Propranolol: Difference between revisions
m drug name: remove INN refenence (link) from title (title is INN by definition, see also documentation for INN exception) (via AWB script) |
Cyberbot II (talk | contribs) Rescuing 1 sources. #IABot |
||
| Line 183: | Line 183: | ||
==External links== |
==External links== |
||
*{{cite journal |author=Stapleton MP |title=Sir James Black and propranolol. The role of the basic sciences in the history of cardiovascular pharmacology |journal=Texas Heart Institute Journal |volume=24 |issue=4 |pages=336–42 |year=1997 |pmid=9456487 |pmc=325477}} |
*{{cite journal |author=Stapleton MP |title=Sir James Black and propranolol. The role of the basic sciences in the history of cardiovascular pharmacology |journal=Texas Heart Institute Journal |volume=24 |issue=4 |pages=336–42 |year=1997 |pmid=9456487 |pmc=325477}} |
||
* [ |
* [ Scientific American Interview with James McGaugh] |
||
* [http://druginfo.nlm.nih.gov/drugportal/dpdirect.jsp?name=propranolol U.S. National Library of Medicine: Drug Information Portal - Propranolol] |
* [http://druginfo.nlm.nih.gov/drugportal/dpdirect.jsp?name=propranolol U.S. National Library of Medicine: Drug Information Portal - Propranolol] |
||
Revision as of 01:28, 28 February 2016
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Inderal |
| AHFS/Drugs.com | Monograph |
| License data |
|
| Pregnancy category |
|
| Routes of administration | By mouth, rectal, IV |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 26% |
| Metabolism | Liver (extensive) 1A2, 2D6; minor: 2C19, 3A4 |
| Elimination half-life | 4–5 hours |
| Excretion | Kidney (<1%) |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.007.618 |
| Chemical and physical data | |
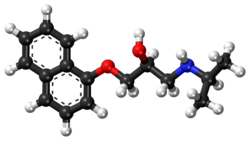
| Formula | C16H21NO2 |
| Molar mass | 259.34 g/mol g·mol−1 |
| 3D model (JSmol) | |
| Chirality | Racemic mixture |
| |
| |
| (verify) | |
Propranolol is a medication of the beta blocker type.[2] It is used to treat high blood pressure, a number of types of irregular heart rate, thyrotoxicosis, capillary hemangiomas, performance anxiety, and essential tremors.[2][3][4] It is used to prevent migraine headaches, and to prevent further heart problems in those with angina or previous heart attacks.[2] It can be taken by mouth or by injection into a vein. The formulation that is taken by mouth comes in short acting and long acting versions. Maximum effect when taken by mouth typically occurs within 90 minutes.[2]
Common side effects include nausea, abdominal pain, and constipation. It should not be used in those with an already slow heart rate and most of those with heart failure. Quickly stopping the medication in those with coronary artery disease may worsen symptoms. It may worsen the symptoms of asthma. Greater care is recommended in those with liver or kidney problems.[2] Propranolol may possibly cause harmful effects in the baby if taken during pregnancy.[5] Its use during breastfeeding is likely okay but the baby should be monitored for side effects.[6] It is a nonselective beta blocker which works by blocking β-adrenergic receptors.[2]
Propranolol was discovered in 1964.[7][8] It is on the World Health Organization's List of Essential Medicines, the most important medications needed in a basic health system.[9] Propranolol is available as a generic medication.[2] The wholesale cost is between 0.24 and 2.16 USD per month.[10] In the United States it costs about 15 USD per month at a typical dose.[2]
Medical uses


Heart disease
Propranolol is used for treating various conditions, including:
- Hypertension
- Angina pectoris (with the exception of variant angina)
- Tachyarrhythmias
- Myocardial infarction
- Control of tachycardia/tremor associated with anxiety, panic, hyperthyroidism, or lithium therapyWhile once a first-line treatment for hypertension, the role for beta blockers was downgraded in June 2006 in the United Kingdom to fourth-line, as they do not perform as well as other drugs, particularly in the elderly, and evidence is increasing that the most frequently used beta blockers at usual doses carry an unacceptable risk of provoking type 2 diabetes.[11]
Propranolol is not recommended for the treatment of hypertension by the Eighth Joint National Committee (JNC 8) because a higher rate of the primary composite outcome of cardiovascular death, myocardial infarction, or stroke compared to an angiotensin receptor blocker was noted in one study.[12]
Propranolol is also used to lower portal vein pressure in portal hypertension and prevent esophageal variceal bleeding and ascites.
Psychological
It is occasionally used to treat performance anxiety.[3] Evidence to support the use in other anxiety disorders is poor.[13]
- Some experimentation has been conducted in other psychiatric areas:[14]
- Treating the excessive drinking of fluids in psychogenic polydipsia[15][16]
- Aggressive behavior of patients with brain injuries[17]
Propranolol is being investigated as a potential treatment for post-traumatic stress disorder (PTSD).[18][19] Propranolol works to inhibit the actions of norepinephrine, a neurotransmitter that enhances memory consolidation. Individuals given propranolol immediately after trauma experienced fewer stress-related symptoms and lower rates of PTSD than respective control groups who did not receive the drug.[20]
It has been studied for improvement of social communication skills in people with autism spectrum disorder.[21]
Ethical and legal questions have been raised surrounding the use of propranolol-based medications for use as a "memory damper", including: altering memory-recalled evidence during an investigation, modifying behavioral response to past (albeit traumatic) experiences, the regulation of these drugs, and others.[22] However, Hall and Carter have argued that many such objections are "based on wildly exaggerated and unrealistic scenarios that ignore the limited action of propranolol in affecting memory, underplay the debilitating impact that PTSD has on those who suffer from it, and fail to acknowledge the extent to which drugs like alcohol are already used for this purpose."[23]
Other
- Essential tremor. Evidence for use for akathesia however is insufficient[24]
- Migraine prevention[25][26]
- Cluster headache prevention
- Hyperhidrosis
- Proliferating infantile hemangioma
- Glaucoma
- Thyrotoxicosis by deiodinase inhibition
- Primary exertional headache[27]
Propranolol may be used to treat severe infantile hemangiomas (IHs). This treatment shows promise as being superior to corticosteroids when treating IHs. Extensive clinical case evidence and a small controlled trial support its efficacy.[28]
Adverse effects
Due to the high penetration across the blood-brain barrier, lipophilic beta blockers such as propranolol and metoprolol are more likely than other less lipophilic beta blockers to cause sleep disturbances such as insomnia and vivid dreams, and nightmares.[29]
Adverse drug reactions (ADRs) associated with propranolol therapy are similar to other lipophilic beta blockers.
Precautions and contraindications
Propranolol should be used with caution in people with:[30]
- Diabetes mellitus or hyperthyroidism, since signs and symptoms of hypoglycaemia may be masked
- Peripheral vascular disease and Raynaud's syndrome, which may be exacerbated
- Phaeochromocytoma, as hypertension may be aggravated without prior alpha blocker therapy
- Myasthenia gravis, which may be worsened
- Other drugs with bradycardic effects
Propranolol is contraindicated in patients with:[30]
- Reversible airways diseases, particularly asthma or chronic obstructive pulmonary disease (COPD)
- Bradycardia (<60 beats/minute)
- Sick sinus syndrome
- Atrioventricular block (second- or third-degree)
- Shock
- Severe hypotension
- Cocaine toxicity [per American Heart Association guidelines, 2005]
Pregnancy and lactation
Propranolol, like other beta blockers, is classified as pregnancy category C in the United States and ADEC category C in Australia. β-blocking agents in general reduce perfusion of the placenta which may lead to adverse outcomes for the neonate, including pulmonary or cardiac complications, or premature birth. The newborn may experience additional adverse effects such as hypoglycemia and bradycardia.[31]
Most β-blocking agents appear in the milk of lactating women. However, propranolol is highly bound to proteins in the bloodstream and is distributed into breast milk at very low levels.[32] These low levels are not expected to pose any risk to the breastfeeding infant, and the American Academy of Pediatrics considers propranolol therapy "generally compatible with breastfeeding".[31][32][33][34]
Interactions
Since beta blockers are known to relax the cardiac muscle and to constrict the smooth muscle, these beta-adrenergic antagonists, including propranolol, have an additive effect with other drugs which decrease blood pressure, or which decrease cardiac contractility or conductivity. Clinically significant interactions particularly occur with:[30]
- Verapamil
- Epinephrine (adrenalin)
- β2-adrenergic receptor agonists
- Salbutamol, levosalbutamol, formoterol, salmeterol, etc.
- Clonidine
- Ergot alkaloids
- Isoprenaline (isoproterenol)
- Nonsteroidal anti-inflammatory drugs (NSAIDs)
- Quinidine
- Cimetidine
- Lidocaine
- Phenobarbital
- Rifampicin
- Fluvoxamine slows down the metabolism of propranolol significantly, leading to increased blood levels of propranolol.[35]
Pharmacokinetics
Propranolol is rapidly and completely absorbed, with peak plasma levels achieved about 1–3 hours after ingestion. Coadministration with food appears to enhance bioavailability.[36] Despite complete absorption, propranolol has a variable bioavailability due to extensive first-pass metabolism. Hepatic impairment therefore increases its bioavailability. The main metabolite 4-hydroxypropranolol, with a longer half-life (5.2–7.5 hours) than the parent compound (3–4 hours), is also pharmacologically active.
Propranolol is a highly lipophilic drug achieving high concentrations in the brain. The duration of action of a single oral dose is longer than the half-life and may be up to 12 hours, if the single dose is high enough (e.g., 80 mg). Effective plasma concentrations are between 10 and 100 mg/l. Toxic levels are associated with plasma concentrations above 2000 mg/l.
Mechanism of action
Propranolol is a nonselective beta blocker; that is, it blocks the action of epinephrine and norepinephrine on both β1- and β2-adrenergic receptors. It has little intrinsic sympathomimetic activity, but has strong membrane stabilizing activity (only at high blood concentrations, e.g. overdosage). Propranolol has inhibitory effects on the norepinephrine transporter (NET) and/or stimulates norepinephrine release (the concentration of norepinephrine is increased in the synapse).[37] Since propranolol blocks β-adrenoceptors, the increase in synaptic norepinephrine only results in α-adrenergic activation, with the α1-adrenoceptor being particularly important for effects observed in animal models. Therefore, it can be looked upon as an indirect α1 agonist, as well as a β antagonist. Probably owing to the effect at the α1-adrenoceptor, the racemic and the individual enantiomers of propranolol have been shown to substitute for cocaine in rats, with the most potent enantiomer being (S)-(−)-propranolol. In addition, some evidence suggests propranolol may function as a partial agonist at one or more serotonin receptors (possibly 5-HT1B).
Both enantiomers of the drug have a local anesthetic (topical) effect, which is normally mediated by blockade of voltage-gated sodium channels. Few studies have demonstrated propranolol's ability to block cardiac, neuronal, and skeletal voltage-gated sodium channels, accounting for its known "membrane stabilizing effect" and antiarrhythmic and other central nervous system effects.[38][39][40]
History
British scientist James W. Black developed propranolol in the 1960s.[41] In 1988, he was awarded the Nobel Prize in Medicine for this discovery. Propranolol was derived from the early β-adrenergic antagonists dichloroisoprenaline and pronethalol. The key structural modification, which was carried through to essentially all subsequent beta blockers, was the insertion of an oxymethylene group into the aryl ethanolamine structure of pronethalol, thus greatly increasing the potency of the compound. This also apparently eliminated the carcinogenicity found with pronethalol in animal models.
Newer, more cardio-selective beta blockers (such as bisoprolol, nebivolol, carvedilol, or metoprolol) are now used in the treatment of hypertension.
Society and culture
In a 1987 study by the International Conference of Symphony and Opera Musicians, 27% of interviewed members admitted to using beta blockers such as propranolol for musical performances.[42] For about 10–16% of performers, their degree of stage fright is considered pathological.[42][43] Propranolol is used by musicians, actors, and public speakers for its ability to treat anxiety symptoms activated by the sympathetic nervous system.[44] This can be seen as giving participating individuals an unfair advantage, especially in competitions, akin to the use of performance-enhancing drugs in athletes.[45]
Brand names
Original propranolol was marketed in 1965 under the brand name Inderal and manufactured by ICI Pharmaceuticals (now AstraZeneca). Propranolol is also marketed under brand names Avlocardyl, Deralin, Dociton, Inderalici, InnoPran XL, Sumial, Anaprilin, and Bedranol SR (Sandoz). In India it is marketed under brand names such as Ciplar and Ciplar LA by Cipla. Hemangeol, a 4.28 mg/mL solution of propranolol, is indicated for the treatment of proliferating infantile hemangioma.[46]
Research
In 2015, a trial in women with epithelial ovarian cancer showed that the intake of a nonselective β-blocker was associated with a longer survival compared to a β1-selective β-blocker or no β-blocker.[47] Currently, an interventional study is being conducted at the M.D. Anderson Cancer Center to access the feasibility of a nonselective β-blocker plus standard chemotherapy (paclitaxel and carboplatin or possibly docetaxel) to treat ovarian cancer.[48]
References
- ^ "FDA-sourced list of all drugs with black box warnings (Use Download Full Results and View Query links.)". nctr-crs.fda.gov. FDA. Retrieved 22 October 2023.
- ^ a b c d e f g h "Propranolol hydrochloride". Monograph. The American Society of Health-System Pharmacists. Retrieved 1 January 2015.
- ^ a b Davidson, JR (2006). "Pharmacotherapy of social anxiety disorder: what does the evidence tell us?". The Journal of clinical psychiatry. 67 Suppl 12: 20–6. PMID 17092192.
- ^ Chinnadurai, S; Fonnesbeck, C; Snyder, KM; Sathe, NA; Morad, A; Likis, FE; McPheeters, ML (February 2016). "Pharmacologic Interventions for Infantile Hemangioma: A Meta-analysis". Pediatrics. 137 (2). PMID 26772662.
- ^ "Prescribing medicines in pregnancy database". Australian Government. 3 March 2014. Retrieved 22 April 2014.
- ^ Yaffe, Gerald G. Briggs, Roger K. Freeman, Sumner J. (2011). Drugs in pregnancy and lactation : a reference guide to fetal and neonatal risk (9th ed.). Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. p. 1226. ISBN 9781608317080.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ^ Russell, RM (January 2004). "The enigma of beta-carotene in carcinogenesis: what can be learned from animal studies". The Journal of nutrition. 134 (1): 262S–268S. PMID 14704331.
- ^ Ravina, Enrique (2011). The evolution of drug discovery : from traditional medicines to modern drugs (1. Aufl. ed.). Weinheim: Wiley-VCH. p. 331. ISBN 9783527326693.
- ^ "WHO Model List of EssentialMedicines" (PDF). World Health Organization. October 2013. Retrieved 22 April 2014.
- ^ "Name". International Drug Price Indicator Guide. Retrieved January 2016.
{{cite web}}: Check date values in:|accessdate=(help) - ^ Sheetal Ladva (28 June 2006). "NICE and BHS launch updated hypertension guideline". National Institute for Health and Clinical Excellence. Retrieved 11 October 2009.
- ^ Paul A. James, MD; et al. (5 February 2014). "2014 Evidence-Based Guideline for the Management of High Blood Pressure in Adults". The Journal of the American Medical Association. Retrieved 23 March 2015.
- ^ Steenen, SA; van Wijk, AJ; van der Heijden, GJ; van Westrhenen, R; de Lange, J; de Jongh, A (February 2016). "Propranolol for the treatment of anxiety disorders: Systematic review and meta-analysis". Journal of psychopharmacology (Oxford, England). 30 (2): 128–39. doi:10.1177/0269881115612236. PMID 26487439.
- ^ Kornischka J, Cordes J, Agelink MW (April 2007). "[40 years beta-adrenoceptor blockers in psychiatry]". Fortschritte der Neurologie · Psychiatrie (in German). 75 (4): 199–210. doi:10.1055/s-2006-944295. PMID 17200914.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Vieweg V, Pandurangi A, Levenson J, Silverman J (1994). "The consulting psychiatrist and the polydipsia-hyponatremia syndrome in schizophrenia". International Journal of Psychiatry in Medicine. 24 (4): 275–303. doi:10.2190/5WG5-VV1V-BXAD-805K. PMID 7737786.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Kishi Y, Kurosawa H, Endo S (1998). "Is propranolol effective in primary polydipsia?". International Journal of Psychiatry in Medicine. 28 (3): 315–25. doi:10.2190/QPWL-14H7-HPGG-A29D. PMID 9844835.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Thibaut F, Colonna L (1993). "[Anti-aggressive effect of beta-blockers]". L'Encéphale (in French). 19 (3): 263–7. PMID 7903928.
- ^ "Doctors test a drug to ease traumatic memories - Mental Health - MSNBC.com". Retrieved 30 June 2007.
- ^ Brunet A, Orr SP, Tremblay J, Robertson K, Nader K, Pitman RK (May 2008). "Effect of post-retrieval propranolol on psychophysiologic responding during subsequent script-driven traumatic imagery in post-traumatic stress disorder". Journal of Psychiatric Research. 42 (6): 503–6. doi:10.1016/j.jpsychires.2007.05.006. PMID 17588604.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Vaiva, G.; Ducrocq, F.; Jezekiel, K.; Averland, B.; Lestavel, P.; Brunet, A.; Marmar, C.R. (2003). "Immediate treatment with propranolol decreases post-traumatic stress disorder two months after trauma". Biological Psychiatry. 54: 947–949. doi:10.1016/s0006-3223(03)00412-8.
- ^ "Blood pressure medicine may improve conversational skills of individuals with autism". University of Missouri at Columbia via PsyPost.com. 1 February 2016.
- ^ Kolber, Adam J. (2006). "Therapeutic Forgetting: The Legal and Ethical Implications of Memory Dampening". Vanderbilt Law Review, San Diego Legal Studies Paper No. 07-37. 59: 1561.
- ^ Hall, Wayne; Carter, Adrian (2007). "Debunking Alarmist Objections to the Pharmacological Prevention of PTSD". American Journal of Bioethics. 7 (9): 23–25. doi:10.1080/15265160701551244.
{{cite journal}}:|access-date=requires|url=(help) - ^ Lima, AR; Bacalcthuk, J; Barnes, TR; Soares-Weiser, K (18 October 2004). "Central action beta-blockers versus placebo for neuroleptic-induced acute akathisia". The Cochrane database of systematic reviews (4): CD001946. PMID 15495022.
- ^ Shields, Kevin G.; Peter J. Goadsby (January 2005). "Propranolol modulates trigeminovascular responses in thalamic ventroposteromedial nucleus: a role in migraine?". Brain. 128 (1): 86–97. doi:10.1093/brain/awh298. Retrieved 17 August 2012.
- ^ Eadie, M.; J. H. Tyrer (1985). The Biochemistry of Migraine. New York: Springer. p. 148. ISBN 9780852007310. OCLC 11726870.[dead link]
- ^ Clinical summary
- ^ Hogeling, M. (2012). "Propranolol for Infantile Hemangiomas: A Review". Current Dermatology Reports: Online-first. doi:10.1007/s13671-012-0026-6.
- ^ Cruickshank JM (2010). "Beta-blockers and heart failure". Indian Heart J. 62 (2): 101–10. PMID 21180298.
- ^ a b c Rossi S, editor. Australian Medicines Handbook 2006. Adelaide: Australian Medicines Handbook; 2006.
- ^ a b Sweetman, Sean C., ed. (2009). "Cardiovascular Drugs". Martindale: The complete drug reference (36th ed.). London: Pharmaceutical Press. pp. 1226–1381. ISBN 978-0-85369-840-1.
- ^ a b [No authors listed] (2007). "Propranolol". In: Drugs and Lactation Database. U.S. National Library of Medicine Toxicology Data Network. Retrieved 25 February 2013.
- ^ [No authors listed] (September 2001). "Transfer of drugs and other chemicals into human milk". Pediatrics. 108 (3): 776–89. PMID 11533352.
- ^ Spencer JP, Gonzalez LS, Barnhart DJ (July 2001). "Medications in the breast-feeding mother". Am Fam Physician. 64 (1): 119–26. PMID 11456429.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ van Harten J (1995). "Overview of the pharmacokinetics of fluvoxamine". Clinical Pharmacokinetics. 29 (Suppl 1): 1–9. doi:10.2165/00003088-199500291-00003. PMID 8846617.
- ^ Rang, Humphrey P. (2011). Rang & Dale's pharmacology (7th ed.). Edinburgh: Churchill Livingstone. p. 106. ISBN 9780702034718.
- ^ Young R, Glennon RA (April 2009). "S(-)Propranolol as a discriminative stimulus and its comparison to the stimulus effects of cocaine in rats". Psychopharmacology (Berl.). 203 (2): 369–82. doi:10.1007/s00213-008-1317-2. PMID 18795268.
- ^ Wang D. W., Mistry A. M., Kahlig K. M., Kearney J. A., Xiang J., George A. L. Jr (2010). "Propranolol blocks cardiac and neuronal voltage-gated sodium channels". Front. Pharmacol. 1: 144. doi:10.3389/fphar.2010.00144.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - ^ Bankston J. R., Kass R. S. (2010). "Molecular determinants of local anesthetic action of beta-blocking drugs: implications for therapeutic management of long QT syndrome variant 3". J. Mol. Cell. Cardiol. 48: 246–253. doi:10.1016/j.yjmcc.2009.05.012.
- ^ Desaphy J. F., Pierno S., De Luca A., Didonna P., Camerino D. C. (2003). "Different ability of clenbuterol and salbutamol to block sodium channels predicts their therapeutic use in muscle excitability disorders". Mol. Pharmacol. 63 (3): 659–670. doi:10.1124/mol.63.3.659. PMID 12606775.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Black JW, Crowther AF, Shanks RG, Smith LH, Dornhorst AC (1964). "A new adrenergic betareceptor antagonist". The Lancet. 283 (7342): 1080–1081. doi:10.1016/S0140-6736(64)91275-9. PMID 14132613.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Fishbein M, Middlestadt SE, Ottati V, Straus S, Ellis A (1988). "Medical problems among ICSOM musicians: overview of a national survey". Med Probl Perform Artist. 3: 1–8.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Steptoe A, Malik F, Pay C, Pearson P, Price C, Win Z (1995). "The impact of stage fright on student actors". Br J Psychol. 86: 27–39. doi:10.1111/j.2044-8295.1995.tb02544.x.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Alan H. Lockwood (1989). "Medical Problems of Musicians". NEJM. 320 (4): 221–227. doi:10.1056/nejm198901263200405.
- ^ Thomas H. Murray (1983). "The Coercive Power of Drugs in Sports". Hastings Center Report. 13 (4): 24–30. doi:10.2307/3561718.
- ^ "Hemangeol - Food and Drug Administration" (PDF). 1 March 2014. Retrieved 23 March 2015.
- ^ A.K. Sood, J.L.Watkins, P.H. Thaker (2015). "Clinical impact of selective and nonselective beta-blockers on survival in patients with ovarian cancer". Cancer: Online-first. doi:10.1002/cncr.29392.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ https://clinicaltrials.gov/show/NCT01504126. Retrieved 17 October 2015.
{{cite web}}: Missing or empty|title=(help)
External links
- Stapleton MP (1997). "Sir James Black and propranolol. The role of the basic sciences in the history of cardiovascular pharmacology". Texas Heart Institute Journal. 24 (4): 336–42. PMC 325477. PMID 9456487.
- [ Scientific American Interview with James McGaugh]
- U.S. National Library of Medicine: Drug Information Portal - Propranolol
