- ^ Wang JS, DeVane CL; Devane (2003). "Pharmacokinetics and drug interactions of the sedative hypnotics" (PDF). Psychopharmacol Bull. 37 (1): 10–29. doi:10.1007/BF01990373. PMID 14561946. Archived from the original (PDF) on 2007-07-09.
- ^ "Welkom op de GIPdatabank". GIPdatabank.nl (in Dutch). 2013-11-15. Retrieved 2014-01-31.
- ^ "Archived copy" (PDF). Archived from the original (PDF) on June 11, 2014. Retrieved March 8, 2014.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help)CS1 maint: archived copy as title (link) - ^ a b Brett, J; Murnion, B (2015). "Management of benzodiazepine misuse and dependence". Australian Prescriber. 38 (5): 152–155. doi:10.18773/austprescr.2015.055. PMC 4657308. PMID 26648651.
- ^ Griffiths RR, Johnson MW; Johnson (2005). "Relative abuse liability of hypnotic drugs: a conceptual framework and algorithm for differentiating among compounds". J Clin Psychiatry. 66 Suppl 9: 31–41. PMID 16336040.
- ^ Barrero-Hernández FJ, Ruiz-Veguilla M, López-López MI, Casado-Torres A (2002). "[Epileptic seizures as a sign of abstinence from chronic consumption of zolpidem]" [Epileptic seizures as a sign of abstinence from chronic consumption of zolpidem]. Rev Neurol (in Spanish). 34 (3): 253–6. PMID 12022074.
- ^ Gunja N (2013). "In the Zzz Zone: The Effects of Z-Drugs on Human Performance and Driving". Journal of Medical Toxicology. 9 (2): 163–171. doi:10.1007/s13181-013-0294-y. PMC 3657033. PMID 23456542.
- ^ Jones AW, Holmgren A, Kugelberg FC (2007). "Concentrations of scheduled prescription drugs in blood of impaired drivers: considerations for interpreting the results". Therapeutic drug monitoring. 29 (2): 248–60. doi:10.1097/FTD.0b013e31803d3c04. PMID 17417081.
- ^ "Kennedy To Enter Drug Rehab After Car Crash; Congressman Wrecked Car Near Capitol".[dead link]
- ^ Mulvihill K. "Ambien Abuse on Rise Among Teens". KSL. Archived from the original on 2009-02-20. Retrieved 2009-06-22.
- ^ "Swimming Australia's 'Stilnox six' given final warning as AOC decides not to issue any further sanctions". www.abc.net.au. Retrieved 2016-08-03.
- ^ US 4382938, Kaplan J-P, George P, "Imidazo[1,2-a] pyridine derivatives and their application as pharmaceuticals", published 1983-05-10, issued 1984-07-17, assigned to Synthelabo
- ^ a b c d e Brent Schrotenboer (2014-03-26). "Darren Sharper case spotlights sleep drug's dark side". USA Today.
- ^ a b Christian Red (2014-02-17). "In the rape case against Darren Sharper, former LAPD detective says Ambien is used often and can be similar to GHB". New York Daily News.
- ^ Naren Gunja (June 2013). "The Clinical and Forensic Toxicology of Z-drugs". J Med Toxicol. 9 (2): 155–162. doi:10.1007/s13181-013-0292-0. PMC 3657020. PMID 23404347.
- ^ "Stilnox blamed for Harbour Bridge death". nineMSN News. February 23, 2007. Archived from the original on 2007-06-15.
- ^ de Boissezon, X; Peran, P; de Boysson, C; Démonet, JF (July 2007). "Pharmacotherapy of aphasia: myth or reality?". Brain and Language. 102 (1): 114–25. doi:10.1016/j.bandl.2006.07.004. PMID 16982084.
- ^ Georgiopoulos, M; Katsakiori, P; Kefalopoulou, Z; Ellul, J; Chroni, E; Constantoyannis, C (2010). "Vegetative state and minimally conscious state: a review of the therapeutic interventions". Stereotactic and Functional Neurosurgery. 88 (4): 199–207. doi:10.1159/000314354. PMID 20460949.
- ^ Bomalaski, Martin N.; Claflin, Edward S.; Townsend, Whitney; Peterson, Mark D. (2017). "Zolpidem for the Treatment of Neurologic Disorders: A Systematic Review". JAMA Neurology. 74 (9): 1130–1139. doi:10.1001/jamaneurol.2017.1133. PMID 28655027.
Further reading
- Joel Lamoure RPh. BScPhm., FASCP. "How Is Zolpidem Dependence Managed?". Medscape Pharmacists Ask the Expert. WebMD. Archived from the original on 2012-12-13. Retrieved 2010-03-05.
{{cite web}}: Italic or bold markup not allowed in:|publisher=(help); Unknown parameter|dead-url=ignored (|url-status=suggested) (help); Unknown parameter|registration=ignored (|url-access=suggested) (help) - "Prescription Sleep Aid AMBIEN CR". Sanofi-Aventis. Ambien CR official website. April 2013. Retrieved 2009-05-21.
- "Ambien Cr (zolpidem tartrate) Tablet, Coated". DailyMed. U.S. National Library of Medicine, National Institutes of Health, Health & Human Services. Archived from the original on June 9, 2009. Retrieved 2009-05-21.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - U.S. National Library of Medicine: Drug Information Portal – Zolpidem
External links
![]() Media related to Zolpidem at Wikimedia Commons
Media related to Zolpidem at Wikimedia Commons
