Hydrocodone
This article needs more reliable medical references for verification or relies too heavily on primary sources. (April 2013) |  |
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Zohydro ER, Vicodin, Norco |
| Other names | dihydrocodeinone |
| AHFS/Drugs.com | Micromedex Detailed Consumer Information |
| MedlinePlus | a601006 |
| Dependence liability | severe / high |
| Routes of administration | oral, intranasal, rectal |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | High |
| Metabolism | Hepatic: CYP2D6 (minor; converts to hydromorphone), CYP3A4 (major; converts to norhydrocodone) |
| Elimination half-life | 3.8–6 hours |
| Excretion | Renal |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.004.304 |
| Chemical and physical data | |
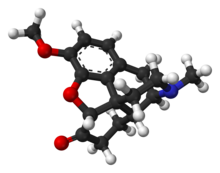
| Formula | C18H21NO3 |
| Molar mass | 299.368 g/mol g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| (verify) | |
Hydrocodone is a semi-synthetic opioid synthesized from codeine, one of the opioid alkaloids found in the opium poppy. It is a narcotic analgesic used orally for relief of moderate to severe pain, but also commonly taken in liquid form as an antitussive/cough suppressant.[1]
Hydrocodone is prescribed predominantly within the United States, with the International Narcotics Control Board reporting that 99% of the worldwide supply in 2007 was consumed in the United States.[2]
Medical uses
Hydrocodone is used to treat moderate to severe pain and as an antitussive to treat cough.[1] In one study comparing the potency of hydrocodone to that of oxycodone, it was found that it took 50% more hydrocodone to achieve the same degree of miosis (pupillary contraction).[3] The investigators interpreted this to mean that oxycodone is about 50% more potent than hydrocodone. However, in a study of emergency room patients with fractures, it was found that an equal amount of either drug provided about the same degree of pain relief, indicating that there is little practical difference between them when used for that purpose.[4] Some references state that the analgesic action of hydrocodone begins in 20–30 minutes and lasts about 4–8 hours.[5] The manufacturer's information says onset of action is about 10–30 minutes and duration is about 4–6 hours.[6] Recommended dosing interval is 4–6 hours.
Adverse effects
Common side effects of hydrocodone are nausea, vomiting, constipation, drowsiness, dizziness, lightheadedness, anxiety, abnormally happy or sad mood, dry throat, difficulty urinating, rash, itching, and narrowing of the pupils. Serious side effects include slowed or irregular breathing and chest tightness.[7]
Several cases of progressive bilateral hearing loss unresponsive to steroid therapy have been described as an infrequent adverse reaction to hydrocodone/paracetamol misuse. This adverse effect has been considered by some to be due to the ototoxicity of hydrocodone.[8][9] Other researchers have suggested that paracetamol is the primary agent responsible for the ototoxicity.[10][11]
Hydrocodone is in U.S. Food and Drug Administration (FDA) pregnancy category C. No adequate and well-controlled studies in humans have been conducted. A newborn of a mother taking opioid medications regularly prior to the birth will be physically dependent. The baby may also exhibit respiratory depression if the opioid dose was high.[12] An epidemiological study indicated that opioid treatment during early pregnancy results in increased risk of various birth defects.[13]
Symptoms of hydrocodone overdose include narrowed or widened pupils; slow, shallow, or stopped breathing; slowed or stopped heartbeat; cold, clammy, or blue skin; excessive sleepiness; loss of consciousness; seizures; or death.[7]
Hydrocodone can be habit-forming, causing physical and psychological dependence. Its abuse liability is similar to morphine and less than oxycodone.[14]
Contraindications and interactions
Patients consuming alcohol, other opioids, antihistamines, anti-psychotics, anti-anxiety agents, or other central nervous system (CNS) depressants together with hydrocodone may exhibit an additive CNS depression.[12] Hydrocodone may interact with serotonergic medications.[15]
Pharmacology
As a narcotic, hydrocodone relieves pain by binding to opioid receptors in the CNS. It acts primarily on μ-opioid receptors, with about six times lesser affinity to δ-opioid receptors. In blood, 20–50% of hydrocodone is bound to protein.[5][16]
Studies have shown hydrocodone is stronger than codeine but only one-tenth as potent as morphine at binding to receptors and reported to be only 59% as potent as morphine in analgesic properties. However, in tests conducted on rhesus monkeys, the analgesic potency of hydrocodone was actually higher than morphine.[17] Oral hydrocodone has a mean equivalent daily dosage (MEDD) factor of 0.4, meaning that 1 mg of hydrocodone is equivalent to 0.4 mg of intravenous morphine. However, because of morphine's low oral bioavailability, there is a 1:1 correspondence between orally administered morphine and orally administered hydrocodone.[18] The relative milligram strength of hydrocodone to codeine is given as 6 fold, that is 5 mg has the effect of 30 mg of codeine; by way of the Roman numeral VI this is said to have given rise to the trade name Vicodin.[citation needed]
Pharmacokinetics
In the liver, hydrocodone is transformed into several metabolites. It has a serum half-life that averages 3.8 hours.[17] The hepatic cytochrome P450 enzyme CYP2D6 converts it into hydromorphone, a more potent opioid. However, extensive and poor cytochrome 450 CYP2D6 metabolizers had similar physiological and subjective responses to hydrocodone, and CYP2D6 inhibitor quinidine did not change the responses of extensive metabolizers, suggesting that inhibition of CYP2D6 metabolism of hydrocodone has no practical importance.[19][20] Ultra-rapid CYP2D6 metabolizers (1-2% of the population) may have an increased response to hydrocodone; however, hydrocodone metabolism in this population has not been studied.[21]
A major metabolite, norhydrocodone, is predominantly formed by CYP3A4-catalyzed oxidation. Inhibition of CYP3A4 in a child who was, in addition, a poor CYP2D6 metabolizer, resulted in a fatal overdose of hydrocodone.[22] Approximately 40% of hydrocodone metabolism is attributed to non-cytochrome-catalyzed reactions.[23]
Formulations
Combination products

Most hydrocodone is formulated in combination with a second analgesic, such as paracetamol (acetaminophen) or ibuprofen. Examples of hydrocodone combinations include Norco, Vicodin, Lortab and Vicoprofen.
Zohydro ER
| What is this drug for? | |
|---|---|
| treatment of severe, chronic pain that requires around-the-clock opioid treatment[24] | |
| Who might consider taking it? | |
| Adults who need opioid treatment but who find alternative treatments to be inadequate[24] | |
| Who should not take it? | |
| |
| What other choices are there? | |
|

In 2014, the FDA approved prescription-only marketing by Zogenix Pharmaceuticals of the first pure hydrocodone product in the U.S, known by the brand name Zohydro ER.[25] The drug comes in extended-release capsules with hydrocodone powder inside, in doses of 10 mg, 15 mg, 20 mg, 30 mg, 40 mg and 50 mg. This is up to 5 times as much active opioid as the highest strength hydrocodone/APAP product (10 mg/325 mg), but it is important to note that the hydrocodone in Zohydro formulations is intended to be slowly released over 12 hours. Zohydro ER (hydrocodone bitartrate) is indicated for the management of pain severe enough to require daily, around-the-clock, long-term opioid treatment for which alternative treatment options are inadequate. Zohydro is a schedule II controlled substance under the CSA.[26]
The approval of Zohydro ER was controversial, due to concerns over its potential for substance abuse. The FDA approved Zohydro ER over the objections of its own review panel, which voted 12 to 2 against approval. The panel stated that if approved, Zohydro ER would likely "be abused, possibly at a rate greater than that of currently available hydrocodone combination products". Thirty U.S. states asked the FDA not to approve Zohydro ER in capsule form due to its potency and the ease with which it could be abused, by being crushed and then snorted or injected.[27] Zohydro ER was briefly prohibited in Massachusetts before a federal judge ruled that the state's ban was preempted by the earlier federal approval.[28][29]
Detection in body fluids
Hydrocodone concentrations are measured in blood, plasma, and urine to seek evidence of misuse, to confirm diagnoses of poisoning, and to assist in investigations into deaths. Many commercial opiate screening tests react indiscriminately with hydrocodone, other opiates, and their metabolites, but chromatographic techniques can easily distinguish hydrocodone uniquely. Blood and plasma hydrocodone concentrations typically fall into the 5–30 µg/L range among people taking the drug therapeutically, 100–200 µg/L among recreational users, and 100–1,600 µg/L in cases of acute, fatal overdosage. Co-administration of the drug with food or alcohol can very significantly increase the resulting plasma hydrocodone concentrations that are subsequently achieved.[30][31]
Regulation
This section needs additional citations for verification. (April 2013) |
Australia
In Australia, hydrocodone is a Schedule 8 (S8) or Controlled Drug.
Austria
Hydrocodone is regulated in Austria in the same fashion as in Germany (see below) under the Austrian Suchtmittelgesetz; since 2002, it has been available in the form of German products and those produced elsewhere in the European Union under Article 76 of the Schengen Treaty—prior to this, no Austrian companies produced hydrocodone products, with dihydrocodeine, nicomorphine, and nicocodeine being more commonly used for the same levels of pain and the former and last for coughing. The latter two were Austrian inventions of the first years of the 20th Century.
Nicocodeine, the nicotinoyl ester of codeine, is virtually identical in strength to hydrocodone. A third, nicodicodeine, the dihydrocodeine analogue of nicocodeine, and acetyldihydrocodeine and thebacon, acetyl esters of dihydrocodeine and hydrocodone respectively, were also used. Nicocodeine is known as Tusscodin, and abroad as Lyopect.[clarification needed] Nicocodeine is a prodrug for nicomorphine in the same way hydrocodone is for hydromorphone; nicomorphine is a strong opioid of the 3,6 diester (heroin-nicomorphine-dibenzoylmorphine) type, which is also stronger than morphine, not quite the milligram strength of hydromorphone, but with a faster onset of action.
Belgium
In Belgium, hydrocodone is no longer available for medical use.
Canada
In Canada, hydrocodone is a Schedule I controlled substance and is available by prescription only. Hydrocodone is prescribed alone as well as in proprietary combinations, typically with an NSAID or paracetamol.
France
In France, hydrocodone is no longer available for medical use. Hydrocodone is a prohibited narcotic.
Germany
In Germany, hydrocodone is no longer available for medical use. Hydrocodone is listed under the Betäubungsmittelgesetz as a Suchtgift in the same category as morphine.
Luxembourg
In Luxembourg, hydrocodone is available by prescription under the name Biocodone. Prescriptions are more commonly given for use as a cough suppressant (antitussive) rather than for pain relief (analgesic).
The Netherlands
In the Netherlands, hydrocodone is not available for medical use and is classified as a List 1 drug under the Opium Law.
Sweden
Hydrocodone is no longer available for medical use in Sweden. The last remaining formula was deregistered in 1967.
United Kingdom
In the United Kingdom, hydrocodone is not available for medical use and is listed as a Class A drug under the Misuse of Drugs Act 1971. Various formulations of dihydrocodeine, a weaker opioid, are frequently used as an alternative for the aforementioned indications of hydrocodone use.
United States
Hydrocodone was usually not commercially available in pure form in the United States due to a separate regulation, and was typically sold with an NSAID, paracetamol (acetaminophen), antihistamine, expectorant, antibiotic or homatropine. In solid pill form, Zohydro ER contains only hydrocodone as its active ingredient in an extended release format. As of 6 October 2014 all hydrocodone products are listed as Schedule II Controlled substance. They will no longer be a Schedule III narcotic. Prescriptions can no longer have refills and a handwritten paper script must be obtained for each fill. In some states a Schedule II substance can be electronically prescribed if the doctor has the proper technology and an electronic signature license.
Prior to 6 October 2014, hydrocodone was listed as both a Schedule II and Schedule III substance, depending on the amount of hydrocodone and type and amount of additional ingredient it was compounded with:
- Schedule II lists hydrocodone in pure form and any formulations of combination products containing more than 15 mg hydrocodone per dosage unit. This shares the ACSCN of bulk hydrocodone (9193)
- Schedule III also lists hydrocodone in combinations products containing "Not more than 300 milligrams of dihydrocodeinone (hydrocodone) per 100 milliliters or not more than 15 milligrams per dosage unit, with a fourfold or greater quantity of an isoquinoline alkaloid of opium" as ACSCN 9805.
- Schedule III also lists hydrocodone in combinations products containing "Not more than 300 milligrams of dihydrocodeinone (hydrocodone) per 100 milliliters or not more than 15 milligrams per dosage unit, with one or more active nonnarcotic ingredients in recognized therapeutic amounts" as ACSCN 9806 (e.g. Norco, Vicodin, Lortab)
Prior to August 1990, formulations with at least three active ingredients which were less than one-ten thousandth hydrocodone base by weight were Schedule V, meaning a handful of hydrocodone syrups including a phenyltoloxamine-based, decongestant-containing version of Tussionex were available OTC (for those willing to sign a Narcotic Exempt Register) in about a dozen states.
As of 2006, hydrocodone was the active antitussive in more than 200 formulations of cough syrups and tablets sold in the United States. In late 2006, the U.S. Food and Drug Administration (FDA) began forcing the recall of many of these formulations due to reports of deaths in infants and children under the age of six. The legal status of drug formulations originally sold between 1938 and 1962—before FDA approval was required—was ambiguous. As a result of FDA enforcement action, by August 2010, 88% of the hydrocodone-containing medications had been removed from the market.[32][failed verification] As a result, doctors, pharmacists, and codeine-sensitive or allergic patients or sensitive to the amounts of histamine released by its metabolites had to choose among rapidly dwindling supplies of the Hycodan-Codiclear-Hydromet type syrups, Tussionex—an extended-release suspension similar to the European products Codipertussin (codeine hydrochloride), Paracodin suspension (dihydrocodeine hydroiodide), Tusscodin (nicocodeine hydrochloride) and others—and a handful of weak dihydrocodeine syrups. The low sales volume and Schedule II status of dilaudid cough syrup predictably leads to under-utilisation of the drug. There are several conflicting views concerning the US availability of cough preparations containing ethylmorphine (also called dionine or codethyline)—Feco Syrup and its equivalents were first marketed circa 1895 and still in common use in the 1940s and 1950s, and the main ingredient is treated like codeine under the Controlled Substances Act of 1970.[citation needed]
As of July 2010, the FDA was considering banning some hydrocodone and oxycodone fixed-combination proprietary prescription drugs—based on the paracetamol content and the widespread occurrence of liver damage. FDA action on this suggestion would ostensibly also affect codeine and dihydrocodeine products such as the Tylenol With Codeine and Panlor series of drugs.[citation needed] In 2010, it was the most prescribed drug in the USA, with 131.2 million prescriptions of hydrocodone (combined with acetaminophen) being written.[33]
The rationale of combining hydrocodone with other pain-killers is that the combination may increase efficacy, and the adverse effects may be reduced as compared with an equally effective dose of a single agent.[34][35] A combination of hydrocodone and ibuprofen was more effective than either of the drugs on their own in relieving postoperative pain. The overall effect of the combination could be presented as a sum of the effects of ibuprofen and hydrocodone, which is consistent with differing mechanisms of action of these drugs.[36][37][38] Similar results were observed for hydrocodone-acetaminophen combination.[34]
Four pharmaceutical companies (Purdue Pharma, Cephalon, Egalet and Zogenix) are developing extended-release formulations of hydrocodone by itself; the Zogenix product was approved by the US FDA on 25 October 2013 and was launched in the 1st Quarter of the Market[clarification needed] in 2014. These formulations were designed to avoid the issue of hepatotoxicity precipitated by acetaminophen. These new extended-release preparations also offer lower abuse potential.[39]
On 25 October 2013, with support from critics of hydrocodone use and the DEA, the U.S. Food & Drug Administration proposed tightening control of the drug by reclassifying the existing Schedule III formulations of hydrocodone as Schedule II.[40] Critics of the change included pharmaceutical firms, medical professionals, and patients, particularly those undergoing pain management, who stressed that reclassification is unnecessary and would be counter-productive to effectively provide pain relief for those suffering. One issue regarding Class II drugs as compared to Class III drugs is that doctors cannot "call in" Class II medications to a pharmacy over the phone or fax: the prescription must be hand written and taken to the pharmacy by the patient. Another issue with Class II drugs is that the doctor can only prescribe a one-month supply at a time, which means the prescription cannot have any refills. Those opposed to reclassification also maintain that the existing protocol for prescribing opioids and the existing inclusion of acetaminophen along with other NSAIDs are effective measures in deterring misuse.
Effective 6 October 2014, 21 CFR 1308.13 was amended (at 79 FR 49661) to remove ACSCNs 9805 and 9806 from Schedule III, the result being that all hydrocodone-containing preparations are now Schedule II, regardless of amount of hydrocodone or additional components.
History
Hydrocodone was first synthesized in Germany in 1920 by Carl Mannich and Helene Löwenheim.[41] It was approved by the Food and Drug Administration on 23 March 1943 for sale in the United States and approved by Health Canada for sale in Canada under the brand name Hycodan.[42][43]
Hydrocodone was first marketed by Knoll as Dicodid, starting in February 1924 in Germany. This name is analogous to other products the company introduced or otherwise marketed: Dilaudid (hydromorphone, 1926), Dinarkon (oxycodone, 1917), Dihydrin (dihydrocodeine, 1911), and Dimorphan (dihydromorphine). Paramorfan is the trade name of dihydromorphine from another manufacturer, as is Paracodin, for dihydrocodeine.
The name Dicodid was registered in the United States and appears without a monograph as late as 1978 in the Physicians' Desk Reference; Dicodid may have been marketed to one extent or another in North America in the 1920s and early 1930s. The drug was pure hydrocodone in small 5 and 10 mg tablets, physically similar to the Dilaudid tablets. It is no longer manufactured by Knoll in Germany, nor is a generic available. Hydrocodone was never as common in Europe as it is in North America—dihydrocodeine is used for its spectrum of indications. Germany was the number two consumer of hydrocodone until the manufacture of the drug was discontinued there. Now, the world outside the United States accounts for less than 1% of annual consumption. It was listed as a Suchtgift under the German Betäubungsmittelgesetz and regulated like morphine. It became available in the Schengen Area of the European Union as of 1 January 2002 under Title 76 of the Schengen Treaty.
See also
- Conorfone (structural analogue)
- Equianalgesic (opioid comparison chart)
References
- ^ a b Karch, Steven B. (2008). Pharmacokinetics and pharmacodynamics of abused drugs. Boca Raton: CRC Press. pp. 55–56. ISBN 1-4200-5458-9.
- ^ International Narcotics Control Board Report 2008. United Nations Pubns. 2009. p. 20. ISBN 9211482321.
- ^ Zacny, J. P.; Gutierrez, S. (2009). "Within-subject comparison of the psychopharmacological profiles of oral hydrocodone and oxycodone combination products in non-drug-abusing volunteers". Drug and Alcohol Dependence. 101 (1–2): 107–114. doi:10.1016/j.drugalcdep.2008.11.013. PMID 19118954.
- ^ Marco, C. A.; Plewa, M. C.; Buderer, N; Black, C; Roberts, A (2005). "Comparison of oxycodone and hydrocodone for the treatment of acute pain associated with fractures: A double-blind, randomized, controlled trial". Academic Emergency Medicine. 12 (4): 282–8. doi:10.1197/j.aem.2004.12.005. PMID 15805317.
- ^ a b Vallejo, R.; Barkin, R. L.; Wang, V. C. (2011). "Pharmacology of opioids in the treatment of chronic pain syndromes". Pain physician. 14 (4): E343–E360. PMID 21785485.
- ^ "Opioid (Narcotic Analgesics and Acetaminophen Systemic )". Retrieved 22 March 2014.
- ^ a b MedlinePlus; Drug Information: Hydrocodone. Last Revised—1 October 2008. Retrieved on 20 April 2013.
- ^ Friedman RA, House JW, Luxford WM, Gherini S, Mills D; House; Luxford; Gherini; Mills (March 2000). "Profound hearing loss associated with hydrocodone/acetaminophen abuse". Am J Otol. 21 (2): 188–91. doi:10.1016/S0196-0709(00)80007-1. PMID 10733182.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Ho T, Vrabec JT, Burton AW; Vrabec; Burton (May 2007). "Hydrocodone use and sensorineural hearing loss". Pain Physician. 10 (3): 467–72. PMID 17525781.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Yorgason, J. G.; Kalinec, G. M.; Luxford, W. M.; Warren, F. M.; Kalinec, F. (2010). "Acetaminophen ototoxicity after acetaminophen/hydrocodone abuse: Evidence from two parallel in vitro mouse models". Otolaryngology - Head and Neck Surgery. 142 (6): 814–819, 819.819–2. doi:10.1016/j.otohns.2010.01.010. PMID 20493351.
- ^ Curhan, S. G.; Eavey, R.; Shargorodsky, J.; Curhan, G. C. (2010). "Analgesic Use and the Risk of Hearing Loss in Men". The American Journal of Medicine. 123 (3): 231–237. doi:10.1016/j.amjmed.2009.08.006. PMC 2831770. PMID 20193831.
- ^ a b "REPREXAIN (hydrocodone bitartrate, ibuprofen) tablet, film coated". http://dailymed.nlm.nih.gov. NIH. Retrieved 27 April 2013.
{{cite web}}: External link in|work= - ^ Broussard, C. S.; Rasmussen, S. A.; Reefhuis, J.; Friedman, J. M.; Jann, M. W.; Riehle-Colarusso, T.; Honein, M. A.; National Birth Defects Prevention Study (2011). "Maternal treatment with opioid analgesics and risk for birth defects". American Journal of Obstetrics and Gynecology. 204 (4): 314.3e1–11. doi:10.1016/j.ajog.2010.12.039. PMID 21345403.
- ^ Wightman, R.; Perrone, J.; Portelli, I.; Nelson, L. (2012). "Likeability and Abuse Liability of Commonly Prescribed Opioids". Journal of Medical Toxicology. 8 (4): 335–340. doi:10.1007/s13181-012-0263-x. PMID 22992943.
- ^ Gnanadesigan N, Espinoza RT, Smith RL; Espinoza; Smith (June 2005). "The serotonin syndrome". N Engl J Med. 352 (23): 2454–6, author reply 2454–6. doi:10.1056/NEJM200506093522320. PMID 15948273.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Thompson, C. M.; Wojno, H.; Greiner, E.; May, E. L.; Rice, K. C.; Selley, D. E. (2003). "Activation of G-Proteins by Morphine and Codeine Congeners: Insights to the Relevance of O- and N-Demethylated Metabolites at - and -Opioid Receptors". Journal of Pharmacology and Experimental Therapeutics. 308 (2): 547–554. doi:10.1124/jpet.103.058602. PMID 14600248.
- ^ a b Davis, Mellar P. (2005). "Hydrocodone". Opioids for cancer pain. Oxford UK: Oxford University Press. pp. 59–68. ISBN 0-19-852943-0.
- ^ "Instructions for Mean Equivalent Daily Dose (MEDD)" (PDF). Retrieved 22 August 2010.
- ^ Kaplan, H. L.; Busto, U. E.; Baylon, G. J.; Cheung, S. W.; Otton, S. V.; Somer, G.; Sellers, E. M. (1997). "Inhibition of cytochrome P450 2D6 metabolism of hydrocodone to hydromorphone does not importantly affect abuse liability". The Journal of Pharmacology and Experimental Therapeutics. 281 (1): 103–108. PMID 9103485.
- ^ Gardiner, S. J.; Begg, E. J. (2006). "Pharmacogenetics, Drug-Metabolizing Enzymes, and Clinical Practice". Pharmacological Reviews. 58 (3): 521–590. doi:10.1124/pr.58.3.6. PMID 16968950.
- ^ Crews, K. R.; Gaedigk, A.; Dunnenberger, H. M.; Klein, T. E.; Shen, D. D.; Callaghan, J. T.; Kharasch, E. D.; Skaar, T. C.; Clinical Pharmacogenetics Implementation Consortium (2011). "Clinical Pharmacogenetics Implementation Consortium (CPIC) Guidelines for Codeine Therapy in the Context of Cytochrome P450 2D6 (CYP2D6) Genotype". Clinical Pharmacology & Therapeutics. 91 (2): 321–326. doi:10.1038/clpt.2011.287. PMC 3289963. PMID 22205192.
- ^ Madadi, P; Hildebrandt, D; Gong, I. Y.; Schwarz, U. I.; Ciszkowski, C; Ross, C. J.; Sistonen, J; Carleton, B. C.; Hayden, M. R.; Lauwers, A. E.; Koren, G (2010). "Fatal hydrocodone overdose in a child: Pharmacogenetics and drug interactions". Pediatrics. 126 (4): e986-9. doi:10.1542/peds.2009-1907. PMID 20837591.
- ^ Landau, R.; Stamer, U. M.; Landau, R. (2012). "Pharmacogenomic considerations in opioid analgesia". Pharmacogenomics and Personalized Medicine. 5: 73–87. doi:10.2147/PGPM.S23422. PMC 3513230. PMID 23226064.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ a b c d e f g h i Informulary (February 2015). "Drug Facts Box: ZOHYDRO ER (hydrocodone bitartrate)" (PDF). Consumer Reports. Consumer Reports. Retrieved 5 November 2015.
- ^ "Zohydro ER Product Monograph" (PDF). http://www.zogenix.com/pdf/ZOHYDRO%20ER%20Full%20Prescribing%20Information.pdf. Zogenix. Retrieved 1 July 2014.
{{cite web}}: External link in|website= - ^ http://www.zogenix.com/content/products/zohydro.htm
- ^ Rubin, Rita (27 February 2014). "Critics Oppose FDA Approval of Painkiller Zohydro". WebMD. Retrieved 14 May 2014.
- ^ Heger, Monica (7 May 2014). "State challenges to painkiller could threaten FDA authority". Nature Medicine. Retrieved 14 May 2014.
- ^ Valencia, Milton (23 April 2014). "Mass. limits use of the potent painkiller Zohydro". Boston Globe. Retrieved 14 May 2014.
- ^ Spiller HA. Postmortem oxycodone and hydrocodone blood concentrations. J. Forensic Sci. 48: 429–431, 2003.
- ^ R. Baselt, Disposition of Toxic Drugs and Chemicals in Man, 10th edition, Biomedical Publications, Seal Beach, CA, 2014, pp. 1011–1013.
- ^ "Medical News: FDA Pulls Plug on 200-Plus Unapproved Cough Syrups With Hydrocodone—in Product Alert, Prescriptions from". MedPage Today. Retrieved 22 August 2010.
- ^ DeNoon, Daniel J. (20 April 2011). "The 10 Most Prescribed Drugs". eMedicineHealth. Retrieved 16 August 2012.
- ^ a b Beaver, W. T.; McMillan, D. (1980). "Methodological considerations in the evaluation of analgesic combinations: Acetaminophen (paracetamol) and hydrocodone in postpartum pain". British Journal of Clinical Pharmacology. 10 Suppl 2 (Suppl 2): 215S–223S. doi:10.1111/j.1365-2125.1980.tb01803.x. PMC 1430165. PMID 7192153.
- ^ Raffa, R. B. (2001). "Pharmacology of oral combination analgesics: Rational therapy for pain". Journal of clinical pharmacy and therapeutics. 26 (4): 257–264. doi:10.1046/j.1365-2710.2001.00355.x. PMID 11493367.
- ^ Wideman, G.; Keffer, M.; Morris, E.; Doylejr, R.; Jiang, J.; Beaver, W. (1999). "Analgesic efficacy of a combination of hydrocodone with ibuprofen in postoperative pain". Clinical Pharmacology & Therapeutics. 65 (1): 66–76. doi:10.1016/S0009-9236(99)70123-2. PMID 9951432.
- ^ Sunshine, A.; Olson, N. Z.; O'Neill, E.; Ramos, I.; Doyle, R. (1997). "Analgesic efficacy of a hydrocodone with ibuprofen combination compared with ibuprofen alone for the treatment of acute postoperative pain". Journal of clinical pharmacology. 37 (10): 908–915. doi:10.1002/j.1552-4604.1997.tb04265.x. PMID 9505982.
- ^ Betancourt, J. W.; Kupp, L. I.; Jasper, S. J.; Farooqi, O. A. (2004). "Efficacy of Ibuprofen-Hydrocodone for the Treatment of Postoperative Pain After Periodontal Surgery". Journal of Periodontology. 75 (6): 872–876. doi:10.1902/jop.2004.75.6.872. PMID 15295955.
- ^ Trescot, A.; Krashin, D.; Murinova, A. M. (2013). "Extended-release hydrocodone – gift or curse?". Journal of Pain Research. 6: 53–57. doi:10.2147/JPR.S33062. PMC 3555555. PMID 23358452.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ "F.D.A. Urging a Tighter Rein on Painkillers". The New York Times. 25 October 2013. Retrieved 26 October 2013.
- ^ Mannich, C.; Löwenheim, H. (1920). "Ueber zwei neue Reduktionsprodukte des Kodeins". Archiv der Pharmazie. 258 (2–4): 295–316. doi:10.1002/ardp.19202580218.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ "Drugs@FDA—Approval History: Hycodan". FDA. Retrieved 7 January 2006.
- ^ "FDA Docket No. 2007N-0353, Drug Products Containing Hydrocodone; Enforcement Action Dates". FDA. Retrieved 7 January 2006. See section I. B., DESI Review of Hydrocodone Products
External links
- U.S. National Library of Medicine: Drug Information Portal – Hydrocodone
- DEA Schedules of Controlled Substances: Rescheduling of Hydrocodone Combination Products From Schedule III to Schedule II, effective 6 Oct 2014
