Effects of cannabis
The effects of cannabis are caused by cannabinoids, most notably the chemical substance tetrahydrocannabinol (THC). Cannabis has both psychological and physiological effects on the human body. The drug is one of the most abused for its potency and relative accessibility from illegal sources. Five European countries, Canada, and nineteen US states[1] have legalized medical cannabis if prescribed for nausea, pain or the alleviation of symptoms surrounding chronic illness.[citation needed]
Acute effects while under the influence can include euphoria and anxiety.[2][3] Concerns have been raised about the potential for long-term cannabis consumption to increase risk for schizophrenia, bipolar disorders, and major depression,[4][5] but the ultimate conclusions on these factors are disputed.[6][7][8][9] The evidence of long-term effects on memory is preliminary and hindered by confounding factors.[10][11] For thousands of years people have said that cannabis has religious and spiritual effects.[12]
Biochemical effects




Cannabinoids and cannabinoid receptors
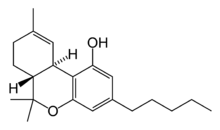
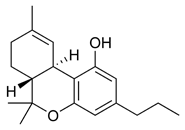
The most prevalent psychoactive substances in cannabis are cannabinoids, most notably THC. Some varieties, having undergone careful selection and growing techniques, can yield as much as 29% THC.[13] Another psychoactive cannabinoid present in Cannabis sativa is tetrahydrocannabivarin (THCV), but it is only found in small amounts and is a cannabinoid antagonist.[14]
In addition, there are also similar compounds contained in cannabis that do not exhibit any psychoactive response but are obligatory for functionality: cannabidiol (CBD), an isomer of THC; cannabinol (CBN), an oxidation product of THC; cannabivarin (CBV), an analog of CBN with a different sidechain, cannabidivarin (CBDV), an analog of CBD with a different side chain, and cannabinolic acid. How these other compounds interact with THC is not fully understood. Some clinical studies have proposed that CBD acts as a balancing force to regulate the strength of the psychoactive agent THC. CBD is also believed to regulate the body’s metabolism of THC by inactivating cytochrome P450, an important class of enzymes that metabolize drugs. Experiments in which mice were treated with CBD followed by THC showed that CBD treatment was associated with a substantial increase in brain concentrations of THC and its major metabolites, most likely because it decreased the rate of clearance of THC from the body.[15] Cannabis cofactor compounds have also been linked to lowering body temperature, modulating immune functioning, and cell protection. The essential oil of cannabis contains many fragrant terpenoids which may synergize with the cannabinoids to produce their unique effects. THC is converted rapidly to 11-hydroxy-THC, which is also pharmacologically active, so the drug effect outlasts measurable THC levels in blood.[13]
THC and cannabidiol are also neuroprotective antioxidants. Research in rats has indicated that THC prevented hydroperoxide-induced oxidative damage as well as or better than other antioxidants in a chemical (Fenton reaction) system and neuronal cultures. Cannabidiol was significantly more protective than either vitamin E or vitamin C.[16]
The cannabinoid receptor is a typical member of the largest known family of receptors called a G protein-coupled receptor. A signature of this type of receptor is the distinct pattern of how the receptor molecule spans the cell membrane seven times. The location of cannabinoid receptors exists on the cell membrane, and both outside (extracellularly) and inside (intracellularly) the cell membrane. CB1 receptors, the bigger of the two, are extraordinarily abundant in the brain: 10 times more plentiful than μ-opioid receptors, the receptors responsible for the effects of morphine. CB2 receptors are structurally different (the sequence similarity between the two subtypes of receptors is 44%), found only on cells of the immune system, and seems to function similarly to its CB1 counterpart. CB2 receptors are most commonly prevalent on B-cells, natural killer cells, and monocytes, but can also be found on polymorphonuclear neutrophil cells, T8 cells, and T4 cells. In the tonsils the CB2 receptors appear to be restricted to B-lymphocyte-enriched areas.
THC and endogenous anandamide additionally interact with glycine receptors.
Biochemical mechanisms in the brain
In 1990 the discovery of cannabinoid receptors located throughout the brain and body, along with endogenous cannabinoid neurotransmitters like anandamide (a lipid material derived ligand from arachidonic acid), suggested that the use of cannabis affects the brain in the same manner as a naturally occurring brain chemical.[citation needed] Cannabinoids usually contain a 1,1'-di-methyl-pyrane ring, a variedly derivatized aromatic ring and a variedly unsaturated cyclohexyl ring and their immediate chemical precursors, constituting a family of about 60 bi-cyclic and tri-cyclic compounds. Like most other neurological processes, the effects of cannabis on the brain follow the standard protocol of signal transduction, the electrochemical system of sending signals through neurons for a biological response. It is now understood that cannabinoid receptors appear in similar forms in most vertebrates and invertebrates and have a long evolutionary history of 500 million years. The binding of cannabinoids to cannabinoid receptors decrease adenylyl cyclase activity, inhibit calcium N channels, and disinhibit K+A channels. There are two types of cannabinoid receptors (CB1 and CB2).[citation needed]
The CB1 receptor is found primarily in the brain and mediates the psychological effects of THC. The CB2 receptor is most abundantly found on cells of the immune system. Cannabinoids act as immunomodulators at CB2 receptors, meaning they increase some immune responses and decrease others. For example, nonpsychotropic cannabinoids can be used as a very effective anti-inflammatory.[15] The affinity of cannabinoids to bind to either receptor is about the same, with only a slight increase observed with the plant-derived compound CBD binding to CB2 receptors more frequently. Cannabinoids likely have a role in the brain’s control of movement and memory, as well as natural pain modulation. It is clear that cannabinoids can affect pain transmission and, specifically, that cannabinoids interact with the brain's endogenous opioid system and may affect dopamine transmission.[17] This is an important physiological pathway for the medical treatment of pain.
Sustainability in the body
Most cannabinoids are lipophilic (fat soluble) compounds that are easily stored in fat, thus yielding a long elimination half-life relative to other recreational drugs. The THC molecule, and related compounds, are usually detectable in drug tests from 3 days up to 10 days according to Redwood Laboratories; heavy users can produce positive tests for up to 3 months after ceasing cannabis use (see drug test).[citation needed]
Toxicity
Cannabis smoke contains many toxic chemicals however THC, the principal psychoactive constituent of the cannabis plant, has an extremely low toxicity and the amount that can enter the body through the consumption of cannabis plants poses no threat of death. In lab animal tests, scientists have had much difficulty administering a dosage of THC that is high enough to be lethal. Accordingly, there is little reason to believe a human would self-administer such doses. According to the Merck Index,[18] the LD50 of THC (the dose which causes the death of 50% of individuals) is 1270 mg/kg for male rats and 730 mg/kg for female rats from oral consumption in sesame oil, and 42 mg/kg for rats from inhalation.[19]
The ratio of cannabis material required to produce a fatal overdose to the amount required to saturate cannabinoid receptors and cause intoxication is approximately 40,000:1.[20][21] A typical marijuana "joint" contains less than 10 mg of THC, and one would have to smoke thousands of those in a short period of time to approach toxic levels. According to a 2006 United Kingdom government report, using cannabis is much less dangerous than tobacco, prescription drugs, and alcohol in social harms, physical harm, and addiction.[22] It was found in 2007 that while tobacco and cannabis smoke are quite similar, cannabis smoke contained higher amounts of ammonia, hydrogen cyanide, and nitrogen oxides, but lower levels of carcinogenic polycyclic aromatic hydrocarbons (PAHs).[23] This study found that directly inhaled cannabis smoke contained as much as 20 times as much ammonia and 5 times as much hydrogen cyanide as tobacco smoke and compared the properties of both mainstream and sidestream (smoke emitted from a smouldering 'joint' or 'cone') smoke.[23] Mainstream cannabis smoke was found to contain higher concentrations of selected polycyclic aromatic hydrocarbons (PAHs) than sidestream tobacco smoke.[23] However, other studies have found much lower disparities in ammonia and hydrogen cyanide between cannabis and tobacco, and that some other constituents (such as polonium-210, lead, arsenic, nicotine, and tobacco-specific nitrosamines) are either lower or non-existent in cannabis smoke.[24][25]
Cannabis smoke contains thousands of organic and inorganic chemical compounds. This tar is chemically similar to that found in tobacco smoke or cigars.[26] Over fifty known carcinogens have been identified in cannabis smoke.[27] These include nitrosamines, reactive aldehydes, and polycylic hydrocarbons, induding benz[a]pyrene.[28] Marijuana smoke was listed as a cancer agent in California in 2009.[29] A study by the British Lung Foundation published in 2012 identifies cannabis smoke as a carcinogen and also finds awareness of the danger is low compared with the high awareness of the dangers of smoking tobacco particularly among younger users. Other observations include possible increased risk from each cigarette; lack of research on the affect of cannabis smoke alone; low rate of addiction compared to tobacco; and episodic nature of cannabis use compared to steady frequent smoking of tobacco.[30]
Professor David Nutt, a UK drug expert, points out that the study cited by the British Lung Foundation has been accused of both “false reasoning” and “incorrect methodology”. Further, he notes that other studies have failed to connect cannabis with lung cancer, and accuses the BLF of "scaremongering over cannabis".[31]
A study in the academic journal, Cancer Epidemiology, Biomarkers & Prevention, demonstrated that a marijuana cigarette deposits four times the amount of tar in the human respiratory tract than a tobacco cigarette.[32][33]
According to Harvard's Lester Grinspoon, there has never been a death associated directly to cannabis.[34][35] In defense of smoked Medical cannabis, Grinspoon noted, "there is very little evidence that smoking marijuana as a means of taking it represents a significant health risk. Although cannabis has been smoked widely in Western countries for more than four decades, there have been no reported cases of lung cancer or emphysema attributed to marijuana. I suspect that a day's breathing in any city with poor air quality poses more of a threat than inhaling a day's dose -- which for many ailments is just a portion of a joint -- of marijuana".[36]
One study in 2005, the largest of its kind, found no cannabis-cancer connection. Donald Tashkin, a pulmonologist at UCLA's David Geffin School of Medicine who studied marijuana for 30 years, noted:[37]
- "We hypothesized that there would be a positive association between marijuana use and lung cancer, and that the association would be more positive with heavier use. What we found instead was no association at all, and even a suggestion of some protective effect."
Tashkin began teaching new medical school students about his findings in 2012.[38][unreliable source?]
Short-term effects
When smoked, the short-term effects of cannabis manifest within seconds and are fully apparent within a few minutes,[39] typically lasting for 1-3 hours, varying by the person and the strain of marijuana.[40] The duration of noticeable effects has been observed to diminish due to prolonged, repeated use and the development of a tolerance to cannabinoids.
Psychoactive effects
The psychoactive effects of cannabis, known as a "high", are subjective and can vary based on the person and the method of use.
Cannabis is often considered an atypical, unique and sometimes paradoxical psychotropic due to its vast and sometimes contradictory array of effects. The subjective experience induced by using cannabis can be considered stimulatory and yet also sedative or depressant, while also having markedly mild psychedelic and even dissociative characteristics[citation needed].
When THC enters the blood stream and reaches the brain, it binds to cannabinoid receptors. The endogenous ligand of these receptors is anandamide, the effects of which THC emulates. This agonism of the cannabinoid receptors results in changes in the levels of various neurotransmitters, especially dopamine and norepinephrine; neurotransmitters which are closely associated with the acute effects of cannabis ingestion, such as euphoria and anxiety. Some effects may include a general alteration of conscious perception, euphoria, feelings of well-being, relaxation or stress reduction, increased appreciation of humor, music or the arts, joviality, metacognition and introspection, enhanced recollection (episodic memory), increased sensuality, increased awareness of sensation, increased libido,[41] and creativity. Abstract or philosophical thinking, disruption of linear memory and paranoia or anxiety are also typical. Anxiety is the most commonly reported side effect of smoking marijuana. Between 20 and 30 percent of recreational users experience intense anxiety and/or panic attacks after smoking cannabis.[42]
Cannabis also produces many subjective and highly tangible effects, such as greater enjoyment of food taste and aroma, an enhanced enjoyment of music and comedy, and marked distortions in the perception of time and space (where experiencing a "rush" of ideas from the bank of long-term memory can create the subjective impression of long elapsed time, while a clock reveals that only a short time has passed). At higher doses, effects can include altered body image, auditory and/or visual illusions, pseudo-hallucinatory or (rarely, at very high doses) fully hallucinatory experiences, and ataxia from selective impairment of polysynaptic reflexes. In some cases, cannabis can lead to dissociative states such as depersonalization[43][44] and derealization;[45] such effects are most often considered desirable, but have the potential to induce panic attacks and paranoia in some unaccustomed users.[citation needed]
Somatic effects

Some of the short-term physical effects of cannabis use include increased heart rate, dry mouth, reddening of the eyes (congestion of the conjunctival blood vessels), a reduction in intra-ocular pressure, muscle relaxation and a sensation of cold or hot hands and feet.[46]
Electroencephalography or EEG shows somewhat more persistent alpha waves of slightly lower frequency than usual.[47] Cannabinoids produce a "marked depression of motor activity" via activation of neuronal cannabinoid receptors belonging to the CB1 subtype.[48]
Duration
Effects of cannabis generally range from 10 minutes to 8 hours, depending on the potency of the dose, other drugs consumed, method of ingestion, set, setting, and personal tolerance to the drug's various effects.[citation needed]
Smoked
The total short-term duration of cannabis use when smoked is based on the potency and how much is smoked. Effects can typically last two to three hours.[40]
A study of ten healthy, robust, male volunteers who resided in a residential research facility sought to examine both acute and residual subjective, physiologic, and performance effects of smoking marijuana cigarettes. On three separate days, subjects smoked one NIDA marijuana cigarette containing either 0%, 1.8%, or 3.6% THC, documenting subjective, physiologic, and performance measures prior to smoking, five times following smoking on that day, and three times on the following morning. Subjects reported robust subjective effects following both active doses of marijuana, which returned to baseline levels within 3.5 hours. Heart rate increased and the pupillary light reflex decreased following active dose administration with return to baseline on that day. Additionally, marijuana smoking acutely produced decrements in smooth pursuit eye tracking. Although robust acute effects of marijuana were found on subjective and physiological measures, no effects were evident the day following administration, indicating that the residual effects of smoking a single marijuana cigarette are minimal.[49]
A Dutch double blind, randomized, placebo-controlled, cross-over study examining male volunteers aged 18–45 years with a self-reported history of regular cannabis use concluded that smoking of cannabis with very high THC levels (marijuana with 9–23% THC), as currently sold in coffee shops in the Netherlands, may lead to higher THC blood-serum concentrations[citation needed]. This is reflected by an increase of the occurrence of impaired psychomotor skills, particularly among younger or inexperienced cannabis smokers, who do not always adapt their smoking-style to the higher THC content.[50] High THC concentrations in cannabis were associated with a dose-related increase of physical effects (such as increase of heart rate, and decrease of blood pressure) and psychomotor effects (such as reacting more slowly, decreased ability to focus and concentrate, making more mistakes during performance testing, having less motor control, and experiencing drowsiness)[citation needed]. It was also observed during the study that the effects from a single joint lasted for more than eight hours[citation needed]. Reaction times remained impaired five hours after smoking, when the THC serum concentrations were significantly reduced, but still present[citation needed]. However, it is important to note that the subjects (without knowing the potency) were told to finish their (unshared) joints rather than titrate their doses, leading in many cases to significantly higher doses than they would normally take[citation needed]. Also, when subjects smoke on several occasions per day, accumulation of THC in blood-serum may occur[citation needed].
Oral
When taken orally (in the form of capsules, food or drink), the psychoactive effects take longer to manifest and generally last longer, typically lasting for 4–10 hours after consumption.[51] Very high doses may last even longer. Also, oral ingestion use eliminates the need to inhale toxic combustion products created by smoking and therefore reduces the risk of respiratory harm associated with cannabis smoking.
Neurological effects
The areas of the brain where cannabinoid receptors are most prevalently located are consistent with the behavioral effects produced by cannabinoids. Brain regions in which cannabinoid receptors are very abundant are the basal ganglia, associated with movement control; the cerebellum, associated with body movement coordination; the hippocampus, associated with learning, memory, and stress control; the cerebral cortex, associated with higher cognitive functions; and the nucleus accumbens, regarded as the reward center of the brain. Other regions where cannabinoid receptors are moderately concentrated are the hypothalamus, which regulates homeostatic functions; the amygdala, associated with emotional responses and fears; the spinal cord, associated with peripheral sensations like pain; the brain stem, associated with sleep, arousal, and motor control; and the nucleus of the solitary tract, associated with visceral sensations like nausea and vomiting.[52]
Most notably, the two areas of motor control and memory are where the effects of cannabis are directly and irrefutably evident. Cannabinoids, depending on the dose, inhibit the transmission of neural signals through the basal ganglia and cerebellum. At lower doses, cannabinoids seem to stimulate locomotion while greater doses inhibit it, most commonly manifested by lack of steadiness (body sway and hand steadiness) in motor tasks that require a lot of attention. Other brain regions, like the cortex, the cerebellum, and the neural pathway from cortex to striatum, are also involved in the control of movement and contain abundant cannabinoid receptors, indicating their possible involvement as well.
Experiments on animal and human tissue have demonstrated a disruption of short-term memory formation,[15] which is consistent with the abundance of CB1 receptors on the hippocampus, the region of the brain most closely associated with memory. Cannabinoids inhibit the release of several neurotransmitters in the hippocampus such as acetylcholine, norepinephrine, and glutamate, resulting in a major decrease in neuronal activity in that region. This decrease in activity resembles a "temporary hippocampal lesion."[15]
In in-vitro experiments THC at extremely high concentrations, which could not be reached with commonly consumed doses, caused competitive inhibition of the AChE enzyme and inhibition of β-amyloid peptide aggregation, implicated in the development of Alzheimer's disease. Compared to currently approved drugs prescribed for the treatment of Alzheimer's disease, THC is a considerably superior inhibitor of A aggregation, and this study provides a previously unrecognized molecular mechanism through which cannabinoid molecules may impact the progression of this debilitating disease.[53]
Effects on driving
Cannabis usage has been shown to negatively affect the ability to drive.[54] The British Medical Journal recently indicated that "Drivers who consume cannabis within three hours of driving are nearly twice as likely to cause a vehicle collision as those who are not under the influence of drugs or alcohol"[55]
An older 2001 study by the United Kingdom Transit Research Laboratory (TRL) also focused on the effects of cannabis use on driving.[56] The report summarizes current knowledge about the effects of cannabis on driving and accident risk based on a review of available literature published since 1994 and the effects of cannabis on laboratory based tasks. The study identified young males, amongst whom cannabis consumption is frequent and increasing, and in whom alcohol consumption is also common, as a risk group for traffic accidents. This is due to driving inexperience and factors associated with youth relating to risk taking, delinquency and motivation. These demographic and psychosocial variables may relate to both drug use and accident risk, thereby presenting an artificial relationship between use of drugs and accident involvement.
The effects of cannabis on laboratory-based tasks show clear impairment with respect to tracking ability, attention, and other tasks depending on the dose administered. Both simulation and road trials generally find that driving behavior shortly after consumption of larger doses of cannabis results in:
- increased variability in lane position (such as taking a curve too tightly or too loosely).
- longer decision times, leading to slower responses to driving situations
Kelly, Darke and Ross[57] show similar results, with laboratory studies examining the effects of cannabis on skills utilised while driving showing impairments in tracking, attention, reaction time, short-term memory, hand-eye coordination, vigilance, time and distance perception, and decision making and concentration. An EMCDDA[58] review concluded that "the acute effect of moderate or higher doses of cannabis impairs the skills related to safe driving and injury risk", specifically "attention, tracking and psychomotor skills".[58] In their review of driving simulator studies, Kelly et al.[57] conclude that there is evidence of dose-dependent impairments in cannabis-affected drivers' ability to control a vehicle in the areas of steering, headway control, speed variability, car following, reaction time and lane positioning. The researchers note that "even in those who learn to compensate for a drug's impairing effects, substantial impairment in performance can still be observed under conditions of general task performance (i.e. when no contingencies are present to maintain compensated performance)."[58]
A report from the University of Colorado, Montana State University, and the University of Oregon found that on average, states that have legalized Medical cannabis had a decrease in traffic-related fatalities by 8-11%.[59] The researchers hypothesized "it’s just safer to drive under the influence of marijuana than it is drunk....Drunk drivers take more risk, they tend to go faster. They don’t realize how impaired they are. People who are under the influence of marijuana drive slower, they don’t take as many risks”. Another consideration, they added, was the fact that users of marijuana tend not to go out as much.[60]
Vascular effects
Cannabis arteritis is a very rare peripheral vascular disease similar to Buerger's disease. There were about 50 confirmed cases from 1960 to 2008, all of which occurred in Europe.[61] However, all of the cases also involved tobacco [citation needed] (a known cause of Buerger's disease) in one way or another, and nearly all of the cannabis use was quite heavy [citation needed]. In Europe, cannabis is typically mixed with tobacco, in contrast to North America. [citation needed]
A 2008 study by the National Institutes of Health Biomedical Research Centre in Baltimore found that heavy, chronic smoking of marijuana (138 joints per week) changed blood proteins associated with heart disease and stroke.[62] This may be a result of raised carboxyhemoglobin levels from carbon monoxide. A similar increase in heart disease and ischemic strokes is observed in tobacco smokers, which suggests that the harmful effects come from combustion products, not marijuana.
A 2005 article in the Journal of Neurology, Neurosurgery and Psychiatry reported on a 36-year-old man who suffered a stroke on three separate occasions after smoking a large amount of marijuana, despite having no known risk factors for the disorder, suggesting that a rare side effect of marijuana use may be an increase in the incidence of strokes among young smokers.[63] A 2000 study by researchers at Boston's Beth Israel Deaconess Medical Center, Massachusetts General Hospital and Harvard School of Public Health also found that a middle-age person's risk of heart attack rises nearly fivefold in the first hour after smoking marijuana, about the same elevated risk as vigorous exercise or sexual intercourse.[64]
Adulterated cannabis
Contaminants may be found in hashish obtained from "soap bar"-type sources.[65] The dried flowers of the plant may be contaminated by the plant taking up heavy metals and other toxins from its growing environment,[66] or by the addition of lead or glass beads, used to increase the weight or to make the cannabis appear as if it has more crystal-looking trichomes indicating a higher THC content.[67] Users who burn hot or mix cannabis with tobacco are at risk of failing to detect deviations from appropriate cannabis taste.
Despite cannabis being generally perceived as a natural or "chemical-free" product,[68] in a recent Australian survey[69] one in four Australians consider cannabis grown indoors under hydroponic conditions to be a greater health risk due to increased contamination, added to the plant during cultivation to enhance the plant growth and quality.
Combination with other drugs
The most obvious confounding factor in cannabis research is the prevalent usage of other recreational drugs, especially alcohol and nicotine.[70] Such complications demonstrate the need for studies on cannabis that have stronger controls, and investigations into alleged symptoms of cannabis use that may also be caused by tobacco. Some critics question whether agencies doing the research make an honest effort to present an accurate, unbiased summary of the evidence, or whether they "cherry-pick" their data to please funding sources which may include the tobacco industry or governments dependent on cigarette tax revenue; others caution that the raw data, and not the final conclusions, are what should be examined.[71]
Cannabis also has been shown to have a synergistic cytotoxic effect on lung cancer cell cultures in vitro with the food additive butylated hydroxyanisole (BHA) and possibly the related compound butylated hydroxytoluene (BHT). The study concluded, "Exposure to marijuana smoke in conjunction with BHA, a common food additive, may promote deleterious health effects in the lung." BHA & BHT are human-made fat preservatives, and are found in many packaged foods including: plastics in boxed cereal, Jello, Slim Jims, and more.[72][further explanation needed]
The Australian National Household Survey of 2001[73] showed that cannabis use in Australia is rarely used without other drugs. 95% of cannabis users also drank alcohol; 26% took amphetamines; 19% took ecstasy and only 2.7% reported not having used any other drug with cannabis.[74] While research has been undertaken on the combined effects of alcohol and cannabis on performing certain tasks, little research has been conducted on the reasons why this combination is so popular. Evidence from a controlled experimental study undertaken by Lukas and Orozco[75] suggests that alcohol causes THC to be absorbed more rapidly into the blood plasma of the user. Data from the Australian National Survey of Mental Health and Wellbeing[76] found that three-quarters of recent cannabis users reported using alcohol when cannabis was not available.[77]
Memory and learning
Studies on cannabis and memory are hindered by small sample sizes, confounding drug use, and other factors.[78] The strongest evidence regarding cannabis and memory focuses on its temporary negative effects on short-term and working memory.[11]
Researchers from the University of California, San Diego School of Medicine failed to show substantial, systemic neurological effects from long-term recreational use of cannabis. Their findings were published in the July 2003 issue of the Journal of the International Neuropsychological Society.[79] The research team, headed by Dr Igor Grant, found that cannabis use did affect perception, but did not cause permanent brain damage. Researchers looked at data from 15 previously published controlled studies involving 704 long-term cannabis users and 484 nonusers. The results showed long-term cannabis use was only marginally harmful on the memory and learning. Other functions such as reaction time, attention, language, reasoning ability, perceptual and motor skills were unaffected. The observed effects on memory and learning, they said, showed long-term cannabis use caused "selective memory defects", but that the impact was "of a very small magnitude".[80]
Appetite
The feeling of increased appetite following the use of cannabis has been documented for hundreds of years,[81] and is known as "the munchies" in popular culture. Clinical studies and survey data have found that cannabis increases food enjoyment and interest in food.[82][83] Scientists have claimed to be able to explain what causes the increase in appetite, concluding that "endocannabinoids in the hypothalamus activate cannabinoid receptors that are responsible for maintaining food intake".[83] Rarely, chronic users experience a severe vomiting disorder, cannabinoid hyperemesis syndrome, after smoking and find relief by taking hot baths.[84]
Endogenous cannabinoids (“endocannabinoids”) were discovered in cow's milk and soft cheeses.[85][86] Endocannabinoids were also found in human breast milk.[87] It is widely accepted that the neonatal survival of many species "is largely dependent upon their suckling behavior, or appetite for breast milk"[88] and recent research has identified the endogenous cannabinoid system to be the first neural system to display complete control over milk ingestion and neonatal survival.[89] It is possible that "cannabinoid receptors in our body interact with the cannabinoids in milk to stimulate a suckling response in newborns so as to prevent growth failure".[88]
Long-term effects
Though the long-term effects of cannabis have been studied, there remains much to be concluded; debated topics include the drug's addictiveness, its potential as a "gateway drug", its effects on intelligence and memory, and its contributions to mental disorders such as schizophrenia and depression. On some such topics, such as the drug's effects on the lungs, relatively little research has been conducted, leading to division as to the severity of its impact. However, a study funded by the US government on the long term lung-related effects of marijuana has concluded that moderate marijuana use does not impair pulmonary function.[90][91]
More research is no guarantee of greater consensus in the field of cannabis studies, however; both advocates and opponents of the drug are able to call upon multiple scientific studies supporting their respective positions. Cannabis has been correlated with the development of various mental disorders in multiple studies, for example a recent 10 year study on 1923 individuals from the general population in Germany, aged 14–24, concluded that cannabis use is a risk factor for the development of incident psychotic symptoms. Continued cannabis use might increase the risk for psychotic disorder.[92]
Efforts to prove the "gateway drug" hypothesis that cannabis and alcohol makes users more inclined to become addicted to "harder" drugs like cocaine and heroin have produced mixed results, with different studies finding varying degrees of correlation between the use of cannabis and other drugs, and some finding none. Some[who?], however, believe the "gateway effect," currently being pinned on the use of marijuana, should not be attributed to the drug itself but rather the illegality of the drug in most countries. Supporters of this theory[attribution needed] believe that the grouping of marijuana and harder drugs in law is, in fact, the cause of users of marijuana to move on to those harder drugs.
There have been debates as to whether cannabis can lead to heavy addiction. According to one of the studies on the issue, the La Guardia Committee of 1944, smoking marijuana could help to get out of the addiction from substances like cocaine or morphine.
Effects in pregnancy
A study of 600 mothers that reported smoking cannabis during pregnancy suggested that it was not associated with increased risk of perinatal mortality.[93] However, frequent and regular use of cannabis throughout pregnancy may be associated with a small but statistically detectable decrease in birth weight.[93]
Melanie Dreher, dean of nursing at Rush Medical Center in Chicago, conducted a study of Jamaican women who used cannabis throughout their pregnancies, as well as their babies' first year. The study was published in the American Journal of Pediatrics in 1994.[94] Dreher expected to see a decrease in birth weight, but saw none. Instead, the exposed babies socialized and made eye contact more quickly, had better organization and modulation of sleeping and waking, and were less prone to anxiety. On difference between the Jamaican and other studies' results, "Medicine hunter" Chris Kilham noted, "In U.S. studies where we've seen a similar investigation, women have concurrently been abusing alcohol and other drugs as well".[95]
Pathogens and microtoxins
Most microorganisms found in cannabis only affect plants and not humans, but some microorganisms, especially those that proliferate when the herb is not correctly dried and stored, can be harmful to humans. Some users may store marijuana in an airtight bag or jar in a refrigerator to prevent fungal and bacterial growth.[96]
Fungi
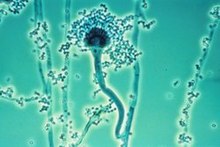
The fungi Aspergillus flavus,[97] Aspergillus fumigatus,[97] Aspergillus niger,[97] Aspergillus parasiticus, Aspergillus tamarii, Aspergillus sulphureus, Aspergillus repens, Mucor hiemalis (not a human pathogen), Penicillium chrysogenum, Penicillium italicum and Rhizopus nigrans have been found in moldy cannabis.[96] Aspergillus mold species can infect the lungs via smoking or handling of infected cannabis and cause opportunistic and sometimes deadly aspergillosis.[citation needed] Some of the microorganisms found create aflatoxins, which are toxic and carcinogenic. Researchers suggest that moldy cannabis thus be discarded.[citation needed]
Mold is also found in smoke from mold infected cannabis,[96][97] and the lungs and nasal passages are a major means of contracting fungal infections. Levitz and Diamond (1991) suggested baking marijuana in home ovens at 150 °C [302 °F], for five minutes before smoking. Oven treatment killed conidia of A. fumigatus, A. flavus and A. niger, and did not degrade the active component of marijuana, tetrahydrocannabinol (THC)."[96]
Bacteria
Cannabis contaminated with Salmonella muenchen was positively correlated with dozens of cases of salmonellosis in 1981.[98] "Thermophilic actinomycetes" were also found in cannabis.[97]
Constraints on open research

In many countries, experimental science regarding cannabis is restricted due to its illegality. Thus, cannabis as a drug is often hard to fit into the structural confines of medical research because appropriate, research-grade samples are difficult to obtain for research purposes, unless granted under authority of national governments.
United States
This issue was highlighted in the United States by the clash between Multidisciplinary Association for Psychedelic Studies (MAPS), an independent research group, and the National Institute on Drug Abuse (NIDA), a federal agency charged with the application of science to the study of drug abuse. The NIDA largely operates under the general control of the Office of National Drug Control Policy (ONDCP), a White House office responsible for the direct coordination of all legal, legislative, scientific, social and political aspects of federal drug control policy.[citation needed]
The cannabis that is available for research studies in the United States is grown at the University of Mississippi and solely controlled by the NIDA, which has veto power over the Food and Drug Administration (FDA) to define accepted protocols. Since 1942, when cannabis was removed from the U.S. Pharmacopoeia and its medical use was prohibited, there have been no legal (under federal law) privately funded cannabis production projects. This has resulted in a limited amount of research being done and possibly in NIDA producing cannabis which has been alleged to be of very low potency and inferior quality.[99]
MAPS, in conjunction with Professor Lyle Craker, PhD, the director of the Medicinal Plant Program at the University of Massachusetts Amherst, sought to provide independently grown cannabis of more appropriate research quality for FDA-approved research studies, and encountered opposition by NIDA, the ONDCP, and the U.S. Drug Enforcement Administration (DEA).[100]
United Kingdom
In countries such as the United Kingdom a license for growing cannabis is required if it is to be used for botanical or scientific reasons.[citation needed] It is referred to as a "controlled drug". In such countries a greater depth and variety of scientific research has been performed. Recently several habitual smokers were invited to partake in various tests by British medical companies in order for the UK government to ascertain the influence of cannabis on operating a motor vehicle, with the conclusion that marijuana strongly impairs the ability to drive a motor vehicle.[citation needed]
See also
- Cannabis smoking
- Contact high
- Harm reduction
- National Cannabis Prevention and Information Centre
- Psychoactive drug
- Responsible drug use
References
- ^ Medical cannabis, en.wikipedia.org, retrieved 2013-01-08
- ^ Osborne, Geraint B.; Fogel, Curtis (2008). "Understanding the Motivations for Recreational Marijuana Use Among Adult Canadians1" (PDF). Substance Use & Misuse. 43 (3–4): 539–72. doi:10.1080/10826080701884911.
- ^ Ranganathan, Mohini; D’souza, Deepak Cyril (2006). "The acute effects of cannabinoids on memory in humans: a review". Psychopharmacology. 188 (4): 425–44. doi:10.1007/s00213-006-0508-y. PMID 17019571.
- ^ Leweke, F. Markus; Koethe, Dagmar (2008). "Cannabis and psychiatric disorders: it is not only addiction". Addiction Biology. 13 (2): 264–75. doi:10.1111/j.1369-1600.2008.00106.x. PMID 18482435.
- ^ Rubino, T; Parolaro, D (2008). "Long lasting consequences of cannabis exposure in adolescence". Molecular and Cellular Endocrinology. 286 (1–2 Suppl 1): S108–13. doi:10.1016/j.mce.2008.02.003. PMID 18358595.
- ^ Michael Slezak (2009-09-01), Doubt cast on cannabis, schizophrenia link, Abc.net.au, retrieved 2013-01-08
- ^ Boston Municipal Courtcentral Division. Docket # 0701CR7229 (PDF), 2008, retrieved 2013-01-08
- ^ Delisi, Lynn E (2008). "The effect of cannabis on the brain: can it cause brain anomalies that lead to increased risk for schizophrenia?". Current Opinion in Psychiatry. 21 (2): 140–50. doi:10.1097/YCO.0b013e3282f51266. PMID 18332661.
- ^ Denson, TF; Earleywine, M (2006). "Decreased depression in marijuana users". Addictive behaviors. 31 (4): 738–42. doi:10.1016/j.addbeh.2005.05.052. PMID 15964704.
- ^ Grotenhermen, Franjo (2007). "The Toxicology of Cannabis and Cannabis Prohibition". Chemistry & Biodiversity. 4 (8): 1744–69. doi:10.1002/cbdv.200790151. PMID 17712818.
- ^ a b Riedel, G.; Davies, S. N. (2005). "Cannabinoid Function in Learning, Memory and Plasticity". Handbook of Experimental Pharmacology. Handbook of Experimental Pharmacology. 168 (168): 445–477. doi:10.1007/3-540-26573-2_15. ISBN 3-540-22565-X. PMID 16596784.
- ^ Touw, Mia. "The religious and medicinal uses of Cannabis in China, India and Tibet" (PDF). J Psychoactive Drugs. 13 (1).
- ^ a b H.K. Kalant & W.H.E. Roschlau (1998). Principles of Medical Pharmacology (6th ed.). pp. 373–375.
- ^ Turner, Carlton E.; Bouwsma, Otis J.; Billets, Steve; Elsohly, Mahmoud A. (1980). "Constituents ofCannabis sativa L. XVIII – Electron voltage selected ion monitoring study of cannabinoids". Biological Mass Spectrometry. 7 (6): 247–56. doi:10.1002/bms.1200070605.
- ^ a b c d J.E. Joy, S. J. Watson, Jr., and J.A. Benson, Jr, (1999). Marijuana and Medicine: Assessing The Science Base. Washington D.C: National Academy of Sciences Press. ISBN 0-585-05800-8.
{{cite book}}: CS1 maint: extra punctuation (link) CS1 maint: multiple names: authors list (link)[page needed] - ^ Hampson, A. J.; Grimaldi, M.; Axelrod, J.; Wink, D. (1998). "Cannabidiol and (−)Δ9-tetrahydrocannabinol are neuroprotective antioxidants". Proceedings of the National Academy of Sciences. 95 (14): 8268–73. Bibcode:1998PNAS...95.8268H. doi:10.1073/pnas.95.14.8268. PMC 20965. PMID 9653176.
- ^ H. Abadinsky (2004). Drugs: An Introduction (5th ed.). pp. 62–77, 160–166. ISBN 0-534-52750-7.
- ^ 1996. The Merck Index, 12th ed., Merck & Co., Rahway, New Jersey
- ^ Cannabis Chemistry, Erowid.org
- ^ http://www.druglibrary.org/schaffer/library/mjfaq1.htm [unreliable source?]
- ^ http://www.askmen.com/sports/health/20_mens_health.html [unreliable source?]
- ^ "UK government report" (PDF). House of Commons Science and Technology Committee. 2006-07-18. Retrieved 2006-08-29.The information is not in the report, but in evidence submitted to the committee. Needs correcting -- can cite Lancet paper by David Nutt et al.
- ^ a b c Moir, David; Rickert, William S.; Levasseur, Genevieve; Larose, Yolande; Maertens, Rebecca; White, Paul; Desjardins, Suzanne (2008). "A Comparison of Mainstream and Sidestream Marijuana and Tobacco Cigarette Smoke Produced under Two Machine Smoking Conditions". Chemical Research in Toxicology. 21 (2): 494–502. doi:10.1021/tx700275p. PMID 18062674.
- ^ "Marijuana v.s. Tobacco smoke compositions", from: Institute of Medicine, Marijuana and Health, Washington, D.C. National Academy Press, Erowid.org, 1988
{{citation}}:|access-date=requires|url=(help); Unknown parameter|ur=ignored (help) - ^ David Malmo-Levine (2002-01-02), Radioactive Tobacco, retrieved 2013-01-09
- ^ Gumbiner, Jann (17 February 2011), Does Marijuana Cause Cancer?, Psychology Today, retrieved 23 June 2012
{{citation}}: Cite has empty unknown parameter:|coauthors=(help) - ^ Does smoking cannabis cause cancer?, Cancer Research UK, 20 September 2010, retrieved 23 June 2012
- ^ Tashkin, Donald (1997), Effects of marijuana on the lung and its immune defenses, UCLA School of Medicine, retrieved 2012-06-23
{{citation}}: Unknown parameter|month=ignored (help) - ^ Chemicals known to the state to cause cancer or reproductive toxicity (PDF), ca.gov, 2012-07-20, retrieved 2013-01-08
- ^ The impact of cannabis on your lung, British Lung Association, 2012, retrieved 2013-01-08
{{citation}}: Unknown parameter|month=ignored (help) - ^ Le, Bryan (2012-06-08), Drug prof slams pot lung-danger claims, The Fix, retrieved 2013-01-09
- ^ Zuo-Feng Zhang, Hal Morgenstern, Margaret R. Spitz, Donald P. Tashkin, Guo-Pei Yu, James R. Marshall, T. C. Hsu and Stimson P. Schantz (December 1999). "Marijuana Use and Increased Risk of Squamous Cell Carcinoma of the Head and Neck". Cancer Epidemiology, Biomarkers & Prevention. 8 (1071). PMID 10613339.
In addition, a single marijuana cigarette deposits four times as much tar in the respiratory tract as that deposited from a single filtered tobacco cigarette of approximately the same weight. The higher content of carcinogenic polycyclic aromatic hydrocarbons in marijuana smoke and the greater deposition of marijuana tar in the lung act together to amplify exposure of the marijuana smoker to carcinogens in the particulate phase.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Tzu-Chin WU, Donald P. Tashkin, Behnam Djahed, Jed E. Rose (1988). "Pulmonary hazards of smoking marijuana as compared with tobacco". New England Journal of Medicine. 318 (6): 347–51. PMID 3340105.
We conclude that smoking marijuana, regardless of tetrahydrocannabinol content, results in a substantially greater respiratory burden of carbon monoxide and tar than smoking a similar quantity of tobacco.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Grinspoon, Lester (2012-09-23), Grinspoon: Marijuana is here to stay, The MetroWest Daily News, retrieved 2013-01-08
- ^ Dave Smith (2012-08-08), Medical marijuana: 10 health benefits that legitimize legalization, Ibtimes.com, retrieved 2012-12-31
- ^ Puffing is the best medicine, latimes.com, 2006-05-05, retrieved 2013-01-08
- ^ Study finds no cancer-marijuana connection, Washingtonpost.com, 2006-05-25, retrieved 2013-01-08
- ^ Fred Gardner (2012-10-24), Media ignored expert's shocking findings that marijuana helps prevent lung cancer: now it's med-school material, Alternet, retrieved 2013-01-08
- ^ Ashton, C. H. (2001). "Pharmacology and effects of cannabis: a brief review". The British Journal of Psychiatry. 178 (2): 101–6.
- ^ a b Cannabis, Dasc.sa.gov.au, retrieved 2011-04-20
- ^ http://cannabislink.ca/info/MotivationsforCannabisUsebyCanadianAdults-2008.pdf
- ^ <Please add first missing authors to populate metadata.> (2010). "Medical Marijuana and the Mind". Harvard Mental Health Letter. Retrieved April 25, 2011.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Medication-Associated Depersonalization Symptoms
- ^ Shufman, E; Lerner, A; Witztum, E (2005). "Depersonalization after withdrawal from cannabis usage" (PDF). Harefuah (in Hebrew). 144 (4): 249–51, 303. PMID 15889607.
- ^ Johnson, BA (1990). "Psychopharmacological effects of cannabis". British journal of hospital medicine. 43 (2): 114–6, 118–20, 122. PMID 2178712.
- ^ Moelker, Wendy (19 Sep 2008). "How does Marijuana Affect Your Body? What are the Marijuana Physical Effects?".
- ^ H.K. Kalant & W.H.E. Roschlau (1998). Principles of Medical Pharmacology (6th ed.). pp. 373–375.
- ^ Andersson, M.; Usiello, A; Borgkvist, A; Pozzi, L; Dominguez, C; Fienberg, AA; Svenningsson, P; Fredholm, BB; Borrelli, E (2005). "Cannabinoid Action Depends on Phosphorylation of Dopamine- and cAMP-Regulated Phosphoprotein of 32 kDa at the Protein Kinase A Site in Striatal Projection Neurons". Journal of Neuroscience. 25 (37): 8432–8. doi:10.1523/JNEUROSCI.1289-05.2005. PMID 16162925.
- ^ Fant, R (1998). "Acute and Residual Effects of Marijuana in Humans". Pharmacology Biochemistry and Behavior. 60 (4): 777–84. doi:10.1016/S0091-3057(97)00386-9.
- ^ Tj. T. Mensinga. A double-blind, randomized, placebo-controlled, cross-over study on the pharmacokinetics and effects of cannabis (PDF). RIVM. Retrieved 2007-09-21.
{{cite book}}: Invalid|display-authors=1(help); Unknown parameter|author-separator=ignored (help) - ^ http://www.erowid.org/plants/cannabis/cannabis_effects.shtml[unreliable medical source?]
- ^ Pertwee, R (1997). "Pharmacology of cannabinoid CB1 and CB2 receptors". Pharmacology & Therapeutics. 74 (2): 129–80. doi:10.1016/S0163-7258(97)82001-3.
- ^ Eubanks, Lisa M.; Rogers, Claude J.; Beuscher, 4th; Koob, George F.; Olson, Arthur J.; Dickerson, Tobin J.; Janda, Kim D. (2006). "A Molecular Link Between the Active Component of Marijuana and Alzheimer's Disease Pathology". Molecular Pharmaceutics. 3 (6): 773–7. doi:10.1021/mp060066m. PMC 2562334. PMID 17140265.
{{cite journal}}: CS1 maint: numeric names: authors list (link) - ^ Li MC, Brady JE, DiMaggio CJ, Lusardi AR, Tzong KY, Li G. (2012), Marijuana use and motor vehicle crashes., Epidemiol Rev. 2012 Jan;34(1):65-72., PMID 21976636
{{citation}}:|access-date=requires|url=(help)CS1 maint: multiple names: authors list (link) - ^ Ashbridge, Mark (2012), Acute cannabis consumption and motor vehicle collision risk, British Medical Journal, retrieved 14 june, 2012
{{citation}}: Check date values in:|accessdate=(help) - ^ "Cannabis and driving: a review of the literature and commentary (No.12)". The National Archives (UK). 8 February 2010. Archived from the original on 2010. Retrieved 1 February 2011.
{{cite web}}: Check date values in:|archivedate=(help) - ^ a b Kelly, Erin; Darke, Shane; Ross, Joanne (2004). "A review of drug use and driving: epidemiology, impairment, risk factors and risk perceptions". Drug and Alcohol Review. 23 (3): 319–44. doi:10.1080/09595230412331289482. PMID 15370012.
- ^ a b c Sznitman, Sharon Rödner; Olsson, Börje; Room, Robin, eds. (2008). A cannabis reader: global issues and local experiences (PDF). Vol. 2. Lisbon: European Monitoring Centre for Drugs and Drug Addiction. doi:10.2810/13807. ISBN 978-92-9168-312-3.
{{cite book}}: Unknown parameter|month=ignored (help)[page needed] - ^ Morrison, James (2013-01-01), Separating fact vs. fear on medical marijuana, The Herald News, retrieved 2013-01-08
- ^ Driving stoned: safer than driving drunk?, Abcnews.go.com, 2011-12-02, retrieved 2013-01-08
- ^ Peyrot, I; Garsaud, A-M; Saint-Cyr, I; Quitman, O; Sanchez, B; Quist, D (2007). "Cannabis arteritis: a new case report and a review of literature". Journal of the European Academy of Dermatology and Venereology. 21 (3): 388–91. doi:10.1111/j.1468-3083.2006.01947.x. PMID 17309465.
- ^ "Heavy pot smoking could raise risk of heart attack, stroke". CBC. 2008-05-13. Retrieved 2009-04-17.
- ^ Norton, Amy (2005-02-22). "More Evidence Ties Marijuana to Stroke Risk". Reuters Health. Retrieved 2009-04-26.
- ^ Noble, Holcomb B. (2000-03-03). "Report Links Heart Attacks To Marijuana". New York Times. Retrieved 2009-04-26.
- ^ Soapbar – Just Say No to polluted hash[unreliable medical source?]
- ^ Flin Flon Mine Area Marijuana Contamination, Medicalmarihuana.ca, retrieved 2011-04-20
- ^ "Warnings over glass in cannabis". BBC News. 2007-02-01. Retrieved 2010-05-23.
- ^ Hall, W.; Nelson, J. (1995). Public perceptions of the health and psychological consequences of cannabis use. Canberra: Australian Government Publishing Service. ISBN 978-0-644-42830-9.[page needed]
- ^ StollzNow (2006). Market research report: Australians on cannabis. Report prepared for NDARC and Pfizer Australia. Sydney: StollzNow Research and Advisory.[page needed]
- ^ Zhang, Zuo-Feng; Morgenstern, Hal; Spitz, Margaret R.; Tashkin, Donald P.; Yu, Guo-Pei; Marshall, James R.; Hsu, T. C.; Schantz, Stimson P. (1999). "Marijuana use and increased risk of squamous cell carcinoma of the head and neck". Cancer epidemiology, biomarkers & prevention. 8 (12): 1071–8. PMID 10613339.
- ^ Public opinion on drugs and drug policy. Transform Drug Policy Foundation: Fact Research Guide. "Data is notoriously easy to cherry pick or spin to support a particular agenda or position. Often the raw data will conceal all sorts of interesting facts that the headlines have missed." Transform Drug Policy Foundation, Easton Business Centre, Felix Rd., Bristol, UK. Retrieved on 24 March 2007.
- ^ Sarafian, Theodore A.; Kouyoumjian, Shaghig; Tashkin, Donald; Roth, Michael D. (2002). "Synergistic cytotoxicity of Δ9-tetrahydrocannabinol and butylated hydroxyanisole". Toxicology Letters. 133 (2–3): 171–9. doi:10.1016/S0378-4274(02)00134-0. PMID 12119125.
- ^ "2001 National Drug Strategy Household Survey: detailed findings". Australian Institute of Health and Welfare. 2002-12-19. Retrieved 2011-02-01. AIHW cat no. PHE 41.
- ^ "2001 National Drug Steategy Household Survey: first results". Australian Institute of Health and Welfare. 2002-05-20. Retrieved 2011-02-01. AIHW cat no. PHE 35.
- ^ Lukas, Scott E.; Orozco, Sara (2001). "Ethanol increases plasma Δ9-tetrahydrocannabinol (THC) levels and subjective effects after marihuana smoking in human volunteers". Drug and Alcohol Dependence. 64 (2): 143–9. doi:10.1016/S0376-8716(01)00118-1. PMID 11543984.
- ^ Kee, Carol (1998). National Survey of Mental Health and Wellbeing of Adults 1997. ACT Department of Health and Community Care.
{{cite book}}: Unknown parameter|month=ignored (help) - ^ Hall, Louisa; Degenhardt, Wayne (2001). "The relationship between tobacco use, substance-use disorders and mental health: results from the National Survey of Mental Health and Well-being". Nicotine & Tobacco Research. 3 (3): 225–34. doi:10.1080/14622200110050457.
- ^ Riedel, G.; Davies, S. N. (2005). "Cannabinoids". Handbook of experimental pharmacology. Handbook of Experimental Pharmacology. 168 (168): 445–77. doi:10.1007/3-540-26573-2_15. ISBN 3-540-22565-X. PMID 16596784.
{{cite journal}}:|chapter=ignored (help) - ^ Minimal Long-Term Effects of Marijuana Use Found
- ^ http://www.cmcr.ucsd.edu/images/pdfs/Reuters_062703.pdf
- ^ Mechoulam, R. (1984). Cannabinoids as therapeutic agents. Boca Raton, FL: CRC Press. ISBN 0-8493-5772-1.[page needed]
- ^ Ad Hoc Group of Experts. "Report to the Director, National Institutes of Health" (Workshop on the Medical Utility of Marijuana). Institute of Medicine.
- ^ a b Bonsor, Kevin. "How Marijauan Works: Other Physiological Effects". HowStuffWorks. Retrieved on 2007-11-03
- ^ Sontineni, Siva P.; Chaudhary, Sanjay; Sontineni, Vijaya; Lanspa, Stephen J. (2009). "Cannabinoid hyperemesis syndrome: Clinical diagnosis of an underrecognised manifestation of chronic cannabis abuse". World Journal of Gastroenterology. 15 (10): 1264–1266. doi:10.3748/wjg.15.1264. Retrieved 20 December 2012.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Di Marzo, Vincenzo; Sepe, Nunzio; De Petrocellis, Luciano; Berger, Alvin; Crozier, Gayle; Fride, Ester; Mechoulam, Raphael (1998). "Trick or treat from food endocannabinoids?". Nature. 396 (6712): 636. Bibcode:1998Natur.396..636D. doi:10.1038/25267. PMID 9872309.
{{cite journal}}: More than one of|pages=and|page=specified (help) - ^ Di Tomaso, Emmanuelle; Beltramo, Massimiliano; Piomelli, Daniele (1996). "Brain cannabinoids in chocolate". Nature. 382 (6593): 677–8. Bibcode:1996Natur.382..677D. doi:10.1038/382677a0. PMID 8751435.
- ^ Ester Fride (2004). "The endocannabinoid-CB1 receptor system in pre- and postnatal life". European Journal of Pharmacology. 500: 289–97. doi:10.1016/j.ejphar.2004.07.033.
{{cite journal}}: Unknown parameter|issues=ignored (help); Unknown parameter|month=ignored (help) - ^ a b NCPIC Research Briefs • NCPIC, Ncpic.org.au, 2011-03-11, retrieved 2011-04-20
- ^ Fride, E (2004). "The endocannabinoid-CB1 receptor system in pre- and postnatal life". European Journal of Pharmacology. 500 (1–3): 289–97. doi:10.1016/j.ejphar.2004.07.033. PMID 15464041.
- ^ Szalavitz, Maia (2012-01-10), Study: smoking marijuana not linked with lung famage, TIME.com, retrieved 2013-01-08
- ^ "Association Between Marijuana Exposure and Pulmonary Function Over 20 Years". Journal of the American Medical Association. 307 (2): 173–181. doi:10.1001/jama.2011.1961.
{{cite journal}}: Cite uses deprecated parameter|authors=(help) - ^ Kuepper, R.; Van Os, J.; Lieb, R.; Wittchen, H.-U.; Hofler, M.; Henquet, C. (2011-03-01). "Continued cannabis use and risk of incidence and persistence of psychotic symptoms: 10 year follow-up cohort study". BMJ. 342. BMJ: d738. doi:10.1136/bmj.d738. PMC 3047001. PMID 21363868. Retrieved 2011-08-23.
- ^ a b Attention: This template ({{cite doi}}) is deprecated. To cite the publication identified by doi:10.1111/j.1471-0528.2002.01020.x, please use {{cite journal}} (if it was published in a bona fide academic journal, otherwise {{cite report}} with
|doi=10.1111/j.1471-0528.2002.01020.xinstead. - ^ "Identifying prenatal cannabis exposure and effects of concurrent tobacco exposure on neonatal growth". Clinical Chemestry. 56 (9): 1442–1450. 2010-07-13. doi:10.1373/clinchem.2010.147876.
{{cite journal}}: Cite uses deprecated parameter|authors=(help) - ^ Researchers study neuroprotective properties in cannabis, Fox News, 2012-03-20, retrieved 2013-01-08
- ^ a b c d "Microbiological contaminants of marijuana". www.hempfood.com. Retrieved 2008-06-22.
- ^ a b c d e Kagen, S; Kurup, V; Sohnle, P; Fink, J (1983). "Marijuana smoking and fungal sensitization". Journal of Allergy and Clinical Immunology. 71 (4): 389–93. doi:10.1016/0091-6749(83)90067-2. PMID 6833678.
- ^ Taylor, David N.; Wachsmuth, I. Kaye; Shangkuan, Yung-hui; Schmidt, Emmett V.; Barrett, Timothy J.; Schrader, Janice S.; Scherach, Charlene S.; McGee, Harry B.; Feldman, Roger A. (1982). "Salmonellosis Associated with Marijuana". New England Journal of Medicine. 306 (21): 1249–53. doi:10.1056/NEJM198205273062101. PMID 7070444.
- ^ Lyle E. Craker, Ph. D. v. U.S. Drug Enforcement Administration, Docket No. 05-16, May 8, 2006, 8–27 PDF
- ^ People Working to Legalize Medical Marijuana, ACLU, 2005-11-29, retrieved 2010-03-05
External links
This article's use of external links may not follow Wikipedia's policies or guidelines. (October 2012) |
- MSN | Stoned Drivers Safer Than Drunks
- Cannabis Use and Psychosis from National Drug and Alcohol Research Centre, Australia
- The key research on cannabis use and mental illness at BBC News
- Provision of Marijuana and Other Compounds For Scientific Research recommendations of The National Institute on Drug Abuse National Advisory Council
- Scientific American Magazine (December 2004 Issue) The Brain's Own Marijuana
- Ramström, J. (2003), Adverse Health Consequences of Cannabis Use, A Survey of Scientific Studies Published up to and including the Autumn of 2003, National institute of public health, Sweden, Stockholm.
- Hall, W., Solowij, N., Lemon, J., The Health and Psychological Consequences of Cannabis Use. Canberra: Australian Government Publishing Service; 1994.
- World Health Organisation, PROGRAMME ON SUBSTANCE ABUSE, Cannabis: a health perspective and research agenda;1997.
- Cannabis and mental health factsheet
- Bibliography of scholarly histories on cannabis and hashish. (Updated to include article abstracts.)
- Marijuana and Immunity
- The National Cannabis Prevention and Information Centre (Australia)
- EU Research paper on the potency of Cannabis (2004)
- Driving under the influence of cannabis: a brief review of the literature
- Cannabis Contamination Research Brief
- Cannabinoids and appetite
- NCPIC e-zine December 2007/ January 2008 Commentary on cannabis toxicity research and Moir report
- Cannabis use and reproduction
- Evidence-based answers to cannabis questions
- NCPIC Cannabis and alcohol factsheet
- Fast Facts on Mental Health + Cannabis National Cannabis Prevention and Information Centre (Australia)
- Cannabis and Mental Health information leaflet from mental health charity The Royal College of Psychiatrists
- http://well.blogs.nytimes.com/2012/01/11/marijuana-smoking-does-not-harm-lungs-study-finds/
