Decompression (diving): Difference between revisions
→In water recompression: wrong word used |
Undid revision 497791682 by 14.202.65.49 (talk) "resolve" is the correct word. ~~~~ |
||
| Line 664: | Line 664: | ||
{{main|In-water recompression}} |
{{main|In-water recompression}} |
||
If a chamber is not available for recompression within a reasonable period, a riskier alternative is [[in-water recompression]] at the dive site.<ref name=Edmonds1998>{{cite journal |author=Edmonds, Carl |year=1998 |title=Underwater oxygen for treatment of decompression sickness: A review |journal=South Pacific Underwater Medicine Society Journal |volume=25 |issue=3 |issn=0813-1988 |oclc=16986801 |url=http://archive.rubicon-foundation.org/6428 |accessdate=2011-10-31}}</ref><ref name=Pyle1995>{{cite journal |last=Pyle |first=Richard L. |coauthors=Youngblood, David A |title=In-water Recompression as an emergency field treatment of decompression illness |journal=AquaCorp |volume=11 |year=1995 |url=http://archive.rubicon-foundation.org/6083 |accessdate=2008-06-08 }}</ref><ref name=uhms/> |
If a chamber is not available for recompression within a reasonable period, a riskier alternative is [[in-water recompression]] at the dive site.<ref name=Edmonds1998>{{cite journal |author=Edmonds, Carl |year=1998 |title=Underwater oxygen for treatment of decompression sickness: A review |journal=South Pacific Underwater Medicine Society Journal |volume=25 |issue=3 |issn=0813-1988 |oclc=16986801 |url=http://archive.rubicon-foundation.org/6428 |accessdate=2011-10-31}}</ref><ref name=Pyle1995>{{cite journal |last=Pyle |first=Richard L. |coauthors=Youngblood, David A |title=In-water Recompression as an emergency field treatment of decompression illness |journal=AquaCorp |volume=11 |year=1995 |url=http://archive.rubicon-foundation.org/6083 |accessdate=2008-06-08 }}</ref><ref name=uhms/> |
||
In-water recompression (IWR) is the emergency treatment of decompression sickness (DCS) by sending the diver back underwater to allow the gas bubbles in the tissues, which are causing the symptoms, to |
In-water recompression (IWR) is the emergency treatment of decompression sickness (DCS) by sending the diver back underwater to allow the gas bubbles in the tissues, which are causing the symptoms, to resolve. It is a risky procedure that should only be used when it is not practicable to travel to the nearest recompression chamber in time to save the victim's life.<ref name=Pyle1995/><ref name=uhms>{{cite book |last=Kay |first=E |coauthors=M. P. Spencer |title=In water recompression. 48th Undersea and Hyperbaric Medical Society Workshop |year=1999 |publisher=Undersea and Hyperbaric Medical Society |volume=UHMS Publication Number RC103.C3 |location=United States |pages=108 |url=http://archive.rubicon-foundation.org/5629 |accessdate=2008-06-08 }}</ref> |
||
The procedure is high risk as a diver suffering from DCS may become paralysed, unconscious or stop breathing whilst under water. Any one of these events may result in the diver drowning or further injury to the diver during a subsequent rescue to the surface. These risks can be mitigated to some extent by using a helmet or full-face mask with voice communications on the diver, and suspending the diver from the surface so that depth is positively controlled, and by having an in-water standby diver attend the diver undergoing the treatment at all times. |
The procedure is high risk as a diver suffering from DCS may become paralysed, unconscious or stop breathing whilst under water. Any one of these events may result in the diver drowning or further injury to the diver during a subsequent rescue to the surface. These risks can be mitigated to some extent by using a helmet or full-face mask with voice communications on the diver, and suspending the diver from the surface so that depth is positively controlled, and by having an in-water standby diver attend the diver undergoing the treatment at all times. |
||
Revision as of 00:43, 16 June 2012

Decompression in the context of diving derives from the reduction in ambient pressure experienced by the diver during the ascent at the end of a dive or hyperbaric exposure and refers to both the reduction in pressure and the process of allowing dissolved inert gases to be eliminated from the tissues during decompression.
When a diver descends in the water column the ambient pressure rises. Since breathing gas is supplied at the same ambient pressure as the surrounding water some of the gas dissolves in the diver's blood and other fluids. Invert gas continues to move into the diver until the gas dissolved in the diver is in a state of equilibrium with that being supplied to the diver (see: "Saturation diving") or begins to move out of the diver as a result of the diver moving up in the water column and thus reducing the ambient pressure of the divers breathing gas.
In a manner similar to the fizzing of carbonated beverage when opened, inert gases such as nitrogen or helium can form bubbles in the blood and tissues of the diver if the partial pressure of the gas in the diver gets too high when compared to the ambient pressure. These bubbles (and perhaps blood clots caused by the bubbles) can cause damage to tissues known as decompression sickness or the bends. The immediate goal of planned decompression is to avoid development of symptoms of bubble formation in the tissues of the diver, and the long term goal is to also avoid complications due to sub-clinical decompression injury.
The symptoms of decompression sickness are known to be caused by damage resulting from the formation and growth of bubbles of inert gas within the tissues and by blockage of arterial blood supply to tissues by gas bubbles and other emboli consequential to bubble formation and tissue damage.
The precise mechanisms of bubble formation and the damage they cause has been the subject of medical research for a considerable time and several hypotheses have been advanced and tested. Tables and algorithms for predicting the outcome of decompression schedules for specified hyperbaric exposures and have been proposed, tested and used, and usually found to be of some use but not entirely reliable. Decompression remains a procedure with some risk, but this has been reduced and is generally considered to be acceptable for dives within the well tested range of commercial, military and recreational diving.
Decompression may be continuous or staged (ascent interrupted by stops at regular depth intervals), but the entire ascent is part of the decompression, and ascent rate can be critical to successful elimination of inert gas. What is commonly known as no-decompression diving, or more accurately no-stop decompression, relies on limiting ascent rate for avoidance of excessive bubble formation.
During effective decompression, the venous microbubbles present after most dives are eliminated from the diver's body through the lungs. If they are not given enough time, or more bubbles are created than can be eliminated safely, the bubbles grow in size and number causing the symptoms and injuries of decompression sickness.[1]
When diving with nitrogen-based breathing gases, decompression stops are typically carried out in the 3 to 20 metres (10 to 70 ft) depth range. With helium-based breathing gases the stop depths may start deeper.
The period at surface pressure after dives is also an important part of decompression and can be thought of as the last decompression stop of a dive. It typically takes up to 24 hours for the body to return to its normal atmospheric levels of inert gas saturation after a dive.[2] When time is spent on the surface between dives this is known as the "surface interval" and is considered when calculating decompression requirements of the subsequent dive.
Divers breathing gas at high pressure may need to do decompression stops, but a diver who breathes gas at atmospheric pressure when free-diving, does not usually need to do decompression stops. However, it is possible to get taravana from repetitive deep free-diving with short surface intervals.[3]
Divers who use a snorkel to free-dive near the surface or use an atmospheric diving suit will not need to decompress.
Physics and physiology of decompression
Decompression involves a complex interaction of gas solubility, partial pressures and concentration gradients, bulk transport and bubble mechanics in living tissues.
This section provides an introductory discussion of some of the factors influencing inert gas uptake and elimination in living tissues.
Solubility
Solubility is the property of a gas, liquid or solid substance (the solute) to be held homogeneously dispersed as molecules or ions in a liquid or solid medium (the solvent).
In decompression theory the solubility of gases in liquids is of primary importance.
Solubility of gases in liquids is influenced by three main factors:
- The nature of the solvent liquid and the solute gas
- Temperature (gases are less soluble in water at higher temperatures, but may be more soluble in organic solvents)
- Pressure (solubility of a gas in a liquid is proportional to the partial pressure of the gas on the liquid - Henry's Law)
- The presence of other solutes in the solvent can also influence solubility.
| Gas | Molecular weight | Water solubility | Lipid solubility | Water/lipid solubility ratio |
|---|---|---|---|---|
| Hydrogen | 2 | 0.016 | 0.048 | 3.1 |
| Helium | 4 | 0.0085 | 0.015 | 1.7 |
| Neon | 20 | 0.0097 | 0.019 | 2.07 |
| Nitrogen | 28 | 0.013 | 0.067 | 5.2 |
| Oxygen | 32 | 0.024 | 0.12 | 5.0 |
| Carbon dioxide | 44 | 0.56 | 0.876 | 1.6 |
Diffusion
Diffusion is the movement of molecules or ions in a medium when there is no gross mass flow of the medium, and can occur in gases, liquids or solids, or any combination.
Diffusion is driven by the kinetic energy of the diffusing molecules - it is faster in gases and slower in solids when compared with liquids due to the variation in distance between collisions, and diffusion is faster when the temperature is higher as the average energy of the molecules is greater. Diffusion is also faster in smaller, lighter molecules of which helium is the extreme example. Diffusivity of Helium is 2.65 times faster than Nitrogen[5]
In decompression theory the diffusion of gases, particularly when dissolved in liquids, is of primary importance.
Partial pressure gradient
Also known as concentration gradient, this can be used as a model for the driving mechanism of diffusion. The partial pressure gradient is the variation of partial pressure (or more accurately, the concentration) of the solute (dissolved gas) from one point to another in the solvent. The solute molecules will randomly collide with the other molecules present, and tend over time to spread out until the distribution is statistically uniform. This has the effect that molecules will diffuse from regions of higher concentration (partial pressure) to regions of lower concentration, and the rate of diffusion is proportional to the rate of change of the concentration.
Molecules of solute will also tend to aggregate in areas of greater solubility in a non-homogenous solvent medium.
Inert gas uptake (Ingassing)


In this context, inert gas refers to a gas which is not metabolically active. Atmospheric nitrogen (N2) is the most common example. Helium (He) is the other inert gas commonly used in breathing mixtures for divers. Atmospheric nitrogen has a partial pressure of approximately 0.78bar. Air in the alveoli of the lungs is diluted by saturated water vapour (H2O) and carbon dioxide (CO2), given off by the blood as a metabolic product, and contains less oxygen (O2) as some of it is taken up by the blood for metabolic use, The resulting partial pressure of nitrogen is about 0,758bar.[6] At atmospheric pressure the body tissues are therefore normally saturated with nitrogen at 0.758bar (569mmHg). At increased ambient pressures due to depth or habitat pressurisation, a diver’s lungs are filled with breathing gas at the increased pressure.
For example: At 10 meters sea water (msw) the partial pressure of nitrogen in air will be 1.58 bar.
The inert gases from the breathing gas in the lungs diffuse into blood in the alveolar capillaries ("moves down the pressure gradient") and are distributed around the body by the systemic circulation in the process known as perfusion.
Perfusion
Perfusion is the mass flow of blood through the tissues. Dissolved materials are transported in the blood much faster than they would be distributed by diffusion alone (order of minutes compared to hours). The dissolved gas in the alveolar blood is transported to the body tissues by the blood circulation. There it diffuses through the cell walls into the tissues, where it will eventually reach equilibrium. The greater the blood supply to a tissue the faster it will reach equilibrium with gas at the new partial pressure.
Saturation and supersaturation
If the supply of gas to a solvent is unlimited, the gas will diffuse into the solvent until there is so much dissolved that the amount diffusing back out is equal to the amount diffusing in. This is called saturation.
If the external partial pressure of the gas (in the lungs) is then reduced, more gas will diffuse out than in. This is a condition known as supersaturation. The gas will not necessarily form bubbles in the solvent at this stage.
Tissue compartments
Most decompression models work with slow and fast tissue compartments. These are imaginary tissues which are designated as fast and slow to describe the rate of saturation. Real tissues will also take more or less time to saturate, but the models do not need to use actual tissue values to produce a useful result. Models with from one to 16 tissue compartments[7] have been used to generate decompression tables.
For example: Tissues with a high lipid content take up a larger amount of nitrogen, but often have a poor blood supply. These will take longer to reach equilibrium, and are described as slow, than tissues with a good blood supply and less capacity for dissolved gas, which are described as fast.
Tissue half times
Half time of a tissue is the time it takes for the tissue to become 50% saturated at a new partial pressure. For each consecutive half time the tissue will become half again saturated in the sequence ½, ¾, 7/8, 15/16, 31/32, 63/64 etc. The number of half times chosen to assume full saturation depends on the decompression model, and typically ranges from 4 (93.75%) to 6 (98.44%).
For example: A 5 minute tissue will be 50% saturated in 5 minutes, 75% in 10 minutes, 87.5% in 15 minutes and for practical purposes, saturated in about 30 minutes (98.44% saturated at 6 half times)
Tissue compartment half times range from 1 minute to 720 minutes[8] or more in current decompression models.
Saturated tissues
Gas remains in the tissue in dissolved form until the partial pressure of that gas in the lungs is reduced. A lower partial pressure in the lungs will result in more gas diffusing out into the lungs and less into the blood. As the pressure reduces, the diffusion will reach a state where more gas diffuses into the lungs than into the blood.

Inherent unsaturation
There is a metabolic reduction of total gas pressure in the tissues.[9]
The sum of partial pressures of the gas that the diver breathes must necessarily balance with the sum of partial pressures in the lung gas. In the alveoli the gas has been humidified by a partial pressure of approximately 63 mbar (47 mmHg) and has gained about 55 mbar (41 mmHg) carbon dioxide from the venous blood. Oxygen has also diffused into the arterial blood, reducing the partial pressure of oxygen in the alveoli by about 67 mbar(50 mmHg) As the total pressure in the alveoli must balance with the ambient pressure, this dilution results in an effective partial pressure of nitrogen of about 758 mb (569 mmHg) in air at normal atmospheric pressure.
At a steady state, when the tissues have been saturated by the inert gases of the breathing mixture, metabolic processes reduce the partial pressure of the less soluble oxygen and replace it with carbon dioxide, which is considerably more soluble in water. In the cells of a typical tissue, the partial pressure of oxygen will drop to around 13 mbar (10 mmHg), while the partial pressure of carbon dioxide will be about 65 mbar (49 mmHg). The sum of these partial pressures (water, oxygen, carbon dioxide and nitrogen) comes to roughly 900 mbar (675 mmHg), which is some 113 mbar (85 mmHg) less than the total pressure of the respiratory gas. This is a significant saturation deficit, and it provides a buffer against supersaturation and a driving force for dissolving bubbles.[9]
Experiments suggest that the degree of unsaturation increases linearly with pressure for a breathing mixture of fixed composition, and decreases linearily with fraction of inert gas in the breathing mixture.[10] As a consequence, the conditions for maximising the degree of unsaturation are a breathing gas with the lowest possible fraction of inert gas - i.e. pure oxygen, at the maximum permissible partial pressure.
This saturation deficit is also referred to as the "Oxygen window".[11] or partial pressure vacancy.[12]
Supersaturated tissues
When the gas in a tissue is at a concentration where more diffuses out then in it is called supersaturated and starts degassing: dissolved gas diffuses into the bloodstream and out of the system via the lungs.
Some authorities define supersturation in this context as when the partial pressure of inert gas dissolved in a tissue exceeds the total ambient pressure on the tissue[13]
If the ambient pressure is too low, bubbles may form in the tissues.
Inert gas elimination (Outgassing)
For optimised decompression the driving force for tissue desaturation should be kept at a maximum, provided that this does not cause symptomatic tissue injury due to bubble formation and growth (symptomatic decompression sickness), or produce a condition where diffusion is retarded for any reason.
There are two fundamentally different ways this has been approached. The first is based on an assumption that there is a level of supersaturation which does not produce symptomatic bubble formation and is based on empirical observations of the maximum decompression rate which does not result in an unacceptable rate of symptoms. This approach seeks to maximise the concentration gradient providing there are no symptoms. The second assumes that bubbles will form at any level of supersaturation where the total gas tension in the tissue is greater than the ambient pressure and that gas in bubbles is eliminated more slowly than dissolved gas. These philosophies result in differing characteristics of the decompression profiles derived for the two models: The critical supersaturation approach gives relatively rapid initial ascents, which maximise the concentration gradient, and long shallow stops, while the bubble models require slower ascents, with deeper first stops, but may have shorter shallow stops.
The critical supersaturation approach
Critical ratio model
J.S. Haldane originally used a pressure ratio of 2 to 1 for decompression on the principle that the saturation of the body should at no time be allowed to exceed about double the air pressure.[14] This principle was applied as a pressure ratio of total ambient pressure and did not take into account the partial pressures of the component gases of the breathing air. His experimental work on goats and observations of human divers appeared to support this assumption. However, in time, this was found to be inconsistent with incidence of decompression sickness and changes were made to the initial assumptions. This was later changed to a 1.58:1 ratio of nitrogen partial pressures.
Critical difference models
Further research by people such as Robert Workman suggested that the criterion was not the ratio of pressures, but the actual pressure differentials. Applied to Haldane's work, this would suggest that the limit is not determined by the 1.58:1 ratio but rather by the difference of 0.58 atmospheres between tissue pressure and ambient pressure. Most tables today, including the Buhlmann tables, are based on the critical difference model.[15]
M-values
At a given ambient pressure, the M-value is the maximum value of absolute inert gas pressure that a tissue compartment can take without presenting symptoms of decompression sickness. M-values are limits for the tolerated gradient between inert gas pressure and ambient pressure in each compartment. Alternative terminology for M-values include "supersaturation limits", "limits for tolerated overpressure", and "critical tensions".[16][17]
Gradient factors
Gradient factors are a way of modifying the M-value to a more conservative value for use in a decompression algorithm. The gradient factor is a percentage of the M-value chosen by the algorithm designer, and varies linearly between the maximum depth and the surface. They are expressed as a two number designation, where the first number is the percentage of the deep M-value, and the second is a percentage of the shallow M-value.[18]
For example: A 30/85 gradient factor would limit the allowed supersaturation at depth to 30% of the designer's maximum, and to 85% at the surface.
In effect the user is selecting a lower maximum supersaturation than the designer considered appropriate. Use of gradient factors will increase decompression time, particularly in the depth zone where the M-value is reduced the most. Gradient factors may be used to force deeper stops in a model which would otherwise tend to produce relatively shallow stops, by using a gradient factor with a small first number.
Gradient factors produce an M-value which is linearly variable in proportion to ambient pressure.
The critical volume approach
The critical-volume criterion assumes that whenever the total volume of gas phase accumulated in the tissues exceeds a critical value, signs or symptoms of DCS will appear. This assumption is supported by doppler bubble detection surveys. The consequences of this approach depend strongly on the bubble formation and growth model used, primarily whether bubble formation is practicably avoidable during decompression.
This approach is used in decompression models that assume that during practical decompression profiles, there will be growth of stable microscopic bubble nuclei which always exist in aqueous media, including living tissues.
Efficient decompression will minimise the total ascent time while limiting the total accumulation of bubbles to an acceptable non-symptomatic critical value. The physics and physiology of bubble growth and elimination indicate that it is more efficient to eliminate bubbles while they are very small. Models which include bubble phase have produced decompression profiles with slower ascents and deeper initial decompression stops as a way of curtailing bubble growth and facilitating early elimination, in comparison with the models which consider only dissolved phase gas.
The no-supersaturation approach
According to the thermodynamic model of LeMessurier and Hills,[19] this condition of optimum driving force for outgassing is satisfied when the hydrostatic pressure is just sufficient to prevent phase separation (bubble formation).
The fundamental difference of this approach is equating absolute ambient pressure with the total of the partial gas tensions in the tissue for each gas after decompression as the limiting point beyond which bubble formation is expected.
The model assumes that the natural unsaturation in the tissues due to metabolic reduction in oxygen partial pressure provides the buffer against bubble formation, and that the tissue may be safely decompressed provided that the reduction in ambient pressure does not exceed this unsaturation value. Clearly any method which increases the unsaturation would allow faster decompression, as the concentration gradient would be greater without risk of bubble formation.
The natural unsaturation increases with depth, so a larger ambient pressure differential is possible at greater depth, and reduces as the diver surfaces. This model leads to slower ascent rates and deeper first stops, but shorter shallow stops, as there is less bubble phase gas to be eliminated.
Bubble formation, growth and elimination
Bubble mechanics
Equilibrium of forces on the surface is required for a bubble to exist. These are:
- Ambient pressure, exerted on the outside of the surface, acting inwards
- Pressure due to tissue distortion, also on the outside and acting inwards
- Surface tension of the liquid at the interface between the bubble and the surroundings. This is along the surface of the bubble, so the resultant acts towards the centre of curvature. This will tend to squeeze the bubble, and is more severe for small bubbles as it is an inverse function of the radius.
- The resulting forces must be balanced by the pressure on the inside of the bubble. This is the sum of the partial pressures of the gases inside due to the net diffusion of gas to and from the bubble.
- The force balance in the bubble may be modified by a layer of surface active molecules which can stabilise a microbubble at a size where surface tension on a a clean bubble would cause it to collapse rapidly.[20]
- This surface layer may vary in permeability, so that if the bubble is compressed it may become impermeable to diffusion at sufficient compression.[20]
If the solvent outside the bubble is saturated or unsaturated, the partial pressure will be less than in the bubble, and the surface tension will be increasing the internal pressure in direct proportion to surface curvature, providing a pressure gradient to increase diffusion out of the bubble, effectively "squeezing the gas out of the bubble", and the smaller the bubble the faster it will get squeezed out. A gas bubble can only grow at constant pressure if the surrounding solvent is sufficiently supersaturated to overcome the surface tension or if the surface layer provides sufficient reaction to overcome surface tension.[20]
Clean bubbles that are sufficiently small will collapse due to surface tension if the supersaturation is low. Bubbles with semipermeable surfaces will either stabilise at a specific radius depending on the pressure, the composition of the surface layer, and the supersaturation, or continue to grow indefinitely, if larger than the critical radius.[21]
Bubble nucleation
Bubble formation occurs in the blood or other tissues, possibly in crevices in macromolecules.[22]
A solvent can carry a supersaturated load of gas in solution. Whether it will come out of solution in the bulk of the solvent to form bubbles will depend on a number of factors. Something which reduces surface tension, or adsorbs gas molecules, or locally reduces solubility of the gas or causes a local reduction in static pressure in a fluid may result in a bubble nucleation or growth. This may include velocity changes and turbulence in fluids and local tensile loads in solids and semi-solids. Lipids and other hydrophobic surfaces may reduce surface tension (blood vessel walls may have this effect) Dehydration may reduce gas solubility in a tissue due to higher concentration of other solutes, and less solvent to hold the gas.
Another theory presumes that microscopic bubble nuclei always exist in aqueous media, including living tissues. These bubble nuclei are spherical gas phases that are small enough to remain in suspension yet strong enough to resist collapse, their stability being provided by an elastic surface layer consisting of surface-active molecules which resists the effect of surface tension.[23]
Bubble growth
Once a micro-bubble forms it may continue to grow if the tissues are still supersaturated. As the bubble grows it may distort the surrounding tissue and cause damage to cells and pressure on nerves resulting in pain.
If a bubble or an object exists which collects gas molecules this may reach a size where the internal pressure exceeds the combined surface tension and external pressure and the bubble will grow.
If the solvent is sufficiently supersaturated, the diffusion of gas into the bubble will exceed the rate at which it diffuses back into solution. If this excess pressure is greater than the pressure due to surface tension the bubble will grow. When a bubble grows, the surface tension decreases, and the interior pressure drops, allowing gas to diffuse in faster, and diffuse out slower, so the bubble grows or shrinks in a positive feedback situation. The growth rate is reduced as the bubble grows by the fact that the surface area increases as the square of the radius, while the volume increases as the cube of the radius. If the external pressure is reduced (due to reduced hydrostatic pressure during ascent, for example) the bubble will also grow.
The VPM ordering hypothesis says that nuclei are neither created nor totally eliminated during the pressure cycle, and the initial ordering according to size is preserved. therefore each bubble count is determined by the properties and behavior of a nominal "critical" nucleus which is at the threshold of bubble-formation - all larger nuclei will form bubbles, and all smaller nuclei will not.[20]
Bubble distribution
Decompression bubbles appear to form mostly in the capillaries where the gas concentration is highest, often those feeding the veins draining the active limbs. They do not generally form in the arteries, as arterial blood has recently had the opportunity to release excess gas into the lungs. The bubbles carried back to the heart in the veins may be transferred to the systemic circulation via a patent foramen ovale in divers with this septal defect, after which there is a risk of occlusion of capillaries in whichever part of the body they end up in.
Bubbles are also known to form within other tissues, where they may cause damage leading to symptoms of decompression sickness. This damage is likely to be caused by mechanical deformation and stresses on the cells rather than local hypoxia, which is the assumed mechanism in the case of gas embolism of the capillaries.
Bubble elimination
Bubbles which are carried back to the heart in the veins will normally find their way to the right side of the heart, and from there they will normally enter the pulmonary circulation and eventually pass through or be trapped in the capillaries of the lungs, which are around the alveoli and very near to the respiratory gas, where the gas will diffuse from the bubbles though the capillary and alveolar walls into the gas in the lung. If the number of lung capillaries blocked by these bubbles is relatively small, the diver will not display symptoms, and no tissue will be damaged (lung tissues are adequately oxygenated by diffusion).
The bubbles which are small enough to pass through the lung capillaries may be small enough to be dissolved due to a combination of surface tension and diffusion to a lowered concentration in the surrounding blood, though the Varying Permeability Model nucleation theory implies that most bubbles passing through the pulmonary circulation will lose enough gas to pass through the capillaries and return to the systemic circulation as recycled but stable nuclei.[24]
Bubbles which form within the tissues must be eliminated in situ by diffusion, which implies a suitable pressure gradient.
Isobaric counterdiffusion (ICD)
Isobaric counterdiffusion is the diffusion of gases in opposite directions caused by a change in the composition of the external ambient gas or breathing gas without change in the ambient pressure. During decompression after a dive this can occur when a change is made to the breathing gas, or when the diver moves into a gas filled environment which differs from the breathing gas.
While not strictly speaking a phenomenon of decompression, it is a complication that can occur during decompression, and that can result in the formation or growth of bubbles without changes in the environmental pressure. Two forms of this phenomenon have been described by Lambertsen:[25][26]
Superficial ICD
Superficial ICD (also known as Steady State Isobaric Counterdiffusion[27]) occurs when the inert gas breathed by the diver diffuses more slowly into the body than the inert gas surrounding the body.[25][26][27]
An example of this would be breathing air in an heliox environment. The helium in the heliox diffuses into the skin quickly, while the nitrogen diffuses more slowly from the capillaries to the skin and out of the body. The resulting effect generates supersaturation in certain sites of the superficial tissues and the formation of inert gas bubbles.
Deep Tissue ICD
Deep Tissue ICD (also known as Transient Isobaric Counterdiffusion[27]) occurs when different inert gases are breathed by the diver in sequence.[25][26] The rapidly diffusing gas is transported into the tissue faster than the slower diffusing gas is transported out of the tissue.
This can occur as divers switch from a nitrogen mixture to a helium mixture (diffusivity of helium is 2.65 times faster than nitrogen), or when saturation divers breathing hydreliox switch to a heliox mixture.[citation needed]
There is another effect which can manifest as a result of the disparity in solubility between inert breathing gas diluents, which occurs in isobaric gas switches near the decompression ceiling between a low solubility gas (typically helium, and a higher solubility gas, typically nitrogen)
An inner ear decompression model by Doolette and Mitchell[28] suggests that a transient increase in gas tension after a switch from helium to nitrogen in breathing gas may result from the difference in gas transfer between compartments. If the transport of nitrogen into the vascular compartment by perfusion exceeds removal of helium by perfusion, while transfer of helium into the vascular compartment by diffusion from the perilymph and endolymph exceeds the counterdiffusion of nitrogen, this may result in a temporary increase in total gas tension, as the input of nitrogen exceeds the removal of helium, which can result in bubble formation and growth. This model suggests that diffusion of gases from the middle ear across the round window is negligible. The model is not necessarily applicable to all tissue types.
ICD Prevention
Lambertsen made suggestions to help avoid ICD while diving:[25][26]
- If the diver is surrounded by or saturated with nitrogen, they should not breathe helium rich gases.
- Gas switches that involve going from helium rich mixtures to nitrogen rich mixtures would be acceptable, but changes from nitrogen to helium should include recompression.
However Doolette and Mitchell's more recent study of Inner Ear Decompression Sickness (IEDCS) shows that the inner ear may not be well-modelled by common (e.g. Bühlmann) algorithms. Doolette and Mitchell propose that a switch from a helium-rich mix to a nitrogen-rich mix, as is common in technical diving when switching from trimix to nitrox on ascent, may cause a transient supersaturation of inert gas within the inner ear and result in IEDCS. They suggest that:[28]
- Breathing-gas switches from helium-rich to nitrogen-rich mixtures should be carefully scheduled either deep (with due consideration to nitrogen narcosis) or shallow to avoid the period of maximum supersaturation resulting from the decompression. Switches should also be made during breathing of the largest inspired oxygen partial pressure that can be safely tolerated with due consideration to oxygen toxicity.
A similar hypothesis to explain the incidence of IEDCS when switching from trimix to nitrox was proposed by Steve Burton, who considered the effect of the much greater solubility of nitrogen than helium in producing transient increases in total inert gas pressure, which could lead to DCS under isobaric conditions.[29]
Burton argues that effect of switching to Nitrox from Trimix with a large increase of nitrogen fraction at constant pressure has the effect of increasing the overall gas loading within particularly the faster tissues, since the loss of helium is more than compensated by the increase in nitrogen. This could cause immediate bubble formation and growth in the fast tissues. A simple rule for avoidance of ICD when gas switching at a decompression ceiling is suggested:
- Any increase in gas fraction of nitrogen in the decompression gas should be limited to 1/5 of the decrease in gas fraction of helium.[29]
This rule has been found to successfully avoid ICD on hundreds of deep trimix dives.[29]
Doppler ultrasonic bubble detection
Doppler bubble detection equipment uses ultrasonic signals reflected from bubble surfaces to identify and quantify gas bubbles present in venous blood. This method was used by Dr Merrill Spencer of the Institute of Applied Physiology and Medicine in Seattle, who published a report in 1976 recommending that the then current no-decompression limits be reduced on the basis that large counts of venous gas bubbles were detected in divers exposed to the US Navy no-decompression limits. These non-symptomatic bubbles have become known as "silent bubbles", and are thought to be nitrogen bubbles released from solution during ascent.[30]
Decompression sickness and injuries
Problems due to vascular decompression bubbles
Bubbles may be trapped in the lung capillaries, temporarily blocking them. If this is severe, the symptom called "chokes" may occur.[31]
If the diver has a patent foramen ovale (or a shunt in the pulmonary circulation), bubbles may pass through it and bypass the pulmonary circulation to enter the arterial blood. If these bubbles are not absorbed in the arterial plasma and lodge in systemic capillaries they will block the flow of oxygenated blood to the tissues supplied by those capillaries, and those tissues will be starved of oxygen. Moon and Kisslo concluded that "the evidence suggests that the risk of serious neurological DCI or early onset DCI is increased in divers with a resting right-to-left shunt through a PFO. There is, at present, no evidence that PFO is related to mild or late onset bends."[32]
Extravascular bubbles
Bubbles form within other tissues as well as the blood vessels.[31] Inert gas can diffuse into bubble nuclei between tissues. In this case, the bubbles can distort and permanently damage the tissue. As they grow, the bubbles may also compress nerves as they grow causing pain.
Extravascular bubbles usually form in slow tissues such as joints, tendons and muscle sheaths. Direct expansion causes tissue damage, with the release of histamines and their associated affects. Biochemical damage may be as important as, or more important than mechanical effects.[31]
Factors influencing uptake and elimination of dissolved gases and decompression risk
The exchange of dissolved gases between the blood and tissues is controlled by perfusion and to a lesser extent by diffusion, particularly in heterogenous tissues. The distribution of blood flow to the tissues is variable and subject to a variety of influences. When the flow is locally high, that area is dominated by perfusion, and by diffusion when the flow is low. The distribution of flow is controlled by the mean arterial pressure and the local vascular resistance, and the arterial pressure depends on cardiac output and the total vascular resistance. Basic vascular resistance is controlled by the sympathetic nervous system, and metabolites, temperature, and local and systemic hormones have secondary and often localised effects, which can vary considerably with circumstances. Peripheral vasoconstriction in cold water decreases heat loss without increasing oxygen consumption until shivering begins, at which point oxygen consumption will rise, though the vasoconstriction can persist.[31]
Breathing gas composition
The composition of the breathing gas during pressure exposure and decompression is the most significant factor in inert gas uptake and elimination for a given pressure exposure profile, for two main reasons:
Gas fraction and partial pressure of the component inert gas
Breathing gas mixtures for diving will typically have a different gas fraction of nitrogen to that of air. The partial pressure of each component gas will differ to that of nirogen in air at any given depth, and uptake and elimination of each inert gas component is proportional to the actual partial pressure over time. The two foremost reasons for use of mixed breathing gases are the reduction of nitrogen partial pressure by dilution with oxygen, to make Nitrox mixtures, primarily to reduce the rate of nitrogen uptake during pressure exposure, and the substitution of helium (and occasionally other gases) for the nitrogen to reduce the narcotic effects under high partial pressure exposure. Depending on the proportions of helium and nitrogen, these gases are called Heliox, if there is no nitrogen, or Trimix, if there is nitrogen and helium along with the essential oxygen.
Solubility characteristics of the inert gases in the mixture
The inert gases used as substitutes for nitrogen have different solubility and diffusion characteristics in living tissues to the nitrogen they replace. For example, the most common inert gas diluent substitute for nitrogen is helium, which is significantly less soluble[33] in living tissue, but also diffuses faster[34] due to the relatively small size and mass of the He atom in comparison with the N2 molecule.
Body temperature and exercise
Blood flow to skin and fat are affected by skin and core temperature, and resting muscle perfusion is controlled by the temperature of the muscle itself. During exercise increased flow to the working muscles is often balanced by reduced flow to other tissues, such as kidneys spleen and liver.
Blood flow to the muscles is lower in cold water, but exercise keeps the muscle warm and flow elevated even when the skin is chilled. Blood flow to fat normally increases during exercise, but this is inhibited by immersion in cold water. Adaptation to cold reduces the extreme vasoconstiction which usually occurs with cold water immersion.
Variations in perfusion distribution do not necessarily affect respiratory inert gas exchange, though some gas may be locally trapped by changes in perfusion. Rest in a cold environment will reduce inert gas exchange from skin, fat and muscle, whereas exercise will increase gas exchange. Exercise during decompression can reduce decompression time and risk, providing bubbles are not present, but can increase risk if bubbles are present.
Inert gas exchange is least favourable for the diver who is warm and exercises at depth during the ingassing phase, and rests and is cold during decompression.[31]
Other factors
Other factors which can affect decompression risk include oxygen concentration, carbon dioxide levels, body position, vasodilators and constrictors, positive or negative pressure breathing.[31] and dehydration (blood volume).[35]
Personal factors
Individual susceptibility to decompression sickness has components which can be attributed to a specific cause, and components which appear to be random. The random component makes successive decompressions a poor test of susceptibility.[31] Obesity and high serum lipid levels have been implicated as risk factors, and risk seems to increase with age. Other factors, such as gender and previous injury provide inconsistent results.
A more recent study has shown that older subjects tended to bubble more than younger subjects for reasons not yet known. No trends between weight, body fat, or gender and bubbles were identified, and the question of why some people are more likely to form bubbles than others remains unclear.[36]
Decompression models
A fundamental problem in the design of decompression tables is that the rules that govern a single dive and ascent do not apply when some tissue bubbles already exist, as these will delay inert gas elimination and equivalent decompression may result in decompression sickness.[37]
One attempt at a solution was the development of multi-tissue models, which assumed that different parts of the body absorbed gas at different rates. Each tissue, or compartment, has a different half-life. Fast tissues absorb gas relatively quickly, but will release it quickly during ascent. A fast tissue may become saturated in the course of a normal sports dive, while a slow tissue may hardly have absorbed any gas. By calculating the levels in each compartment separately, researchers are able to construct better tables. In addition, each compartment may be able to tolerate more or less supersaturation than others. The final form is a complicated model, but one that allows for the construction of tables suited to a wide variety of diving. A typical dive computer has a 8-12 tissue model, with half times varying from 5 minutes to 400 minutes.[citation needed] The Bühlmann tables have 16 tissues, with half times varying from 4 minutes to 640 minutes.[7]
The ideal decompression profile creates the greatest possible gradient for inert gas elimination from a tissue without causing bubbles to form,[38] but it is not certain whether this is practically possible: some of the decompression models assume that stable bubble micronuclei always exist.[23] However, the dissolved phase decompression models are based on the assumption that bubble formation can be avoided. The bubble models make the assumption that there will be bubbles, but there is a tolerable total gas phase volume[23] or a tolerable gas bubble size,[39] and limit the maximum gradient to take these tolerances into account. A number of empirical modifications to dissolved phase models have been made since the identification of venous bubbles by doppler measurement in asymptomatic divers soon after surfacing.
Repetitive diving, multiple ascents within a single dive, and surface decompression procedures are significant risk factors for DCS.[38]
Validation of models
It is important that any theory be validated by carefully controlled testing procedures. As testing procedures and equipment become more sophisticated, researchers learn more about the effects of decompression on the body. Initial research focused on producing dives that were free of recognizable symptoms decompression sickness (DCS). With the later use of Doppler ultrasound testing, it was realized that bubbles were forming within the body even on dives where no DCI signs or symptoms were encountered. This phenomenon has become known as "silent bubbles". The US Navy 1956 tables were based on limits determined by external DCS signs and symptoms. Later researchers were able to improve on this work by adjusting the limitations based on Doppler testing. However the US Navy CCR tables based on the Thalmann algorithm also used only recognisable DCS symptoms as the test criteria.[40][41]
Since the testing procedures are lengthy and costly, it is common practice for researchers to make initial validations of new models based on experimental results from earlier trials. This has some implications when comparing models.
Residual inert gas
Gas bubble formation has been experimentally shown to significantly inhibit inert gas elimination.[6][42]
A considerable amount of inert gas will remain in the tissues after a diver has surfaced. This residual gas may be dissolved or in sub-clinical bubble form, and will continue to outgas while the diver remains at the surface. If a repetitive dive is made, the tissues are preloaded with this residual gas which will make them saturate faster.
In repetitive diving, the slower tissues can accumulate gas day after day. This can be a problem for multi-day multi-dive situations. Multiple decompressions per day over multiple days can increase the risk of decompression sickness because of the build up of asymptomatic bubbles, which reduce the rate of off-gassing and are not accounted for in most decompression algorithms.[43] Consequently, some diver training organisations make extra recommendations such as taking "the seventh day off".[44]
Deterministic models
Deterministic decompression models are a rule based approach to calculating decompression.[45] These models work from the idea that "excessive" supersaturation in various tissues is "unsafe" (resulting in decompression sickness). The models usually contain multiple depth and tissue dependent rules based on mathematical models of idealised tissue compartments. There is no objective mathematical way of evaluating the rules or overall risk other than comparison with empirical test results. The models are compared with experimental results and reports from the field, and rules are revised by qualitative judgment and curve fitting so that the revised model more closely predicts observed reality, and then further observations are made to assess the reliability of the model in extrapolations into previously untested ranges. The usefulness of the model is judged on its accuracy and reliability in predicting the onset of symptomatic decompression sickness and asymptomatic venous bubbles during ascent.
It may be reasonably assumed that in reality, both perfusion transport by blood circulation, and diffusion transport in tissues where there is little or no blood flow occur. The problem with attempts to simultaneously model perfusion and diffusion is that there are large numbers of variables due to interactions between all of the tissue compartments and the problem becomes intractable.
A way of simplifying the modelling of gas transfer into and out of tissues is to make assumptions about the limiting mechanism of dissolved gas transport to the tissues which control decompression. Assuming that either perfusion or diffusion has a dominant influence, and the other can be disregarded, can greatly reduce the number of variables.
Perfusion limited tissues and parallel tissue models

The assumption that perfusion is the limiting mechanism leads to a model comprising a group of tissues with varied rates of perfusion, but supplied by blood of approximately equivalent gas concentration. It is also assumed that there is no gas transfer between tissue compartments by diffusion. This results in a parallel set of independent tissues, each with its own rate of ingassing and outgassing dependent on the rate of blood flowing through the tissue. Gas uptake for each tissue is generally modelled as an exponential function, with a fixed compartment half-time, and gas elimination may also be modelled by an exponential function, with the same or a longer half time, or as a more complex function, as in the exponential-linear elimination model.
Critical ratio hypothesis
This hypothesis predicts that the development of bubbles will occur in a tissue when the ratio of dissolved gas partial pressure to ambient pressure exceeds a particular ratio for a given tissue. The ratio may be the same for all tissue compartments or it may vary, and each compartment is allocated a specific critical supersaturation ratio, based on experimental observations.
John Scott Haldane
Haldane introduced the concept of half times to model the uptake and release of nitrogen into the blood. He suggested 5 tissue compartments with half times of 5, 10, 20, 40 and 75 minutes.
In this early hypothesis (Haldane 1908)[14] it was predicted that if the ascent rate does not allow the inert gas partial pressure in each of the hypothetical tissues to exceed the environmental pressure by more than 2:1 bubbles will not form.
Basically this meant that one could ascend from 30 m (4 bar) to 10 m (2 bar), or from 10 m (2 bar) to the surface when saturated, without a decompression problem.
To ensure this a number of decompression stops were incorporated into the ascent schedules.
The ascent rate and the fastest tissue in the model determine the time and depth of the first stop. Thereafter the slower tissues determine when it is safe to ascend further.
This 2:1 ratio was found to be too conservative for fast tissues (short dives) and not conservative enough for slow tissues (long dives). The ratio also seemed to vary with depth.
The ascent rates used on older tables were 18 m/min, but newer tables use 9 m/min.
Critical pressure hypothesis
Robert D. Workman
Haldane's approach to decompression modeling was used from 1908 to the 1960s with minor modifications, primarily changes to the number of compartments and half times used. The 1937 US Navy tables were based on research by O. D. Yarborough and used 3 compartments. The 5 and 10 min compartments were dropped. In the 1950s the tables were revised and the 5 and 10 minute compartments restored, and a 120 minute compartment added.
In the 1960s Robert D. Workman of the U.S. Navy Experimental Diving Unit (NEDU) undertook a review of the basis of the model and subsequent research performed by the US Navy. Tables based on Haldane’s work and subsequent refinements were observed to still be inadequate for longer and deeper dives.
Workman revised Haldane’s model to allow each tissue compartment to tolerate a different amount of supersaturation which varies with depth. He introduced the term "M-value" to indicate the maximum amount of supersaturation each compartment could tolerate at a given depth and added three additional compartments with 160, 200 and 240 minute half times.
Workman presented his findings as an equation which could be used to calculate the results for any depth and stated that a linear projection of M-values would be useful for computer programming.
Albert A. Bühlmann
A large part of Bühlmann’s research was to determine the longest half time compartments for Nitrogen and Helium, and he increased the number of compartments to 16. He investigated the implications of decompression after diving at altitude and published decompression tables that could be used at a range of altitudes. Bühlmann used a method for decompression calculation similar to that proposed by Workman, which included M-values expressing a linear relationship between maximum inert gas pressure in the tissue compartments and ambient pressure, but based on absolute pressure, which made them more easily adapted for altitude diving.
Bühlmann’s algorithm was used to generate the standard decompression tables for a number of sports diving associations, and are used in several personal decompression computers, sometimes in a modified form.
Thermodynamic model and deep stops
Torres Strait pearl divers
B.A. Hills and D.H. LeMessurier studied the empirical decompression practices of Okinawan pearl divers in the Torres Strait and observed that they made deeper stops but reduced the total decompression time compared with the generally used tables of the time. Their analysis strongly suggested that bubble presence limits gas elimination rates, and emphasised the importance of inherent unsaturation of tissues due to metabolic processing of oxygen.[19]
Pyle stops
A "Pyle stop" is an additional brief deep-water stop, which is increasingly used in deep diving (named after Richard Pyle, an early advocate of deep stops).[46] Typically, a Pyle stop is 2 minutes long and at the depth where the pressure change halves on an ascent between the bottom and the first conventional decompression stop.
For example, a diver ascends from a maximum depth of 60 metres (200 ft), where the ambient pressure is 7 bars (100 psi), to a decompression stop at 20 metres (66 ft), where the pressure is 3 bars (40 psi). The Pyle stop would take place at the halfway pressure, which is 5 bars (70 psi) corresponding to a depth of 40 metres (130 ft).[47][48]
Pyle found that on dives where he stopped periodically to vent the swim-bladders of his fish specimens, he felt better after the dive, and based the deep stop procedure on the depths and duration of these pauses. The hypothesis is that these stops provide an opportunity to eliminate gas while still dissolved, or at least while the bubbles are still small enough to be easily eliminated, and the result is that there will be considerably fewer or smaller venous bubbles to eliminate at the shallower stops as predicted by the thermodynamic model of Hills.
Diffusion limited tissues and the "Tissue slab" and series models

The assumption that diffusion is the limiting mechanism of dissolved gas transport in the tissues results in a rather different tissue compartment model. In this case a series of compartments has been postulated, with perfusion transport into one compartment, and diffusion between the compartments, which for simplicity are arranged in series, so that for the generalised compartment, diffusion is to and from only the two adjacent compartments on opposite sides, and the limit cases are the first compartment where the gas is supplied and removed via perfusion, and the end of the line, where there is only one neighbouring compartment.
The simplest series model is a single compartment, and this can be further reduced to a one dimensional "tissue slab" model.
Bubble models
Bubble decompression models are a rule based approach to calculating decompression. These models work from the idea that microscopic bubble nuclei always exist in water and tissues that contain water and that by predicting and controlling the bubble growth, one can avoid decompression sickness.
Probabilistic models
Probabilistic decompression models are designed to calculate the risk (or probability) of decompression sickness (DCS) occurring on a given decompression profile.[45] These models can vary the decompression stop depths and times to arrive at a final decompression schedule that assumes a specified probability of DCS occurring. The model does this while minimizing the total decompression time. This process can also work in reverse allowing one to calculate the probability of DCS for any decompression schedule.
Planning and monitoring decompression
Decompression algorithms

A decompression algorithm is used to calculate the decompression stops needed for a particular dive profile to reduce the risk of decompression sickness occurring after surfacing at the end of a dive. The algorithm can be used to generate decompression schedules for a particular dive profile, decompression tables for more general use, or be implemented in dive computer software.
No decompression limit
The no decompression limit (NDL) or no stop time, is the interval that a diver may theoretically spend at a given depth without having to perform decompression stops.[49] The NDL helps divers plan dives so that they can stay at a given depth and ascend without stopping while avoiding significant risk of decompression sickness.
The NDL is a theoretical time obtained by calculating inert gas uptake and release in the body, using a model such as the Bühlmann decompression algorithm.[49] Although the science of calculating these limits has been refined over the last century, there is still much that is unknown about how inert gas enter and leave the human body. In addition, every individual's body is unique and may absorb and release inert gases at different rates. For this reason, dive tables typically have a degree of safety built into their recommendations. Divers can and do suffer decompression sickness while remaining inside NDLs.[49]
Each NDL for a range of depths is printed on dive tables in a grid that can be used to plan dives.[49] There are many different tables available as well as software programs and calculators, which will calculate no decompression limits. Most personal decompression computers (dive computers) will indicate a remaining no decompression limit at the current depth during a dive. The displayed interval is continuously revised to take into account changes of depth as well as elapsed time.
Surface interval
The surface interval (SI) or surface interval time (SIT) is the time spent by a diver at surface pressure after a dive during which inert gas which was still present at the end of the dive is further eliminated from the tissues. This continues until the tissues are at equilibrium with the surface pressures. This may take several hours. In the case of the US Navy 1956 Air tables, it is considered complete after 12 hours,[50] The US Navy 2008 Air tables specify up to 16 hours for normal exposure.[51] but other algorithms may require more than 24 hours to assume full equilibrium.
Repetitive dives
Any dive which is done while the tissues retain residual inert gas is considered a repetitive dive. This means that the decompression required for the dive is influenced by the divers decompression history. Allowance must be made for inert gas preloading of the tissues which will result in them containing more dissolved gas than would have been the case if the diver has fully equalized before the dive. The diver will need to decompress longer to eliminate this increased gas loading.
Residual nitrogen time
For the planned depth of the repetitive dive, a bottom time can be calculated using the relevant algorithm which will provide an equivalent gas loading to the residual gas after the surface interval. This is called "residual nitrogen time" (RNT) when the gas is nitrogen. The RNT is added to the planned "actual bottom time" (ABT) to give an equivalent "total bottom time" (TBT) which is used to derive the required decompression schedule for the planned dive.
Equivalent residual times can be derived for other inert gases. These calculations are done automatically in personal diving computers, which is the reason why they should not be shared by divers, and why a diver should not switch computers without a sufficient surface interval (about 24 hours in most cases).
Residual inert gas can be computed for all modeled tissues, but repetitive group designations in decompression tables are generally based on only the one tissue, considered by the table designers to be the most limiting tissue for likely applications. In the case of the US Navy Air Tables (1956) this is the 120 minute tissue,[52] while the Bühlmann tables use the 80 minute tissue.[53]
Diving at altitude
The atmospheric pressure decreases with altitude, and this has an effect on the absolute pressure of the diving environment. The most important effect is that the diver must decompress to a lower surface pressure, and this requires longer decompression for the same dive profile. A second effect is that a diver ascending to altitude, will be decompressing en route, and will have residual nitrogen until all tissues have equalized to the local pressures. This means that the diver should consider any dive done before equilibration as a repetitive dive, even if it is the first dive in several days. The decompression algorithms can be adjusted to compensate for altitude. This was first done by Bühlmann, and is now common on diving computers, where an altitude setting can be selected.
Flying and ascent to altitude after diving
Exposure to reduced atmospheric pressure during the period after a dive when the residual gas levels have not yet stabilised at atmospheric saturation levels can incur a risk of decompression sickness. Rules for safe ascent are based on extension of the decompression model calculations to the desired altitude, but are generally simplified to a few fixed periods for a range of exposures. For the extreme case of an exceptional exposure dive, the US Navy requires a surface interval of 48 hours before ascent to altitude. A surface interval of 24 hours for a Heliox decompression dive and 12 hours for Heliox no-decomprssion dive are also specified.[54]
More detailed surface interval requirements based on the highest repetitive group designator obtained in the preceding 24hour period are given on the US Navy Diving Manual Table 9.6,[54] both for ascents to specified altitudes, and for commercial flights in aircraft nominally pressurised to 8000 ft.
The first DAN flying after diving workshop in 1989 consensus guidelines recommended:[55]
- wait for 12 hours before flying after up to two hours of no-stop diving within the previous 48 hours;
- wait for 24 hours before flying after multiday, unlimited no-stop diving;
- wait for 24–48 hours before flying after dives that required decompression stops;
- do not fly with DCS symptoms unless necessary to obtain hyperbaric treatment.
DAN later proposed a simpler 24-hour wait after any and all recreational diving, but there were objections on the grounds that such a long delay would result in lost business for island diving resorts and the risks of DCS when flying after diving were too low to warrant this blanket restraint.
The DAN Flying after Diving workshop of 2002 made the following recommendations for flying after recreational diving:[55]
- a 12-hour surface interval for uncertified individuals who took part in a "resort" or introductory scuba experience;
- an 18-hour surface interval for certified divers who make an unlimited number of no-decompression air or nitrox dives over multiple days; and
- substantially longer than 18 hours for technical divers who make decompression dives or used helium breathing mixes, as no specific evidence concerning decompression or helium diving was available.
These recommendations apply to flying at an altitude greater than, or cabin pressure less than, an altitude equivalent of 2,000 feet (610 meters)
NASA astronauts train underwater to simulate the weightlessness and occasionally need to fly afterwards at cabin altitudes not exceeding 10,000 feet (3,000 meters). Training dives use 46% Nitrox and can exceed six hours at a maximum depth of 40 ffw (12 mfw) for a maximum equivalent air depth (EAD) of 24 fsw (7 msw). NASA guidelines for EADs of 20-50 fsw (6-15 msw) with maximum dive durations of 100–400 minutes allow either air or oxygen to be breathed in the preflight surface intervals. Oxygen breathing during surface intervals reduces the time to fly by a factor of seven to nine times compared with air.[55]
A study by another military organization, the Special Operations Command also indicated that preflight oxygen might be an effective means for reducing DCS risk.[55]
Decompression tables
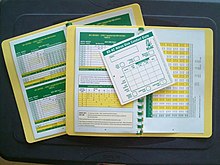

Dive tables or decompression tables are printed cards or booklets that allow divers to determine for a decompression schedule for a particular dive profile and breathing gas.
With dive tables, it is assumed that the dive profile is a square dive, meaning that the diver descends to maximum depth immediately and stays at the same depth until resurfacing (approximating a rectangular line when drawn in a coordinate system where one axis is depth and the other is duration). Some dive tables also assume physical condition or acceptance of a specific level of risk from the diver. Some recreational tables only provide for no-stop dives at sea level sites, but the more complete tables can take into account staged decompression dives and dives performed at altitude.
Commonly used decompression tables
- US Navy tables;[56]
- Bühlmann tables;[7][57][58]
- Royal Navy {RNPL} tables;
- BSAC 88 tables;[59][60]
- PADI tables: the recreational dive planner (RDP) and "the wheel";[61]
- DCIEM tables;[62][63]
- French Navy MN90 tables;[64]
- NAUI Dive tables.[65]
Other published tables
Recreational Dive Planner

The Recreational Dive Planner (or RDP) is a decompression table in which no-stop time underwater is calculated.[68] The RDP was developed by DSAT and was the first dive table developed exclusively for recreational, no stop diving.[61] There are four types of RDPs: the original table version first introduced in 1988, The Wheel version, the original electronic version or eRDP introduced in 2005 and the latest electronic multi-level version or eRDPML introduced in 2008.
The low price and convenience of many modern dive computers mean that many recreational divers only use tables such as the RDP for a short time during training before moving on to use a diving computer.
Decompression software
Decompression software such as Departure, DecoPlanner, Ultimate Planner, Z-Planner, V-Planner and GAP are available, which simulate the decompression requirements of different dive profiles with different gas mixtures using decompression algorithms.[69][70][71][72]
Bespoke tables or schedules generated by decompression software represent a diver's specific dive plan and breathing gas mixtures. It is usual to generate a schedule for the planned profile and for the most likely contingency profiles.
Decompression software is available based on:
- US Navy model
- Buhlmann model (eg: Z-planner)
- Reduced Gradient Bubble model (eg: GAP)
- Varying Permeability model (eg: V-Planner)
and variations of these
Personal decompression computers
The personal dive computer is a small computer with pressure sensor which is mounted in a waterproof and pressure resistant housing and has been programmed to model the inert gas loading of the diver's tissues in real time during a dive. Most are wrist mounted, but a few are mounted in a console with the submersible pressure gauge and possibly other instruments. A display allows the diver to see critical data during the dive, including the maximum and current depth, duration of the dive, and decompression data. Other data such as water temperature and cylinder pressure are also sometimes displayed. The dive computer has the advantages of monitoring the actual dive, as opposed to the planned dive, and does not work on a "square profile" - it dynamically calculates the real profile of pressure exposure in real time, and keeps track of residual gas loading for each tissue used in the algorithm.
Choice of tables or algorithms
During the 1980s the US recreational diving community tended to move away from the US Navy tables to a range of tables published by other organisations, including several of the diver certification agencies (BSAC, NAUI, PADI).[73]
Depending on the table or computer chosen the range of no-decompression limits at a given depth on air can vary considerably, for example for 100fsw (30msw) NSL varies from 25 minutes to 8 minutes. It is not possible to discriminate between "right" and "wrong" options, but is is possible to say that the risk of developing DCS is greater for the longer exposures and less for the shorter exposures.[73]
The choice of tables for professional diving use is generally made by the organisation employing the divers, and for recreational training it is usually prescribed by the certifying agency, but for recreational purposes the diver is generally free to make use of any of the published tables, and for that matter, to modify them to suit himself.[73]
Teaching of decompression theory and tables
Decompression is an area where you discover that, the more you learn, the more you know that you really dont know what is going on. For behind the "black-and-white" exactness of table entries, the second-by-second countdowns of dive computers, and beneath the mathematical purity of decompression models, lurks a dark and mysterious physiological jungle that has barely been explored.
— Karl E. Huggins, 1992[74]
Exposure to the various theories, models, tables and algoritms is needed to allow the diver to make educated and knowledgeable decisions regarding their personal decompression needs.[75]
Decompression procedures
Bottom time
Bottom time is the time spent at depth before starting the ascent. Bottom time used for decompression planning may be defined differently depending on the tables or algorithm used. It may include descent time, but not in all cases. It is important to check what bottom time is defined for the tables before they are used.
Continuous decompression
Continuous decompression is decompression without stops. Instead of a fairly rapid ascent rate to the first stop, followed by a period at static depth during the stop, the ascent is slower, but without officially stopping. In theory this is the optimum decompression profile. In practice this is very difficult to do manually, and it may be necessary to stop the ascent occasionally to get back on schedule, but these stops are not part of the schedule, they are corrections. To further complicate the practice, the ascent rate may vary with the depth, and is typically faster at greater depth and reduces as the depth gets shallower. In practice a continuous decompression profile may be approximated by ascent in steps as small as the chamber pressure gauge will resolve, and timed to follow the theoretical profile as closely as conveniently practicable.
For example, continuous decompression is used in USN treatment table 7. This table uses an ascent rate of 3 fsw per hour from 60 fsw to 40 fsw, followed by 2 fsw per hour from 40 fsw to 20 fsw and 1 fsw per hour from 20 fsw to 4 fsw.[50]
No decompression dives, ascent rate and safety stops
A "no stop" dive is a dive that needs no decompression stops during the ascent[49] and relies on a controlled ascent rate for the elimination of excess inert gases. In effect, the diver is doing continuous decompression during the ascent.
Dive computers
Dive computers are designed to be worn by a diver during a dive.[76] These computers contain, at a minimum, a pressure sensor and an electronic timer. They use a decompression algorithm to calculate the inert gas loading on one or more tissue compartments and display the remaining no decompression limit calculated in real time for the diver throughout the dive. When planning a dive using dive tables, divers assume that the entire dive is spent at whatever the maximum depth will be. Using a computer, the diver is credited for the time they spend at lesser depths during a multi-level dive.
Dive computers also provide a measure of safety for divers that accidentally dive a different profile to that originally planned. If the diver exceeds a no decompression limit, decompression additional to the ascent rate will be necessary. Many dive computers will provide required decompression information in the event that the no decompression limits are exceeded.
Ascent rate
In addition to stops, the diver must not exceed a safe ascent rate during the whole of the ascent from depth. Normally the time to ascend from the shallowest stop to the surface will take at least 1 minute. Typically with tables, the maximum ascent rate is 10 metres (33 ft) per minute when deeper than 6 metres (20 ft). Some dive computers have variable maximum ascent rates, depending on depth.
Safety stop
As a precaution against any unnoticed dive computer malfunction, diver error or physiological predisposition to decompression sickness, many divers do an extra "safety stop" in addition to those ordered by their dive computer or tables.[77] A safety stop is typically 1 to 5 minutes at 3 to 6 metres (10 to 20 ft). They are usually done during no-stop dives and may be added to the obligatory decompression on staged dives.
Staged decompression and decompression stops

A decompression stop is a period a diver must spend at a constant depth in shallow water at the end of a dive to safely eliminate absorbed inert gases from the diver's body to avoid decompression sickness.[49] The practice of making decompression stops is called staged decompression,[7][78] as opposed to continuous decompression.[79][80]
A decompression schedule is a series of increasingly shallower decompression stops—often for increasing amounts of time—that a diver uses to outgas inert gases from their body during ascent to the surface to reduce the risk of decompression sickness. In a decompression dive, the decompression phase may make up a large part of the time spent underwater (in many cases it is longer than the actual time spent at depth).
The depth and duration of each stop is dependent on many factors, primarily the profile of depth and time of the dive, but also the breathing gas mix, the interval since the previous dive and the altitude of the dive site. The diver obtains the depth and duration of each stop from a dive computer, decompression tables or dive planning computer software. A deco diver will typically prepare more than one decompression schedule to plan for contingencies such as going deeper than planned or spending longer at depth than planned.
Doing a decompression stop

The diver uses decompression tables,[81] software planning tools or dive computers to find, for his planned dive profile and breathing gas, if decompression stops are needed, and if so, the depths and durations of the stops.
Shorter and shallower decompression dives may only need one single short shallow decompression stop, for example 5 minutes at 3 metres (10 ft). Longer and deeper dives often need a series of decompression stops, each stop being longer but shallower than the previous stop.
After the bottom sector of the dive, the ascent is made at the recommended rate until the diver reaches the depth of the first stop. The diver then maintains the specified stop depth for the specified period, before ascending to the next stop depth at the recommended rate, and follows the same procedure again. This is repeated until all required decompression has been completed and the diver reaches the surface.
Once on the surface the diver will continue to eliminate inert gas until the concentrations have returned to normal surface saturation, which can take several hours, and is considered by some tables to be effectively compete after 12 hours,[50] and by others to take up to, or even more than 24 hours.
Missed stops
A diver missing a required decompression stop risks developing decompression sickness. The risk is related to the depth and duration of the missed stops. The usual causes for missing stops are: not having enough breathing gas to complete the stops, or accidentally losing control of buoyancy. An aim of most basic diver training is to prevent these two faults. There are less predictable causes of missing decompression stops. Diving suit failure in cold water forces the diver to choose between hypothermia and decompression sickness. Diver injury or marine animal attack may also limit the duration of stops the diver is willing to carry out.
Technical diving education organizations define special procedures to be done if decompression stops are missed. These procedures may need repeating one or several stops.
A procedure for dealing with omitted decompression stops is described in the US Navy Diving Manual[50] In principle the procedure allows a diver who is not yet presenting symptoms of decompression sickness, to go back down and complete the omitted decompression, with some extra added to deal with the bubbles which are assumed to have formed during the period where the decompression ceiling was violated. Divers who become symptomatic before they can be returned to depth are treated for decompression sickness, and do not attempt the omitted decompression procedure as the risk is considered unacceptable under normal operational circumstances.
Accelerated decompression
Decompression can be accelerated by the use of breathing gases during ascent with lowered inert gas fractions (as a result of increased oxygen fraction). This will result in a greater diffusion gradient for a given ambient pressure, and consequently accelerated decompression for a relatively low risk of bubble formation. Nitrox mixtures and oxygen are the most commonly used gases for this purpose, but oxygen rich Trimix blends can also be used after a Trimix dive, and may reduce risk of isobaric counterdiffusion complications. Doolette and Mitchell showed that "breathing-gas switches should be scheduled deep or shallow to avoid the period of maximum supersaturation resulting from decompression".[82]
Decompression using a personal decompression computer
The personal decompression computer provides a real time modelling of the inert gas load on the diver according to the decompression algorithm programmed into the computer by the manufacturer, with possible personal adjustments for conservatism and altitude set by the user. In all cases the computer monitors the depth and elapsed time of the dive, and many have input specifying the gas mixture.
Most computers require the diver to specify the mixture before the dive, but some allow the choice of mixture to be changed during the dive, which allows for the use of gas switching for accelerated decompression. A third category, mostly used by closed circuit rebreather divers, monitors the partial pressure of oxygen in the breathing mix using a remote oxygen sensor, but requires diver intervention to specify the inert gas constituents and ratio of the mix in use.
The computer retains the diver's pressure exposure history, and continuously updates the tissue loads on the surface, so the current tissue loading should always be correct according to the algorithm, though it is possible to provide the computer with misleading input conditions, which can nullify its reliability.
This ability to provide real-time tissue loading data allows the computer to indicate the diver's current decompression obligation, and to update it for any permissible profile change, so the diver with a decompression ceiling does not have to decompress at any specific depth provided the ceiling is not violated, though the decompression rate will be affected by the depth. As a result, the diver can make a slower ascent than would be called for by a decompression schedule computed by the identical algorithm, as my suit the circumstances, and will be credited for gas elimination during the slower ascent, and penalised if necessary for additional ingassing for those tissues affected. This provides the diver with an unprecedented flexibility of dive profile, while remaining within the safety envelope of the algorithm in use.
Ratio decompression
Ratio decompression (usually referred to in abbreviated form as ratio deco) is a technique for calculating decompression schedules for scuba divers engaged in deep diving without using dive tables, decompression software or a dive computer. It is generally taught as part of the "DIR" philosophy of diving promoted by organisations such Global Underwater Explorers (GUE) and Unified Team Diving (UTD) at the advanced technical diving level. It is designed for decompression diving executed deeper than standard recreational diving depth limits using trimix as a "bottom mix" breathing gas.[83]
It is largely an empirical procedure, and has a reasonable safety record within the scope of its intended application. Advantages are reduced overall decompression time and easy estimation of decompression by the use of a simple rule-based procedure which can be done underwater by the diver. It requires the use of specific gas mixtures for given depth ranges.
It is not clear why this procedure is considered to be an advantage over the use of personal decompression computers which are programmed to allow for a variety of gas mixtures and gas switches during a dive.
Surface decompression
Surface decompression is a procedure in which some or all of the staged decompression obligation is done in a decompression chamber instead of in the water. This reduces the time that the diver spends in the water, exposed to environmental hazards such as cold water or currents, which will enhance diver safety. The decompression in the chamber is more controlled, in a more comfortable environment, and oxygen can be used at greater partial pressure as there in no risk of drowning and a lower risk of oxygen toxicity convulsions. A further operational advantage is that once the divers are in the chamber, new divers can be supplied from the diving panel, and the operations can continue with less delay.
A typical surface decompression procedure is described in the US Navy Diving Manual. If there is no in-water 40 ft stop required the diver is surfaced directly. All required decompression up to and including the 40 ft (12 m) stop is completed in-water. The diver is then surfaced and pressurised in a chamber to 50 fsw within 5 minutes of leaving 40 ft depth in the water. If this "surface interval" from 40 ft in the water to 50 fsw in the chamber exceeds 5 minutes, a penalty is incurred, as this indicates a higher risk of DCS symptoms developing, so longer decompression is required.
In the case where the diver is successfully recompressed within the nominal interval, he will be decompressed according to the schedule in the air decompression tables for surface decompression, preferably on oxygen, which is used from 40 fsw (12 msw), a partial pressure of 2.2 bar. Stops are also done at 30 fsw and 20 fsw, for times according to the schedule. Air breaks of 5 minutes are taken at the end of each 30 minutes of oxygen breathing.[50]
Surface decompression procedures have been described as "semi-controlled accidents".[37]
Dry bell decompression
"Dry", or "Closed" diving bells are pressure vessels for human occupation which can be deployed from the surface to transport divers to the underwater workplace at pressures greater than ambient. They are equalized to ambient pressure at the depth where the divers will get out and back in after the dive, and are then re-sealed for transport back to the surface, which also generally takes place with controlled internal pressure greater than ambient. During and/or after the recovery from depth, the divers may be decompressed in the same way as if they were in a decompression chamber, so in effect, the dry bell is a mobile decompression chamber. Another option, used in saturation diving, is to decompress to storage pressure (pressure in the habitat part of the saturation spread) and then transfer the divers to the saturation habitat under pressure (transfer under pressure - TUP), where they will stay until the next shift, or until decompressed at the end of the saturation period.
Saturation decompression
Once all the tissue compartments have reached saturation for a given pressure and breathing mixture, continued exposure will not increase the gas loading of the tissues. From this point onwards the required decompression remains the same. If divers work and live at pressure for a long period, and are decompressed only at the end of the period, the risks associated with decompression are limited to this single exposure. This principle has led to the practice of saturation diving, and as there is only one decompression, and it is done in the relative safety and comfort of a saturation habitat, the decompression is done on a very conservative profile, minimising the risk of bubble formation, growth and the consequent injury to tissues. A consequence of these procedures is that saturation divers are more likely to suffer decompression sickness symptoms in the slowest tissues, whereas bounce divers are more likely to develop bubbles in faster tissues.
Therapeutic decompression
Therapeutic decompression is a procedure for treating decompression sickness by recompressing the diver, thus reducing bubble size, and allowing the gas bubbles to re-dissolve, then decompressing slowly enough to avoid further formation or growth of bubbles, or eliminating the inert gases by breathing oxygen under pressure.
Therapeutic decompression on air
Historically, therapeutic decompression was done by recompressing the diver to the depth of relief of pain, or a bit deeper, maintaining that pressure for a while, so that bubbles could be re-dissolved, and performing a slow decompression back to the surface pressure. Later air tables were standardised to specific depths, followed by slow decompression. This procedure has been superseded almost entirely by hyperbaric oxygen treatment.[81][84][85][86] Recompression on atmospheric air was shown to be an effective treatment for minor DCS symptoms by Keays in 1909.[87]
Hyperbaric oxygen therapy

Evidence of the effectiveness of recompression therapy utilizing oxygen was first shown by Yarbrough and Behnke,[86] and has since become the standard of care for treatment of DCS.[88]
A typical hyperbaric oxygen treatment schedule is the US Navy Table 6, which provides for a standard treatment of 3 to 5 periods of 20 minutes of oxygen breathing at 60 fsw (18msw) followed by 2 to 4 periods of 60 minutes at 30 fsw (9 msw) before surfacing. Air breaks are taken between oxygen breathing to reduce the risk of oxygen toxicity.[50]
In water recompression

If a chamber is not available for recompression within a reasonable period, a riskier alternative is in-water recompression at the dive site.[89][90][91] In-water recompression (IWR) is the emergency treatment of decompression sickness (DCS) by sending the diver back underwater to allow the gas bubbles in the tissues, which are causing the symptoms, to resolve. It is a risky procedure that should only be used when it is not practicable to travel to the nearest recompression chamber in time to save the victim's life.[90][91]
The procedure is high risk as a diver suffering from DCS may become paralysed, unconscious or stop breathing whilst under water. Any one of these events may result in the diver drowning or further injury to the diver during a subsequent rescue to the surface. These risks can be mitigated to some extent by using a helmet or full-face mask with voice communications on the diver, and suspending the diver from the surface so that depth is positively controlled, and by having an in-water standby diver attend the diver undergoing the treatment at all times.
The principle behind in water recompression treatment is the same as that behind the treatment of DCS in a recompression chamber[90][91]
Although in-water recompression is regarded as risky, and to be avoided, there is increasing evidence that technical divers who surface and demonstrate mild DCS symptoms may often get back into the water and breathe pure oxygen at a depth 20 feet/6 meters for a period to seek to alleviate the symptoms. This trend is noted in paragraph 3.6.5 of DAN's 2008 accident report.[92] The report also notes that whilst the reported incidents showed very little success, "[w]e must recognize that these calls were mostly because the attempted IWR failed. In case the IWR were successful, [the] diver would not have called to report the event. Thus we do not know how often IWR may have been used successfully."[92]
Historically, in-water recompression was the usual method of treating decompression sickness in remote areas. Procedures were often informal and based on operator experience, and used air as the breathing gas as it was all that was available. The divers generally used standard diving gear, which was relatively safe for this procedure, as the diver was at low risk of drowning if he lost consciousness.[19]
Decompression equipment

There are several types of equipment used to help divers carry out decompression. Some are used to mark the underwater position of the diver and act as a buoyancy control aid and position reference in low visibility or currents.
Decompression may be shortened (or accelerated) by breathing an oxygen-rich "deco gas" such as a nitrox with 50% or more oxygen. The high partial pressure of oxygen in such decompression mixes create the effect of the oxygen window. This decompression gas is often carried in side-slung cylinders.
Controlling depth and ascent rate
A critical aspect of successful decompression is that the depth and ascent rate of the diver must be monitored and sufficiently accurately controlled. Practical in-water decompression requires a reasonable tolerance for variation in depth and rate of ascent, but unless the decompression is being monitored in real time by a decompression computer, any deviations from the nominal profile will affect the risk. Several items of equipment are used to assist in facilitating accurate adherence to the planned profile, by allowing the diver to more easily control depth and ascent rate, or to transfer this control to specialist personnel at the surface.
Shot lines

A shot line is a rope between a float at the surface, and a sufficiently heavy weight holding the rope approximately vertical. The shot line float should be sufficiently buoyant to support the weight of all divers that are likely to be using it at the same time. As divers are seldom weighted to be very negatively buoyant, a positive buoyancy of 50 kg is considered adequate by some authorities for general commercial use.[93] Recreational divers are free to choose lesser buoyancy ay their own risk. The shot weight should be sufficient to prevent a diver from lifting it from the bottom by over-inflation of the buoyancy compensator or dry suit, but not sufficient to sink the float if the slack on the line is all taken up. Various configurations of shot line are used to control the amount of slack.
The diver ascends along the shotline, and may use it purely as a visual reference, or can hold on to it to positively control depth, or can climb up it hand over hand. A Jonline may be used to fasten a diver to an anchor line or rope during a decompression stop.
An adequate shotline can significntly contribute to diver safety, but insufficient buoyancy has led to accidents, in some cases fatal, when the buoy submerged under the load of divers hanging on the line, and a diver decompressing on oxygen did not notice and lost consciousness due to oxygen toxicity and drowned, [citation needed]
Shot line configurations:
- Basic shot line
- Self tensioning arrangements
- Running weight
- Running float
- Lazy shot line
Decompression trapezes
A decompression trapeze is a device used in recreational diving and technical diving to make decompression stops more comfortable and more secure and provide the divers' surface cover with a visual reference for the divers' position.
It consists of a horizontal bar or bars suspended at the depth of intended decompression stops by buoys. The bars are of sufficient weight and the buoys of sufficient buoyancy that the trapeze will not easily change depth in turbulent water or if the divers experience buoyancy control problems.[94]
Trapezes are often used with diving shots. When diving in tidal waters at the end of slack water, the trapeze may be released from the diving shot to drift in the current as the divers make their decompression stops.
-
Basic shotline: Weight, and float connected by a line
-
Bottom tensioned shotline: The line passes through a ring at the weight and is tensioned by a small float, often a small lift bag which can later help lift the shot as the air expands.
-
Top tensioned shotline: The line passes through a ring at the float and is tensioned by a smaller weight hanging from it. This weight may be hooked to the main part of the line by a sliding clip to restrain it from swinging.
-
A shotline with a lazy shot - a second float with a short weighted line tethersd to it at just below the depth of the deepest long decompression stop.
-
A shotline with a decompression trapeze - a series of crossbars suspended from a float at each end and ballasted as necessary, tethered to the main shotline.
Surface marker buoy and delayed surface marker buoy

A surface marker buoy (SMB) with a reel and line is often used by a dive leader to allow the boat to monitor progress of the dive. This can provide the operator with a positive control of depth, by remaining slightly negative and using the buoyancy of the float to support this slight overweighting. This allows the line to be kept under slight tension which reduces the risk of entanglement. The reel or spool used to store and roll up the line is usually slightly negative, so that if released it will hang down and not float away.
A delayed or deployable surface marker buoy (DSMB) is a soft inflatable tube which is attached to a reel or spool line at one end, and is inflated by the diver under water and released to float to the surface, deploying the line as it ascends. This provides information to the surface that the diver is about to ascend, and where he is. This equipment is commonly used by recreational and technical divers, and requires a certain level of skill to operate safely. Once deployed, the use is identical to that for the standard surface marker and reel.
Diving stages and wet bells
A diving stage, sometimes known as the basket, is a platform on which a diver stands which is hoisted into the water, lowered to the workplace ot the bottom, and then hoisted up again to return the diver to the surface and lift him out of the water. This equipment is almost exclusively used by surface supplied professional divers, as it requires fairly complex lifting equipment. A diving stage allows the surface team to conveniently manage a diver's decompression as it can be hoisted at a controlled rate and stopped at the correct depth for decompression stops, and allows the divers to rest during the ascent. It also allows the divers to be safely and conveniently lifted out of the water and returned to the deck or quayside.
A wet bell, or open bell, is similar to a diving stage in concept, but has an air space, open to the water at the bottom in which the divers, or at least their heads, can shelter during ascent and descent.
Providing gases to accelerate decompression

Reducing the partial pressure of the inert gas component of the breathing mixture will accelerate decompression as the concentration gradient will be greater for a given depth. This is usually achieved by increasing the partial pressure of oxygen in the breathing gas, as substituting a different inert gas may have counterdiffusion complications due to differing rates of diffusion, which can lead to a net gain in total dissolved gas tension in a tissue. This can lead to bubble formation and growth, with decompression sickness as a consequence. Partial pressure of oxygen is usually limited to 1.6 bar during in water decompression, but can be up to 2.2 bar when using the US Navy tables for surface decompression.
Stage cylinders
Open circuit scuba divers by definition are independent of surface supply, and must take any gas mixture with them that is to be used on a dive. However if they are confident of returning by a specific route, the decompression gas may be stored at appropriate places on that route. The cylinders used for this purpose are called stage cylinders, and they are usually provided with a standard regulator and a submersible pressure gauge, and are usually left at the stop with the regulator pressurised, but the cylinder valve turned off to minimise the risk of gas loss. Similar cylinders are carried by the divers when the route back is not secure. They are commonly mounted as sling cylinders, clipped to D-rings at the sides of the diver's harness.
Divers take great care to avoid breathing oxygen enriched "deco gas" at great depths because of the high risk of oxygen toxicity. To prevent this happening, cylinders containing oxygen-rich gases must always be positively identifiable. One way of doing this is by marking them with their maximum operating depth as clearly as possible.[95] Other safety precautions may include using different coloured regulator housing, flavoured mouthpieces, or simply placing a rubber band vertically across the mouthpiece as an alert.[96]
Surface panel gas switching
Surface supplied divers may be supplied with a gas mixture suitable for accelerated decompression by connecting a supply to the surface gas panel and connecting it through the valve system to the divers. This allows accelerated decompression, usually on oxygen, which can be used to a maximum depth of 6 m in water[50] Surface supplied heliox bounce divers will be provided with mixtures suitable for their current depth, and the mixture may be changed several times during descent and ascent from great depths.[citation needed]
Continuously variable mixture in closed circuit rebreathers

Closed circuit rebreathers are usually controlled to provide a fairly constant partial pressre of oxygen during the dive (set point), and may be reset to a richer mix for decompression. The effect is to keep the partial pressure of inert gases as low as safely practicable throughout the dive. This minimises the absorption of inert gas in the first place, and accelerates the elimination of the inert gases during ascent.
Deck decompression chambers

Deck decompression chambers are used for surface decompression, described in a previous section.
A deck decompression chamber (DDC) is a two compartment pressure vessel for human occupation which has sufficient space in the main chamber for two or more occupants, and a forechamber which can allow a person to be pressurised or decompressed while the main chamber remains under constant pressure. This allows an attendant to be locked in or out during treatment of the occupant(s) of the main chamber. There is usually also a medical lock, which serves a similar function but is much smaller. This is used to transfer medical material, food and specimens into and out of the main chamber while it is under pressure. Most deck decompression chambers are fitted with built in breathing systems (BIBS), which supply an alternative breathig gas to the occupants (usually oxygen), and discharge the exhaled gas outside the chamber, so the chamber gas is not excessively enriched by oxygen, which would cause an unacceptable fire hazard, and require frequent flushing with chamber gas (usually air).
A deck decompression chamber is intended for surface decompression and emergency hyperbaric treatment of divers, but can be used for other hyperbaric treatment under the appropriate supervision of hyperbaric medical personnel.
Portable or mobile one and two occupant single compartment chambers are not generally intended for routine surface decompression, but may be used in an emergency.
Dry bells and Saturation spreads


A "Saturation System" or "Saturation spread" typically comprises a living chamber, transfer chamber and submersible decompression chamber, which is commonly referred to in commercial diving and military diving as the diving bell,[97] PTC (Personnel Transfer Capsule) or SDC (Submersible Decompression Chamber).[81] The system can be permanently placed on a ship or ocean platform, but is more commonly capable of being moved from one vessel to another by crane. The entire system is managed from a control room (van), where depth, chamber atmosphere and other system parameters are monitored and controlled. The diving bell is the elevator or lift that transfers divers from the system to the work site. Typically, it is mated to the system utilizing a removable clamp and is separated from the system tankage bulkhead by a trunking space, a kind of tunnel, through which the divers transfer to and from the bell. At the completion of work or a mission, the saturation diving team is decompressed gradually back to atmospheric pressure by the slow venting of system pressure, at an average of 15 metres (49 ft) per day, at 24 hours a day (schedules vary). Thus the process involves only one ascent, thereby mitigating the time-consuming and comparatively risky process of multiple decompressions normally associated with non-saturation ("bounce diving") operations.[98]
The divers use surface supplied umbilical diving equipment, utilizing deep diving breathing gas, such as helium and oxygen mixtures, stored in large capacity, high pressure cylinders.[98] The gas supplies are plumbed to the control room, where they are routed to supply the system components. The bell is fed via a large, multi-part umbilical that supplies breathing gas, electricity, communications and hot water. The bell also is fitted with exterior mounted breathing gas cylinders for emergency use. The divers are supplied from the bell through umbilicals.
A hyperbaric lifeboat may be provided for emergency evacuation of saturation divers from a saturation system. This would be used if the platform is at immediate risk due to fire or sinking, and allows the divers under saturation to get clear of the immediate danger. A hyperbaric lifeboat is self-contained and can be operated from the inside by the occupants while under pressure. It must be self-sufficient for several days at sea, in case of a delay in rescue due to sea conditions. The occupants would normally start decompression immediately after launching.
A dry bell may also be used for bounce dives to great depths, and then used as the decompression chamber during the ascent and later on board the support vessel. In this case it is not always necessary to transfer into a deck chamber, as the bell is quite capable of performing this function, though it would be relatively cramped, as a bell is usually as small as conveniently possible to minimise weight for deployment.
History of decompression research and development
Timeline

- 1660 - Sir Robert Boyle conducted an experiment on a bird in an air pump. This predates actual intentional investigations into decompression, but the experiment was effectively a rapid decompression and caused the death of the bird by asphyxiation.
- 1670 – Sir Robert Boyle performed an experiment with a viper in a vacuum. A bubble was observed in its eye and it displayed signs of extreme discomfort. This was the first recorded description of decompression sickness.[99]
- 1841 – Jacques Triger documented the first cases of decompression sickness in humans when two miners involved in pressurised caisson work developed symptoms.[99]
- 1847 – The effectiveness of recompression for treatment of DCS in caisson workers was described by Pol and Watelle[99][100]
- 1857 - Hoppe-Seyler repeated Boyle's experiments and suggested that sudden death in compressed air workers was caused by bubble formation, and recommended recompression therapy.[101]
- 1868 – Alfred Le Roy de Méricourt – Decompression sickness described as a sponge divers occupational illness[100]
- 1873 – Dr. Andrew Smith first used the terms "caisson disease" and "compressed air illness", describing 110 cases of decompression sickness as the physician in charge during construction of the Brooklyn Bridge.[101][102] The nickname "the bends" was used after workers emerging from pressurized construction on the Brooklyn Bridge adopted a posture similar to fashionable ladies of the period "the Grecian Bend".[99]
- 1878 – Paul Bert determined that decompression sickness is caused by nitrogen gas bubbles which were released from tissues and blood during or after decompression, and showed the advantages of breathing oxygen after developing decompression sickness.[79]
- 1897 - N. Zuntz proposed a perfusion based tissue model.[103]
- 1906 - V. Schrotter suggested a uniform decompression of 20 minutes per atmosphere. J.S. Haldane was commissioned by the British Admiralty to study decompression sickness.[101]
- 1908 – John Scott Haldane - the first recognised decompression table was prepared for the British Admiralty.[14] This table was based on experiments performed on goats using an end point of symptomatic DCS.[78][99]
- 1912 – Chief Gunner George D. Stillson of the United States Navy created a program to test and refine Haldane's tables.[104] This program ultimately led to the first publication of the United States Navy Diving Manual and the establishment of a Navy Diving School in Newport, Rhode Island. Diver training programs were later cut at the end of World War I.
- 1912 – Leonard Erskine Hill – continuous uniform decompression[99][100]
- 1927 – Naval School, Diving and Salvage was re-established at the Washington Navy Yard. At this time the United States moved their Navy Experimental Diving Unit (NEDU) to the same naval yard. In the following years, the Experimental Diving Unit developed the US Navy Air Decompression Tables which became the accepted world standard for diving with compressed air.[105]
- 1930's - Hawkins, Schilling and Hansen conduct extensive experimental dives to determine allowable supersturation ratios for different tissue compartments for Haldanean model[106]
- 1935 – Albert R. Behnke et al. experimented with oxygen for recompression therapy.[99]
- 1937 - US Navy 1937 tables published (Yarborough)[106]
- 1941 – Altitude DCS is treated with hyperbaric oxygen for the first time.[107]
- 1956 - US Navy Decompression Tables (1956) published
- 1960 – FC Golding et al. split the classification of DCS into Type 1 and 2.[108]
- 1965 – LeMessurier and Hills paper on A thermodynamic approach arising from a study on Torres Strait diving techniques which suggests that decompression by conventional models results in bubble formation which is then eliminated by re-dissolving at the decompression stops, which is slower than elimination while still in solution, thus indicating the importance of minimising bubble phase for efficient gas elimination.[19][109]
- 1965 - French Navy GERS (Groupe d’Etudes et Recherches Sous-marines) 1965 table
- 1965 – Goodman and Workman - Introduction of recompression tables utilizing oxygen to accelerate elimination of inert gas[110][111]
- 1972 - Royal Navy Physiological Laboratory (RNPL) tables based on Hempleman's tissue slab diffusion model.[112]
- 1973 - Isobaric counterdiffusion first described by Graves, Idicula, Lambertsen, and Quinn in subjects who breathed one inert gas mixture while being surrounded by another.[113][114]
- 1973 - French civilian Tables du Ministère du Travail 1974 (MT74)
- 1976 - The sensitivity of decompression testing increased by the use of ultrasonic methods which can detect mobile venous bubbles before symptoms of DCS emerge.[115]
- 1981 - Huggins model and tables using Spencer's formula for no-decompression limits.[65]
- 1982 – Paul K Weathersby, Louis D Homer and Edward T Flynn introduce survival analysis into the study of decompression sickness.[116]
- 1983/4 – Albert A. Bühlmann publishes Decompression-Decompression sickness.[7] Bühlmann recognized the problems associated with altitude diving, and proposed a method which calculated maximum nitrogen loading in the tissues at a particular ambient pressure.
- 1984 - DCIEM (Defence and Civil Institution of Environmental Medicine, Canada) release No-Decompression and Decompression Tables based on Kidd/Stubbs serial compartment model and extensive ultrasonic testing.[30]
- 1984 - Edward D. Thalmann publishes USN E-L algorithm and tables for constant PO2 Nitrox closed circuit rebreather applications
- 1985 - Thalmann extends use of E-L model for constant PO2 Heliox CCR.
- 1985 - Bassett tables (based on USN Tables)[66]
- 1986 - Swiss Sport Diving Tables based on Buhlmann model[65]
- 1986 - D. E. Yount and D. C. Hoffman propose a bubble model.
- 1988 - BSAC'88 tables[117]
- 1990 - DCIEM sport diving tables released.
- 1990 - French Navy - Marine Nationale 90 (MN90) decompression tables
- 1991 - D.E. Yount describes Varied Permeability Model
- 1992 - French civilian Tables du Ministère du Travail 1992 (MT92)
- 1999 - NAUI Trimix and Nitrox tables based on RGBM model
- 2001 - NAUI recreational air tables based on RGBM model
- 2007 - Gerth & Doolette publish VVal 18 and VVal 18M parameter sets for tables and programmes based on the Thalmann E-L algorithm, and produce an internally compatible set of decompression tables for open circuit and CCR on air and Nitrox, including in water air/oxygen decompression and surface decompression on oxygen.
- 2008 - US Navy Diving Manual Revision 6 includes a version of the 2007 tables by Gerth & Doolette.
Haldanean (perfusion limited, dissolved phase) models
Early decompression theory generally assumed that inert gas bubble formation in the tissues could be avoided during decompression, and the aim of the decompression tables and algorithms was to prevent bubble formation, while minimising decompression time. Most dissolved phase models are perfusion limited, and differ mainly by the number of compartments, range of half times, and supersaturation tolerances assumed. These models are commonly referred to as Haldanean.
Haldane's theory and tables
John Scott Haldane was commissioned by the Royal Navy to develop a safe decompression procedure. The current method was a slow linear decompression, and Haldane was concerned that this was ineffective due to additional nitrogen buildup in the slow early stages of the ascent.[118]
Theory
Haldane's hypothesis was that a diver could ascend immediately to a depth where the supersaturation reaches but does not exceed the critical supersaturation level, at which depth the pressure gradient for off-gassing is maximised and the decompression is most efficient. The diver would remain at this depth until saturation had reduced sufficiently for him to ascend another 10 feet, to the new depth of critical supersaturation, where the process would be repeated until it was safe for the diver to reach the surface. Haldane assumed a constant critical ratio of dissolved nitrogen pressure to ambient pressure which was invariant with depth.[118]
Experimental work
Large number of decompression experiments were performed using goats, which were compressed for three hours to assumed saturation, rapidly decompressed to surface pressure, and examined for symptoms of decompression sickness. Goats which had been compressed to 2.25 bar absolute or less showed no signs of DCS after rapid decompression to the surface. Goats compressed to 6 bar and rapidly decompressed to 2.6 bar (pressure ratio 2.3 to 1) also showed no signs of DCS. Haldane and his co-workers concluded that a decompression from saturation with a pressure ratio of 2 to 1 was unlikely to produce symptoms.[119]
Haldane's model
The decompression model formulated from these findings made the following assumptions.
- Living tissues become saturated at different rates in different parts of the body. Saturation time varies from a few minutes to several hours
- The rate of saturation follows a logarithmic curve, and is approximately complete in 3 hours in goats, and 5 hours in humans.
- The desaturation process follows the same pressure/time function as saturation (symmetrical), provided no bubbles have formed
- The slow tissues are most important in avoiding bubble formation
- A pressure ratio of 2 to 1 during decompression will not produce decompression symptoms
- A supersaturation of dissolved Nitrogen that exceeds twice ambient atmospheric pressure is unsafe
- Efficient decompression from high pressures should start by rapidly halving the absolute pressure, followed by a slower ascent to ensure that the partial pressure in the tissues does not at any stage exceed about twice the ambient pressure.
- The different tissues were designated as tissue groups with different half times, and saturation was assumed after four half times (93.75%)
- Five tissue compartments were chosen, with half times of 5, 10, 20, 40 and 75 minutes.[120]
- Depth intervals of 10 ft were chosen for decompression stops.
Decompression tables
This model was used to compute a set of tables. The method comprises choosing a depth and time exposure, and calculation the nitrogen partial pressure in each of the tissue compartments at the end of that exposure.
- The depth of the first stop is found from the tissue compartment with the highest partial pressure, and the depth of first decompression stop is the standard stop depth where this partial pressure is nearest without exceeding the critical pressure ratio.
- The time at each stop is the time required to reduce partial pressure in all compartments to a level safe for the next stop, 10 ft shallower.
- The controlling compartment for the first stop is usually the fastest tissue, but this generally changes during the ascent, and slower tissues usually control the shallower stop times. The longer the bottom time and closer to saturation of the slower tissues, the slower the tissue controlling the final stops will be.
Chamber tests and open water dives with two divers were made in 1906. The divers were successfully decompressed from each exposure. The tables were adopted by the Royal Navy in 1908. The Haldane tables of 1906 are considered to be the first true set of decompression tables, and the basic concept of parallel tissue compartments with half times and critical supersaturation limits are still in use in several later decompression models, algorithms, tables and decompression computers.[121]
US Navy decompression tables have gone through a lot of development over the years. They have mostly been based on parallel multi-compartment exponential models. The number of compartments has varied, and the allowable supersaturation in the various compartments during ascent has undergone major development based on experimental work and records of decompression sickness incidents.
C&R tables (1915)
The first decompression tables produced for the U.S.Navy were developed by the Bureau of Construction and Repair in 1915 and were consequently known as the C&R tables. They were derived from a Haldanean model, with oxygen decompression to depths up to 300fsw on air, and were successfully used to depths of slightly over 300fsw[122]
Hawkins Schilling and Hansen (1930's)
Submarine escape training led US Navy personnel to believe that Haldane's allowable supersaturation ratios for fast tissues were unnecessarily conservative, as calculated values indicated that supersaturation in trainees exceeded Haldane's limits, but they did not develop DCS.
A large number (2143) of experimental dives were conducted over 3 years to derive allowable supersaturation ratios for a Haldanian 5 compartment model with compartment half-times of 5, 10, 20, 40 and 70 minutes. Values for critical supersaturation derived from this experimental work were different for each tissue compartment. Values for slow tissues (75 and 40 minute) were close to Haldane's findings, but considerably higher values were found for the fast tissues. These values were so high that the researchers concluded that the 5 and 10 minute tissues were not relevant to the development of DCS. Based on these conclusions, a set of tables was computed which omitted the 5 and 10 minute tissues.[106]
Yarborough (1937 tables)
Yarborough's 1937 tables were based on a Haldanean 3 compartment model with compartment half-times of 20, 40 and 70 minutes. Ascent rate was chosen to be 25 ft per minute, which was a convenient rate to pull up a diver in standard dress.[106]
1956 tables
Van der Aue worked on procedures for surface decompression and oxygen us in the early 1950s and during this research found problems with the 1937 tables for long dive times. He also found that the fast tissues which had been dropped in the 1930s would control decompression in some cases, so re-introduced the fast compartments to the model, and added a extra slower compartment to better model long duration dives.[123]
Assumptions of the 1956 model:[123]
- 6 parallel tissue compartments with exponential uptake and elimination of gas with compartment half times of 5, 10, 20, 40, 80 and 120 minutes.
- Symmetrical uptake and elimination half times (same half time for each compartment for uptake and elimination)
- Supersaturation ratios decrease linearly with increased ambient pressure, (M-values) and are different for each compartment.
- Each tissue compartment is assumed to fully saturate/desaturate in 6 half times. This means desaturation of the slowest (120min) compartment takes 12 hours – hence the 12 hour surface interval before a dive is not considered repetitive with these tables.
Ascent rate was chosen at 60fsw/min as a compromise between the practical requirements for military scuba and surface supplied diving operations.[124]
Repetitive diving was accommodated in the tables using the slowest compartment to control surface off-gassing.[125]
A minimum surface interval of 10 minutes was found necessary to ensure that the 120 minute compartment would have controlling effect for repetitive dives.[52]
The US Navy 1956 tables were soon found to be problematic for dives deeper than 100fsw for longer than 2 to 4 hours.
US Navy exceptional exposure tables use an 8 compartment Haldanean model developed by Workman, with half times of 5, 10, 20, 40, 80, 120, 160 and 240 minutes, and are not compatible with the rest of the US Navy Air tables for repetitive diving, although for convenience they have been appended to the standard US Navy Air tables.[126] The tables warn that no repetitive diving is permitted following an exceptional exposure dive, and although the 240 minute tissue would only desaturate completely in 24 hours, there is no restriction to assuming an unsaturated diver after 12 hours.[127]
Some of the earliest modifications to the U.S. Navy tables involved changes to their layout by the recreational diving community. These include:[128]
- Nu-Way repetitive dive tables
- Dacor "No calculation dive tables"
Decompression theory is not an exact science. Decompression models approximate a physiological process that is incompletely understood, and rather complex, by simple mathematical models, in the hope of producing a useful procedure with acceptably low risk of injury to the user. New information allows theories and models to be modified to provide more reliable results, and the availability of faster and more powerful computer processors at low cost has made more exhaustive numerical methods more practicable, and the computation of relatively far more complex models is now quite possible, even in real time.
Several factors have encouraged researchers to modify existing tables and develop new models:
- Doppler bubble detection allows models to use bubble formation as an endpoint rather than symptomatic DCS.
- The use of safety stops has been shown by Dr Andrew Pilmanis of the Catalina Marine Science Centre to greatly reduce bubble formation in divers.
- Many decompression models use a slower ascent rate than the 60fpm (18m/min) of the 1956 US Navy tables (The 2008 US Navy tables have reduced ascent rate to 30fpm (9m/min)).[81]
- Multiple repetitive dives. The US Navy tables were designed for a single repetitive dive, and there were concerns about the safety of extending their use to multiple repetitive dives.As an attempt to address this issue, some tables were modified to reduce the allowable bottom time for repetitive dives.
- Longer nitrogen retention. Addition of longer half-time compartments allows the accumulation of residual nitrogen over longer periods to be accounted for.
Jeppesen tables
Jeppesen made the simplest modification to the U.S. Navy tables by drawing a new line to reduce no-stop limits on an otherwise unchanged table. Divers were recommended to remain within the modified no-stop limit. If one of the new time limits was not listed on the U.S. Navy table, the next shorter table entry was to be selected.[129]
Bassett tables
These tables were based on the 1956 US Navy tables and the no-decompression limits recommended by Bruce Bassett.[66]
Changes were also made to the table rules and decompression requirements:
- Ascent rate of 10m per minute.
- A safety stop of 3 to 5 minutes at 3 to 5 metres is recommended where possible for all dives deeper than 9msw.
- Total dive time is used to calculate repetitive group.
NAUI tables
The first NAUI tables were based on unmodified US Navy 1956 tables and issued in the early 1980's.[citation needed] The next version was a NAUI modification of the US Navy 1956 tables using the following modifications,[66] and released a few years later.
- No decompression limits have been reduced. In most cases this results in the repetitive group shifting one letter down, but for 50fsw it shifted 2 letters, and for 40fsw, by three letters.
- A precautionary decompression stop (safety stop) of 3 minutes at 15fsw is recommended after all dives, but the time spent at the safety stop is not included in the time used to calculate repetitive group.
- A surface interval of at least one hour between repetitive dives is recommended.
- Repetitive dive depths are limited to 100fsw
- A repetitive dive is defined as occurring within 24 hours of the previous dive (this allows for the slowest tissues to equilibriate with atmospheric partial pressures)
- All required decompression is done at a stop depth of 15fsw
NAUI adapted the 1995 DCIEM Sports Table for use in all NAUI courses and these were used until they were replaced by RGBM based tables in 2002.[130] (The NAUI recreational air tables based on RGBM model are copyrighted 2001)[131]
NAUI RGBM Trimix and Nitrox tables copyrighted 1999 have also been released.[132]
Pandora tables
These tables were designed for use on the excavation of the wreck of the Pandora[66]
- Table values at 30 fsw and deeper were shortened by 1 to 4 minutes, putting divers into higher repetitive groups sooner.
- Repetitive group selection tables for repetitive dives were modified. The first repetitive dive uses the same repetitive group selection as the U.S. Navy tables but subsequent dives use more conservative tables which place the diver in a higher repetitive group than the Navy tables would for the same profile. This tendency is continued for the third and fourth repetitive dives.
- Safety stops at 3 msw (10 fsw) are required for repetitive dives; 3 minutes is required after the second dive, 6
minutes after the third and 9 minutes after the fourth dive.
- Maximum ascent rate was specified as 10 msw/min. (35 fsw/min.).
Huggins model and tables
In 1981 Karl Huggins modified the US Navy 6 compartment model using M values derived to follow the Spencer no-decompression limits. The tables are exclusively for no-decompression diving and are presented in the same format as the US Navy tables.
A major difference from the US Navy tables is that the repetitive group designators represent nitrogen levels in all tissues, unlike the USN table which represent only the 120 minute compartment. The Huggins repetitive group indicates a percentage of the M0 for the most saturated tissue, and this is intended to make the tables more applicable to multilevel diving procedures.
The Huggins tables have not been officially tested, but are more conservative than the 1956 US Navy tables. They have been calculated from limits which would theoretically produce venous bubbles 10 to 20% of the time.[133]
PADI Recreational Dive Planner
The PADI tables known as the PADI Recreational Dive Planner (RDP)were developed by Raymond Rogers and tested by DSAT (Diving Science And Technology, an affiliate of PADI Inc.). The M values were derived from Spencer's no-stop limits and the repetitive group designators were based on a 60 minute tissue compartment. This combination resulted in more conservative first dives, but less conservative repetitive dives.
The RDP tables were developed for no-stop diving, but recommend a safety stop at 15fsw for 3 minutes. Emergency decompression for dives which inadvertently exceed the no-stop limit is specified.
The RDP tables are available in two formats:
- A regular table
- "The Wheel", Which is a circular slide-rule type calculator, and allows depths to be read to 5fsw inervals, and times to the nearest minute.
The RDP was tested for single day multi-level dives and multi-day dives with multiple dives per day. There were no incidences of symptomatic DCS during testing.[134]
Buhlmann tables
Professor A.A. Buhlmann of the Laboratory of Hyperbaric medicine of the Medical Clinic of the University of Zurich developed the Swiss tables, more often referred to as Buhlmann tables, in the early 1960s. The model is Haldanian, with 16 tissue compartments with half times from 2.65 minutes to 635 minutes, each with with linearly varying supersaturation limits depending on the tissue and the ambient pressure, and is based on absolute pressures, which simplifies application to altitude diving.
The full set of Swiss Tables consists of tables for four altitude ranges: 0 to 700m, 701 to 1500m, 1501 to 2500m and 2501 to 3500m. Ascent rate was chosen as 10m per minute
No stop limits and decompression schedules tend to be more conservative than the US Navy air tables.
The Swiss tables use the 80 minute tissue compartment for control of repetitive dive calculations, which tends to be less conservative than the US Navy tables for this application.[53]
Modified Buhlmann tables
Swiss sport diving tables
In 1986 the Buhlmann model was used to generate dive tables for recreational divers. One set was for altitudes from 0 to 700m above sea level (0 to 2300 ft.) and other for altitudes from 701 to 2500m (2301 to 8200 ft.). The repetitive group designators are based on the 80-minute compartment.[65]
Buhlmann/Hann tables (German)
The German tables were developed by Dr. Max Hann using a derivative of the Buhlmann model. Three sets were published for altitude ranges 0-25Om, 201-70Om, and 701-1,200m. The repetitive group designators are based on the 80-minute compartment.
Safety factors were added to the depths on the table to take into account depth gauge errors. The depth used for calculations was 2.4% greater than the actual depth for the two lower altitude tables, and 3% + 1 msw greater than actual depth on the highest altitude table.[65]
The mathematical model used for the development of the MN 90 tables is Haldanian, and was also used for the GERS (Groupe d’Etudes et Recherches Sous-marines) 1965 table.[64]
Haldane's assumptions about the limiting factors for ascent are:
- gas exchange in decompression is symmetrical with compression
- the role of bubbles in the modification of blood-tissue exchange is neglected,
- normal decompression does not produce bubbles: DCS occurs when bubbles appear,
- bubbles appear in a compartment where the ratio of the dissolved gas pressure and ambient hydrostatic pressure reaches a critical value, characterizing the maximum tolerable pressure compartment.
Specific assumptions and conditions for use of the MN90 model and tables are as follows:
- For Scuba dives using air as the breathing gas at sea level, with the diver initially saturated at atmospheric pressure
- 12 parallel tissue compartments with half times from 5 to 120 minutes, each with its own critical ratio
- The ascent rate used is 15 to 17 metres per minute to the first stop, which is the same as used in the GERS 1965 tables. From the first stop to the surface this is reduced to 6 m/min
- The reference population with respect to physiology is based on 1095 medically fit divers from the French Navy in 1988:
- weight 74 kg plus or minus 8 kg,
- height 175.9 plus or minus 5.7 cm,
- age 32.3 plus or minus 6.1 years.
- Only the 120 minute tissue is used for calculation of residual nitrogen for repetitive dives. Letter groups are used to indicate the residual gas content of the 120 minute tissue. Letter groups are modified according to surface interval. A residual nitrogen time is found from the repetitive group and the repetitive dive depth which is to be added to the planned bottom time.
- Decompression stops are at 3m intervals
- The tables have been validated by experimental dives and modified where necessary.
- The maximum permitted depth for use of air is 60 m. The data for the decompression depths of 62 m and 65m are included in the table in case of accidentally exceeding the depth limit of 60 m.
- Only one repetitive dive is allowed as there is no validation data for multiple repetitive dives
- Altitude corrections are available
- The tables can be used for Nitrox by calculating equivalent air depth
- Oxygen may be used to accelerate decompression in-water at depths not exceeding 6m
- An unusual feature of these tables is a table for reduction of residual nitrogen by breathing pure oxygen on the surface between dives.
Non-Haldanean dissolved phase models
In the early 1950s Hempleman developed a diffusion limited model for gas transfer from the capillaries into the tissues (Haldanian model is perfusion model). The basis for this model is radial diffusion from a capillary into the surrounding tissue, but by assuming closely packed capillaries in a plane the model was developed into a "tissue slab" equivalent to one dimensional linear bulk diffusion in two directions into the tissues from a central surface.
The 1972 RNPL tables were based on a modified Hempleman tissue slab model, and are more conservative than the US Navy tables.[117]
A version of the RNPL tables were used by the British Sub Aqua Club until the production of the BSAC'88 tables in 1988.
DCIEM model and tables
In the mid 1960's, the Canadian Defence and Civil Institute of Environmental Medicine developed the Kidd/Stubbs serial decompression model. This differs from Haldanian models which are parallel models, and assume that all compartments are exposed to ambient partial pressures and no gas interchange occurs between compartments. A serial model assumes that the diffusion takes place through a series of compartments, and only one is exposed to the ambient partial pressures, and is in effect a compartmentalised version of the Hempelman bulk diffusion slab model.[30]
The Kidd/Stubbs model has four serial compartments,[135] each with a half time of approximately 21 minutes. Allowable surfacing supersaturation ratios for the initial two compartments are taken as 1.92 and 1.73, while the gas concentration in the last two compartments is not considered in the computation.
DCIEM has continuously evaluated and modified the model over the years. A revised set of tables was released in 1984, based on thousands of Doppler evaluated dives.[30] The DCIEM 1983 decompression model is a decompression calculation model rather than a physiological model.[135] Modifications were made to the model to get it to fit observed data, as the original model had several observed shortcomings, while retaining the basic model structure so that it could be applied to existing hardware with minimal modifications.
Mixed phase models (dissolved and bubble phases)
Tables du Ministère du Travail
Tables du Ministère du Travail 1974 (MT74)
The first French official (civilian) air decompression tables were published in 1974 by the Ministère du Travail [136][39]
Tables du Ministère du Travail 1992 (MT92)
In 1982, the French government funded a research project for the evaluation of the MT74 tables using computer analysis of the dive report database, which indicated that the MT74 tables had limitations for severe exposures.[137] The government then supported a second project to develop and validate new tables [138]. A complete set of air tables, with options of pure oxygen breathing at 6m (surface supplied), at 12 m (wet bell), surface decompression, split level diving, repetitive diving, etc. was developed in 1983. This early model already implemented the concept of continuous compartment half-times. For the safe ascent criteria, the Arterial Bubble model was not derived mathematically, but an approximation was defined empirically by fitting mathematical expressions to selected exposures from the Comex database. At the time, the best fit was obtained by the expression now called AB Model-1, which was used to compute a set of decompression tables that was evaluated offshore on selected Comex worksites. In 1986, after some minor adjustments, the tables were included in the Comex diving manuals and used as standard procedures. In 1992, the tables were included in the new French diving regulations under the name of Tables du Ministère du Travail 1992 or MT92 tables[139]
The arterial bubble decompression model
The arterial bubble assumption is that the filtering capacity of the lung has a threshold radius of the size of a red blood cell and that sufficiently small decompression bubbles can pass to the arterial side, especially during the initial phase of ascent. Later in the ascent, bubbles grow to a larger size and remain trapped in the lung. This may explain why conventional Doppler measurements have not detected any bubbles in the arterial circulation.[39]
The arterial bubble assumption can introduce variability in the decompression outcome through the lung function. The first variable is individual susceptibility. The filtering capacity of the lung may be assumed to vary between individuals, and for a given individual, from day to day, and may account for the inter-personal and intra-persona variability which have been observed in DCS susceptibility. Basically, a good diver is a good bubble filter. This is a justification for divers who seek top physical fitness for severe decompression exposures.
The second variable is related to dive conditions and speculates an influence of CO2 on the lung filter. Raised levels of CO2 could decrease the lungs' filtration capacity and allow bubbles to pass to the arterial side of the circulation. Thus diving situations associated with CO2 retention and hypercapnia would be associated with a higher risk of Type II DCS. This could explain why the following situations, which are all related to high levels of CO2, have been identified as contributing factors to DCS:[39]
- anxiety and stress,
- exhaustion or hyperventilation due to intense activity,
- cold,
- high work of breathimg.
The arterial bubble assumption is also consistent with accidental production of arterial bubbles. One scenario considers a shunt at the heart or lung level that passes bubbles from the venous to the arterial side. A PFO is thought to only open in certain conditions.[140][141] A PFO conveniently explains neurological accidents after recreational air diving without any procedure violation, but it does not explain vestibular hits in deep diving. Vestibular symptoms can appear very early in the decompression, long before the massive bubble production required to overload the system.
A second scenario considers pressure increases during decompression that reduce bubble diameters. This can allow bubbles trapped in the lung during a normal decompression to suddenly pass through the capillaries and become responsible for Type II DCS symptoms. This could explain the difference in outcomes of in-water decompression versus surface decompression[142]. Data collected in the North Sea have shown that if the overall incidence rate of the two diving methods is about the same, that surface decompression tends to produce ten times more type II DCS than in-water decompression. It is assumed that when the diver ascends to the surface, bubbles are produced that are trapped by the lung capillaries, and on recompression of the diver in the deck chamber, these bubbles are reduced in diameter and pass to the arterial side, later causing neurological symptoms. The same scenario was proposed for type II DCS recorded after sawtooth diving profiles or multiple repetitive dives.
The arterial bubble assumption also provides an explanation for the criticality of the initial ascent phase. Bubbles associated with symptoms are not necessarily generated on site. There is an growth process at the beginning of the ascent that may last for several cycles until the bubbles have reached a critical size, when they are either filtered in the lung or stopped at the tissue level. It is postulated that the production of a shower of small arterial bubbles during the first minutes of the initial ascent is a precursor for DCS symptoms.
An attempt was made to turn this scenario into a decompression model.
The arterial bubble model assumptions[39]
- A Diver breathes a compressed gas mixture that contains inert gas which dissolves in the various tissues during the pressure exposure. When the ascent is initiated, the inert gas is off-loaded as soon as a suitable gradient is created.
- Bubbles are normally produced in the vascular bed and transported by the venous system to heart, then to the lungs.
- The lungs work as a filter and trap the bubbles in the capillaries which have a smaller diameter. Gas transfer into the alveoli eliminates the bubbles.
- The critical issue is the filtering capacity of the lung system. Small bubbles may pass through the lungs into the systemic circulation.
- At the level of the aortic arch, the distribution of blood likely to carry bubbles to neurological tissue such as the brain or the spinal cord.
- The brain is a fast tissue and might be in supersaturated state in the early phase of decompression. It acts as a gas reservoir and feeds any local bubble which will grow. The bubble may just proceed through the capillaries to the venous side for another cycle, but may be trapped and will then grow in place, causing local restriction of the blood supply and finally ischemia. This may develop into central neurological symptoms.
- Similarly, arterial bubbles may reach the spinal cord and grow on site from local gas and produce spinal neurological symptoms.
- Much later in the decompression, bubbles may reach a significant size and exert a local deformation, particularly in stiffer tissues such as tendons and ligaments, that excites nerve terminations and produces pain.
Derivation of the Arterial Bubble Model
A model based on the Arterial Bubble assumption (Arterial Bubble model version 2, or AB Model 2) was developed for the calculation of decompression tables. This gas phase model uses an equation which can be compared to a classic "M-value" associated to a corrective factor that reduces the permitted gradient for small values of the compartment time constant.
The consequence is the introduction of deeper stops than a classic dissolved phase decompression model.

The use of simple symmetrical exponential gas kinetics models has shown up the need for a model that would give slower tissue washout.[143] In the early 1980s the US Navy Experimental Diving Unit developed an algorithm using a decompression model with exponential gas absorption as in the usual Haldanian model, but a slower linear release during ascent. The effect of adding linear kinetics to the exponential model is to lengthen the duration of risk accumulation for a given compartment time constant[143]
The model was originally developed for programming decompression computers for constant oxygen partial pressure closed circuit rebreathers.[144][145] Initial experimental diving using an exponential-exponential algorithm resulted in an unacceptable incidence of DCS, so a change was made to a model using the linear release model, with a reduction in DCS incidence. The same principles were applied to developing an algorithm and tables for a constant oxygen partial pressure model for Heliox diving[146]
The linear component is active when the tissue pressure exceeds ambient pressure by a given amount specific to the tissue compartment. When the tissue pressure drops below this cross-over criterion the tissue is modelled by exponential kinetics. During gas uptake tissue pressure never exceeds ambient, so it is always modelled by exponential kinetics. This results in a model with the desired asymmetrical characteristics of slower washout than uptake.[147] The linear/exponential transition is smooth. Choice of cross-over pressure determines the slope of the linear region as equal to the slope of the exponential region at the cross-over point.
During the development of these algorithms and tables, it was recognized that a successful algorithm could be used to replace the existing collection of incompatible tables for various air and Nitrox diving modes currently in the U. S. Navy Diving Manual with a set of mutually compatible decompression tables based on a single model, which was proposed by Gerth and Doolette in 2007.[148] This has been done in Revision 6 of the US Navy Diving Manual published in 2008, though some changes were made.
An independent implementation of the EL-Real Time Algotithm was developed by Cochran Consulting, Inc. for the diver-carried Navy Dive Computer under the guidance of E. D. Thalmann.[149]
Physiological interpretation
Computer testing of a theoretical bubble growth model reported by Ball, Himm, Homer and Thalmann produced results which led to the interpretation of the three compertments used in the probabilistic LE model, with fast (1.5min), intermediate (51 min) and slow (488min) time constants, of which only the intermediate compartment uses the linear kinetics modification during decompression, as possibly not representing distinct anatomically identifiable tissues, but three different kinetic processes which relate to different elements of DCS risk.[150]
They conclude that bubble evolution may not be sufficient to explain all aspects of DCS risk, and the relationship between gas phase dynamics and tissue injury requires further investigation.[151]
BSAC'88 Tables
The BSAC '88 Tables are published in the form of a booklet of four table sets giving no calculation repetitive diving solutions from sea level to 3000 metres altitude.
Very little information on the theoretical model and algorithm for the BSAC 1988 tables appears to be available. What is known, is that the tables were developed specifically for recreational diving for the British Sub-Aqua Club by Dr Tom Hennessy and were released in 1988.[152]
Also in 1988, a chapter titled Modelling Human Exposure to Altered Pressure Environments, by T.R. Hennessy was published in Environmental Ergonomics,[153] discussing the shortcomings of several decompression models and the associated experimental validation procedures. In this work Hennessy proposes an alternative combined perfusion/diffusion model. The number of compartments discussed ranges fron 4 in model "A", (perfusion limited aqueous tissue, perfusion limited lipid tissue, diffusion limited aqueous tissue and diffusion limited lipid tissue) to 2 in model "B" (where the assumption is made that if there is intravascular undissolved gas (bubbles), the perfusion limited comparments would become diffusion limited).
Hennessy concludes that if the undissolved and dissolved gas content of a tissue cannot be independently measured either directly or indirectly then the safe maximum limits relative to the ambient pressure cannot be accurately determined through decompression trials and it will not be possible to systematically develop a comprehensive biophysical model for gas exchange. He proposes a best fit double compartment model for dissolved gas and a single compartment model for undissolved gas as these are the simplest models consistent with available data.
Varying Permeability Model
This decompression model was developed by D.E. Yount and others at the University of Hawaii to model laboratory observations of bubble formation and growth in both inanimate and in vivo systems exposed to pressure variations. It presumes that microscopic bubble nuclei always exist in aqueous media, including living tissues. These bubble nuclei are spherical gas phases that are small enough to remain in suspension yet strong enough to resist collapse, their stability being provided by elastic surface layer consisting of surface-active molecules with variable gas permeability.[23] These skins resist the effect of surface tension, as surface tension tends to collapse a small bubble by raising internal pressure above ambient so that the partial pressure gradient favours diffusion out of the bubble in inverse proportion to the radius of the surface.
Any nuclei larger than a specific "critical" size, (more physics needed here) will grow during decompression.[citation needed] The VPM aims to limit the cumulative volume of these growing bubbles during and after decompression to a tolerable level by limiting the pressure difference between the gas in the bubbles and the ambient pressure. In effect this is equivalent to limiting the supersaturation, but instead of using an arbitrary linear fit to experimental data, the physics of bubble growth is used to model the acceptable supersaturation for any given pressure exposure history.
Growth in size and number of gas bubbles is computed based on factors representing pressure balances in the bubbles, physical properties of the "skins" and the surrounding environment. If the total volume of gas in the bubbles is predicted to be less than a "critical volume", then the diver is assumed to be within the safe limits of the model.
The bubble model is superposed on a multiple parallel tissue compartment model. Ingassing is assumed to follow the classic Haldanean model.
Bubble population distribution
Bubble size vs number has an exponential distribution[154]
Bubble nucleation
Gas bubbles with a radius greater than 1 micron should float to the surface of a standing liquid, whereas smaller ones should dissolve rapidly due to surface tension. The Tiny Bubble Group has been able to resolve this apparent paradox by developing and experimentally verifying a new model for stable gas nuclei.[155]
According to the varying-permeability model, gas bubble nuclei are simply stable microbubbles. The stability of these microbubbles is due to elastic skins or membranes consisting of surface-active molecules. These skins are normally permeable to gas, and collapse is prevented by their compression strength. These skins can become stiff and effectively impermeable to gas when they are subjected to large compressions, typically exceeding 8 atm, at which stage the pressure inside increases during further compression as predicted by Boyle's law.
Essentially, there are three parameters in the VP model: the compression strength of the skin; the initial radius; and the onset pressure for impermeability.
Ordering hypothesis
The ordering hypothesis states that nuclei are neither created nor destroyed by the pressure schedule, and initial ordering according to size is preserved.
It follows from the ordering hypothesis that each bubble count is determined by the properties and behavior of that one "critical" nucleus which is right at the bubble-formation threshold. All nuclei that are larger than the critical nucleus will form bubbles, and all nuclei that are smaller will not. Furthermore, a family of pressure schedules which yields the same bubble count N is characterized by the same critical nucleus and hence by the same critical radius, the same crumbling compression, and the same onset of impermeability.[21]
Development of decompression model
The original assumption was that bubble number is directly proportional to decompression stress. This approach worked well for long exposures, but not when the exposure time varied considerably.
A better model was obtained by allowing more bubbles to form on the shorter dives than on the longer dives. The constant bubble number assumption was replaced by a "dynamic-critical-volume hypothesis". As in earlier applications of the critical-volume criterion,[156] it was assumed that whenever the total volume of gas phase accumulated exceeds a critical value, signs or symptoms of DCS will appear. In the special case of long exposures the two models are equivalent[157]
The "dynamic" aspect of this hypothesis is that gas is continuously entering and leaving the gas phase.[158]
The accumulated volume is calculated as a function of time by integrating over the product of the bubble number and the degree of supersaturation, and subtracting the free gas that is being dissipated continuously by the lung.[8]
Gas uptake and elimination are assumed to be exponential, as in conventional Haldanean models, and the tissue half-times used range from 1 to 720 min.[158]
As a first approximation only the inert gasses are taken into account. For oxygen partial pressures above 2.4 bar, the quantity of oxygen dissolyed in the arterial blood exceeds the amount that the body can use, and the hemoglobin is saturated with oxygen in both the veins and the arteries. If more oxygen is added, the partial pressure of oxygen in the venous blood rises.[159]
Comparison of VPM profiles with other models
Comparisons of VPM profiles with USN decompression schedules for extreme exposure dives consistently produce similar total ascent times, but significantly deeper first decompression stops.[157]
Reduced Gradient Bubble Model
The RGBM developed by Dr Bruce Wienke at Los Alamos National Laboratory is a hybrid model which modifies a Haldanian model with factors to take some account of bubble mechanics to model gas phase production during decompression. The bubble factor modifies the M-values of the Haldanian model, making it more conservative.
Features of the modifying factor ξ include:[160]
- ξ starts on the first dive of a repetitive series with the maximum value of one, so it will make the model more conservative or unchanged.
- ξ decreases for repetitive dives.
- ξ decreases as exposure time increases.
- ξ increases with increased surface interval.
- ξ modifies fast compartments more than slow compartments.
- ξ decreases with the depth of a dive segment
- ξ has more effect on repetitive dives which are deeper than previous dives in the series.
The effect is to reduce no-stop dive time or increase decompression requirements for repetitive dive in the following categories:
- Following a short surface interval.
- Following a long dive.
- Following a deep dive.
- Which are deeper than previous dives.
The model has been used to some extent in some Suunto dive computers,[161] and in the HydroSpace Explorer computer, where it is a user selected option[162] for computation formula, with a choice of additional conservatism factors.
The complete RGBM treats coupled perfusion-diffusion transport as a two stage process, with perfusion providing as a boundary condition for gas penetration of the tissues by diffusion. Either process can dominate the exchange depending on time and rate ceofficents.
Simplified implementations which require less computational power are available for use in personal decompression computers. These are dominated by perfusion. The inherent biological unsaturation of tissues is considered in the calculations.[10]
The model assumes that bubble nuclei are always present in a specific size distribution, and that a certain number are induced to grow by compression and decompression. An iterative computation is used to model ascent to limit the combined volume of the gas phase. Gas mixtures of helium, nitrogen, and oxygen contain bubble distributions of different sizes, but the same phase volume limit is used.[163]
The model postulates bubble nuclei with aqueous and/or lipid skin structure, in a number and size distribution quantified by an equation-of-state. Like the VPM, RGBM assumes the size distribution is exponentially decreasing in size. Unlike the varying permeability model, bubble seeds are assumed permeable to gas transfer across skin boundaries under all pressures.
The size of nuclei which will grow during decompression is inversely proportional to the supersaturation gradient.
At higher pressures, skin tension of the bubble nuclei reduces gas diffusion to a slower rate. The model assumes that bubble skins are stabilized by surfactants over calculable times scales, which results in variable persistence of the bubble nuclei in the tissues.[163]
Modifications to models and algorithms for diluent gases other than nitrogen
Decompression models and algorithms developed for binary mixtures of nitrogen and oxygen can not be used for gases containing significant amounts of other diluent gases without modification to take into account the different solubilities and diffusion constants of the alternative or added diluents. It is also highly desirable to test any such modifications, to make sure the schedules produced by them are acceptably safe.
Alternative diluent gases
- Helium is by far the most important of the alternative diluents used to date.
- Hydrogen
- Neon
- Combinations of these gases, particularly the trinary mixtures of helium, nitrogen and oxygen known generically as Trimix.
Decompression models which have been adapted to include alternative and multiple diluents
Commercial diving tables
To a large extent commercial offshore diving uses Heliox tables that have been developed by the major commercial diving enterprises such as Comex, Oceaneering International (OI) Alpha tables, American Oilfield Diving (AOD) Company gas tables, though modifications of the US Navy Partial pressure tables are also used.[165] In 2006 the unmodified US Navy tables (Revision 5) were considered to result in an unacceptably high rate of decompression sickness for commercial applications.[165]
See also
References
- ^ Sport Diving, British Sub Aqua Club, ISBN 0-09-163831-3, page 104
- ^ BSAC '88 Decompression Tables Levels 1 to 4
- ^ Wong, R. M. (1999). "Taravana revisited: Decompression illness after breath-hold diving". South Pacific Underwater Medicine Society Journal. 29 (3). ISSN 0813-1988. OCLC 16986801. Retrieved 8 April 2008.
- ^ Chris W Dueker, MD,‘Scuba Diving in Safety & Health, ISBN 0-9614638-0-5
- ^ Burton, Steve (December 2004). "Isobaric Counter Diffusion". ScubaEngineer. Retrieved 3 February 2011.
- ^ a b Hills, Brian A (1978). "Effect of decompression per se on nitrogen elimination". J Appl Physiol. 45 (6): 916–921. PMID 730597. Retrieved 31 October 2011.
- ^ a b c d e Bühlmann Albert A. (1984). Decompression-Decompression Sickness. Berlin New York: Springer-Verlag. ISBN 0-387-13308-9.
- ^ a b Yount 1991, p. 137
- ^ a b Hills, Brian A (1978). "A fundamental approach to the prevention of decompression sickness". South Pacific Underwater Medicine Society Journal. 8 (2): 20–47. ISSN 0813-1988. OCLC 16986801. Retrieved 31 October 2011.
- ^ a b Wienke 2002, p. 10
- ^ Behnke, Albert R (1967). "The isobaric (oxygen window) principle of decompression". Trans. Third Marine Technology Society Conference, San Diego. The New Thrust Seaward. Washington DC: Marine Technology Society. Retrieved 19 June 2010.
{{cite conference}}: Unknown parameter|booktitle=ignored (|book-title=suggested) (help) - ^ Van Liew, Hugh D; Conkin, J; Burkard, ME (1993). "The oxygen window and decompression bubbles: estimates and significance". Aviation, Space, and Environmental Medicine. 64 (9): 859–65. ISSN 0095-6562. PMID 8216150.
- ^ Huggins 1992, chpt. 1 page 7
- ^ a b c Boycott, AE; Damant, GCC; Haldane, John Scott (1908). "Prevention of compressed air illness". Journal of Hygiene. 8 (3): 342–443. doi:10.1017/S0022172400003399. PMC 2167126. PMID 20474365. Retrieved 30 May 2010.
- ^ Beresford, M.: CMAS-ISA Normoxic Trimix Manual
- ^ Workman, Robert D (1957). "Calculation of air saturation decompression tables". Navy Experimental Diving Unit Technical Report. NEDU-RR-11-57. Retrieved 31 October 2011.
- ^ Baker, Erik (1998). "Understanding M-values". Immersed. 3 (3): 23–27.
- ^ Matti Anttila, Gradient Factors, http://www.diverite.com/education/rebreather/tips/gradient%20factors/ accessed May 2, 2012
- ^ a b c d LeMessurier and Hills. (1965) Decompression Sickness. A thermodynamic approach arising from a study on Torres Strait diving techniques. Hvalradets Skrifter, Nr. 48, 54-84.
- ^ a b c d Yount 1991, p. 131
- ^ a b Yount 1991, p. 132
- ^ Hills BA (1992). "A hydrophobic oligolamellar lining to the vascular lumen in some organs". Undersea Biomed Res. 19 (2): 107–20. PMID 1561717. Retrieved 31 October 2011.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ a b c d Yount 1991
- ^ Yount 1991, pp. 131, 136
- ^ a b c d Hamilton, Robert W; Thalmann, Edward D (2003). "Decompression Practice". In Brubakk, Alf O; Neuman, Tom S. Bennett and Elliott's physiology and medicine of diving (5th ed.). United States: Saunders. pp. 477–8. ISBN 0-7020-2571-2. OCLC 51607923
- ^ a b c d Lambertson, Christian J (1989). Relations of isobaric gas counterdiffusion and decompression gas lesion diseases. In Vann, RD. "The Physiological Basis of Decompression". 38th Undersea and Hyperbaric Medical Society Workshop UHMS Publication Number 75(Phys)6-1-89. http://archive.rubicon-foundation.org/6853. Retrieved 10 January 2010.
- ^ a b c D'Aoust, BG; White, R; Swanson, H; Dunford, RG; Mahoney, J (1982). "Differences in Transient and Steady State Isobaric Counterdiffusion". Report to the Office of Naval Research. http://archive.rubicon-foundation.org/4629. Retrieved 10 January 2010.
- ^ a b Doolette, David J; Mitchell, Simon J (June 2003). "Biophysical basis for inner ear decompression sickness". Journal of Applied Physiology 94 (6): 2145–50. doi:10.1152/japplphysiol.01090.2002 (inactive 2010-01-09). PMID 12562679. http://jap.physiology.org/cgi/pmidlookup?view=long&pmid=12562679. Retrieved 10 January 2010.
- ^ a b c Burton, Steve (December 2004). "Isobaric Counter Diffusion". ScubaEngineer. http://www.scubaengineer.com/isobaric_counter_diffusion.htm. Retrieved 10 January 2010.
- ^ a b c d Huggins 1992, chpt. 4 page 6
- ^ a b c d e f g Vann, R.D.(ed) (1989), The Physiological basis of decompression: an overview. pp1-10, Proceedings of the thirty-eighth undersea and hyperbaric medical sociaty workshop, Undersea and Hyperbaric Midical Society, bethesda, Maryland. http://archive.rubicon-foundation.org/6853
- ^ Moon, Richard E; Kisslo, Joseph (1998). "PFO and decompression illness: An update". South Pacific Underwater Medicine Society Journal. 28 (3). ISSN 0813-1988. OCLC 16986801. Retrieved 31 October 2011.
- ^ Scharlin, P.; Battino, R. Silla, E.; Tuñón, I.; Pascual-Ahuir, J. L. (1998). "Solubility of gases in water: Correlation between solubility and the number of water molecules in the first solvation shell". Pure & Appl. Chem. 70 (10): 1895–1904. doi:10.1351/pac199870101895
- ^ Clifford A. Hampel (1968). The Encyclopedia of the Chemical Elements. New York: Van Nostrand Reinhold. pp. 256–268. ISBN 0-442-15598-0.
- ^ Williams, ST; Prior, F; Bryson, PJ (2005), Haematocrit change in recreational Scuba divers following single dive exposure. http://archive.rubicon-foundation.org/1691
- ^ Bookspan, J (2003), "Detection of endogenous gas phase formation in humans at altitude", Medicine & Science in Sports & Exercise Suppl., 35 (5, ): S164, retrieved 7 May 2012
{{citation}}: Text "# 901" ignored (help)CS1 maint: extra punctuation (link) - ^ a b Gorman, Des F (1989). "Decompression tables: their use and problems". South Pacific Underwater Medicine Society Journal. 19 (3): 111–113. Retrieved 31 October 2011.
- ^ a b Gorman, Desmond F; Pearce, A; Webb, RK (1988). "Dysbaric illness treated at the Royal Adelaide Hospital 1987, a factorial analysis". South Pacific Underwater Medicine Society Journal. 18 (3): 95–101.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b c d e JP Imbert, D Paris, J Hugon, Divetech, France. 2004; The Arterial Bubble Model for Decompression Tables Calculations, EUBS 2004, http://gtuem.praesentiert-ihnen.de/tools/literaturdb/project2/pdf/Imbert%20JP.%20-%20EUBS%202004.pdf
- ^ Thalmann 1984, p. 24
- ^ Thalmann 1985, p. 5
- ^ Kindwall, Eric P; Baz, A; Lightfoot, EN; Lanphier, Edward H; Seireg, A (1975). "Nitrogen elimination in man during decompression". Undersea Biomedical Research. 2 (4): 285–297. ISSN 0093-5387. OCLC 2068005. PMID 1226586. Retrieved 31 October 2011.
- ^ Lang, Michael A; Vann, Richard D (1991). Proceedings of the AAUS Repetitive Diving Workshop. Duke University, Durham, NC: American Academy of Underwater Sciences. p. 339. Retrieved 31 October 2011.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ^ Cole, Bob (2008). "Diver Behaviour – Micro-bubble Control". SAA Buhlmann Deep Stop System Handbook. Sub-Aqua Association. p. 4-2. ISBN 0-9532904-8-4.
The SAA recommends that you to [sic] take at least the seventh day off to allow your body to off-gas and return to some level of normality
- ^ a b Doolette David J (2005). "Development and testing of deterministic and probabilistic decompression models". South Pacific Underwater Medicine Society Journal. 35 (1). Retrieved 10 January 2012.
- ^ "Decoweenie Manual" (PDF). decoweenie.com. Retrieved 26 September 2008.
- ^ Pyle, Richard L (27 September 2007). "Deep Decompression Stops". Bishop Museum. Retrieved 9 September 2009.
- ^ Pyle, Richard L (1997). "The importance of deep safety stops: Rethinking ascent patterns from decompression dives". South Pacific Underwater Medicine Society Journal (reprinted from: Deep Tech). 27 (2). Retrieved 31 October 2011.
- ^ a b c d e f Brubakk, A. O. (2003). Bennett and Elliott's physiology and medicine of diving, 5th Rev ed. United States: Saunders Ltd. ISBN 0-7020-2571-2.
{{cite book}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) Cite error: The named reference "Brubakk" was defined multiple times with different content (see the help page). - ^ a b Huggins 1992, chpt. 3 page 13
- ^ a b Huggins 1992, chpt. 4 pages 2-3
- ^ a b c d Paul J. Sheffield, D.Richard D. Vann, (2002), Flying After Recreational Diving Workshop Proceedings, Divers Alert Network, Durham, North Carolina. http://archive.rubicon-foundation.org/xmlui/handle/123456789/5611 Accessed 2012-02-06
- ^ Bühlmann, Albert A (1995). Tauchmedizin (in German). Berlin: Springer-Verlag. ISBN 3-540-55581-1.
- ^ Bühlmann, Albert A (1992). Tauchmedizin: Barotrauma Gasembolie Dekompression Dekompressionskrankheit (in German). Berlin: Springer-Verlag. ISBN 3-540-55581-1.
- ^ Deco for divers, "Other decompression models"; page 203
- ^ Adkisson, G (1991). "The BS-AC '88 decompression tables". South Pacific Underwater Medicine Society Journal. 21 (1). Retrieved 10 January 2012.
- ^ a b Hamilton Jr RW, Rogers RE, Powell MR (1994). "Development and validation of no-stop decompression procedures for recreational diving: the DSAT recreational dive planner". Tarrytown, NY: Diving Science & Technology Corp. Retrieved 15 June 2008.
{{cite journal}}: Cite journal requires|journal=(help)CS1 maint: multiple names: authors list (link) - ^ Deco for divers, "Other decompression models"; page 209-13
- ^ Nishi, RY; Tikuisis, P (1996). "Current Trends in Decompression Development: Statistics and Data Analysis". Defence R&D Canada Technical Report. DCIEM-96–R-65. Retrieved 10 January 2012.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Jean-Noël Trucco, avec le concours de Jef Biard, Jean-Yves Redureau et Yvon Fauvel, (1999): Table Marine National 90 (MN90), Version du 03/05/1999, F.F.E.S.S.M. Comité interrégional Bretagne & Pays de la Loire; Commission Technique Régionale. (in French) http://www.acb-plongee.com/site/formation/pdf/theorie/tables_mn90.pdf
- ^ a b c d e f g h Huggins 1992, chpt. 4 page 11
- ^ a b c d e Huggins 1992, chpt. 4 page 10
- ^ Huggins 1992, chpt. 4 page 15
- ^ Duis, D. (1991). "Using the Recreational Diver Planner for multi-level diving". In: Hans-Jurgen, K; Harper Jr, DE (eds.) International Pacifica Scientific Diving... 1991. Proceedings of the American Academy of Underwater Sciences Eleventh Annual Scientific Diving Symposium held 25–30 September 1991. University of Hawaii, Honolulu, Hawaii. Retrieved 17 October 2011.
- ^ Departure - Dive Planning and Decompression software
- ^ DecoPlanner, decompression simulation software
- ^ GAP-software, decompression simulation software
- ^ Ultimate Planner - decompression planning software tool http://www.techdivingmag.com/ultimateplanner.html
- ^ a b c Huggins 1992, Introduction page 1
- ^ Huggins 1992, Introduction page 3
- ^ Huggins 1992, Introduction page 2
- ^ Lang, M.A. and Hamilton, Jr R.W. (1989). Proceedings of the AAUS Dive Computer Workshop. United States: USC Catalina Marine Science Center. p. 231. Retrieved 7 August 2008.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ^ Uguccioni, DM (1984). Doppler Detection of Silent Venous Gas Emboli in Non-Decompression Diving Involving Safety Stops. Wilmington, NC: University of North Carolina at Wilmington. Retrieved 25 April 2008.
- ^ a b Boycott, A. E. (1908). "The Prevention of Compressed-air Illness". J. Hygiene. 8 (3): 342–443. doi:10.1017/S0022172400003399. PMC 2167126. PMID 20474365. Retrieved 6 August 2008.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ a b Bert, P. (originally published 1878). "Barometric Pressure: researches in experimental physiology". Translated by: Hitchcock MA and Hitchcock FA. College Book Company; 1943.
{{cite journal}}: Check date values in:|date=(help) - ^ Sport Diving, British Sub Aqua Club, ISBN 0-09-163831-3, page 110
- ^ a b c d US Navy Diving Manual Revision 6 Cite error: The named reference "usn" was defined multiple times with different content (see the help page).
- ^ Doolette, David J; Mitchell, Simon J (2003). "Biophysical basis for inner ear decompression sickness". Journal of Applied Physiology. 94 (6): 2145–50. doi:10.1152/japplphysiol.01090.2002. PMID 12562679. Retrieved 10 January 2010.
{{cite journal}}: Unknown parameter|doi_brokendate=ignored (|doi-broken-date=suggested) (help); Unknown parameter|month=ignored (help) - ^ Deco for divers, "Other decompression models"; pages 213-217
- ^ Moon, RE (2000). "Recompression treatments should be to a pressure equivalent to 18 m depth. (Part 2 of 5 part Pro Con Debate)". South Pacific Underwater Medicine Society Journal. 30 (3). ISSN 0813-1988. OCLC 16986801. Retrieved 8 June 2008.
- ^ Berghage, T. E. (1978). "Recompression treatment tables used throughout the world by government and industry". US Naval Medical Research Center Technical Report. NMRI-78-16. Retrieved 8 June 2008.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ a b Yarbrough, O. D. (1939). "The treatment of compressed air illness using oxygen". J Ind Hyg Toxicol. 21: 213–218. ISSN 0095-9030.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Keays, FJ (1909). "Compressed air illness, with a report of 3,692 cases". Department of Medicine Publications of Cornell University Medical College 2: 1–55.
- ^ Berghage, Thomas E; Vorosmarti Jr, James; Barnard, EEP (1978). "Recompression treatment tables used throughout the world by government and industry". US Naval Medical Research Center Technical Report NMRI-78-16. http://archive.rubicon-foundation.org/3414. Retrieved 25 May 2010.
- ^ Edmonds, Carl (1998). "Underwater oxygen for treatment of decompression sickness: A review". South Pacific Underwater Medicine Society Journal. 25 (3). ISSN 0813-1988. OCLC 16986801. Retrieved 31 October 2011.
- ^ a b c Pyle, Richard L. (1995). "In-water Recompression as an emergency field treatment of decompression illness". AquaCorp. 11. Retrieved 8 June 2008.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ a b c Kay, E (1999). In water recompression. 48th Undersea and Hyperbaric Medical Society Workshop. Vol. UHMS Publication Number RC103.C3. United States: Undersea and Hyperbaric Medical Society. p. 108. Retrieved 8 June 2008.
{{cite book}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ a b Vann, Richard D; Uguccioni, Donna M (eds). "Annual Diving Report:2008 edition" (pdf). Divers Alert Network. Retrieved 1 September 2009.
{{cite journal}}:|author=has generic name (help); Cite journal requires|journal=(help)CS1 maint: multiple names: authors list (link) - ^ Diving Regulations 2001 of the South African Occupational Heath and Safety Act
- ^ "Technical Issues". Newry & Mourne Sub Aqua Club. Retrieved 28 August 2009.
- ^ Jablonski, Jarrod (2006). "Details of DIR Equipment Configuration". Doing it Right: The Fundamentals of Better Diving. High Springs, Florida: Global Underwater Explorers. p. 113. ISBN 0-9713267-0-3.
- ^ Gary Gentile, The Technical Diving Handbook
- ^ Bevan, J. (1999). "Diving bells through the centuries". South Pacific Underwater Medicine Society Journal. 29 (1). ISSN 0813-1988. OCLC 16986801. Retrieved 25 April 2008.
- ^ a b Beyerstein, G (2006). Lang, MA; Smith, NE (eds.). Commercial Diving: Surface-Mixed Gas, Sur-D-O2, Bell Bounce, Saturation. Proceedings of Advanced Scientific Diving Workshop. Washington, DC. Retrieved 12 April 2010.
{{cite conference}}: More than one of|location=and|place=specified (help) - ^ a b c d e f g Acott, C. (1999). "A brief history of diving and decompression illness". South Pacific Underwater Medicine Society Journal. 29 (2). ISSN 0813-1988. OCLC 16986801. Retrieved 10 January 2012.
- ^ a b c Hill, L. (1912). Caisson Sickness. Arnold, London. Cite error: The named reference "Hill1912" was defined multiple times with different content (see the help page).
- ^ a b c Huggins 1992, chpt. 1 page 8
- ^ Butler, WP (2004). "Caisson disease during the construction of the Eads and Brooklyn Bridges: A review". Undersea and Hyperbaric Medicine. 31 (4): 445–59. PMID 15686275. Retrieved 10 January 2012.
- ^ Zuntz, N. (1897); Zur Pathogenese und Therapie der durch rasche Luftdruck-änderungen erzeugten Krankheiten, Fortschr, d. Med. 15, 532-639
- ^ Stillson, GD (1915). "Report in Deep Diving Tests". US Bureau of Construction and Repair, Navy Department. Technical Report. Retrieved 6 August 2008.
- ^ US Navy. "Diving in the U.S. Navy: A Brief History". Retrieved 6 August 2008.
- ^ a b c d Huggins 1992, chpt. 3 page 2
- ^ Davis Jefferson C, Sheffield Paul J, Schuknecht L, Heimbach RD, Dunn JM, Douglas G, Anderson GK (1977). "Altitude decompression sickness: hyperbaric therapy results in 145 cases". Aviation, Space, and Environmental Medicine. 48 (8): 722–30. PMID 889546.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Golding, F Campbell; Griffiths, P; Hempleman, HV; Paton, WDM; Walder, DN (1960). "Decompression sickness during construction of the Dartford Tunnel". British Journal of Industrial Medicine. 17 (3): 167–80. PMC 1038052. PMID 13850667.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Hills, BA (1978). "A fundamental approach to the prevention of decompression sickness". South Pacific Underwater Medicine Society Journal. 8 (2). Retrieved 10 January 2012.
- ^ How, J., West, D. and Edmonds, C. (1976); Decompression sickness and diving, Singapore Medical Journal, Vol. 17, No. 2, June 1976.
- ^ Goodman, MW; Workman, RD (1965). "Minimal-recompression, oxygen-breathing approach to treatment of decompression sickness in divers and aviators". United States Navy Experimental Diving Unit Technical Report. NEDU-RR-5-65. Retrieved 10 January 2012.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Huggins 1992, chpt. 4 page 3
- ^ Graves, DJ; Idicula, J; Lambertsen, Christian J; Quinn, JA (February 1973). "Bubble formation in physical and biological systems: a manifestation of counterdiffusion in composite media". Science 179 (4073): 582–584. doi:10.1126/science.179.4073.582. PMID 4686464. http://www.sciencemag.org/cgi/pmidlookup?view=long&pmid=4686464. Retrieved 10 January 2010.
- ^ Graves, DJ; Idicula, J; Lambertsen, Christian J; Quinn, JA (March 1973). "Bubble formation resulting from counterdiffusion supersaturation: a possible explanation for isobaric inert gas 'urticaria' and vertigo". Physics in medicine and biology 18 (2): 256–264. doi:10.1088/0031-9155/18/2/009. PMID 4805115. http://stacks.iop.org/0031-9155/18/256. Retrieved 10 January 2010.
- ^ Spencer MP (1976). "Decompression limits for compressed air determined by ultrasonically detected blood bubbles". Journal of Applied Physiology. 40 (2): 229–35. PMID 1249001. Retrieved 10 January 2012.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Weathersby, Paul K; Homer, Louis D; Flynn, Edward T (1984). "On the likelihood of decompression sickness". Journal of Applied Physiology. 57 (3): 815–25. PMID 6490468. Retrieved 27 April 2009.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ a b Huggins 1992, chpt. 4 page 4
- ^ a b Huggins 1992, chpt. 2 page 1
- ^ Huggins 1992, chpt. 2 pages 1-2
- ^ Huggins 1992, chpt. 2 pages 2-3
- ^ Huggins 1992, chpt. 2 pages 3-6
- ^ Huggins 1992, chpt. 3 page 1
- ^ a b Huggins 1992, chpt. 3 page 3
- ^ Huggins 1992, chpt. 3 page 9
- ^ Huggins 1992, chpt. 3 page 12
- ^ Huggins 1992, chpt. 4 pages 1-2
- ^ US Navy. US Navy Diving Manual, 5th revision. United States: US Naval Sea Systems Command.
- ^ Huggins 1992, chpt. 4 page 2
- ^ Huggins 1992, chpt. 4 page 9
- ^ Deco for divers, "Other decompression models"; page 213
- ^ http://www.divetable.de/dekotg_e.htm
- ^ Bruce R. Wienke, and Timothy R. O'Leary (2001), Full Up Phase Model Decompression Tables, Advanced Diver Magazine, Issue 5, 2001 Advanced diver magazine, http://www.advanceddivermagazine.com/articles/rgbmphase/rgbmphase.html
- ^ Huggins 1992, chpt. 4 page 12
- ^ Huggins 1992, chpt. 4 page2 12-13
- ^ a b Nishi, Ronald, and Lauchner, G. (1984). "Development of the DCIEM 1983 Decompression Model for Compressed Air Diving". Defence and Civil Institute of Environmental Medicine Technical Report. DCIEM-84–R-44. Retrieved 13 January 2012.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Mesures particulières de protection applicables aux scaphandriers. Fascicule Spécial no 74-48 bis. Bulletin Officiel du Ministère du travail. Imprimerie du Journal Officiel, 26 rue Desaix, 75732 Paris cedex 15.
- ^ Imbert JP, Bontoux M. Safety analysis of French 1974 air decompression tables. Proceedings of the Undersea Medical Society Workshop on Decompression in surface-based diving. Tokyo, Japan, September 12th, 1986.
- ^ Imbert JP, Bontoux M. A method for introducing new decompression procedures. Proceedings of the Undersea Medical Society Workshop on validation of decompression schedules. Bethesda, Maryland, 13-14 February 1987.
- ^ Travaux en Milieu Hyperbare. Mesures particulières de prévention. Fascicule no 1636. Imprimerie du Journal Officiel, 26 rue Desaix, 75732 Paris cedex 15. ISBN 2-11-073322-5.
- ^ Balestra C, P Germonpre, and A Marroni. Intrathoracic pressure changes after Valsalva strain and other maneuvers: implication for divers with patent foramen ovale. Undersea hyperb. Med, 1998. 25(3): page 171-4.
- ^ Germonpre P et al; Patent foramen ovale and decompression sickness in sport divers. J. Appl. Physiol, 1988, 84(5): p1622-6.
- ^ Imbert JP. Decompression tables versus decompression procedures: an analysis of decompression sickness using diving data-bases. Proceedings of the XVIIth annual meeting of Diving and Hyperbaric Medicine, Heraklion, Crete, Greece, 20 September-3 October 1991.
- ^ a b Parker 1992, p. 1
- ^ Thalmann 1984, abstract
- ^ Huggins, 1992 & loc-chpt. 4 page 13
- ^ Thalmann, 1985 & p-6
- ^ Parker 1992, p. 3
- ^ Gerth&Doolette 2007, p. 1
- ^ Gerth&Doolette 2007, p. 2
- ^ Ball 1995, p. 272
- ^ Ball 1995, p. 273
- ^ http://www.bsac.com/shop.asp?section=1362§ionTitle=Decompression+Tables&itemid=1677
- ^ Hennessy T.R. 1988; Modelling human exposure to altered pressure environments. In: Environmental Ergonomics pp. 316 to 331, (eds Mekjavik, IB, Banister, EW, Morrison, JB,). London: Taylor & Francis
- ^ Yount 1991, p. 136
- ^ Yount 1991, p. 130
- ^ Hennessy, T. R. and H. V. Hempleman. 1977. An examination of the critical released gas volume concept in decompression sickness. Proceedings of the Royal Society of London. Series B, 197: 299-313.
- ^ a b Yount 1991, p. 138
- ^ a b Yount, D. E. and D. C. Hoffman. 1986. On the use of a bubble formation model to calculate diving tables. Aviation, Space, and Environmental Medicine, 57: 149-156.
- ^ Yount, D. E. and D. A. Lally. 1980. On the use of oxygen to facilitate decompression. Aviation, Space, and Environmental Medicine, 51: 544-550.
- ^ Huggins 1992, chpt. 4 page 14
- ^ Suunto Reduced Gradient Bubble Model, suunto_brochure.qxd 24.7.2003 11:53 Sivu 2, http://www.suunto.com/za/Sports/Diving/Diving-Academy/suunto-rgbm
- ^ a b HS Explorer Dive Computer Owner's Manual,2003, HydroSpace Engineering, Inc. St. Augustine, FL, http://hs-eng.com
- ^ a b Wienke 2002, p. 11
- ^ http://www.hhssoftware.com/v-planner/
- ^ a b Beyerstein, Gary (2006), Commercial Diving: Surface-Mixed Gas, Sur-D-O2, Bell Bounce, Saturation., New Orleans, La
{{citation}}: Text "accessdate-2012-05-07" ignored (help)CS1 maint: location missing publisher (link)
Sources
- Ball, R; Himm, J; Homer, LD; Thalmann, ED (1995). "Does the time course of bubble evolution explain decompression sickness risk?". Undersea and Hyperbaric Medical Society, Inc. (http://www.uhms.org ). Retrieved 28 January 2012.
{{cite journal}}: External link in|journal= - Gerth, Wayne A; Doolette, David J (2007). "VVal-18 and VVal-18M Thalmann Algorithm - Air Decompression Tables and Procedures". Navy Experimental Diving Unit, TA 01-07, NEDU TR 07-09. Retrieved 27 January 2012.
- Hamilton, Robert W; Thalmann, Edward D (2003). "10.2: Decompression Practice". In Brubakk, Alf O; Neuman, Tom S (eds.). Bennett and Elliott's physiology and medicine of diving (5th Revised ed.). United States: Saunders Ltd. pp. 455–500. ISBN 0-7020-2571-2. OCLC 51607923.
- Huggins, Karl E (1992). "Dynamics of decompression workshop". Course taught at the University of Michigan. Retrieved 10 January 2012.
- Parker, E. C. (1992). "Statistically Based Decompression Tables VIII: Linear Exponential Kinetics". Naval Medical Research Institute Report. 92–73. Retrieved 16 March 2008.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help)CS1 maint: ref duplicates default (link) - Powell, Mark (2008). Deco for Divers. Southend-on-Sea: Aquapress. ISBN 1-905492-07-3.
- Thalmann, E. D. (1984). "Phase II testing of decompression algorithms for use in the U.S. Navy underwater decompression computer". Navy Exp. Diving Unit Res. Report. 1–84. Retrieved 16 March 2008.
{{cite journal}}: CS1 maint: ref duplicates default (link) - Thalmann, E. D. (1985). "Development of a Decompression Algorithm for Constant Oxygen Partial Pressure in Helium Diving". Navy Exp. Diving Unit Res. Report. 1–85. Retrieved 16 March 2008.
{{cite journal}}: CS1 maint: ref duplicates default (link) - US Navy (2008). US Navy Diving Manual, 6th revision. United States: US Naval Sea Systems Command. Retrieved 15 June 2008.
- Wienke, Bruce R; O’Leary, Timothy R (13 February 2002). "Reduced gradient bubble model: Diving algorithm, basis and comparisons" (PDF). Tampa, Florida: NAUI Technical Diving Operations. Retrieved 25 January 2012.
- Yount, DE (1991). "Gelatin, bubbles, and the bends". International Pacifica Scientific Diving... Hans-Jurgen, K; Harper Jr, DE (eds.), (Proceedings of the American Academy of Underwater Sciences Eleventh Annual Scientific Diving Symposium held 25–30 September 1991. University of Hawaii, Honolulu, Hawaii). Retrieved 25 January 2012.
Further reading
- Powell, Mark (2008). Deco for Divers. Southend-on-Sea: Aquapress. ISBN 1-905492-07-3.
- Hills. B. (1966); A thermodynamic and kinetic approach to decompression sickness. Thesis
- Gribble, M. de G. (1960); A comparison of the High-Altitude and High-Pressure syndromes of decompression sickness, Brit. J. industr. Med., 1960, 17, 181.
- Lippmann, John; Mitchell, Simon (2005). Deeper into Diving (2nd ed.). Melbourne, Australia: J L Publications. ISBN 0-9752290-1-X. Section 2 chapters 13–24 pages 181–350
External links
- Dive tables from the NOAA
- German BGV C 23 table, permitting a simplified procedure of decompression planning
- Online dive table calculator