Vortioxetine
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Brintellix |
| Other names | Lu AA21004 |
| License data |
|
| Routes of administration | Oral |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 75% (peak at 7–11 hours) |
| Protein binding | 98% |
| Metabolism | extensive hepatic, primarily CYP2D6-mediated oxidation |
| Elimination half-life | 66 hours |
| Excretion | 59% in urine, 26% in feces |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| ChemSpider | |
| KEGG | |
| ChEBI | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.258.748 |
| Chemical and physical data | |
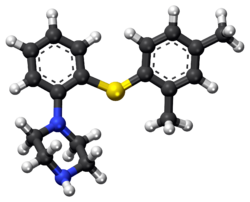
| Formula | C18H22N2S |
| Molar mass | 298.45 g/mol (379.36 as hydrobromide) g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| | |
Vortioxetine (vor-tye-OKS-e-teen, trade name Brintellix (BRIN-tel-ix[2]) and Trintellix in Canada) is an atypical antidepressant (a serotonin modulator and stimulator) made by Lundbeck and Takeda.[3] On September 30, 2013, it was approved by the U.S. FDA for the treatment of major depressive disorder (MDD) in adults.[4] Vortioxetine was also investigated as a treatment for generalized anxiety disorder (GAD) but was not found to be superior to placebo.[5][6]
Following a positive opinion by the Committee for Medicinal Products for Human Use (CHMP) in October 2013,[7] Lundbeck announced December 27, 2013, that European marketing authorization for Brintellix had been obtained.[8]
Indications
Depression
In May 22, 2011, Lundbeck presented the results of four phase III trials on vortioxetine at the 2011 Annual Meeting of the American Psychiatric Association. A statistically significant effect was shown in two of the studies (one for active treatment using the Hamilton Depression Rating Scale (HAM-D), the second as a maintenance treatment), vortioxetine failed to prove superiority over placebo in a third (again using the HAM-D) and the fourth was nullified by an exceptionally high placebo response (according to the Montgomery-Åsberg Depression Rating Scale (MADRS)).[9]
In July 2011, Lundbeck published the results of a double-blind, randomized, placebo-controlled clinical trial with venlafaxine as an active reference. It was found to be superior to placebo in treating MDD.[10] Similarly, in May 2012, Lundbeck published the results of a double-blind, randomized, placebo-controlled clinical trial with duloxetine evaluating vortioxetine in elderly depressed patients, and it was found superior to placebo.[11]
In May 2012, Lundbeck disclosed the results of three phase III clinical trials, showing vortioxetine's superiority over placebo according to the MADRS.[12]
In August 2012, a randomized, double-blind trial confirms the superiority of vortioxetine over placebo according to all measures, except the Sheehan Disability scale.[13]
In September 2012, a randomised, double-blind trial reveals that a dose of 5 mg shows superiority over placebo only in patients that suffer from comorbid anxiety.[14] This is consistent with results from another trial published in December 2012, demonstrating that 2.5 mg and 5 mg doses are ineffective.[15]
Some 2014 studies showed Vortioxetine was effective and well tolerated after inadequate response to SSRI/SNRI,[16] as initial agent up to 20 mg,[17] and as maintenance use lasting 52 weeks.[18]
A 2014 Meta-analysis of 7 randomized trials concluded Vortioxetine had significant reductions vs placebo in depression scores and patients with 50% reduction. Vortioxetine was ranked among 7 antidepressants with different mechanisms, placing vortioxetine greater efficacy than escitalopram, vilazodone, and sertraline with better tolerability,[19] concluding that Vortioxetine has a favorable combination of comparable effect and excellent tolerability.
Anxiety
In August 2012, contradictory results of two randomized, double-blind trial were published. The first demonstrated vortioxetine's superiority over the placebo,[20] but the second showed no efficacy, leading the authors to question the designs of the different trials.[21] Two studies on adult GAD disorders which concluded in 2014 found no effect at 8 weeks with up to 10 mg.[22][23]
Other effects
Vortioxetine enhances some forms of memory in rats.[24] This finding has not been demonstrated in human trials.
Vortioxetine significantly improved objective and subjective measures of cognitive function in adults with recurrent Major Depression Disorder.[25]
Side effects
The most common side effects reported with vortioxetine are nausea, diarrhea, dry mouth, constipation, vomiting, flatulence, dizziness, and sexual dysfunction.[3] Vortioxetine used alone in high dose or in combination with other medications, such as other antidepressants, can produce a potentially life-threatening drug reaction known as serotonin syndrome.[9][11][12]
Incidence of sexual dysfunction is reportedly higher in patients taking vortioxetine than in patients taking placebos,[3] but lower than in patients taking venlafaxine.
Pharmacodynamics
Vortioxetine is a so-called "serotonin modulator and stimulator".Cite error: The <ref> tag has too many names (see the help page). It has been shown to possess the following pharmacological actions:[3][26][27]
- Serotonin transporter (SERT) blocker (i.e. serotonin reuptake inhibitor (SRI)) — Ki (binding affinity) = 1.6 nM, IC50 = 5.4 nM
- Norepinephrine transporter (NET) blocker — Ki = 113 nM
- 5-HT1A receptor high-efficacy partial agonist/near-full agonist — Ki = 15 nM, IA = 80%
- 5-HT1B receptor partial agonist — Ki = 33 nM
- 5-HT1D receptor antagonist — Ki = 54 nM
- 5-HT3A receptor antagonist — Ki = 3.7 nM
- 5-HT7 receptor antagonist — Ki = 19 nM
- β1-Adrenergic receptor ligand — Ki = 46 nM[26]
It has also been shown that vortioxetine increases extracellular levels of acetylcholine and histamine in the rat medial prefrontal cortex following contextual fear conditioning and may be useful in the treatment of Alzheimer's disease.[24]
Pharmacokinetics
Vortioxetine is indicated for the treatment of major depressive disorder (MDD) in the United States and is supplied in 5 mg, 10 mg, 15 mg and 20 mg tablets. The drug reaches peak plasma concentration (Cmax) within 7 to 11 hours post-administration (Tmax), and its mean terminal half-life (t½) is ≈ 66 hours. Steady-state plasma concentrations are typically reached within two weeks. No differences were observed between the fed and fasting states, and therefore it may be taken with or without food at the patient's discretion.[3] It has no active metabolites (i.e. it is not a prodrug).[3]
Patients typically initiate drug therapy at 10 mg daily, which may be subsequently increased to 20 mg daily. In the case that the initial 10 mg dosing is poorly tolerated, the doctor/patient may elect to decrease the maintenance dose to 5 mg per day, though available evidence demonstrating clinical efficacy at this lower dosage is not entirely conclusive and is questionably reliable. Likewise, though the prescribing information invariably recommends that the maintenance dose be increased to 20 mg/day, there is equally unsatisfying data to prove that there is any clinically significant difference in regards to success and remission rates at higher doses.
While linear kinetics follow as expected, actual efficacy figures provided show only fractional improvements in those patients in the group receiving a higher dose of 20 mg/day (based on deviation from baseline, which compare 10 mg/day vs. 20 mg/day groups). It would not be true to state that the reported efficacy data (across documented trials) highlights any linear (positive) correlations to patient doses. While there is a positive correlation, the amount of variance in efficacy between tiers is clinically unremarkable. Further studies are likely needed to elucidate such inconsistencies that destabilize confidence in the currently published clinical trial outcomes.
See also
- Tedatioxetine
- Paroxetine
- Buspar
- Vilazodone — a recently FDA-approved antidepressant with a similar dual mechanism of action.
- Serotonin modulator and stimulator — also, commonly "SMS" or simply "serotonin modulator".
References
- ^ "FDA-sourced list of all drugs with black box warnings (Use Download Full Results and View Query links.)". nctr-crs.fda.gov. FDA. Retrieved 22 Oct 2023.
- ^ H. Lundbeck A/S (December 12, 2012). "FDA accepts Takeda and Lundbeck's filing for review of Brintellix (vortioxetine) for the treatment of major depression". Retrieved June 12, 2015.
- ^ a b c d e f "BRINTELLIX™ (vortioxetine) tablets for oral use. Full Prescribing Information, Section 12.2 (Pharmacodynamics)." Takeda Pharmaceuticals America Inc. and Lundbeck, 2013. Revised September 2013.
- ^ FDA approves new drug to treat major depressive disorder, U.S. Food and Drug Administration Press Announcement.
- ^ Anthony J. Rothschild; et al. (December 2012). "Vortioxetine (Lu AA21004) 5 mg in generalized anxiety disorder: Results of an 8-week randomized, double-blind, placebo-controlled clinical trial in the United States". European Neuropsychopharmacology. 22 (12): 858–866. doi:10.1016/j.euroneuro.2012.07.011.
- ^ Jancin B (December 2009). "Lu AA21004 Looks Promising for Depression" (PDF). Clinical Psychiatry News. 37 (12): 24–25.
- ^ http://www.ema.europa.eu/ema/index.jsp?curl=pages/medicines/human/medicines/002717/smops/Positive/human_smop_000601.jsp&mid=WC0b01ac058001d127&source=homeMedSearch&category=human
- ^ Lundbeck press release (December 27, 2013): Lundbeck receives European marketing authorization for Brintellix for the treatment of adults with Major Depressive Episodes [1]
- ^ a b http://investor.lundbeck.com/releasedetail.cfm?ReleaseID=608559
- ^ Alvarez E, Perez V, Dragheim M, Loft H, Artigas F (July 2011). "A double-blind, randomized, placebo-controlled, active reference study of Lu AA21004 in patients with major depressive disorder". The International Journal of Neuropsychopharmacology / Official Scientific Journal of the Collegium Internationale Neuropsychopharmacologicum (CINP). 15 (5): 1–12. doi:10.1017/S1461145711001027. PMC 3349292. PMID 21767441.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Katona C, Hansen T, Olsen Ck (July 2012). "A randomized, double-blind, placebo-controlled, duloxetine-referenced, fixed-dose study comparing the efficacy and safety of Lu AA21004 in elderly patients with major depressive disorder". International clinical psychopharmacology. 27 (4): 215–23. doi:10.1097/YIC.0b013e3283542457. PMID 22572889.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b http://www.fiercebiotech.com/press-releases/statistically-significant-clinical-phase-iii-results-lu-aa21004-provide-bas
- ^ Henigsberg N, Mahableshwarkar AR, Jacobsen P, Chen Y, Thase ME (July 2012). "A randomized, double-blind, placebo-controlled 8-week trial of the efficacy and tolerability of multiple doses of Lu AA21004 in adults with major depressive disorder". J Clin Psychiatry. 73 (7): 953–9. doi:10.4088/JCP.11m07470. PMID 22901346.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Jain R, Mahableshwarkar AR, Jacobsen PL, Chen Y, Thase ME (September 2012). "A randomized, double-blind, placebo-controlled 6-wk trial of the efficacy and tolerability of 5 mg vortioxetine in adults with major depressive disorder". Int. J. Neuropsychopharmacol. 16 (2): 1–9. doi:10.1017/S1461145712000727. PMID 22963932.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Mahableshwarkar AR, Jacobsen PL, Chen Y (December 2012). "A Randomized, Double-Blind Trial of 2.5 mg and 5 mg Vortioxetine (Lu AA21004) Versus Placebo for 8 Weeks in Adults With Major Depressive Disorder". Curr Med Res Opin. 29 (3): 217–26. doi:10.1185/03007995.2012.761600. PMID 23252878.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ "A randomised, double-blind study in adults with major depressive disorder with an inadequate response to a single course of selective serotonin reuptake inhibitor or serotonin-noradrenaline reuptake inhibitor treatment switched to vortioxetine or agomelatine". Hum Psychopharmacol. 29: 470–82. Aug 4, 2014. doi:10.1002/hup.2424. PMID 25087600.
- ^ "Efficacy and safety of vortioxetine (Lu AA21004), 15 and 20 mg/day: a randomized, double-blind, placebo-controlled, duloxetine-referenced study in the acute treatment of adult patients with major depressive disorder.
Boulenger JP1, Loft H, Olsen CK". Int Clin Psychopharmacol. 29: 138–49. May 2014. doi:10.1097/YIC.0000000000000018. PMID 24257717.
{{cite journal}}: line feed character in|title=at position 217 (help) - ^ "Safety, tolerability, and efficacy of vortioxetine (Lu AA21004) in major depressive disorder: results of an open-label, flexible-dose, 52-week extension study". International Clinical Psychopharmacology. 29: 36–44. Jan 2014. doi:10.1097/YIC.0000000000000010. PMID 24169027.
- ^ "Relative efficacy and tolerability of vortioxetine versus selected antidepressants by indirect comparisons of similar clinical studies". Curr Med Res Opin. 30: 2589–606. Oct 10, 2014. doi:10.1185/03007995.2014.969566. PMID 25249164.
- ^ Henigsberg N, Mahableshwarkar AR, Jacobsen P, Chen Y, Thase ME (13 August 2012). "A randomized, double-blind, placebo-controlled 8-week trial of the efficacy and tolerability of multiple doses of lu aa21004 in adults with major depressive disorder". European neuropsychopharmacology. 22 (12): 847–57. doi:10.1016/j.euroneuro.2012.07.012. PMID 22898365.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Rothschild AJ, Mahableshwarkar AR, Jacobsen P, Yan M, Sheehan DV (14 August 2012). "Vortioxetine (Lu AA21004) 5mg in generalized anxiety disorder: Results of an 8-week randomized, double-blind, placebo-controlled clinical trial in the United States". European neuropsychopharmacology. 22 (12): 858–66. doi:10.1016/j.euroneuro.2012.07.011. PMID 22901736.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ "A randomized, double-blind, fixed-dose study comparing the efficacy and tolerability of vortioxetine 2.5 and 10 mg in acute treatment of adults with generalized anxiety disorder". Hum Psychopharmacol. 29: 64–72. Jan 2014. doi:10.1002/hup.2371. PMID 24424707.
- ^ "A randomised, double-blind, placebo-controlled, duloxetine-referenced study of the efficacy and tolerability of vortioxetine in the acute treatment of adults with generalised anxiety disorder". Int J Clin Pract. 68: 49–59. Jan 2014. doi:10.1111/ijcp.12328. PMID 24341301.
- ^ a b Mørk A, Montezinho LP, Miller S, Trippodi-Murphy C, Plath N, Li Y, Gulinello M, Sanchez C (1 February 2013). "Vortioxetine (Lu AA21004), a novel multimodal antidepressant, enhances memory in rats". Pharmacology, Biochemistry, and Behavior. 105: 41–50. doi:10.1016/j.pbb.2013.01.019. PMID 23380522.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Roger S. McIntyre , Søren Lophaven , Christina K. Olsen (Oct 2014). "A randomized, double-blind, placebo-controlled study of vortioxetine on cognitive function in depressed adults". International Journal of Neuropsychopharmacology. 17: 1557–1567. doi:10.1017/S1461145714000546.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Bang-Andersen B, Ruhland T, Jørgensen M, et al. (May 2011). "Discovery of 1-[2-(2,4-dimethylphenylsulfanyl)phenyl]piperazine (Lu AA21004): a novel multimodal compound for the treatment of major depressive disorder". Journal of Medicinal Chemistry. 54 (9): 3206–21. doi:10.1021/jm101459g. PMID 21486038.
- ^ N. Moore; B. Bang-Andersen; L. Brennum; K. Fredriksen; S. Hogg; A. Mork; T. Stensbol; H. Zhong; C. Sanchez; D. Smith (August 2008). "Lu AA21004: a novel potential treatment for mood disorders". European Neuropsychopharmacology. 18 (Supplement 4): S321. doi:10.1016/S0924-977X(08)70440-1.
{{cite journal}}: CS1 maint: multiple names: authors list (link)
