Fentanyl: Difference between revisions
→Society and culture: Added links, Added additional links and information. Tags: Mobile edit Mobile app edit Android app edit |
Adding further references to and context for dismissal of claims that dermal exposure to fentanyl is dangerous for first responders. |
||
| Line 209: | Line 209: | ||
The intravenous dose causing 50% of opioid-naive experimental subjects to die ({{LD50}}) is "3 mg/kg in rats, 1 mg/kg in cats, 14 mg/kg in dogs, and 0.03 mg/kg in monkeys."<ref>{{cite web |title=Fentanyl citrate injection, USP |publisher=U.S. [[Food and Drug Administration]] |url=https://www.accessdata.fda.gov/drugsatfda_docs/label/2013/016619s034lbl.pdf}}</ref> The LD<sub>50</sub> in mice has been given as 6.9 mg/kg by intravenous administration, 17.5 mg/kg intraperitoneally, 27.8 mg/kg by oral administration.<ref>{{cite journal | vauthors = Yadav SK, Maurya CK, Gupta PK, Jain AK, Ganesan K, Bhattacharya R | date = June 2014 | title = Synthesis and biological evaluation of some novel 1-substituted fentanyl analogs in Swiss albino mice | journal = Interdisciplinary Toxicology | volume = 7 | issue = 2 | pages = 93–102 | pmid = 26109885 | pmc = 4427721 | doi = 10.2478/intox-2014-0013 }}</ref> The LD<sub>50</sub> in humans is unknown,<ref>{{cite web|url=https://www.drugbank.ca/drugs/DB00813|title=Fentanyl|publisher=Drugbank}}</ref><ref>{{cite journal | vauthors = Vardanyan RS, Hruby VJ | title = Fentanyl-related compounds and derivatives: current status and future prospects for pharmaceutical applications | journal = Future Medicinal Chemistry | volume = 6 | issue = 4 | pages = 385–412 | date = March 2014 | pmid = 24635521 | pmc = 4137794 | doi = 10.4155/fmc.13.215 }}</ref> but a lethal dose for the average person is estimated to be 2 mg.<ref name=DEAphoto>{{cite web | title = Fentanyl |at=image 4 of 17 | publisher = [[Drug Enforcement Administration]] | url = https://www.dea.gov/galleries/drug-images/fentanyl}}</ref>{{verify source|date=May 2021}} |
The intravenous dose causing 50% of opioid-naive experimental subjects to die ({{LD50}}) is "3 mg/kg in rats, 1 mg/kg in cats, 14 mg/kg in dogs, and 0.03 mg/kg in monkeys."<ref>{{cite web |title=Fentanyl citrate injection, USP |publisher=U.S. [[Food and Drug Administration]] |url=https://www.accessdata.fda.gov/drugsatfda_docs/label/2013/016619s034lbl.pdf}}</ref> The LD<sub>50</sub> in mice has been given as 6.9 mg/kg by intravenous administration, 17.5 mg/kg intraperitoneally, 27.8 mg/kg by oral administration.<ref>{{cite journal | vauthors = Yadav SK, Maurya CK, Gupta PK, Jain AK, Ganesan K, Bhattacharya R | date = June 2014 | title = Synthesis and biological evaluation of some novel 1-substituted fentanyl analogs in Swiss albino mice | journal = Interdisciplinary Toxicology | volume = 7 | issue = 2 | pages = 93–102 | pmid = 26109885 | pmc = 4427721 | doi = 10.2478/intox-2014-0013 }}</ref> The LD<sub>50</sub> in humans is unknown,<ref>{{cite web|url=https://www.drugbank.ca/drugs/DB00813|title=Fentanyl|publisher=Drugbank}}</ref><ref>{{cite journal | vauthors = Vardanyan RS, Hruby VJ | title = Fentanyl-related compounds and derivatives: current status and future prospects for pharmaceutical applications | journal = Future Medicinal Chemistry | volume = 6 | issue = 4 | pages = 385–412 | date = March 2014 | pmid = 24635521 | pmc = 4137794 | doi = 10.4155/fmc.13.215 }}</ref> but a lethal dose for the average person is estimated to be 2 mg.<ref name=DEAphoto>{{cite web | title = Fentanyl |at=image 4 of 17 | publisher = [[Drug Enforcement Administration]] | url = https://www.dea.gov/galleries/drug-images/fentanyl}}</ref>{{verify source|date=May 2021}} |
||
Contrary to what has been reported in some media outlets, [[topical]] (or transdermal; via the skin) and [[Inhalation|inhalative]] exposure to fentanyl is extremely unlikely to cause intoxication or overdose (except in cases of prolonged exposure with very large quantities of fentanyl), and first responders such as paramedics and police officers are at minimal risk of fentanyl poisoning through accidental contact with intact skin.<ref>{{cite press release |title=American College of Medical Toxicology Position Statement on Fentanyl Exposure |url=https://www.acmt.net/cgi/page.cgi/_zine.html/Press_Releases/ACMT_Position_Statement_on_Fentanyl_Exposure |url-status=live}}</ref><ref>{{cite journal | vauthors = Thors L, Öberg L, Forsberg E, Wigenstam E, Larsson A, Bucht A | date = September 2020 | title = Skin penetration and decontamination efficacy following human skin exposure to fentanyl | journal = Toxicology in Vitro | volume = 67 | page = 104914 | pmid = 32540164 | doi = 10.1016/j.tiv.2020.104914 | s2cid = 219704174 }}</ref><ref>{{cite news |author=Ross, Casey |date=2017-08-09 |title=Are people really falling ill from touching fentanyl? In most cases, scientists say no |website=Stat News |url=https://www.statnews.com/2017/08/09/fentanyl-falling-ill |access-date=2021-08-07}}</ref> |
Contrary to what has been reported in some media outlets, [[topical]] (or transdermal; via the skin) and [[Inhalation|inhalative]] exposure to fentanyl is extremely unlikely to cause intoxication or overdose (except in cases of prolonged exposure with very large quantities of fentanyl), and first responders such as paramedics and police officers are at minimal risk of fentanyl poisoning through accidental contact with intact skin.<ref>{{cite press release |title=American College of Medical Toxicology Position Statement on Fentanyl Exposure |url=https://www.acmt.net/cgi/page.cgi/_zine.html/Press_Releases/ACMT_Position_Statement_on_Fentanyl_Exposure |url-status=live}}</ref><ref>{{cite journal | vauthors = Thors L, Öberg L, Forsberg E, Wigenstam E, Larsson A, Bucht A | date = September 2020 | title = Skin penetration and decontamination efficacy following human skin exposure to fentanyl | journal = Toxicology in Vitro | volume = 67 | page = 104914 | pmid = 32540164 | doi = 10.1016/j.tiv.2020.104914 | s2cid = 219704174 }}</ref><ref>{{cite news |author=Ross, Casey |date=2017-08-09 |title=Are people really falling ill from touching fentanyl? In most cases, scientists say no |website=Stat News |url=https://www.statnews.com/2017/08/09/fentanyl-falling-ill |access-date=2021-08-07}}</ref>. A 2020 article from the Journal of Medical Toxicology stated that "the consensus of the scientific community remains that illness from unintentional exposures is extremely unlikely, because opioids are not efficiently absorbed through the skin and are unlikely to be carried in the air."<ref>{{cite journal |last1=Herman |first1=Paul Alexander |title=Media Reports of Unintentional Opioid Exposure of Public Safety First Responders in North America |journal=Journal of Medical Toxicology |date=24 February 2020 |volume=16 |pages=112-115 |doi=https://doi.org/10.1007/s13181-020-00762-y |url=https://link.springer.com/article/10.1007/s13181-020-00762-y}}</ref> Fear of skin exposure to fentanyl may actually inhibit effective overdose response and "perpetuates community-wide stigma against people who use drugs by inaccurately portraying them as toxic and dangerous to be around."<ref>{{cite journal |last1=del Pozo |first1=Brandon |last2=Sightes |first2=Emily |title=Can touch this: training to correct police officer beliefs about overdose from incidental contact with fentanyl |journal=Health & Justice |date=24 November 2021 |volume=9 |issue=34 |doi=https://doi.org/10.1186/s40352-021-00163-5 |url=https://healthandjusticejournal.biomedcentral.com/articles/10.1186/s40352-021-00163-5}}</ref> |
||
'''Prevention''' |
'''Prevention''' |
||
Revision as of 00:05, 20 May 2022
 | |
 | |
| Clinical data | |
|---|---|
| Pronunciation | /ˈfɛntənɪl/ or /ˈfɛntənəl/ |
| Trade names | Actiq, Duragesic, Fentora, Sublimaze, others |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a605043 |
| License data | |
| Pregnancy category |
|
| Dependence liability | High[1] |
| Routes of administration | Buccal, epidural, IM, IT, IV, sublingual, skin patch |
| Drug class | Opioid |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | 92% (transdermal) 89% (intranasal) 50% (buccal) 33% (ingestion) 100% (intramuscular) 55% (inhaled) |
| Protein binding | 80–85% |
| Metabolism | Liver, primarily by CYP3A4 |
| Onset of action | 5 minutes[3] |
| Elimination half-life | IV: 6 mins (T1/2 α) 1 hours (T1/2 β) 16 hours (T1/2 ɣ) Intranasal: 6.5 hours Transdermal: 20–27 hours[4] Sublingual/buccal (single dose): 2.6–13.5 hours[4] |
| Duration of action | IV: 30–60 minutes[3][5] |
| Excretion | Mostly urinary (metabolites, < 10% unchanged drug)[4] |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.006.468 |
| Chemical and physical data | |
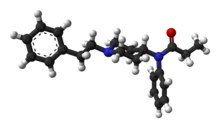
| Formula | C22H28N2O |
| Molar mass | 336.479 g·mol−1 |
| 3D model (JSmol) | |
| Density | 1.1 g/cm3 |
| Melting point | 87.5 °C (189.5 °F) |
| |
| |
| (verify) | |
Fentanyl, also spelled fentanil, is a powerful opioid used as a pain medication and, together with other medications, for anesthesia.[4] It is also used as a recreational drug, sometimes mixed with heroin, cocaine, or methamphetamine. Its potentially deadly overdose effects can be neutralized by naloxone.[6] Fentanyl is commonly used to create counterfeit pills disguised as OxyContin, Xanax, Adderall, among others. It has a rapid onset and its effects generally last under two hours.[4] Medically, it is used by injection, nasal spray, or skin patch, or absorbed through the cheek as a lozenge or tablet.[4][7]
Common side effects of fentanyl include nausea, vomiting, constipation, itching, sedation, confusion, and injuries related to poor coordination.[4][8] Serious side effects may include respiratory depression, hallucinations, serotonin syndrome, low blood pressure, or development of an opioid use disorder.[4][8] Fentanyl works primarily by activating μ-opioid receptors.[4] It is around 100 times stronger than morphine and about 50 times stronger than heroin. Some fentanyl analogues such as carfentanil are up to 10,000 times stronger than morphine.[9]
Fentanyl was first made by Paul Janssen in 1960 and approved for medical use in the United States in 1968.[4][10] In 2015, 1,600 kilograms (3,500 pounds) were used in healthcare globally.[11] As of 2017[update], fentanyl was the most widely used synthetic opioid in medicine;[12] in 2019, it was the 278th most commonly prescribed medication in the United States, with more than 1 million prescriptions.[13][14] It is on the World Health Organization's List of Essential Medicines.[15]
Starting around 2013, fentanyl disrupted the North American market for illegal drugs, capitalizing on pre-existing demand for opiates such as heroin and prescription pharmaceuticals.[16] In 2016, fentanyl and fentanyl analogues were the most common cause of overdose deaths in the United States at more than 20,000, about half of all opioid-related deaths.[17][18][19] Most of these overdose deaths were due to illegally-made fentanyl.[20] There is concern that the growing demand may prove highly attractive to organized crime and aspiring criminals, especially those operating in areas around the Golden Triangle in Southeast Asia, e.g. Shan State in Myanmar, where production of synthetic drugs has expanded dramatically since the late 2000s. Compared to heroin, it is more potent, has higher profit margins, and, because it is compact, has simpler logistics. It can be cut into, or even replace entirely, the supply of heroin and other opiates.[21]
Medical uses
Anesthesia
Intravenous fentanyl is often used for anesthesia and to treat pain.[22] To induce anesthesia, it is given with a sedative-hypnotic, like propofol or thiopental, and a muscle relaxant.[23] To maintain anesthesia, inhaled anesthetics and additional fentanyl may be used.[23] These are often given in 15–30 minute intervals throughout procedures such as endoscopy and surgeries and in emergency rooms.[24][25]
For pain relief after surgery, use can decrease the amount of inhalational anesthetic needed for emergence from anesthesia.[23] Balancing this medication and titrating the drug based on expected stimuli and the person's responses can result in stable blood pressure and heart rate throughout a procedure and a faster emergence from anesthesia with minimal pain.[23]
Regional anesthesia
Fentanyl is the most commonly used intrathecal opioid because its lipophilic profile allows a quick onset of action (5–10 min.) and intermediate duration of action (60–120 min.).[26] Spinal administration of hyperbaric bupivacaine with fentanyl may be the optimal combination. The almost immediate onset of fentanyl reduces visceral discomfort and even nausea during the procedure.[27]
Obstetrics
Fentanyl is sometimes given intrathecally as part of spinal anesthesia or epidurally for epidural anaesthesia and analgesia. Because of fentanyl's high lipid solubility, its effects are more localized than morphine, and some clinicians prefer to use morphine to get a wider spread of analgesia.[28] However, it is widely used in obstetrical anesthesia because of its short time to action peak (about 5 min.), the rapid termination of its effect after a single dose, and the occurrence of relative cardiovascular stability.[29] In obstetrics, the dose must be closely regulated in order to prevent large amounts of transfer from mother to fetus. At high doses, the drug may act on the fetus to cause postnatal respiratory distress.[29] For this reason, shorter acting agents such as alfentanyl or remifentanil may be more suitable in the context of inducing general anaesthesia.[30]
Pain management

The bioavailability of intranasal fentanyl is about 70–90%, but with some imprecision due to clotted nostrils, pharyngeal swallow, and incorrect administration. For both emergency and palliative use, intranasal fentanyl is available in doses of 50, 100, and 200 µg. In emergency medicine, safe administration of intranasal fentanyl with a low rate of side effects and a promising pain-reducing effect was demonstrated in a prospective observational study in about 900 out-of-hospital patients.[31]
In children, intranasal fentanyl is useful for the treatment of moderate and severe pain and is well tolerated.[32]
Chronic pain
It is also used in the management of chronic pain including cancer pain.[33] Often, transdermal patches are used.[34] The patches work by slowly releasing fentanyl through the skin into the bloodstream over 48 to 72 hours, allowing for long-lasting pain management.[35] Dosage is based on the size of the patch, since, in general, the transdermal absorption rate is constant at a constant skin temperature.[35] Each patch should be changed every 72 hours.[36] Rate of absorption is dependent on a number of factors. Body temperature, skin type, amount of body fat, and placement of the patch can have major effects. The different delivery systems used by different makers will also affect individual rates of absorption. Under normal circumstances, the patch will reach its full effect within 12 to 24 hours; thus, fentanyl patches are often prescribed with a fast-acting opioid (such as morphine or oxycodone) to handle breakthrough pain.[35] It is unclear if fentanyl gives long-term pain relief to people with neuropathic pain.[37]
Breakthrough pain
Sublingual fentanyl dissolves quickly and is absorbed through the sublingual mucosa to provide rapid analgesia.[38] Fentanyl is a highly lipophilic compound,[38][39] which is well absorbed sublingually and generally well tolerated.[38] Such forms are particularly useful for breakthrough cancer pain episodes, which are often rapid in onset, short in duration, and severe in intensity.[40]
Palliative care

In palliative care, transdermal fentanyl patches have a definitive, but limited role for:
- people already stabilized on other opioids who have persistent swallowing problems and cannot tolerate other parenteral routes such as subcutaneous administration.
- people with moderate to severe kidney failure.
- troublesome side effects of oral morphine, hydromorphone, or oxycodone.[41][42]
When using the transdermal patch, patients must be careful to minimize or avoid external heat sources (direct sunlight, heating pads, etc.), which can trigger the release of too much medication and cause potentially deadly complications.
Combat medicine
USAF Pararescue combat medics in Afghanistan used fentanyl lozenges in the form of lollipops on combat casualties from IED blasts and other trauma.[43] The stick is taped to a finger and the lozenge put in the cheek of the person. When enough fentanyl has been absorbed, the (sedated) person generally lets the lollipop fall from the mouth, indicating sufficient analgesia and somewhat reducing the likelihood of overdose and associated risks.[43]
Dyspnea
Fentanyl can also be used for patients in whom morphine is not tolerated, or whose breathlessness is refractory to morphine. Fentanyl is especially useful for concomitant treatment in palliative care settings where pain and shortness of breath are severe and need to be treated with high strength opioids.[citation needed]
Other
Some routes of administration such as nasal sprays and inhalers generally result in a faster onset of high blood levels, which can provide more immediate analgesia but also more severe side effects, especially in overdose. The much higher cost of some of these appliances may not be justified by marginal benefit compared with buccal or oral options. Intranasal fentanyl appears to be equally effective as IV morphine and superior to intramuscular morphine for the management of acute hospital pain.[32]
A fentanyl patient-controlled transdermal system (PCTS) is under development, which aims to allow patients to control administration of fentanyl through the skin to treat postoperative pain.[44]
Adverse effects


Fentanyl's most common side effects, which affect more than 10% of people, include nausea, vomiting, constipation, dry mouth, somnolence, confusion, and asthenia (weakness). Less frequently, in 3-10% of people, fentanyl can cause abdominal pain, headache, fatigue, anorexia and weight loss, dizziness, nervousness, anxiety, depression, flu-like symptoms, dyspepsia (indigestion), shortness of breath, hypoventilation, apnoea, and urinary retention. Fentanyl use has also been associated with aphasia.[45] Despite being a more potent analgesic, fentanyl tends to induce less nausea, as well as less histamine-mediated itching, than morphine.[46]
The duration of action of fentanyl has sometimes been underestimated, leading to harm in a medical context.[47][48][49][50] In 2006, the U.S. Food and Drug Administration (FDA) began investigating several respiratory deaths, but doctors in the United Kingdom were not warned of the risks with fentanyl until September 2008.[51] The FDA reported in April 2012 that twelve young children had died and twelve more made seriously ill from separate accidental exposures to fentanyl skin patches.[52]
Fentanyl has a therapeutic index of 270.[53]
Respiratory depression
The most dangerous adverse effect of fentanyl is respiratory depression,[54] that is, decreased sensitivity to carbon dioxide leading to reduced rate of breathing, which can cause anoxic brain injury or death. This risk is decreased when the airway is secured with an endotracheal tube (as during anesthesia).[55] This risk is higher in specific groups, like those with obstructive sleep apnea.[55]
Other factors that increase the risk of respiratory depression are:[55]
- High fentanyl doses
- Sleep
- Older age
- Simultaneous use of CNS depressants like benzodiazepines, barbiturates, alcohol, and inhaled anesthetics
- Hyperventilation
- Decreased CO2 levels in the serum
- Respiratory acidosis
- Decreased fentanyl clearance from the body
- Decreased blood flow to the liver
- Renal insufficiency
Sustained release fentanyl preparations, such as patches, may also produce unexpected delayed respiratory depression.[56][57][58] The precise reason for sudden respiratory depression is unclear, but there are several hypotheses:
- Saturation of the body fat compartment in people with rapid and profound body fat loss (people with cancer, cardiac or infection-induced cachexia can lose 80% of their body fat).
- Early carbon dioxide retention causing cutaneous vasodilation (releasing more fentanyl), together with acidosis, which reduces protein binding of fentanyl, releasing yet more fentanyl.
- Reduced sedation, losing a useful early warning sign of opioid toxicity and resulting in levels closer to respiratory-depressant levels.
Another related complication of fentanyl overdoses includes the so-called wooden chest syndrome which quickly induces complete respiratory failure by paralyzing the thoracic muscles, explained in more detail in the Muscle rigidity section below.
Heart and blood vessels
- Bradycardia: Fentanyl decreases the heart rate by increasing vagal nerve tone in the brainstem, which increases the parasympathetic drive.[55]
- Vasodilation: It also vasodilates arterial and venous blood vessels through a central mechanism, by primarily slowing down vasomotor centers in the brainstem. To a lesser extent, it does this by directly affecting blood vessels.[55] This is much more profound in patients who have an already increased sympathetic drive, like patients who have high blood pressure or congestive heart failure.[55] It does not affect the contractility of the heart when regular doses are administered.[55]
Muscle rigidity
If high boluses of fentanyl are administered quickly, muscle rigidity of the vocal cords can make bag-mask ventilation very difficult.[55] The exact mechanism of this effect is unknown, but it can be prevented and treated using neuromuscular blockers.[55]
Wooden chest syndrome
A prominent idiosyncratic adverse effect of fentanyl also includes a sudden onset of rigidity of the abdominal muscles and the diaphragm which induces respiratory failure; this is seen with high doses and is known as wooden chest syndrome.[59] The syndrome is believed to be the main cause of death as a result of fentanyl overdoses.[60]
Wooden chest syndrome is reversed by naloxone and is believed to be caused by a release of noradrenaline which activates α-adrenergic receptors and also possibly via an activation of cholinergic receptors.[61]
Wooden chest syndrome is unique to the most powerful opioids—which today comprise fentanyl and its analogs—while other less-powerful opioids like heroin produce mild rigidity of the respiratory muscles to a much lesser degree.[62][61]
Overdose
Fentanyl poses an exceptionally high overdose risk in humans, due to having an extremely unpredictable fatal dosage when mixed with other drugs. In its pure form, overdoses are only moderately unpredictable, with most overdose deaths occurring at serum concentrations of between 150 and 250 ng/mL. But when mixed with other drugs, overdoses can occur with as little as 0.1 ng/mL.[citation needed] Over 85% of overdoses involved at least one other drug, and there was no clear correlation showing at which level the mixtures were fatal. The dosages of fatal mixtures varied by over three magnitudes in some cases. This extremely unpredictable volatility with other drugs makes it especially difficult to avoid fatalities.[63]
Naloxone can completely or partially reverse an opioid overdose.[64] In July 2014, the Medicines and Healthcare products Regulatory Agency (MHRA) of the UK issued a warning about the potential for life-threatening harm from accidental exposure to transdermal fentanyl patches, particularly in children,[65] and advised that they should be folded, with the adhesive side in, before being discarded. The patches should be kept away from children, who are most at risk from fentanyl overdose.[66] In the US, fentanyl and fentanyl analogs caused over 29,000 deaths in 2017, a large increase over the previous four years.[67][16]

Most of the recent increases in fentanyl deaths do not involve prescription fentanyl but are related to illicitly-made fentanyl that is being mixed with or sold as heroin.[68] Death from fentanyl overdose continues to be a public health issue of national concern in Canada since September 2015.[69] In 2016, deaths from fentanyl overdoses in the province of British Columbia averaged two persons per day.[70] In 2017 the death rate rose over 100% with 368 overdose-related deaths in British Columbia between January and April 2017.[71]
Fentanyl has started to make its way into heroin as well as illicitly-manufactured opioids and benzodiazepines. Fentanyl contamination in cocaine, methamphetamine, ketamine, MDMA, and other drugs is common.[72][73] A kilogram of heroin laced with fentanyl may sell for more than US$100,000, but the fentanyl itself may be produced far more cheaply, for about US$6,000 per kilogram. Fentanyl was often produced in China and exported illegally to the U.S.[74][75] The UK illicit drug market is no longer reliant on China, as domestic fentanyl production is replacing imports.[76]
As of 2018, fentanyl was the most commonly listed opioid in overdose drug deaths, surpassing heroin. From 2013 until 2016, overdose deaths involving fentanyl were increasing by 113% per year.[77] In 2021, the Public Health Agency of Canada noted that 87% of accidental apparent opioid toxicity deaths involved fentanyl.[78]
The intravenous dose causing 50% of opioid-naive experimental subjects to die (LD50) is "3 mg/kg in rats, 1 mg/kg in cats, 14 mg/kg in dogs, and 0.03 mg/kg in monkeys."[79] The LD50 in mice has been given as 6.9 mg/kg by intravenous administration, 17.5 mg/kg intraperitoneally, 27.8 mg/kg by oral administration.[80] The LD50 in humans is unknown,[81][82] but a lethal dose for the average person is estimated to be 2 mg.[83][verification needed]
Contrary to what has been reported in some media outlets, topical (or transdermal; via the skin) and inhalative exposure to fentanyl is extremely unlikely to cause intoxication or overdose (except in cases of prolonged exposure with very large quantities of fentanyl), and first responders such as paramedics and police officers are at minimal risk of fentanyl poisoning through accidental contact with intact skin.[84][85][86]. A 2020 article from the Journal of Medical Toxicology stated that "the consensus of the scientific community remains that illness from unintentional exposures is extremely unlikely, because opioids are not efficiently absorbed through the skin and are unlikely to be carried in the air."[87] Fear of skin exposure to fentanyl may actually inhibit effective overdose response and "perpetuates community-wide stigma against people who use drugs by inaccurately portraying them as toxic and dangerous to be around."[88]
Prevention
Many public health initiatives have been started to prevent the misuse and overdose of fentanyl. One of the initiatives that have been started to prevent fentanyl overdose is from the CDC [1]. The effort has been categorized as a Health Alert Network Advisory signaled to a multitude of professionals within the health field. The advisory explains four key action points. Those points include the (a) local need to expand the distribution and use of naloxone and overdose prevention education, (b) expand awareness, access, and availability of treatment for substance use disorders, (c) intervene early with individuals at highest risk for overdose, and (d) improve detection of overdose outbreaks to facilitate more effective response.[89]
Another initiative is a social media campaign from the United States Drug Enforcement Administration (DEA)[90] called "One Pill Can Kill". This social media campaigns goal was to spread awareness of the prevalence of counterfeit pills that are being sold in America that is leading to the large overdose epidemic in America. This campaign also shows the difference between counterfeit pills and real pills. This campaign also offers resources for help with drug addiction and rehabilitation. [91]
In New Jersey another initiative was started called "The Partnership for a Drug-Free New Jersey" (PDFNJ) was created to inform the people of New Jersey the harm of taking drugs and where to dispose of expired or unneeded prescription medications. Some of this programs campaigns also focus on children and teaching children how to deal with the influence and peer pressures of these drugs.
Rehab Options and resources
Opioid rehabilitation is common within America and there are many different facilities and resources that a person can reach out to if they need assistance or if someone they know needs assistance with an opioid addiction. One of these resources that a person could reach out to is the American Addiction Centers[92]’ website. This website has many different resources like a helpline where a person could discuss treatment options for either themselves or someone else. This website also shows the locations of the facilities that the American Addiction Centers have throughout the country. They have facilities in Texas, California, Nevada, Florida, Rhode Island, Massachusetts, Mississippi, and New Jersey. This website also offers different treatment and rehab options including drug detoxification, inpatient treatment, outpatient treatment, etc. This website also shows the types of medications that could be used to help with the rehabilitation process as well.
Another resource that could be used is the Hazelden Betty Ford Foundation[93] which is the nation's largest nonprofit treatment providers. They have locations in California, Minnesota, Oregon, Illinois, New York, Florida, Massachusetts, Colorado and Washington. This foundation provides resources on many different types of addiction including opioids. They also provide information about signs of addiction, and how to have an intervention for the party that is affected by the addiction.[citation needed]
Pharmacology
Classification
Fentanyl is a synthetic opioid in the phenylpiperidine family, which includes sufentanil, alfentanil, remifentanil, and carfentanil.[94][95]
Structure-activity
The structures of opioids share many similarities. Whereas opioids like codeine, hydrocodone, oxycodone, and hydromorphone are synthesized by simple modifications of morphine, fentanyl and its relatives are synthesized by modifications of meperidine.[55] Meperidine is a fully synthetic opioid, and other members of the phenylpiperidine family like alfentanil and sufentanil are complex versions of this structure.[55]
Like other opioids, fentanyl is a weak base that is highly lipid-soluble, protein-bound, and protonated at physiological pH.[55] All of these factors allow it to rapidly cross cellular membranes, contributing to its quick effect in the body and the central nervous system.[46][94]
Mechanism of action
| Affinities, Ki | Ratio | ||
|---|---|---|---|
| MOR | DOR | KOR | MOR:DOR:KOR |
| 0.39 nM | >1,000 nM | 255 nM | 1:>2564:654 |
Fentanyl, like other opioids, acts on opioid receptors. These receptors are G-protein-coupled receptors, which contain seven transmembrane portions, intracellular loops, extracellular loops, intracellular C-terminus, and extracellular N-terminus.[55] The extracellular N-terminus is important in differentiating different types of binding substrates.[55] When fentanyl binds, downstream signaling leads to the inhibitory effects, such as decreased cAMP production, decreased calcium ion influx, and increased potassium efflux.[55] This inhibits the ascending pathways in the central nervous system to increase pain threshold by changing the perception of pain; this is mediated by decreasing propagation of nociceptive signals, resulting in analgesic effects.[97][98]
As a μ-receptor agonist, fentanyl binds 50 to 100 times more potently than morphine.[97] It can also bind to the delta and kappa opioid receptors but with a lower affinity. It has high lipid solubility, allowing it to more easily penetrate the central nervous system.[94][46] It attenuates "second pain" with primary effects on slow-conducting, unmyelintated C-fibers and is less effective on neuropathic pain and "first pain" signals through small, myelinated A-fibers.[55]
Fentanyl can produce the following clinical effects strongly, through μ-receptor agonism.[99]
- Supraspinal analgesia (μ1)
- Respiratory depression (μ2)
- Physical dependence
- Muscle rigidity
It produces sedation and spinal analgesia through Κ-receptor agonism.[99]
Therapeutic effects
- Pain relief: Primarily, fentanyl provides the relief of pain by acting on the brain and spinal μ-receptors.[55]
- Sedation: Fentanyl produces sleep and drowsiness, as the dosage is increased, and can produce the δ-waves often seen in natural sleep on electroencephalogram.[55]
- Suppression of the cough reflex: Fentanyl can decrease the struggle against an endotracheal tube and excessive coughing by decreasing the cough reflex, becoming useful when intubating people who are awake and have compromised airways.[55] After receiving a bolus dose of fentanyl, people can also experience paradoxical coughing, which is a phenomenon that is not well understood.[55]
Detection in biological fluids
Fentanyl may be measured in blood or urine to monitor for abuse, confirm a diagnosis of poisoning, or assist in a medicolegal death investigation. Commercially available immunoassays are often used as initial screening tests, but chromatographic techniques are generally used for confirmation and quantitation. The Marquis Color test may also be used to detect the presence of fentanyl. Using formaldehyde and sulfuric acid, the solution will turn purple when introduced to opium drugs. Blood or plasma fentanyl concentrations are expected to be in a range of 0.3–3.0 μg/L in persons using the medication therapeutically, 1–10 μg/L in intoxicated people, and 3–300 μg/L in victims of acute overdosage.[100] Paper spray-mass spectrometry (PS-MS) may be useful for initial testing of samples.[101][102]
History
Fentanyl was first synthesized in Belgium by Paul Janssen under the label of his relatively newly formed Janssen Pharmaceutica in 1959.[103] It was developed by screening chemicals similar to pethidine (meperidine) for opioid activity.[104] The widespread use of fentanyl triggered the production of fentanyl citrate (the salt formed by combining fentanyl and citric acid in a 1:1 stoichiometric ratio).[105] Fentanyl citrate entered medical use as a general anaesthetic in 1968, manufactured by McNeil Laboratories under the trade name Sublimaze.[106]
In the mid-1990s, Janssen Pharmaceutica developed and introduced into clinical trials the Duragesic patch, which is a formulation of an inert alcohol gel infused with select fentanyl doses, which are worn to provide constant administration of the opioid over a period of 48 to 72 hours. After a set of successful clinical trials, Duragesic fentanyl patches were introduced into medical practice.
Following the patch, a flavored lollipop of fentanyl citrate mixed with inert fillers was introduced in 1998 under the brand name of Actiq, becoming the first quick-acting formation of fentanyl for use with chronic breakthrough pain.[107]
In 2009, the US Food and Drug Administration approved Onsolis (fentanyl buccal soluble film), a fentanyl drug in a new dosage form for cancer pain management in opioid-tolerant subjects.[108] It uses a medication delivery technology called BEMA (BioErodible MucoAdhesive), a small dissolvable polymer film containing various fentanyl doses applied to the inner lining of the cheek.[108]
Fentanyl has a US DEA ACSCN of 9801 and a 2013 annual aggregate manufacturing quota of 2,108.75 kg, unchanged from the prior year.
Society and culture
Legal status
In the UK, fentanyl is classified as a controlled Class A drug under the Misuse of Drugs Act 1971.[109]
In the Netherlands, fentanyl is a List I substance of the Opium Law.
In the U.S., fentanyl is a Schedule II controlled substance per the Controlled Substance Act. Distributors of Abstral are required to implement an FDA-approved risk evaluation and mitigation strategy (REMS) program.[110][111] In order to curb misuse, many health insurers have begun to require precertification and/or quantity limits for Actiq prescriptions.[112][113][114]
In Canada, fentanyl is considered a schedule I drug as listed in Canada's Controlled Drugs and Substances Act.[115]
Estonia is known to have been home to the world's longest documented fentanyl epidemic, especially following the Taliban ban on opium poppy cultivation in Afghanistan.[116]
A 2018 report by The Guardian indicated that many major drug suppliers on the dark web have voluntarily banned the trafficking of fentanyl.[117]
Recreational use
Illicit use of pharmaceutical fentanyl and its analogues first appeared in the mid-1970s in the medical community and continues in the present. More than 12 different analogues of fentanyl, all unapproved and clandestinely produced, have been identified in the U.S. drug traffic. In February 2018, the U.S. Drug Enforcement Administration indicated that illicit fentanyl analogs have no medically valid use, and thus applied a "Schedule I" classification to them.[118]
Fentanyl analogues may be hundreds of times more potent than heroin. Fentanyl is used orally, smoked, snorted, or injected. Fentanyl is sometimes sold as heroin or oxycodone, sometimes leading to overdoses. Many fentanyl overdoses are initially classified as heroin overdoses.[119] Recreational use is not particularly widespread in the EU except for Tallinn, Estonia, where it has largely replaced heroin. Estonia has the highest rate of 3-methylfentanyl overdose deaths in the EU, due to its high rate of recreational use.[120]
Fentanyl is sometimes sold on the black market in the form of transdermal fentanyl patches such as Duragesic, diverted from legitimate medical supplies. The gel from inside the patches is sometimes ingested or injected.[121]
Another form of fentanyl that has appeared on the streets is the Actiq lollipop formulation. The pharmacy retail price ranges from US$15 to US$50 per unit based on the strength of the lozenge, with the black market cost ranging from US$5 to US$25, depending on the dose.[122] The attorneys general of Connecticut and Pennsylvania have launched investigations into its diversion from the legitimate pharmaceutical market, including Cephalon's "sales and promotional practices for Provigil, Actiq and Gabitril."[122]
Non-medical use of fentanyl by individuals without opioid tolerance can be very dangerous and has resulted in numerous deaths.[121] Even those with opiate tolerances are at high risk for overdoses. Like all opioids, the effects of fentanyl can be reversed with naloxone, or other opiate antagonists. Naloxone is increasingly available to the public. Long acting or sustained release opioids may require repeat dosage. Illicitly synthesized fentanyl powder has also appeared on the United States market. Because of the extremely high strength of pure fentanyl powder, it is very difficult to dilute appropriately, and often the resulting mixture may be far too strong and, therefore, very dangerous.[123]
Some heroin dealers mix fentanyl powder with heroin to increase potency or compensate for low-quality heroin. In 2006, illegally manufactured, non-pharmaceutical fentanyl often mixed with cocaine or heroin caused an outbreak of overdose deaths in the United States and Canada, heavily concentrated in the cities of Dayton, Ohio; Chicago; Detroit; and Philadelphia.[124]
Enforcement

Several large quantities of illicitly produced fentanyl have been seized by U.S. law enforcement agencies. In November 2016, the DEA uncovered an operation making counterfeit oxycodone and Xanax from a home in Cottonwood Heights, Utah. They found about 70,000 pills in the appearance of oxycodone and more than 25,000 in the appearance of Xanax. The DEA reported that millions of pills could have been distributed from this location over the course of time. The accused owned a tablet press and ordered fentanyl in powder form from China.[126][127] A seizure of a record amount of fentanyl occurred on February 2, 2019, by U.S. Customs and Border Protection in Nogales, Arizona. The 254 pounds (115 kg) of fentanyl, which was estimated to be worth US$3.5M, was concealed in a compartment under a false floor of a truck transporting cucumbers.[128] The "China White" form of fentanyl refers to any of a number of clandestinely produced analogues, especially α-methylfentanyl (AMF).[129] One US Department of Justice publication lists "China White" as a synonym for a number of fentanyl analogues, including 3-methylfentanyl and α-methylfentanyl,[130] which today are classified as Schedule I drugs in the United States.[129] Part of the motivation for AMF is that, despite the extra difficulty from a synthetic standpoint, the resultant drug is more resistant to metabolic degradation. This results in a drug with an increased duration.[131]
In June 2013, the United States Centers for Disease Control and Prevention (CDC) issued a health advisory[132] to emergency departments alerting to 14 overdose deaths among intravenous drug users in Rhode Island associated with acetylfentanyl, a synthetic opioid analog of fentanyl that has never been licensed for medical use. In a separate study conducted by the CDC, 82% of fentanyl overdose deaths involved illegally manufactured fentanyl, while only 4% were suspected to originate from a prescription.[133]
Beginning in 2015, Canada has seen a number of fentanyl overdoses. Authorities suspected that the drug was being imported from Asia to the western coast by organized crime groups in powder form and being pressed into pseudo-OxyContin tablets.[134] Traces of the drug have also been found in other recreational drugs including cocaine, MDMA, and heroin. The drug has been implicated in multiple deaths from the homeless to young professionals, including multiple teens and young parents.[135] Because of the rising deaths across the country, especially in British Columbia where 1,716 deaths were reported in 2020 and 1,782 from January to October 2021,[136] Health Canada is putting a rush on a review of the prescription-only status of naloxone in an effort to combat overdoses of the drug.[137] In 2018, Global News reported allegations that diplomatic tensions between Canada and China hindered cooperation to seize imports, with Beijing being accused of inaction.[138]
Fentanyl has been discovered for sale in illicit markets in Australia in 2017[139] and in New Zealand in 2018.[140] In response, New Zealand experts called for wider availability of naloxone.[141]
In 2020, the Myanmar military and police confiscated 990 gallons of methyl fentanyl, as well as precursors for the illicit synthesis of the drug. According to the United Nations Office on Drugs and Crime, the Shan State of Myanmar has been identified as a major source for fentanyl derivatives. In 2021, the agency reported a further drop in opium poppy cultivation in Burma, as the region’s synthetic drug market continues to expand and diversify.[142][143]
Recalls
In February 2004, a leading fentanyl supplier, Janssen Pharmaceutica Products recalled one lot, and later, additional lots of fentanyl (brand name: Duragesic) patches because of seal breaches that might have allowed the medication to leak from the patch. A series of class II recalls was initiated in March 2004, and in February 2008 ALZA Corporation recalled their 25 µg/h Duragesic patches due to a concern that small cuts in the gel reservoir could result in accidental exposure of patients or health care providers to the fentanyl gel.[144]
Brand names
Brand names include Sublimaze,[45] Actiq, Durogesic, Duragesic, Fentora, Matrifen, Haldid, Onsolis,[145] Instanyl,[146] Abstral,[147] Lazanda[148] and others.[149]
Cost
In the United States, the 800 mcg tablet was 6.75 times more expensive as of 2020 than the lozenge.[150][151]
Storage and disposal
The fentanyl patch is one of a few medications that may be especially harmful, and in some cases fatal, with just one dose, if misused by a child.[152][153] Unused fentanyl patches should be kept in a secure location out of children's sight and reach, such as a locked cabinet.
In British Columbia, Canada, where there are environmental concerns about toilet flushing or garbage disposal, pharmacists recommend that unused patches be sealed in a child-proof container which is then returned to a pharmacy.[154] In the United States where patches cannot always be returned through a medication take-back program, flushing is recommended for fentanyl patches because it is the fastest and surest way to remove them from the home to prevent them from ingestion by children, pets or others not intended to use them.[153][155]
Notable deaths
- Slipknot bassist Paul Gray died on May 24, 2010 from an overdose of morphine and fentanyl. [156]
- Medical examiners concluded that musician Prince died on April 21, 2016, from an accidental fentanyl overdose.[157] Fentanyl was among many substances identified in counterfeit pills recovered from his home, especially some that were mislabeled as Watson 385, a combination of hydrocodone and paracetamol.[157][158]
- Author & journalist Michelle McNamara died on April 21, 2016, from an accidental overdose; medical examiners determined fentanyl was a contributing factor.[159][160]
- Canadian video game composer Saki Kaskas died of a fentanyl overdose on November 11, 2016;[161] he had been battling heroin addiction for over a decade.[161]
- American rapper Lil Peep died of an accidental fentanyl overdose on November 15, 2017.[162][163]
- On January 19, 2018, the medical examiner-coroner for the county of Los Angeles said musician Tom Petty died from an accidental drug overdose as a result of mixing medications that included fentanyl, acetyl fentanyl, and despropionyl fentanyl (among others). He was reportedly treating "many serious ailments" that included a broken hip.[164]
- In 2018, American rapper Mac Miller died from an accidental overdose of fentanyl, cocaine and alcohol.[165]
- On December 16, 2018, American tech entrepreneur Colin Kroll, founder of social media video-sharing app Vine and quiz app HQ Trivia, died from an overdose of fentanyl, heroin, and cocaine.[166]
- On July 1, 2019, American baseball player Tyler Skaggs died from pulmonary aspiration while under the influence of fentanyl, oxycodone, and alcohol.[167]
- On January 1, 2020, American rapper, singer, and songwriter Lexii Alijai died from accidental toxicity resulting from the combination of alcohol and fentanyl.[168]
- On August 20, 2020, Justin Townes Earle died from an accidental overdose caused by cocaine laced with fentanyl.[169]
- On August 24, 2020, frontman Riley Gale from Grammy nominated Texas metal band Power Trip died as a result of the toxic effects of fentanyl in a manner that was ruled accidental.[170]
State use
In August 2018, Nebraska became the first American state to use fentanyl to execute a prisoner.[171][172][173] Carey Dean Moore, at the time one of the longest-serving death row inmates[174] in the United States, was executed at the Nebraska State Penitentiary. Moore received a lethal injection, administered as an intravenous series of four drugs that included fentanyl citrate, to inhibit breathing and render the subject unconscious. The other drugs included diazepam as a tranquilizer, cisatracurium besylate as a muscle relaxant, and potassium chloride to stop the heart.[175][176] The use of fentanyl in execution caused concern among death penalty experts because it was part of a previously untested drug cocktail.[171][173] The execution was also protested by anti-death penalty advocates at the prison during the execution and later at the Nebraska capitol building.[175][176]
Russian Spetsnaz security forces used a fentanyl analogue, or derivative, to incapacitate people rapidly in the Moscow theater hostage crisis in 2002. The siege was ended, but some hostages may have died from the gas after their health was severely taxed during the days long siege.[citation needed] The Russian Health Minister later stated that the gas was based on fentanyl,[177] but the exact chemical agent has not been identified.
Veterinary use
Fentanyl in injectable formulation is commonly used for analgesia and as a component of balanced sedation and general anesthesia in small animal patients. Its potency and short duration of action make it particularly useful in critically ill patients. In addition, it tends to cause less vomiting and regurgitation than other pure-opiate (codeine, morphine) and synthetic pure-opioid agonists (oxycodone, hydromorphone) when given as a continuous post-operative infusion. As with other pure-opioid agonists, fentanyl can be associated with dysphoria in both dogs and cats.[citation needed]
Transdermal fentanyl has also been used for many years in dogs and cats for post-operative analgesia. This is usually done with off-label fentanyl patches manufactured for humans with chronic pain. In 2012, a highly concentrated (50 mg/mL) transdermal solution, trade name Recuvyra, has become commercially available for dogs only. It is FDA approved to provide four days of analgesia after a single application before surgery. It is not approved for multiple doses or other species.[178] The drug is also approved in Europe.[179]
See also
References
- ^ Bonewit-West, K.; Hunt, S.A.; Applegate, E. (2012). Today's Medical Assistant: Clinical and administrative procedures. Elsevier Health Sciences. p. 571. ISBN 9781455701506.
- ^ "FDA-sourced list of all drugs with black box warnings (Use Download Full Results and View Query links.)". nctr-crs.fda.gov. FDA. Retrieved 22 October 2023.
- ^ a b Clinically Oriented Pharmacology (2nd ed.). Quick Review of Pharmacology. 2010. p. 172.
- ^ a b c d e f g h i j "Fentanyl, Fentanyl Citrate, Fentanyl Hydrochloride". The American Society of Health-System Pharmacists. Archived from the original on 14 December 2017. Retrieved 8 December 2017.
- ^ "Guideline for administration of fentanyl for pain relief in labour" (PDF). RCP. Archived (PDF) from the original on 4 March 2016. Retrieved 7 October 2015.
Onset of action after I.V. administration of Fentanyl is 3–5 minutes; duration of action is 30–60 minutes.
- ^ "Fentanyl drug overdose". CDC Injury Center. 29 August 2017. Archived from the original on 15 December 2017. Retrieved 14 December 2017.
- ^ "Fentanyl buccal 400 mcg tablets".
- ^ a b Fentanyl side effects in detail. Drugs.com (Report). Archived from the original on 16 June 2018. Retrieved 16 June 2018.
- ^ "Commission on Narcotic Drugs takes decisive step to help prevent deadly fentanyl overdoses" (Press release). Commission on Narcotic Drugs, United Nations Office on Drugs and Crime. 16 March 2017. Archived from the original on 20 March 2017. Retrieved 19 March 2017.
- ^ Stanley, T.H. (April 1992). "The history and development of the fentanyl series". Journal of Pain and Symptom Management. 7 (3 suppl): S3–S7. doi:10.1016/0885-3924(92)90047-L. PMID 1517629.
- ^ Narcotic Drugs Estimated World Requirements for 2017 / Statistics for 2015 (PDF) (Report). New York: United Nations. 2016. p. 40. ISBN 978-92-1-048163-2. Archived (PDF) from the original on 22 October 2017. Retrieved 14 December 2017.
- ^ "Fentanyl and analogues". LverTox. 16 October 2017. Archived from the original on 7 January 2017. Retrieved 14 December 2017.
- ^ "The Top 300 of 2019". ClinCalc. Retrieved 16 October 2021.
- ^ "Fentanyl Drug Usage Statistics". ClinCalc. Retrieved 16 October 2021.
- ^ World Health Organization model list of essential medicines (22nd list (2021) ed.). Geneva, CH: World Health Organization. 2021. hdl:10665/345533. WHO/MHP/HPS/EML/2021.02.
- ^ a b c d Overdose Death Rates (Report). National Institute on Drug Abuse (NIDA). 29 January 2021.
- ^ Overdose death rates (Report). National Institute on Drug Abuse. 15 September 2017. Archived from the original on 13 December 2017. Retrieved 14 December 2017.
- ^ "Nearly half of opioid-related overdose deaths involve fentanyl". National Institute on Drug Abuse. 1 May 2018. Archived from the original on 14 June 2018. Retrieved 14 June 2018.
- ^ Hedegaard H, Bastian BA, Trinidad JP, Spencer M, Warner M (December 2018). Drugs most frequently involved in drug overdose deaths: United States, 2011-2016. National Vital Statistics Reports (Report). Vol. 67. pp. 1–14. PMID 30707673.
- ^ Fentanyl drug overdose (Report). Center for Disease Control. 21 December 2018. Retrieved 28 April 2019.
- ^ Douglas, J. (23 February 2018). "In Asia, the unintended consequences of fentanyl". The Globe and Mail.
- ^ Brunton LL, Hilal-Dandan R, Knollmann BC (5 December 2017). Goodman & Gilman's: The pharmacological basis of therapeutics (13th ed.). New York, NY. ISBN 978-1-259-58473-2. OCLC 993810322.
{{cite book}}: CS1 maint: location missing publisher (link) - ^ a b c d Gropper MA, Miller RD, Eriksson LI, Fleisher LA, Wiener-Kronish JP, Cohen LH, Leslie K (7 October 2019). Miller's Anesthesia (9th ed.). Philadelphia, PA. ISBN 978-0-323-61264-7. OCLC 1124935549.
{{cite book}}: CS1 maint: location missing publisher (link) - ^ Godwin SA, Burton JH, Gerardo CJ, Hatten BW, Mace SE, Silvers SM, Fesmire FM (February 2014). "Clinical policy: procedural sedation and analgesia in the emergency department". Annals of Emergency Medicine. 63 (2): 247–58.e18. doi:10.1016/j.annemergmed.2013.10.015. PMID 24438649.
- ^ Smith HS, Colson J, Sehgal N (April 2013). "An update of evaluation of intravenous sedation on diagnostic spinal injection procedures". Pain Physician. 16 (2 Suppl): SE217–SE228. doi:10.36076/ppj.2013/16/SE217. PMID 23615892. Archived from the original on 19 October 2015. Retrieved 1 May 2017.
- ^ Gudin MA, López R, Estrada J, Ortigosa E (28 November 2011). "Neuraxial blockade: Subarachnoid anesthesia". Essentials of Regional Anesthesia. New York, NY: Springer New York. pp. 261–291. doi:10.1007/978-1-4614-1013-3_11. ISBN 978-1-4614-1012-6. Retrieved 4 July 2021.
- ^ Buggy, D. (1 July 2008). "Anesthesiology: D.E. Longnecker, D.L. Brown, M.F. Newman and W.M. Zapol, Editors, McGraw Hill, New York (2007) ISBN: 0071459847, 2278 pp, hardcover, $249 ..." Regional Anesthesia and Pain Medicine (book review). 33 (4). BMJ Journals: 380. doi:10.1016/j.rapm.2008.03.003. ISSN 1098-7339.
- ^ Bujedo BM (July 2014). "Current evidence for spinal opioid selection in postoperative pain". The Korean Journal of Pain. 27 (3): 200–209. doi:10.3344/kjp.2014.27.3.200. PMC 4099232. PMID 25031805.
- ^ a b Moisés EC, de Barros Duarte L, de Carvalho Cavalli R, Lanchote VL, Duarte G, da Cunha SP (August 2005). "Pharmacokinetics and transplacental distribution of fentanyl in epidural anesthesia for normal pregnant women". European Journal of Clinical Pharmacology. 61 (7): 517–522. doi:10.1007/s00228-005-0967-9. PMID 16021436. S2CID 26065578.
- ^ White LD, Hodsdon A, An GH, Thang C, Melhuish TM, Vlok R (November 2019). "Induction opioids for caesarean section under general anaesthesia: A systematic review and meta-analysis of randomised controlled trials". International Journal of Obstetric Anesthesia. 40: 4–13. doi:10.1016/j.ijoa.2019.04.007. PMID 31230994. S2CID 181816438.
- ^ Karlsen AP, Pedersen DM, Trautner S, Dahl JB, Hansen MS (June 2014). "Safety of intranasal fentanyl in the out-of-hospital setting: a prospective observational study". Annals of Emergency Medicine. 63 (6): 699–703. doi:10.1016/j.annemergmed.2013.10.025. PMID 24268523.
- ^ a b Murphy A, O'Sullivan R, Wakai A, Grant TS, Barrett MJ, Cronin J, et al. (October 2014). "Intranasal fentanyl for the management of acute pain in children". The Cochrane Database of Systematic Reviews. 10 (10): CD009942. doi:10.1002/14651858.CD009942.pub2. PMC 6544782. PMID 25300594.
- ^ Plante GE, VanItallie TB (October 2010). "Opioids for cancer pain: The challenge of optimizing treatment". Metabolism. 59 (Suppl 1): S47–S52. doi:10.1016/j.metabol.2010.07.010. PMID 20837194.
- ^ "Fentanyl". www.dea.gov (factsheet). Drug Enforcement Agency. Retrieved 4 December 2018.
- ^ a b c Jasek, W., ed. (2007). Austria-Codex (in German) (62nd ed.). Vienna, AU: Österreichischer Apothekerverlag. pp. 2621 ff. ISBN 978-3-85200-181-4.
- ^ "Fentanyl patches (Durogesic) for chronic pain". NPS Medicinewise.
{{cite web}}: CS1 maint: url-status (link) - ^ Derry S, Stannard C, Cole P, Wiffen PJ, Knaggs R, Aldington D, Moore RA (October 2016). Fentanyl for neuropathic pain in adults. The Cochrane Database of Systematic Reviews (Report). Vol. 10. p. CD011605. doi:10.1002/14651858.CD011605.pub2. PMC 6457928. PMID 27727431.
- ^ a b c "Abstral sublingual tablets". Summary of product characteristics. UK Electronic Medicines Compendium. May 2016. Archived from the original on 23 March 2017. Retrieved 1 May 2017.
- ^ "Abstral (Fentanyl sublingual tablets for breakthrough cancer pain)". P & T. 36 (2): 2–28. February 2011. PMC 3086091. PMID 21560267.
- ^ Ward J, Laird B, Fallon M (2011). "The UK breakthrough cancer pain registry: Origin, methods and preliminary data". BMJ Supportive & Palliative Care. 1: A24. doi:10.1136/bmjspcare-2011-000020.71. S2CID 73185220.
- ^ Aurilio C, Pace MC, Pota V, Sansone P, Barbarisi M, Grella E, Passavanti MB (May 2009). "Opioids switching with transdermal systems in chronic cancer pain". Journal of Experimental & Clinical Cancer Research. 28: 61. doi:10.1186/1756-9966-28-61. PMC 2684533. PMID 19422676.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Minami S, Kijima T, Nakatani T, Yamamoto S, Ogata Y, Hirata H, et al. (8 October 2014). "Opioid switch from low dose of oral oxycodone to transdermal fentanyl matrix patch for patients with stable thoracic malignancy-related pain". BMC Palliative Care. 13 (1): 46. doi:10.1186/1472-684X-13-46. PMC 4195703. PMID 25313295.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ a b Shachtman N (September 10, 2009). "Airborne EMTs Shave Seconds to Save Lives in Afghanistan". Danger Room. Wired. Archived from the original on July 6, 2010. Retrieved July 1, 2010.
- ^ Koo PJ (June 2005). "Postoperative pain management with a patient-controlled transdermal delivery system for fentanyl". American Journal of Health-System Pharmacy. 62 (11): 1171–1176. doi:10.1093/ajhp/62.11.1171. PMID 15914877. Archived from the original on 6 August 2018. Retrieved 28 March 2016.
- ^ a b "Fentanyl". Drugs@FDA. FDA approved drug products. U.S. Food and Drug Administration. Archived from the original on 13 March 2013. Retrieved 4 September 2013.
- ^ a b c Mayes S, Ferrone M (December 2006). "Fentanyl HCl patient-controlled iontophoretic transdermal system for the management of acute postoperative pain". The Annals of Pharmacotherapy. 40 (12): 2178–2186. doi:10.1345/aph.1H135. PMID 17164395. S2CID 24454875. Archived from the original on 1 October 2012. Retrieved 17 December 2010.
- ^ Smydo J (1979). "Delayed respiratory depression with fentanyl". Anesthesia Progress. 26 (2): 47–48. PMC 2515983. PMID 295585.
- ^ van Leeuwen L, Deen L, Helmers JH (August 1981). "A comparison of alfentanil and fentanyl in short operations with special reference to their duration of action and postoperative respiratory depression". Der Anaesthesist. 30 (8): 397–399. PMID 6116461.
- ^ Brown DL (November 1985). "Postoperative analgesia following thoracotomy. Danger of delayed respiratory depression". Chest. 88 (5): 779–780. doi:10.1378/chest.88.5.779. PMID 4053723. S2CID 1836168.
- ^ Nilsson C, Rosberg B (June 1982). "Recurrence of respiratory depression following neurolept analgesia". Acta Anaesthesiologica Scandinavica. 26 (3): 240–241. doi:10.1111/j.1399-6576.1982.tb01762.x. PMID 7113633. S2CID 9232457.
- ^ "Fentanyl patches: serious and fatal overdose from dosing errors, accidental exposure, and inappropriate use". Drug Safety Update. 2 (2): 2. September 2008. Archived from the original on 1 January 2015.
- ^ "Fentanyl patch can be deadly to children". Drugs.com. U.S. Food and Drug Administration. April 19, 2012. Archived from the original on July 25, 2013. Retrieved July 30, 2013.
- ^ Stanley TH, Petty WC (31 March 1983). New Anesthetic Agents, Devices, and Monitoring Techniques. Springer. ISBN 978-90-247-2796-4. Retrieved 20 October 2007.
- ^ Topacoglu H (November 2005). "Respiratory arrest after low-dose fentanyl". Annals of Saudi Medicine. 25 (6): 508–510. doi:10.5144/0256-4947.2005.508. PMC 6089740. PMID 16438465.
- ^ a b c d e f g h i j k l m n o p q r s t Hemmings, H.C.; Egan, T.D. (19 October 2018). Pharmacology and Physiology for Anesthesia: Foundations and clinical application (2nd ed.). Philadelphia, PA. ISBN 9780323568869. OCLC 1063667873.
{{cite book}}: CS1 maint: location missing publisher (link) - ^ McLoughlin R, McQuillan R (September 1997). "Transdermal fentanyl and respiratory depression". Palliative Medicine. 11 (5): 419. doi:10.1177/026921639701100515. PMID 9472602.
- ^ Bülow HH, Linnemann M, Berg H, Lang-Jensen T, LaCour S, Jonsson T (August 1995). "Respiratory changes during treatment of postoperative pain with high dose transdermal fentanyl". Acta Anaesthesiologica Scandinavica. 39 (6): 835–839. doi:10.1111/j.1399-6576.1995.tb04180.x. PMID 7484044. S2CID 22781991.
- ^ Regnard C, Pelham A (December 2003). "Severe respiratory depression and sedation with transdermal fentanyl: four case studies". Palliative Medicine. 17 (8): 714–716. doi:10.1191/0269216303pm838cr. PMID 14694924. S2CID 32985050.
- ^ Chambers D, Huang CL, Matthews G (1 September 2019) [2015]. "Section 2 - Respiratory physiology: Chapter 25: Anaesthesia and the lung". Basic Physiology for Anaesthetists. Cambridge medicine (2nd ed.). Cambridge, UK: Cambridge University Press. pp. 107–110. doi:10.1017/CBO9781139226394.027. ISBN 9781108463997. OCLC 1088737571. Retrieved 9 August 2021 – via Google Books.
- ^ Burns G, DeRienz RT, Baker DD, Casavant M, Spiller HA (June 2016). Seifert SA, Buckley N, Seger D, Thomas S, Caravati EM (eds.). "Could chest wall rigidity be a factor in rapid death from illicit fentanyl abuse?". Clinical Toxicology. 54 (5). McLean, VA: American Academy of Clinical Toxicology (AACT) / European Association of Poisons Centres and Clinical Toxicologist / Taylor & Francis: 420–423. doi:10.3109/15563650.2016.1157722. OCLC 8175535. PMID 26999038. S2CID 23149685.
- ^ a b Torralva R, Janowsky A (November 2019). Trew KD, Dodenhoff R, Vore M, Siuciak JA, Perry J, Wood C, Blumer J (eds.). "Noradrenergic Mechanisms in Fentanyl-Mediated Rapid Death Explain Failure of Naloxone in the Opioid Crisis" (PDF). The Journal of Pharmacology and Experimental Therapeutics. 371 (2). Rockville, Maryland, United States of America: American Society for Pharmacology and Experimental Therapeutics: 453–475. doi:10.1124/jpet.119.258566. LCCN sf80000806. OCLC 1606914. PMC 6863461. PMID 31492824. Archived from the original (PDF) on 9 March 2020. Retrieved 9 August 2021.
- ^ Petrou I (1 September 2016). Levine L, Tan TQ, Shippoli J (eds.). "Chest wall rigidity in fentanyl abuse: illicit fentanyl could be a major factor in sudden onset of this potentially lethal adverse event". Contemporary Pedriatics. 33 (9). Cranbury, New Jersey, United States of America: Intellisphere, LLC./ MJH Life Sciences (Multimedia Medical LLC). ISSN 8750-0507. OCLC 10956598. Retrieved 9 August 2021 – via Gale Academic OneFile.
- ^ "Fatalities caused by novel opioids: a review" Olaf H. Drummer 2018.
- ^ "Narcan (Naloxone hydrochloride injection)". RxList. Side effects, warnings, uses. Retrieved 3 March 2020.
- ^ "Fentanyl patches warning". Pharmaceutical Journal. Archived from the original on 8 April 2016. Retrieved 28 March 2016.
- ^ "MHRA warns about fentanyl patches after children exposed". Pharmaceutical Journal. Archived from the original on 9 April 2016. Retrieved 28 March 2016.
- ^ Katz, J. (September 2, 2017). "The first count of Fentanyl deaths in 2016 - up 540% in three years". The New York Times. Archived from the original on September 4, 2017. Retrieved September 4, 2017.
- ^ "Reported law enforcement encounters testing positive for Fentanyl increase across U.S." CDC Injury Center. www.cdc.gov (Press release). Drug Overdose. Centers for Disease Control. 9 August 2021. Retrieved 3 March 2022.
- ^ "Fentanyl Overdose". Huffington Post. May 20, 2016. Archived from the original on June 5, 2016. Retrieved June 4, 2016.
- ^ Fentanyl-detected in illicit drug overdose deaths, January 1, 2012 to April 30, 2016 (PDF) (Report). British Columbia Coroners Service. Archived from the original (PDF) on 25 June 2016. Retrieved 9 June 2016.
- ^ "Fentanyl contributed to hundreds of deaths in Canada so far this year". globalnews.ca. 31 July 2017. Archived from the original on 14 September 2017. Retrieved 14 September 2017.
- ^ Scaccia, A. (9 October 2018). "How Fentanyl is contaminating America's cocaine supply". Rolling Stone. Retrieved 5 November 2018.
- ^ Daly, M. (30 July 2019). "Exclusive data reveals just how often Fentanyl is in cocaine". Vice. Retrieved 9 January 2020.
- ^ Chang, A. (3 December 2018). "What it means for the U.S. that China will label Fentanyl as 'a controlled substance'". All Things Considered. NPR. Retrieved 6 December 2018.
- ^ "Heroin and cocaine prices in Europe and USA". dataunodc.un.org. Statistics and Data. Retrieved 24 July 2019.
- ^ "Coronavirus triggers UK shortage of illicit drugs". Society. The Guardian. 12 April 2020. Retrieved 23 April 2020.
- ^ Reinberg, S. (12 December 2018). "Fentanyl overtakes heroin as the no. 1 opioid overdose killer". CBS News. Retrieved 12 December 2018.
- ^ "Opioid and Stimulant-related Harms in Canada". Ottawa, Canada: Public Health Agency of Canada. December 2021. Retrieved 18 March 2022.
{{cite web}}: Cite uses deprecated parameter|authors=(help) - ^ "Fentanyl citrate injection, USP" (PDF). U.S. Food and Drug Administration.
- ^ Yadav SK, Maurya CK, Gupta PK, Jain AK, Ganesan K, Bhattacharya R (June 2014). "Synthesis and biological evaluation of some novel 1-substituted fentanyl analogs in Swiss albino mice". Interdisciplinary Toxicology. 7 (2): 93–102. doi:10.2478/intox-2014-0013. PMC 4427721. PMID 26109885.
- ^ "Fentanyl". Drugbank.
- ^ Vardanyan RS, Hruby VJ (March 2014). "Fentanyl-related compounds and derivatives: current status and future prospects for pharmaceutical applications". Future Medicinal Chemistry. 6 (4): 385–412. doi:10.4155/fmc.13.215. PMC 4137794. PMID 24635521.
- ^ "Fentanyl". Drug Enforcement Administration. image 4 of 17.
- ^ "American College of Medical Toxicology Position Statement on Fentanyl Exposure" (Press release).
{{cite press release}}: CS1 maint: url-status (link) - ^ Thors L, Öberg L, Forsberg E, Wigenstam E, Larsson A, Bucht A (September 2020). "Skin penetration and decontamination efficacy following human skin exposure to fentanyl". Toxicology in Vitro. 67: 104914. doi:10.1016/j.tiv.2020.104914. PMID 32540164. S2CID 219704174.
- ^ Ross, Casey (9 August 2017). "Are people really falling ill from touching fentanyl? In most cases, scientists say no". Stat News. Retrieved 7 August 2021.
- ^ Herman, Paul Alexander (24 February 2020). "Media Reports of Unintentional Opioid Exposure of Public Safety First Responders in North America". Journal of Medical Toxicology. 16: 112–115. doi:https://doi.org/10.1007/s13181-020-00762-y.
{{cite journal}}: Check|doi=value (help); External link in|doi= - ^ del Pozo, Brandon; Sightes, Emily (24 November 2021). "Can touch this: training to correct police officer beliefs about overdose from incidental contact with fentanyl". Health & Justice. 9 (34). doi:https://doi.org/10.1186/s40352-021-00163-5.
{{cite journal}}: Check|doi=value (help); External link in|doi= - ^ "Fentanyl | CDC's Response to the Opioid Overdose Epidemic | CDC". www.cdc.gov. 2 October 2021. Retrieved 27 April 2022.
- ^ "One Pill Can Kill". www.dea.gov. Retrieved 27 April 2022.
- ^ "Drug Free NJ - Home". drugfreenj.org. Retrieved 27 April 2022.
- ^ Fuller, Kristen (10 March 2022). "Opioid Rehab & Addiction Treatment Programs Near Me". American Addiction Centers. Retrieved 27 April 2022.
- ^ "About Hazelden Betty Ford and Our Mission". www.hazeldenbettyford.org. Retrieved 27 April 2022.
- ^ a b c Yaksh, T.; Wallace, M. (2011). Goodman & Gilman's: The Pharmacological Basis of Therapeutics. New York, NY: McGraw-Hill. ISBN 978-0-07-162442-8.
- ^ Katzung, B.G. (2017). Basic & Clinical Pharmacology (14th ed.). New York, NY. ISBN 9781259641152. OCLC 1015240036.
{{cite book}}: CS1 maint: location missing publisher (link) - ^ Raynor K, Kong H, Chen Y, Yasuda K, Yu L, Bell GI, Reisine T (February 1994). "Pharmacological characterization of the cloned kappa-, delta-, and mu-opioid receptors". Molecular Pharmacology. 45 (2): 330–334. PMID 8114680.
- ^ a b Suzuki J, El-Haddad S (February 2017). "A review: Fentanyl and non-pharmaceutical fentanyls". Drug and Alcohol Dependence. 171: 107–116. doi:10.1016/j.drugalcdep.2016.11.033. PMID 28068563.
- ^ "Fentanyl". www.drugbank.ca. Retrieved 18 January 2019.
- ^ a b Butterworth IV, J.V.; Wasnick, J.D.; MacKey, D.C. (21 August 2018). Morgan & Mikhail's Clinical Anesthesiology (6th ed.). New York, NY. ISBN 9781259834424. OCLC 1039081701.
{{cite book}}: CS1 maint: location missing publisher (link) - ^ Baselt, R. (2017) Disposition of Toxic Drugs and Chemicals in Man, 11th edition, Biomedical Publications, Foster City, CA, pp. 883–886.
- ^ Vandergrift GW, Hessels AJ, Palaty J, Krogh ET, Gill CG (April 2018). "Paper spray mass spectrometry for the direct, semi-quantitative measurement of fentanyl and norfentanyl in complex matrices". Clinical Biochemistry. 54: 106–111. doi:10.1016/j.clinbiochem.2018.02.005. PMID 29432758.
- ^ Vandergrift GW, Hessels AJ, Palaty J, Krogh ET, Gill CG (April 2018). "Paper spray mass spectrometry for the direct, semi-quantitative measurement of fentanyl and norfentanyl in complex matrices". Clinical Biochemistry. 54: 106–111. doi:10.1016/j.clinbiochem.2018.02.005. PMID 29432758. 10.25316/IR-4343.
- ^ López-Muñoz F, Alamo C (April 2009). "The consolidation of neuroleptic therapy: Janssen, the discovery of haloperidol and its introduction into clinical practice". Brain Research Bulletin. 79 (2): 130–141. doi:10.1016/j.brainresbull.2009.01.005. PMID 19186209. S2CID 7720401.
- ^ Black J (March 2005). "A personal perspective on Dr. Paul Janssen" (PDF). Journal of Medicinal Chemistry. 48 (6): 1687–1688. doi:10.1021/jm040195b. PMID 15771410. Archived from the original (PDF) on 10 October 2007.
- ^ "Fentanyl citrate injection, solution [Hospira, Inc.]". Daily Med (Dailymed.nlm.nih.gov). U.S. National Institutes of Health. Archived from the original on 21 March 2010. Retrieved 31 March 2022.
- ^ "Fentanyl (sublimaze)". Clinical Pharmacology and Therapeutics. 9 (5): 704–706. September 1968. doi:10.1002/cpt196895704. PMID 5676808. S2CID 9743189.
- ^ "ACTIQ® (fentanyl citrate) oral transmucosal lozenge (1968 version revised in 2011)" (PDF). US Food and Drug Administration. December 2011. Archived (PDF) from the original on 10 February 2017. Retrieved 26 December 2017.
- ^ a b "Questions and Answers about Onsolis (fentanyl buccal soluble film)". US Food and Drug Administration. 16 July 2009. Archived from the original on 22 July 2017. Retrieved 26 December 2017.
- ^ "Misuse of Drugs Act 1971". Archived from the original on 14 November 2012. Retrieved 22 March 2017.
- ^ "RelayHealth's pharmacy connectivity network and reach, aligned with McKesson Specialty Care Solutions' REMS expertise, expands cancer patients' access to pain therapy". Atlanta. 20 January 2011. Archived from the original on 29 January 2016. Retrieved 5 November 2015.
- ^ Shelley, S. (22 April 2011). "With a few stumbles, REMS begins to hit its atride". Pharmaceutical Commerce. Archived from the original on 29 January 2016. Retrieved 5 November 2015.
- ^ "Procedures, programs and drugs that require precertification: Participating provider precertification list" (PDF). Aetna Inc. Archived from the original (PDF) on 9 July 2021. Retrieved 4 July 2021.
- ^ "Notice regarding precertification requirement" (PDF). BlueCross BlueShield of Arizona. 5 November 2007. Archived from the original (PDF) on 28 August 2008.
- ^ "Medications requiring precertification". Oxford Health Plans. Archived from the original on 15 October 2006.
- ^ "Canada's Controlled Drugs and Substances Act". laws.justice.gc.ca. Retrieved 8 September 2018.
- ^ Naylor, A. (6 January 2020). "What we can learn from a tiny Baltic country's two-decade Fentanyl crisis". Vice.
- ^ Townsend, M. (1 December 2018). "Dark web dealers voluntarily ban deadly fentanyl". The Guardian. Retrieved 3 December 2018.
- ^ Ducharme, J. (3 December 2018). "China has promised to crack down on Fentanyl. Here's what that could mean for overdose deaths in the U.S." Time. Retrieved 6 December 2018.
- ^ Boddiger D (August 2006). "Fentanyl-laced street drugs "kill hundreds"". Lancet. 368 (9535). London, UK: 569–570. doi:10.1016/S0140-6736(06)69181-2. PMID 16909503. S2CID 39788629.
- ^ "Synthetic drug fentanyl causes overdose boom in Estonia". BBC News. 30 March 2012. Archived from the original on 28 July 2018. Retrieved 21 June 2018.
- ^ a b "Fentanyl" (PDF). U.S. Drug Enforcement Administration. March 2015. Archived (PDF) from the original on 11 June 2016. Retrieved 2 June 2016.
- ^ a b "Mims, B. (11 November 2004). "Painkiller is topic of inquiry". The Salt Lake Tribune. Archived from the original on 24 December 2007.
- ^ Mars SG, Rosenblum D, Ciccarone D (May 2019). "Illicit fentanyls in the opioid street market: Desired or imposed?". Addiction. 114 (5): 774–780. doi:10.1111/add.14474. PMC 6548693. PMID 30512204.
- ^ "CDC Nonpharmaceutical Fentanyl-related deaths – multiple states, April 2005 – March 2007". Cdc.gov. Archived from the original on 26 July 2010. Retrieved 28 July 2010.
- ^ "DEA Microgram Bulletin". Office of Forensic Sciences. Washington, DC: U.S. Drug Enforcement Administration. June 2006. Archived from the original on 21 July 2009. Retrieved 22 June 2009.
- ^ Tanner, C. (2016). "Thousands of fentanyl pills confiscated in Utah drug raid". The Salt Lake Tribune. Archived from the original on 24 November 2016. Retrieved 23 November 2016.
- ^ "Cottonwood Heights drug bust one of the largest in Utah history". fox13now.com. 22 November 2016. Archived from the original on 23 November 2016. Retrieved 23 November 2016.
- ^ "U.S. border officers make largest-ever fentanyl bust: 254 pounds hidden under cucumbers". The Washington Post. 31 January 2019. Retrieved 8 June 2020.
- ^ a b "List of Schedule I Drugs". U.S. Department of Justice. Archived from the original on 9 January 2010.
- ^ Kram TC, Cooper DA, Allen AC (October 1981). "Behind the identification of China White". Analytical Chemistry. 53 (12): 1379A–1386A. doi:10.1021/ac00235a003. PMID 7294353.
- ^ Van Bever WF, Niemegeers CJ, Janssen PA (October 1974). "Synthetic analgesics. Synthesis and pharmacology of the diastereoisomers of N-(3-methyl-1-(2-phenylethyl)-4-piperidyl)-N-phenylpropanamide and N-(3-methyl-1-(1-methyl-2-phenylethyl)-4-piperidyl)-N-phenylpropanamide". Journal of Medicinal Chemistry. 17 (10): 1047–1051. doi:10.1021/jm00256a003. PMID 4420811.
- ^ "Recommendations for Laboratory Testing for Acetyl Fentanyl and Patient Evaluation and Treatment for Overdose with Synthetic Opioids". Centers for Disease Control and Prevention. 20 June 2013. Archived from the original on 24 June 2013. Retrieved 20 June 2013.
{{cite web}}: Cite uses deprecated parameter|authors=(help) - ^ Characteristics of Fentanyl overdose — Massachusetts, 2014–2016 (Report). Centers for Disease Control and Prevention. 14 April 2017.
- ^ "Lethal fentanyl profiting gangs in Western Canada while deaths climb". Metro News Edmonton. 6 August 2015. Archived from the original on 4 September 2015.
- ^ "Fentanyl doesn't discriminate, killing the homeless and young professionals". Edmonton Journal. 22 August 2015. Archived from the original on 20 December 2016.
- ^ Mangione, K.; Hasegawa, R. (9 December 2021). "2021 is now B.C.'s deadliest year in the opioid crisis, with 2 months of data left to collect". CTV News.
- ^ "Winnipeg Naloxone-distribution program could prevent fentanyl deaths". CBC News. CBC. Archived from the original on 31 May 2018. Retrieved 16 January 2018.
- ^ Cooper, S.; Bell, S.; Russell, A. (1 December 2018). "China won't stop flood of fentanyl into Canada, sources say". National. Global News. Canada. Retrieved 21 July 2021.
- ^ Bonini, T. (13 October 2017). "Could fentanyl be Australia's next deadly drug epidemic?". ABC News. Australian Broadcasting Corporation. Archived from the original on 8 May 2018. Retrieved 6 April 2018.
- ^ "Fentanyl found at New Zealand festival". KnowYourStuffNZ. 20 March 2018. Archived from the original on 7 April 2018. Retrieved 6 April 2018.
- ^ Buchanan, J. (27 March 2018). "NZ's 'deadly' indifference to drug overdose antidote". HealthCentral NZ. Archived from the original on 7 April 2018. Retrieved 6 April 2018.
- ^ Beech, H.; Nang, S. (19 May 2020). "Raids reveal massive Fentanyl production in Myanmar". The New York Times. Retrieved 2 May 2021.
- ^ UNODC report: Opium production drops again in Myanmar as the synthetic drug market expands. UNODC (Myanmar) (Report). Retrieved 2 May 2021.
- ^ "Pricara recalls 25 mcg/hr Duragesic (Fentanyl transdermal system) c II pain patches". Food and Drug Administration. 12 February 2008. Archived from the original on 13 May 2008. Retrieved 10 May 2008.
- ^ "Introducing Onsolis". Onsolis.com. Archived from the original on 22 July 2010. Retrieved 28 July 2010.
- ^ Instanyl (PDF) (Report). EPAR summary for the public. European Medicines Agency. Archived (PDF) from the original on 20 May 2012. Retrieved 28 July 2010.
- ^ "Abstral". Prescribing Information. Archived from the original on 14 July 2011. Retrieved 7 January 2011.
- ^ "Lazanda (fentanyl nasal spray) CII". Lazanda.com. Archived from the original on 25 April 2012. Retrieved 14 May 2012.
- ^ "Fentanyl". Drugs.com. International Drug Names. Archived from the original on 16 June 2018. Retrieved 23 January 2018.
- ^ "Fentanyl Buccal".
- ^ "Fentanyl Citrate Generic Actiq". GoodRx. Retrieved 27 May 2020.
- ^ Office of the Commissioner (26 January 2022). "Accidental Exposures to Fentanyl Patches Continue to Be Deadly to Children". FDA.
- ^ a b "Disposal of Unused Medicines: What You Should Know". US Food and Drug Administration. 1 February 2019. Retrieved 2 September 2019.
- ^ "Safe Disposal of Fentanyl Patches". College of Pharmacists of British Columbia. 2019. Retrieved 2 September 2019.
- ^ "Drug Disposal: Flush Potentially Dangerous Medicine (Flush list)". US Food and Drug Administration. 19 December 2018. Retrieved 2 September 2019.
- ^ Crumb MJ (21 June 2010). "Slipknot bassist died of an overdose of morphine". MSNBC. Associated Press. Archived from the original on 24 June 2010. Retrieved 21 June 2010.
- ^ a b Eligon, J.; Kovaleski, S.F. (June 2, 2016). "Prince died from accidental overdose of opioid painkiller". The New York Times. Archived from the original on August 5, 2017. Retrieved March 1, 2017.
- ^ "Official: Mislabeled pills found at Prince's estate contained fentanyl". Chicago Tribune. Archived from the original on August 22, 2016. Retrieved August 22, 2016.
- ^ Mizoguchi, K. (3 February 2017). "Patton Oswalt reveals wife died due to prescription medications and undiagnosed heart condition". People. Retrieved 5 November 2017.
- ^ McCartney, A. (3 February 2017). "Oswalt says heart condition, meds killed wife". AP News. AP Exclusive. Associated Press. Retrieved 30 April 2018.
- ^ a b Kurucz, J. (18 June 2019). "Completing Vancouver musician's album cathartic for those he left behind". Vancouver Courier. Retrieved 21 January 2020.
- ^ "Toxic combo of prescription drugs killed rapper". The New York Times. 8 December 2017. Archived from the original on 10 December 2017. Retrieved 9 December 2017.
- ^ Brown, A. (November 16, 2017). "Lil Peep, hero to the emo and hip-hop scenes, dies of suspected overdose at 21". Los Angeles Times. Archived from the original on November 18, 2017. Retrieved November 16, 2017.
- ^ Coscarelli, J. (2018). "Tom Petty Died From Accidental Drug Overdose Involving Opioids, Coroner Says". The New York Times. ISSN 0362-4331. Archived from the original on 20 January 2018. Retrieved 20 January 2018.
- ^ "Mac Miller's cause of death: Accidental Fentanyl, cocaine overdose". Rolling Stone. 5 November 2018. Retrieved 5 November 2018.
- ^ Paybarah, A. (3 October 2019). "'Mike's candyshop': Behind the overdose death of HQ Trivia's Colin Kroll". The New York Times. ISSN 0362-4331. Archived from the original on 3 October 2019. Retrieved 29 April 2021.
- ^ "Tyler Skaggs' autopsy: Fentanyl, oxycodone and alcohol led to death by choking on vomit". Los Angeles Times. 30 August 2019. Archived from the original on 30 August 2019. Retrieved 30 August 2019.
- ^ "Accidental overdose killed St. Paul rapper Lexii Alijai". MPR News. Retrieved 26 June 2021.
- ^ Bernstein, J. (1 December 2020). "Justin Townes Earle death ruled an accidental drug overdose". Rolling Stone.
- ^ https://www.rollingstone.com/music/music-news/riley-gale-power-trip-singer-dead-obit-1049964/
- ^ a b "Nebraska first to use fentanyl in execution". BBC News. 14 August 2018. Retrieved 15 August 2018.
- ^ "Nebraska becomes first state to use fentanyl in execution". NBC News. 14 August 2018. Retrieved 15 August 2018.
- ^ a b "Nebraska carries out 1st execution using Fentanyl in U.S." National Public Radio. Retrieved 15 August 2018.
- ^ "Nebraska will make history in its execution of a death row inmate". Newsweek. 14 August 2018. Retrieved 15 August 2018.
- ^ a b "Fentanyl used to execute Nebraska inmate, in a first for U.S.". The New York Times. 14 August 2018. Archived from the original on 14 August 2018. Retrieved 15 August 2018.
- ^ a b "Nebraska executes inmate using powerful opioid fentanyl". PBS NewsHour. Public Broadcasting System. 14 August 2018. Retrieved 15 August 2018.
- ^ "Russia names Moscow siege gas". BBC News. October 31, 2002. Archived from the original on June 19, 2018. Retrieved May 18, 2018.
- ^ "Original new animal drug application: Recuvyra" (PDF). Food and Drug Administration. Archived (PDF) from the original on 4 September 2015. Retrieved 22 September 2014.
- ^ "Recuvyra". Veterinary medicines. European Medicines Agency. Archived from the original on 4 March 2016. Retrieved 28 March 2016.
- Tschirhart JN, Zhang S (October 2020). "Fentanyl-induced block of hERG channels is exacerbated by hypoxia, hypokalemia, alkalosis, and the presence of hERG1b". Molecular Pharmacology. 98 (4): 508–517. doi:10.1124/mol.119.119271. PMID 32321735. S2CID 216084895.
External links
- Fentanyl. U.S. National Library of Medicine (Report). Drug Information Portal. National Institutes of Health.
- Fentanyl. US DEA information (Report). Archived from the original on 19 October 2002.
- Fentanyl. National Institute for Occupational Safety and Health (Report). Emergency Response Database. Center for Disease Control. 8 July 2021.
