COVID-19 vaccine


| Part of a series on the |
| COVID-19 pandemic |
|---|
 |
|
|
|
A COVID‑19 vaccine is a vaccine intended to provide acquired immunity against severe acute respiratory syndrome coronavirus 2 (SARS‑CoV‑2), the virus causing coronavirus disease 2019 (COVID‑19). Prior to the COVID‑19 pandemic, there was an established body of knowledge about the structure and function of coronaviruses causing diseases like severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS), which enabled accelerated development of various vaccine technologies during early 2020.[1] On 10 January 2020, the SARS-CoV-2 genetic sequence data was shared through GISAID, and by 19 March, the global pharmaceutical industry announced a major commitment to address COVID-19.[2]
In Phase III trials, several COVID‑19 vaccines have demonstrated efficacy as high as 95% in preventing symptomatic COVID‑19 infections. As of March 2021[update], 12 vaccines were authorized by at least one national regulatory authority for public use: two RNA vaccines (the Pfizer–BioNTech vaccine and the Moderna vaccine), four conventional inactivated vaccines (BBIBP-CorV, CoronaVac, Covaxin, and CoviVac), four viral vector vaccines (Sputnik V, the Oxford–AstraZeneca vaccine, Convidecia, and the Johnson & Johnson vaccine), and two protein subunit vaccines (EpiVacCorona and RBD-Dimer).[3] In total, as of March 2021[update], 308 vaccine candidates were in various stages of development, with 73 in clinical research, including 24 in Phase I trials, 33 in Phase I–II trials, and 16 in Phase III development.[3]
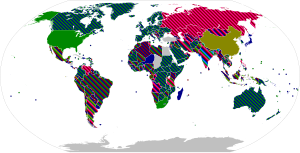
Many countries have implemented phased distribution plans that prioritize those at highest risk of complications, such as the elderly, and those at high risk of exposure and transmission, such as healthcare workers.[4] As of 30 March 2021[update], 574.25 million doses of COVID‑19 vaccine have been administered worldwide based on official reports from national health agencies.[5] AstraZeneca-Oxford anticipates producing 3 billion doses in 2021, Pfizer-BioNTech 1.3 billion doses, and Sputnik V, Sinopharm, Sinovac, and Johnson & Johnson 1 billion doses each. Moderna targets producing 600 million doses and Convidecia 500 million doses in 2021.[6][7] By December 2020, more than 10 billion vaccine doses had been preordered by countries,[8] with about half of the doses purchased by high-income countries comprising 14% of the world's population.[9]
Background


Prior to COVID‑19, a vaccine for an infectious disease had never been produced in less than several years—and no vaccine existed for preventing a coronavirus infection in humans.[10] However, vaccines have been produced against several animal diseases caused by coronaviruses, including (as of 2003) infectious bronchitis virus in birds, canine coronavirus, and feline coronavirus.[11] Previous projects to develop vaccines for viruses in the family Coronaviridae that affect humans have been aimed at severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS). Vaccines against SARS[12] and MERS[13] have been tested in non-human animals.
According to studies published in 2005 and 2006, the identification and development of novel vaccines and medicines to treat SARS was a priority for governments and public health agencies around the world at that time.[14][15][16] As of 2020, there is no cure or protective vaccine proven to be safe and effective against SARS in humans.[17][18] There is also no proven vaccine against MERS.[19] When MERS became prevalent, it was believed that existing SARS research may provide a useful template for developing vaccines and therapeutics against a MERS-CoV infection.[17][20] As of March 2020, there was one (DNA based) MERS vaccine which completed Phase I clinical trials in humans[21] and three others in progress, all being viral-vectored vaccines: two adenoviral-vectored (ChAdOx1-MERS, BVRS-GamVac) and one MVA-vectored (MVA-MERS-S).[22]
Planning and development
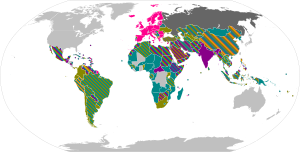
Since January 2020, vaccine development has been expedited via unprecedented collaboration in the multinational pharmaceutical industry and between governments.[23] According to the Coalition for Epidemic Preparedness Innovations (CEPI), the geographic distribution of COVID‑19 vaccine development puts North American entities having about 40% of the activity compared to 30% in Asia and Australia, 26% in Europe, and a few projects in South America and Africa.[23][24]
Multiple steps along the entire development path are evaluated, including:[10][25]
- the level of acceptable toxicity of the vaccine (its safety),
- targeting vulnerable populations,
- the need for vaccine efficacy breakthroughs,
- the duration of vaccination protection,
- special delivery systems (such as oral or nasal, rather than by injection),
- dose regimen,
- stability and storage characteristics,
- emergency use authorization before formal licensing,
- optimal manufacturing for scaling to billions of doses, and
- dissemination of the licensed vaccine.
Challenges
There have been several unique challenges with COVID-19 vaccine development.
The urgency to create a vaccine for COVID‑19 led to compressed schedules that shortened the standard vaccine development timeline, in some cases combining clinical trial steps over months, a process typically conducted sequentially over years.[26]
Timelines for conducting clinical research – normally a sequential process requiring years – are being compressed into safety, efficacy, and dosing trials running simultaneously over months, potentially compromising safety assurance.[26][27] As an example, Chinese vaccine developers and the government Chinese Center for Disease Control and Prevention began their efforts in January 2020,[28] and by March were pursuing numerous candidates on short timelines, with the goal to showcase Chinese technology strengths over those of the United States, and to reassure the Chinese people about the quality of vaccines produced in China.[26][29]
The rapid development and urgency of producing a vaccine for the COVID‑19 pandemic may increase the risks and failure rate of delivering a safe, effective vaccine.[24][30][31] Additionally, research at universities is obstructed by physical distancing and closing of laboratories.[32][33]
Vaccines must progress through several phases of clinical trials to test for safety, immunogenicity, effectiveness, dose levels and adverse effects of the candidate vaccine.[34][35] Vaccine developers have to invest resources internationally to find enough participants for Phase II–III clinical trials when the virus has proved to be a "moving target" of changing transmission rate across and within countries, forcing companies to compete for trial participants;[36] clinical trial organizers may encounter people unwilling to be vaccinated due to vaccine hesitancy[37] or disbelieving the science of the vaccine technology and its ability to prevent infection.[38] Even as new vaccines are developed during the COVID‑19 pandemic, licensure of COVID‑19 vaccine candidates requires submission of a full dossier of information on development and manufacturing quality.[39][40][41]
Organizations
Internationally, the Access to COVID-19 Tools Accelerator is a G20 and World Health Organization (WHO) initiative announced in April 2020.[42][43] It is a cross-discipline support structure to enable partners to share resources and knowledge. It comprises four pillars, each managed by two to three collaborating partners: Vaccines (also called "COVAX"), Diagnostics, Therapeutics, and Health Systems Connector.[44] The WHO's April 2020 "R&D Blueprint (for the) novel Coronavirus" documented a "large, international, multi-site, individually randomized controlled clinical trial" to allow "the concurrent evaluation of the benefits and risks of each promising candidate vaccine within 3–6 months of it being made available for the trial." The WHO vaccine coalition will prioritize which vaccines should go into Phase II and III clinical trials, and determine harmonized Phase III protocols for all vaccines achieving the pivotal trial stage.[45]
National governments have also been involved in vaccine development. Canada announced funding for 96 research vaccine research projects at Canadian companies and universities, with plans to establish a "vaccine bank" that could be used if another coronavirus outbreak occurs,[46] and to support clinical trials and develop manufacturing and supply chains for vaccines.[47] China provided low-rate loans to a vaccine developer through its central bank and "quickly made land available for the company" to build production plants.[27] Three Chinese vaccine companies and research institutes are supported by the government for financing research, conducting clinical trials, and manufacturing.[48] Great Britain formed a COVID‑19 vaccine task force in April 2020 to stimulate local efforts for accelerated development of a vaccine through collaborations of industry, universities, and government agencies. It encompassed every phase of development from research to manufacturing.[49] In the United States, the Biomedical Advanced Research and Development Authority (BARDA), a federal agency funding disease-fighting technology, announced investments to support American COVID‑19 vaccine development and manufacture of the most promising candidates.[27][50] In May 2020, the government announced funding for a fast-track program called Operation Warp Speed.[51][52]
Large pharmaceutical companies with experience in making vaccines at scale, including Johnson & Johnson, AstraZeneca, and GlaxoSmithKline (GSK), formed alliances with biotechnology companies, governments, and universities to accelerate progression to an effective vaccine.[27][26]
History

SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2), the virus that causes COVID-19, was isolated in late 2019.[53] Its genetic sequence was published on 11 January 2020, triggering an urgent international response to prepare for an outbreak and hasten the development of a preventive COVID-19 vaccine.[54][55][56] Since 2020, vaccine development has been expedited via unprecedented collaboration in the multinational pharmaceutical industry and between governments.[57] By June 2020, tens of billions of dollars were invested by corporations, governments, international health organizations, and university research groups to develop dozens of vaccine candidates and prepare for global vaccination programs to immunize against COVID‑19 infection.[55][58][59][60] According to the Coalition for Epidemic Preparedness Innovations (CEPI), the geographic distribution of COVID‑19 vaccine development shows North American entities to have about 40% of the activity, compared to 30% in Asia and Australia, 26% in Europe, and a few projects in South America and Africa.[54][57]
In February 2020, the World Health Organization (WHO) said it did not expect a vaccine against SARS‑CoV‑2 to become available in less than 18 months.[61] Virologist Paul Offit commented that, in hindsight, the development of a safe and effective vaccine within 11 months was a remarkable feat.[62] The rapidly growing infection rate of COVID‑19 worldwide during 2020 stimulated international alliances and government efforts to urgently organize resources to make multiple vaccines on shortened timelines,[63] with four vaccine candidates entering human evaluation in March (see COVID-19 vaccine § Trial and authorization status).[54][64]
On 24 June 2020, China approved the CanSino vaccine for limited use in the military and two inactivated virus vaccines for emergency use in high-risk occupations.[65] On 11 August 2020, Russia announced the approval of its Sputnik V vaccine for emergency use, though one month later only small amounts of the vaccine had been distributed for use outside of the phase 3 trial.[66]
The Pfizer–BioNTech partnership submitted an Emergency Use Authorization (EUA) request to the U.S. Food and Drug Administration (FDA) for the mRNA vaccine BNT162b2 (active ingredient tozinameran) on 20 November 2020.[67][68] On 2 December 2020, the United Kingdom's Medicines and Healthcare products Regulatory Agency (MHRA) gave temporary regulatory approval for the Pfizer–BioNTech vaccine,[69][70] becoming the first country to approve the vaccine and the first country in the Western world to approve the use of any COVID‑19 vaccine.[71][72][73] As of 21 December 2020, many countries and the European Union[74] had authorized or approved the Pfizer–BioNTech COVID‑19 vaccine. Bahrain and the United Arab Emirates granted emergency marketing authorization for the Sinopharm BIBP vaccine.[75][76] On 11 December 2020, the FDA granted an EUA for the Pfizer–BioNTech COVID‑19 vaccine.[77] A week later, they granted an EUA for mRNA-1273 (active ingredient elasomeran), the Moderna vaccine.[78][79][80][81]
On 31 March 2021, the Russian government announced that they had registered the first COVID‑19 vaccine for animals.[82] Named Carnivac-Cov, it is an inactivated vaccine for carnivorous animals, including pets, aimed at preventing mutations that occur during the interspecies transmission of SARS-CoV-2.[83]
In October 2022, China began administering an oral vaccine developed by CanSino Biologics using its adenovirus model.[84]
Despite the availability of mRNA and viral vector vaccines, worldwide vaccine equity has not been achieved. The ongoing development and use of whole inactivated virus (WIV) and protein-based vaccines has been recommended, especially for use in developing countries, to dampen further waves of the pandemic.[85][86]Vaccine types

As of January 2021, nine different technology platforms – with the technology of numerous candidates remaining undefined – are under research and development to create an effective vaccine against COVID‑19.[3][23] Most of the platforms of vaccine candidates in clinical trials are focused on the coronavirus spike protein and its variants as the primary antigen of COVID‑19 infection.[23] Platforms being developed in 2020 involved nucleic acid technologies (nucleoside-modified messenger RNA and DNA), non-replicating viral vectors, peptides, recombinant proteins, live attenuated viruses, and inactivated viruses.[10][23][24][30]
Many vaccine technologies being developed for COVID‑19 are not like vaccines already in use to prevent influenza, but rather are using "next-generation" strategies for precision on COVID‑19 infection mechanisms.[23][24][30] Vaccine platforms in development may improve flexibility for antigen manipulation and effectiveness for targeting mechanisms of COVID‑19 infection in susceptible population subgroups, such as healthcare workers, the elderly, children, pregnant women, and people with existing weakened immune systems.[23][24]
RNA vaccines

An RNA vaccine contains RNA which, when introduced into a tissue, acts as messenger RNA (mRNA) to cause the cells to build the foreign protein and stimulate an adaptive immune response which teaches the body how to identify and destroy the corresponding pathogen or cancer cells. RNA vaccines often, but not always, use nucleoside-modified messenger RNA. The delivery of mRNA is achieved by a coformulation of the molecule into lipid nanoparticles which protect the RNA strands and help their absorption into the cells.[87][88][89][90]
RNA vaccines were the first COVID-19 vaccines to be authorized in the United States and the European Union.[91][92] As of January 2021[update], authorized vaccines of this type are the Pfizer-BioNTech COVID‑19 vaccine
Severe allergic reactions are rare. In December 2020, 1,893,360 first doses of Pfizer-BioNTech COVID‑19 vaccine administration resulted in 175 cases of severe allergic reaction, of which 21 were anaphylaxis.[99] For 4,041,396 Moderna COVID-19 vaccine dose administrations in December 2020 and January 2021, only 10 cases of anaphylaxis were reported.[99] The lipid nanoparticles were most likely responsible for the allergic reactions.[99]
Adenovirus vector vaccines
These vaccines are examples of non-replicating viral vectors, using an adenovirus shell containing DNA that encodes a SARS‑CoV‑2 protein.[100] The viral vector-based vaccines against COVID-19 are non-replicating, meaning that they do not make new virus particles, but rather produce only the antigen which elicits a systemic immune response.[100]
As of January 2021, authorized vaccines of this type are the British Oxford–AstraZeneca COVID-19 vaccine,
Convidecia and Johnson & Johnson's vaccines are both one-shot vaccines which offer less complicated logistics; and can be stored under ordinary refrigeration for several months.[107][108]
Sputnik V uses Ad26 for the first dose the same as Johnson & Johnson's vaccine and Ad5 for the 2nd dose the same as Convidecia with similar single dose effectiveness and full trial taking place on single dose effectiveness.
Inactivated virus vaccines
Inactivated vaccines consist of virus particles that have been grown in culture and then are killed using a method such as heat or formaldehyde to lose disease producing capacity, while still stimulating an immune response.[109]
As of January 2021, authorized vaccines of this type are the Chinese CoronaVac,[110][111][112] BBIBP-CorV
Subunit vaccines
Subunit vaccines present one or more antigens without introducing whole pathogen particles. The antigens involved are often protein subunits, but can be any molecule that is a fragment of the pathogen.[117]
As of January 2021, the only authorized vaccine of this type is the peptide vaccine EpiVacCorona.
Other types
Additional types of vaccines that are in clinical trials include multiple DNA plasmid vaccines,[122]
Scientists investigated whether existing vaccines for unrelated conditions could prime the immune system and lessen the severity of COVID‑19 infection.[131] There is experimental evidence that the BCG vaccine for tuberculosis has non-specific effects on the immune system, but no evidence that this vaccine is effective against COVID‑19.[132]
Efficacy

The effectiveness of a new vaccine is defined by its efficacy during clinical trials.[134] The efficacy is the risk of getting the disease by vaccinated participants in the trial compared with the risk of getting the disease by unvaccinated participants.[134] An efficacy of 0% means that the vaccine does not work (identical to placebo). An efficacy of 50% means that there are half as many cases of infection as in unvaccinated individuals.
It is not straightforward to compare the efficacies of the different vaccines because the trials were run with different populations, geographies, and variants of the virus.[135] In the case of COVID‑19, a vaccine efficacy of 67% may be enough to slow the pandemic, but this assumes that the vaccine confers sterilizing immunity, which is necessary to prevent transmission. Vaccine efficacy reflects disease prevention, a poor indicator of transmissibility of SARS‑CoV‑2 since asymptomatic people can be highly infectious.[136] The US Food and Drug Administration (FDA) and the European Medicines Agency (EMA) set a cutoff of 50% as the efficacy required to approve a COVID‑19 vaccine.[137][138] Aiming for a realistic population vaccination coverage rate of 75%, and depending on the actual basic reproduction number, the necessary effectiveness of a COVID-19 vaccine is expected to be at least 70% to prevent an epidemic and at least 80% to extinguish it without further measures, such as social distancing.[139]
In efficacy calculations, symptomatic COVID-19 is generally defined as having both a positive PCR test and at least one or two of a defined list of COVID-19 symptoms, although exact specifications varying between trials. The trial location also affects the reported efficacy because different countries have different prevalences of SARS-CoV-2 variants. Ranges below are 95% confidence intervals unless indicated otherwise, and all values are for all participants regardless of age. Efficacy against severe COVID-19 is the most important, since hospitalizations and deaths are a public health burden whose prevention is a priority.[140] Authorized and approved vaccines have shown the following efficacies:
| Vaccine | Efficacy by severity of COVID-19 | Trial location | Refs | ||
|---|---|---|---|---|---|
| Mild or moderate[A] | Severe without hospitalization or death[B] | Severe with hospitalization or death[C] | |||
| Moderna vaccine | 94% (89–97%)[D] | 100%[E] | 100%[E] | United States | [141] |
| Pfizer–BioNTech vaccine | 95% (90–98%) | Not reported | Not reported | Multinational | [142] |
| Sputnik V | 92% (86–95%) | 100% (94–100%) | 100% | Russia | [143] |
| Oxford–AstraZeneca vaccine | 81% (60–91%)[F] | 100% (97.5% CI, 72–100%) | 100% | Multinational | [144] |
| 76% (68–82%)[G] | 100% | 100% | United States | [145] | |
| Novavax vaccine | 89% (75–95%) | 100%[H] | 100%[H] | United Kingdom | [146][147] |
| 60% (20–80%) | 100%[H] | 100%[H] | South Africa | ||
| BBIBP-CorV | 79% | 100%[148] | 100%[148] | Multinational | [149][unreliable medical source?] |
| CoronaVac | 78% | 100% | 100% | Brazil | [150][151][152][unreliable medical source?] |
| Johnson & Johnson vaccine | 66% (55–75%)[I][J] | 85% (54–97%)[J] | 100%[J] | Multinational | [153] |
| 72% (58–82%)[I][J] | 86% (−9 to 100%)[J] | 100%[J] | United States | ||
| 68% (49–81%)[I][J] | 88% (8–100%)[J] | 100%[J] | Brazil | ||
| 64% (41–79%)[I][J] | 82% (46–95%)[J] | 100%[J] | South Africa | ||
| Covaxin | 81% | Not reported | Not reported | India | [154][155][unreliable medical source?] |
| Convidecia | 66% | 91% | Not reported | Multinational | [156][unreliable medical source?] |
- ^ Mild symptoms: fever, dry cough, fatigue, myalgia, arthralgia, sore throat, diarrhea, nausea, vomiting, headache, anosmia, ageusia, nasal congestion, rhinorrhea, conjunctivitis, skin rash, chills, dizziness. Moderate symptoms: mild pneumonia.
- ^ Severe symptoms without hospitalization or death for an individual, are any one of the following severe respiratory symptoms measured at rest on any time during the course of observation (on top of having either pneumonia, deep vein thrombosis, dyspnea, hypoxia, persistent chest pain, anorexia, confusion, fever above 38 °C (100 °F)), that however were not persistent/severe enough to cause hospitalization or death: Any respiratory rate ≥30 breaths/minute, heart rate ≥125 beats/minute, oxygen saturation (SpO2) ≤93% on room air at sea level, or partial pressure of oxygen/fraction of inspired oxygen (PaO2/FiO2) <300 mmHg.
- ^ Severe symptoms causing hospitalization or death, are those requiring treatment at hospitals or results in deaths: dyspnea, hypoxia, persistent chest pain, anorexia, confusion, fever above 38 °C (100 °F), respiratory failure, kidney failure, multiorgan dysfunction, sepsis, shock.
- ^ Mild/Moderate COVID-19 symptoms observed in the Moderna vaccine trials, were only counted as such for vaccinated individuals if they began more than 14 days after their second dose, and required presence of a positive RT-PCR test result along with at least two systemic symptoms (fever above 38ºC, chills, myalgia, headache, sore throat, new olfactory and taste disorder) or just one respiratory symptom (cough, shortness of breath or difficulty breathing, or clinical or radiographical evidence of pneumonia).
- ^ a b Severe COVID-19 symptoms observed in the Moderna vaccine trials, were defined as symptoms having met the criteria for mild/moderate symptoms plus any of the following observations: Clinical signs indicative of severe systemic illness, respiratory rate ≥30 per minute, heart rate ≥125 beats per minute, SpO2 ≤93% on room air at sea level or PaO2/FIO2 <300 mm Hg; or respiratory failure or ARDS, (defined as needing high-flow oxygen, non-invasive or mechanical ventilation, or ECMO), evidence of shock (systolic blood pressure <90 mmHg, diastolic BP <60 mmHg or requiring vasopressors); or significant acute renal, hepatic, or neurologic dysfunction; or admission to an intensive care unit or death. No severe cases were detected for vaccinated individuals in the trials, compared with 30 severe cases reported in the placebo group (incidence rate 9.1 per 1000 person-years).
- ^ With 12 weeks or more of interval between doses. For an interval of less than 6 weeks, the trial found an efficacy 55% (33–70%).
- ^ With a 4 week interval between doses. Efficacy is "at preventing symptomatic COVID-19."
- ^ a b c d No cases detected in trial.
- ^ a b c d Moderate cases.
- ^ a b c d e f g h i j k l Efficacy reported 28 days post-vaccination for the Johnson & Johnson single shot vaccine. A lower efficacy was found for the vaccinated individuals 14 days post-vaccination.
Real-world studies of vaccine effectiveness
The real-world studies of vaccine effectiveness, measure to which extend a certain vaccine have succeded preventing COVID-19 infection, symptoms, hospitalization and deaths for the vaccinated individuals in a large population.
- In Israel, among 715,425 individuals vaccinated by the Moderna/Pfizer vaccine during December 20 to January 28, it was observed for the period starting seven days after the second shot, that only 317 people (0.04%) became sick with mild/moderate Covid-19 symptoms and only 16 people (0.002%) were hospitalized.[157]
- Pfizer and Moderna Covid-19 vaccines provide highly effective protection, according to a report from the US Centers for Disease Control and Prevention. Under real-world conditions, mRNA vaccine effectiveness of full immunization (≥14 days after second dose) was 90% against SARS-CoV-2 infections regardless of symptom status; vaccine effectiveness of partial immunization (≥14 days after first dose but before second dose) was 80%.[158]
Variants
The emergence of a SARS-CoV-2 variant that is moderately or fully resistant to the antibody response elicited by the current generation of COVID-19 vaccines may require modification of the vaccines.[159] Trials indicate many vaccines developed for the initial strain have lower efficacy for some variants against symptomatic COVID-19.[160] As of February 2021, the US Food and Drug Administration believed that all FDA authorized vaccines remained effective in protecting against circulating strains of SARS-CoV-2.[159]
B.1.1.7 variant
In December 2020, a new SARS‑CoV‑2 variant, B.1.1.7, was identified in the UK.[161] Early results suggest protection to the UK variant from the Pfizer and Moderna vaccines.[162][163] One study indicated that the Oxford–AstraZeneca vaccine had an efficacy of 42–89% against the B.1.1.7 variant, versus 71–91% against non-B.1.1.7 variants.[164] Preliminary data from a clinical trial indicated that the Novavax vaccine was ~96% effective for symptoms against the original variant, ~86% against B.1.1.7, and ~60% against the "South African" B.1.351 variant.[165]
501.V2 variant
Moderna has launched a trial of a vaccine to tackle the South African 501.V2 variant (also known as B.1.351).[166] On 17 February 2021, Pfizer announced neutralization activity was reduced by two-thirds for the 501.V2 variant, while stating no claims about the efficacy of the vaccine in preventing illness for this variant could yet be made.[167] Decreased neutralizing activity of sera from patients vaccinated with Moderna and Pfizer vaccines against B.1.351 was latter confirmed by several studies.[163][168]
In January, Johnson & Johnson, which held trials for its Ad26.COV2.S vaccine in South Africa, reported the level of protection against moderate to severe COVID-19 infection was 72% in the United States and 57% in South Africa.[169]
On 6 February 2021, the Financial Times reported that provisional trial data from a study undertaken by South Africa's University of the Witwatersrand in conjunction with Oxford University demonstrated reduced efficacy of the Oxford–AstraZeneca COVID-19 vaccine against the 501.V2 variant.[170] The study found that in a sample size of 2,000 the AZD1222 vaccine afforded only "minimal protection" in all but the most severe cases of COVID-19.[171] On 7 February 2021, the Minister for Health for South Africa suspended the planned deployment of around 1 million doses of the vaccine whilst they examine the data and await advice on how to proceed.[172][173]
P1 variant
The P1 variant (also known as 20J/501Y.V3), initially identified in Brazil, seems to partially escape vaccination with the Pfizer/BioNtech vaccine.[168]
Trial and authorization status
Phase I trials test primarily for safety and preliminary dosing in a few dozen healthy subjects, while Phase II trials – following success in Phase I – evaluate immunogenicity, dose levels (efficacy based on biomarkers) and adverse effects of the candidate vaccine, typically in hundreds of people.[34][35] A Phase I–II trial consists of preliminary safety and immunogenicity testing, is typically randomized, placebo-controlled, while determining more precise, effective doses.[35] Phase III trials typically involve more participants at multiple sites, include a control group, and test effectiveness of the vaccine to prevent the disease (an "interventional" or "pivotal" trial), while monitoring for adverse effects at the optimal dose.[34][35] Definition of vaccine safety, efficacy, and clinical endpoints in a Phase III trial may vary between the trials of different companies, such as defining the degree of side effects, infection or amount of transmission, and whether the vaccine prevents moderate or severe COVID‑19 infection.[36][174][175]
A clinical trial design in progress may be modified as an "adaptive design" if accumulating data in the trial provide early insights about positive or negative efficacy of the treatment.[176][177] Adaptive designs within ongoing Phase II–III clinical trials on candidate vaccines may shorten trial durations and use fewer subjects, possibly expediting decisions for early termination or success, avoiding duplication of research efforts, and enhancing coordination of design changes for the Solidarity trial across its international locations.[176][178]
List of authorized and approved vaccines
National regulatory authorities have granted emergency use authorizations for twelve vaccines. Six of those have been approved for emergency or full use by at least one WHO-recognized stringent regulatory authorities.
|
|
| Vaccine, developers/sponsors | Country of origin | Type (technology) | Doses, interval | Storage temperature | Current phase (participants) | Authorization |
|---|---|---|---|---|---|---|
| Sputnik V COVID-19 vaccine (Gam-COVID-Vac) Gamaleya Research Institute of Epidemiology and Microbiology |
Russia | Adenovirus vector (recombinant Ad5 and Ad26) |
2 doses 3 weeks |
≤-18 °C (freezer) |
Phase III (40,000) Randomized double-blind, placebo-controlled to evaluate efficacy, immunogenicity, and safety.[182] Interim analysis from the trial was published in The Lancet, indicating 91.6% efficacy without unusual side effects.[143] Aug 2020 – May 2021, Russia, Belarus,[183] India,[184][185] Venezuela,[186][187] UAE[188] |
Template:CovidVacNum |
| Oxford–AstraZeneca COVID-19 vaccine (Vaxzevria, Covishield) University of Oxford, AstraZeneca, CEPI |
United Kingdom, Sweden | Adenovirus vector (ChAdOx1) |
2 doses 4–12 weeks |
2–8 °C |
Phase III (30,000) Interventional; randomized, placebo-controlled study for efficacy, safety, and immunogenicity.[195] Overall efficacy of 76% after the first dose and 81% after a second dose taken 12 weeks or more after the first.[144] May 2020 – Aug 2021, Brazil (5,000),[196] United Kingdom, India[197] |
Template:CovidVacNum |
| Pfizer–BioNTech COVID-19 vaccine (Comirnaty) BioNTech, Pfizer |
United States, Germany | RNA (modRNA in lipid nanoparticles) |
2 doses 3–4 weeks |
-70±10 °C (ULT) |
Phase III (43,448) Randomized, placebo-controlled. Positive results from an interim analysis were announced on 18 November 2020[203] and published on 10 December 2020 reporting an overall efficacy of 95%.[204][205] Jul – Nov 2020,[206][134] Germany, United States |
Template:CovidVacNum |
| BBIBP-CorV Sinopharm: Beijing Institute of Biological Products, Wuhan Institute of Biological Products |
China | Inactivated SARS‑CoV‑2 (vero cells) |
2 doses 3–4 weeks |
2–8 °C |
Phase III (48,000) Randomized, double-blind, parallel placebo-controlled, to evaluate safety and protective efficacy. Sinopharm's internal analysis indicated a 79% efficacy.[209] Jul 2020 – Jul 2021, United Arab Emirates, Bahrain, Jordan,[210] Argentina,[211] Morocco,[212] Peru[213] |
Template:CovidVacNum |
| CoronaVac[110][111][112] Sinovac |
China | Inactivated SARS‑CoV‑2 (vero cells) |
2 doses 2 weeks |
2–8 °C |
Phase III (33,620) Double-blind, randomized, placebo-controlled to evaluate efficacy and safety. Final Phase III results from Turkey showed an efficacy of 83.5%.[216] Additional results were announced by Indonesia with an efficacy of 65.3%.[217] Brazil announced results showing 50.4% effective at preventing symptomatic infections, 78% effective in preventing mild cases, and 100% effective in preventing severe cases.[218] July 2020 – Oct 2021, Brazil (15,000);[219] Aug 2020 – January 2021, Indonesia (1,620); Chile (3,000);[220] Turkey (13,000)[221] |
Template:CovidVacNum |
| Moderna COVID-19 vaccine Moderna, NIAID, BARDA, CEPI |
United States | RNA (modRNA in lipid nanoparticles) |
2 doses 4 weeks |
-20±5 °C (freezer) |
Phase III (30,000) Interventional; randomized, placebo-controlled study for efficacy, safety, and immunogenicity. Positive results from an interim analysis were announced on 15 November 2020[225] and published on 30 December 2020 reporting an overall efficacy of 94%.[226] Jul 2020 – Oct 2022, United States |
Template:CovidVacNum |
| Johnson & Johnson COVID-19 vaccine[105][106] Janssen Vaccines (Johnson & Johnson), BIDMC |
United States, Netherlands | Adenovirus vector (recombinant Ad26) |
1 dose[228] | 2–8 °C[228] | Phase III (40,000) Randomized, double-blinded, placebo-controlled Positive results from an interim analysis were announced on 29 January 2021. J&J reports an efficacy of 66% against mild and moderate symptoms, and 85% against severe symptoms. Further, the mild and moderate efficacy ranged from 64% in South Africa to 72% in the United States.[229][153] Jul 2020 – 2023, United States, Argentina, Brazil, Chile, Colombia, Mexico, Peru, the Philippines, South Africa, Ukraine |
Template:CovidVacNum |
| Ad5-nCoV (Convidecia) CanSino Biologics, Beijing Institute of Biotechnology of the Academy of Military Medical Sciences |
China | Adenovirus vector (recombinant Ad5) |
1 dose[156] | 2–8 °C[156] | Phase III (40,000) Global multi-center, randomized, double-blind, placebo-controlled to evaluate efficacy, safety and immunogenicity. In February 2021, interim analysis from global trials showed an efficacy of 65.7% against moderate cases of COVID-19 and 90.98% efficacy against severe cases.[156] Mar–Dec 2020, China; Sep 2020 – Dec 2021, Pakistan; Sep – Nov 2020, Russia,[231] China, Argentina, Chile;[232] Mexico;[233] Pakistan;[234] Saudi Arabia[235][236] |
Template:CovidVacNum |
| BBV152 (Covaxin) Bharat Biotech, Indian Council of Medical Research |
India | Inactivated SARS‑CoV‑2 (vero cells) |
2 doses 4 weeks |
2–8 °C |
Phase III (25,800) Randomised, observer-blinded, placebo-controlled[239] The interim efficacy rate is 81% as per third phase trial.[240] All data from the animal, first, second phase trials have been made public through peer-reviewed journals.[241] Phase-3 trials had shown 81% efficacy.[242] Nov 2020 – Mar 2021, India. |
Template:CovidVacNum |
| EpiVacCorona Vector Institute |
Russia | Subunit (peptide) |
2 doses 3 weeks |
2–8 °C |
Phase III (40,000) Randomized double-blind, placebo-controlled to evaluate efficacy, immunogenicity, and safety Nov 2020 – Dec 2021, Russia[245] |
Template:CovidVacNum |
| ZF2001 (RBD-Dimer)[3] Anhui Zhifei Longcom Biopharmaceutical Co. Ltd. |
China | Subunit (recombinant) | 3 doses 30 days |
Phase III (29,000) Randomized, double-blind, placebo-controlled[246] Dec 2020 – Apr 2022, China, Ecuador, Indonesia, Malaysia, Pakistan, Uzbekistan[248][249] |
Template:CovidVacNum | |
| CoviVac[250] The Chumakov Centre at the Russian Academy of Sciences |
Russia | Inactivated SARS‑CoV‑2 |
2 doses 2 weeks |
2–8 °C |
Phase III (3,000) Double-blind, randomized, placebo-controlled to evaluate efficacy and safety. |
Template:CovidVacNum |
Vaccine candidates in human trials
| Vaccine candidates, developers, and sponsors |
Country of origin | Type (technology) | Current phase (participants) design |
Completed phase[f] (participants) Immune response |
Pending authorization | |
|---|---|---|---|---|---|---|
| Novavax COVID-19 vaccine (Covovax) Novavax, CEPI |
United States | Subunit[256][257][258]/virus-like particle[259][260] (SARS‑CoV‑2 recombinant spike protein nanoparticle with adjuvant) | Phase III (45,000) Randomised, observer-blinded, placebo-controlled trial[261] Sep 2020 – Jan 2021, UK (15,000); December 2020 – Mar 2021, US, Mexico, (30,000);[262] India[263] |
Phase I–II (131) IgG and neutralizing antibody response with adjuvant after booster dose.[264] |
||
| CureVac COVID-19 vaccine (CVnCoV) CureVac, CEPI |
Germany | RNA (unmodified RNA)[273] | Phase III (39,020) Phase 2b/3 (36,500): Multicenter efficacy and safety trial in adults. Phase 3 (2,520): Randomized, observer-blinded, placebo-controlled. Nov 2020 – Jun 2021, Argentina, Belgium, Colombia, Dominican Republic, France, Germany, Mexico, Netherlands, Panama, Peru, Spain |
Phase I–II (944) Phase I (284): Partially blind, controlled, dose-escalation to evaluate safety, reactogenicity and immunogenicity. Phase IIa (660):Partially observer-blind, multicenter, controlled, dose-confirmation. Jun 2020 – Oct 2021, Belgium (phase I), Germany (phase I), Panama (phase IIa), Peru (phase IIa) |
Emergency (1)
| |
| CIGB-66 (ABDALA) Center for Genetic Engineering and Biotechnology |
Cuba | Subunit | Phase III (48,000) Multicenter, randomized, double-blind, placebo-controlled. Mar – Jul 2021, Cuba |
Phase I–II (132) Randomized, double-blind, placebo-controlled, factorial. Nov 2020 – May 2021, Cuba |
||
| SOBERANA 02 (FINLAY-FR-2) Instituto Finlay de Vacunas |
Cuba | Conjugate | Phase III (44,010) Multicenter, adaptive, parallel-group, randomized, placebo-controlled, double-blind Mar – Nov 2021, Cuba |
Phase I–II (950) Phase I (40): Non-randomized controlled trial. Masking: Open. Control group: Uncontrolled. Study design: Adaptive, sequential Phase II (910): Randomized controlled trial. Masking: Double Blind. Control group: Placebo. Study design: Parallel. Nov 2020 – Mar 2021, Cuba |
Emergency (1)
| |
| Sanofi–GSK COVID-19 vaccine (VAT00002) Sanofi Pasteur, GSK |
France, United Kingdom | Subunit | Phase III (34,520) Efficacy, Immunogenicity, and Safety of SARS-CoV-2 Recombinant Protein Vaccine with Adjuvant in Adults 18 Years of Age and Older. Dec 2020 – Apr 2022, Kenya |
Phase I–II (1,160) Phase I-IIa (440): Immunogenicity and Safety of SARS-CoV-2 Recombinant Protein Vaccine Formulations (With or Without Adjuvant) in Healthy Adults 18 Years of Age and Older.[286] Phase IIb (720): Immunogenicity and Safety of SARS-CoV-2 Recombinant Protein Vaccine With AS03 Adjuvant in Adults 18 Years of Age and Older.[287] Sep 2020 – Sep 2022, United States |
||
| Unnamed Chinese Academy of Medical Sciences |
China | Inactivated SARS‑CoV‑2 | Phase III (34,020) Randomized, double-blinded, single-center, placebo-controlled Jan – Sep 2021, Brazil, Malaysia |
Phase I–II (942) Randomized, double-blinded, single-center, placebo-controlled May – Sep 2020, Chengdu |
||
| QazCovid-in[294] Research Institute for Biological Safety Problems |
Kazakhstan | Inactivated SARS‑CoV‑2 | Phase III (3,000) Randomised, blind, placebo-controlled trial[295] Dec 2020 – Mar 2021, Kazakhstan [295] |
Phase I–II (244[296]) Sep – Nov 2020, Kazakhstan |
||
| ZyCoV-D Cadila Healthcare |
India | DNA (plasmid expressing SARS‑CoV‑2 S protein) | Phase III (26,000) Randomised, blind, placebo-controlled trial[298] Jan 2021 – ?, India[299] |
Phase I–II (1,000) Interventional; randomized, double-blind, placebo-controlled[300][298] Jul 2020 – Jan 2021, India |
||
| CoVLP[301] Medicago, GSK |
Canada, United Kingdom | Virus-like particles[g] (recombinant, plant-based with AS03) | Phase II–III (30,918) Event-driven, randomized, observer blinded, placebo-controlled[303] Nov 2020 – Dec 2021, Canada |
Phase I (180) Neutralizing antibodies at day 42 after the first injection (day 21 after the second injection) were at levels 10x that of COVID-19 survivors. Jul 2020 – Sept 2021, Canada[304] |
Emergency (1)
| |
| SCB-2019 Clover Biopharmaceuticals,[308][309] GSK, CEPI |
China, United Kingdom | Subunit (Spike protein trimeric subunit with AS03) | Phase II–III (22,000) Randomized, double-blind, controlled Mar 2021 – Jul 2022, Belgium, Brazil, Colombia, Dominican Republic, Germany, Nepal, Panama, the Philippines, Poland, South Africa |
Phase I (150) Jun – Oct 2020, Perth |
||
| COVIran Barakat[310] Barakat Pharmaceutical Group, Shifa Pharmed Industrial Group |
Iran | Inactivated SARS‑CoV‑2 | Phase II–III (20,000) Randomized, double-blind, parallel arms, placebo-controlled.[311] Mar – May 2021, Iran |
Phase I (56) Randomized, double-blind, parallel arms, placebo-control.[312] Dec 2020 – Feb 2021, Iran |
||
| UB-612 United Biomedical,Inc, COVAXX, DASA |
Brazil, United States | Subunit | Phase II–III (11,170) Phase IIa (3,850): Placebo-controlled, Randomized, Observer-blind Study. Phase IIb-III (7,320): Randomized, Multicenter, Double-Blind, Placebo Controlled, Dose-Response. Jan 2021–Mar 2023, Taiwan |
Phase I (60) Open-label study Sep 2020–Jan 2021, Taiwan |
||
| GRAd-COV2 ReiThera, Lazzaro Spallanzani National Institute for Infectious Diseases |
Italy | Adenovirus vector (modified chimpanzee adenovirus vector, GRAd) | Phase II–III (10,300) Randomized, stratified, observer-blind, placebo-controlled. Mar–May 2021, Italy |
Phase I (90) Subjects (two groups: 18–55 and 65–85 years old) randomly receiving one of three escalating doses of GRAd-COV2 or a placebo, then monitored over a 24-week period. 93% of subjects who received GRAd-COV2 developed anti-bodies. Aug–Dec 2020, Rome |
||
| Unnamed Jiangsu Province Centers for Disease Control and Prevention, West China Hospital |
China | Subunit (recombinant with Sf9 cell) | Phase II (4,960) Phase IIa (960):Single-center, Randomized, Double-Blinded, Placebo-Controlled. Phase IIb (4,000):Single-center, Randomized, Double-Blinded, Placebo-Controlled. Nov 2020 – May 2021, China |
Phase I (45) Single-center, Randomized, Placebo-controlled, Double-blind. Aug –Oct 2020, China |
||
| MVC-COV1901 Medigen Vaccine Biologics |
Taiwan | Subunit (recombinant) | Phase II (3,700) Prospective, double-blinded, multi-center, multi-regional Dec 2020 – Jun 2021, Taiwan, Vietnam |
Phase I (45) Prospective, open-labeled, single-center Oct 2020–Jan 2021, Taiwan |
||
| Unnamed Minhai Biotechnology Co. |
China | Inactivated SARS‑CoV‑2 (vero cell) | Phase II (1,000) Randomized, double-blind, placebo parallel-controlled. Oct 2020 – Jun 2021, China |
Phase I (180) Randomized, double-blind, placebo parallel-controlled. Oct 2020 – Jun 2021, China |
||
| DelNS1-2019-nCoV-RBD-OPT Beijing Wantai Biological Pharmacy |
China | Viral vector | Phase II (720) Nov 2020 – Dec 2021, China |
Phase I (60) Sep 2020 – Oct 2021, China |
||
| Nanocovax[330] Nanogen Pharmaceutical Biotechnology JSC |
Vietnam | Subunit (SARS‑CoV‑2 recombinant spike protein with aluminum adjuvant)[331][332] | Phase II (560) Randomization, double-blind, multicenter, placebo-controlled Feb – May 2021, Vietnam |
Phase I (60) Open label, dose escalation Dec 2020 – Jan 2021, Vietnam |
||
| Unnamed PLA Academy of Military Science, Walvax Biotech[335] |
China | RNA | Phase II (420) Jan 2021 – Mar 2022, China[336] |
Phase I (168) Jun 2020 – Dec 2021, China |
||
| INO-4800[123][124] Inovio, CEPI, Korea National Institute of Health, International Vaccine Institute |
South Korea, United States | DNA vaccine (plasmid delivered by electroporation) | Phase II–III (1,041) Phase II/III (401): Randomized, placebo-controlled, multi-center.[337] Phase IIa (640): Randomized, double-blinded, placebo-controlled, dose-finding.[338] Nov 2020 – Sep 2022, United States (phase II/III) |
Phase I–II (280) Phase Ia (120): Open-label trial. Phase Ib-IIa (160): Dose-Ranging Trial.[339] April 2020 – Feb 2022, United States, South Korea (phase Ib-IIa) |
||
| AG0302-COVID‑19 AnGes Inc.,[341] AMED |
Japan | DNA vaccine (plasmid) | Phase II–III (500) Randomized, double-blind, placebo controlled[342] Nov 2020 – May 2021, Japan |
Phase I–II (30) Randomized/non-randomized, single-center, two doses Jun – Nov 2020, Osaka |
||
| IIBR-100 (Brilife) The Israel Institute for Biological Research |
Israel | Vesicular stomatitis vector (recombinant) | Phase I–II (1,040) Oct 2020 – May 2021, Israel |
Preclinical |
||
| ARCT-021 (Lunar-COV19)[344][345] Arcturus Therapeutics, Duke–NUS Medical School |
United States, Singapore | RNA | Phase I–II (798) Phase I/II (92): Randomized, double-blinded, placebo controlled Phase IIa (106): Open label extension[346] Phase IIb (600): Randomized, observer-blind, placebo-controlled[347] Aug 2020 – Apr 2022, Singapore, United States (phase IIb) |
Preclinical |
||
| VBI-2902 Variation Biotechnologies |
United States | Virus-like particle | Phase I–II (780) Randomized, observer-blind, dose-escalation, placebo-controlled Mar 2021 – Jun 2022, Canada |
Preclinical |
||
| NDV-HXP-S Mahidol University |
Thailand | Viral vector | Phase I–II (460) Randomized, placebo-controlled, observer-blind. Mar 2021 – Apr 2022, Thailand |
Preclinical |
||
| MRT5500[350] Sanofi Pasteur and Translate Bio |
France, United States | RNA | Phase I–II (415) Immunogenicity and Safety of the First-in-Human SARS-CoV-2 mRNA Vaccine Formulation in Healthy Adults 18 Years of Age and Older. Mar 2021 – May 2022, United States |
Preclinical |
||
| EuCorVac-19 EuBiologics Co |
South Korea | Subunit | Phase I–II (280) Dose-exploration, randomized, observer-blind, placebo-controlled Feb 2021 – Mar 2022, South Korea |
Preclinical |
||
| RBD SARS-CoV-2 HBsAg VLP SpyBiotech |
United Kingdom | Virus-like particle | Phase I–II (280) Randomized, placebo-controlled, multi-center. Aug 2020 – 2021, Australia |
Preclinical |
||
| GX-19 (GX-19N) Genexine consortium,[355] International Vaccine Institute |
South Korea | DNA vaccine | Phase I–II (380) Phase I-II (170-210): Multi-center, randomized, double-blind, placebo-controlled Jun 2020 – Mar 2021, Seoul |
Preclinical |
||
| AV-COVID-19 AIVITA Biomedical, Inc., Ministry of Health (Indonesia) |
United States, Indonesia | Viral vector | Phase I–II (202) Adaptive. Dec 2020 – Jul 2021, Indonesia (phase I), United States (phase I/II) |
Preclinical |
||
| VLA2001[115][116] Valneva |
France | Inactivated SARS‑CoV‑2 | Phase I–II (150) Randomized, multi-center, double-blinded Dec 2020 – Feb 2021, United Kingdom |
Preclinical |
||
| TAK-919[358] Takeda |
Japan | RNA | Phase I–II (200) Randomized, observer-blind, placebo-controlled Jan 2021 – Mar 2022, Japan |
Preclinical |
||
| TAK-019[360] Takeda |
Japan | Subunit | Phase I–II (200) Randomized, observer-blind, placebo-controlled. Feb 2021 – April 2022, Japan |
Preclinical |
||
| COVID-eVax Takis Biotech |
Italy | DNA | Phase I–II (160) Phase I:First-in-human, dose escalation. Phase II: Open-label, randomize, dose expansion. Feb – Sep 2021, Italy |
Preclinical |
||
| ChulaCov19 Chulalongkorn University |
Thailand | RNA | Phase I–II (96) Dose-finding Study. Jan – Mar 2021, Thailand |
Preclinical |
||
| COVID‑19/aAPC Shenzhen Genoimmune Medical Institute[364] |
China | Lentiviral vector (with minigene modifying aAPCs) | Phase I (100) Mar 2020 – 2023, Shenzhen |
Preclinical |
||
| LV-SMENP-DC Shenzhen Genoimmune Medical Institute[364] |
China | Lentiviral vector (with minigene modifying DCs) | Phase I (100) Mar 2020 – 2023, Shenzhen |
Preclinical |
||
| ImmunityBio COVID-19 vaccine (hAd5) ImmunityBio |
United States | Viral vector | Phase I (160) Open-Label. Oct 2020 – Apr 2022, South Africa, United States |
Preclinical |
||
| COVAX-19 Vaxine Pty Ltd[369] |
Australia | Subunit (recombinant protein) | Phase I (40) Jun 2020 – Jul 2021, Adelaide |
Preclinical |
||
| HGC019 Gennova Biopharmaceuticals, HDT Biotech Corporation[371] |
India, United States | RNA | Phase I (120) Jan 2021 – ?, India |
Preclinical |
||
| Bio E COVID-19 (BECOV2D) Biological E. Limited, Baylor College of Medicine,[375] CEPI |
India, United States | Subunit (using an antigen) | Phase I–II (360) Randomized, Parallel Group Trial Nov 2020 – Feb 2021, India |
Preclinical |
||
| Bangavax Globe Biotech Ltd. of Bangladesh |
Bangladesh | RNA | Phase I (100) Randomized, Parallel Group Trial Feb 2021 – Feb 2022,[380] Bangladesh |
Preclinical |
||
| PTX-COVID19-B[381] Providence Therapeutics |
Canada | RNA | Phase I (60) Jan – May 2021, Canada |
Preclinical |
||
| COVAC-2[382] VIDO (University of Saskatchewan) |
Canada | Subunit | Phase I (108) Feb 2021 – Jan 2022, Halifax |
Preclinical |
||
| COVI-VAC Codagenix Inc. |
United States | Attenuated | Phase I (48) First-in-human, randomised, double-blind, placebo-controlled, dose-escalation Dec 2020 – Jun 2021, United Kingdom |
Preclinical |
||
| CoV2 SAM (LNP) GSK |
United Kingdom | RNA | Phase I (48) Open-label, dose escalation, non-randomized Feb – Jun 2021, United States |
Preclinical |
||
| COVIGEN University of Sydney |
Australia | DNA | Phase I (150) Double-blind, dose-ranging, randomised, placebo-controlled. Feb 2021 – Jun 2022, Sydney |
Preclinical |
||
| BBV154 Bharat Biotech[387] |
India | Adenovirus vector (intranasal) | Phase I (175) Randomized, double-blinded, multicenter. Mar 2021, India |
Preclinical |
||
| MV-014-212[388] Meissa Vaccine Inc. |
United States | Attenuated | Phase I (130) Randomized, double-blinded, multicenter. Mar 2021 – Oct 2022, United States |
Preclinical |
||
| S-268019 Shionogi |
Japan | Subunit | Phase I–II (214) Randomized, double-blind, placebo-controlled, parallel-group. Dec 2020 – Jun 2022, Japan |
Preclinical |
||
| GBP510 SK Bioscience Co. Ltd. |
South Korea | Subunit | Phase I–II (260) Placebo-controlled, randomized, observer-blinded, dose-finding. Jan – Aug 2021, South Korea |
Preclinical |
||
| KBP-201 Kentucky Bioprocessing |
United States | Subunit | Phase I–II (180) First-in-human, observer-blinded, randomized, placebo-controlled, parallel group Dec 2020 – May 2021, United States |
Preclinical |
||
| AdimrSC-2f Adimmune Corporation |
Taiwan | Subunit | Phase I (70) Randomized, single center, open-label, dose-finding. Aug – Nov 2020, Taiwan |
Preclinical |
||
| ERUCOV-VAC Health Institutes of Turkey |
Turkey | Inactivated SARS‑CoV‑2 | Phase I (44) Study for the Determination of Safety and Immunogenicity of Two Different Strengths of the Inactivated COVID-19 Vaccine ERUCOV-VAC, Given Twice Intramuscularly to Healthy Volunteers, in a Placebo Controlled Study Design. Nov 2020 – Mar 2021, Turkey |
Preclinical |
||
| AKS-452 University Medical Center Groningen |
Netherlands | Subunit | Phase I–II (130) Non-randomized, Single-center, open-label, combinatorial. Jan – Apr 2021, Netherlands |
Preclinical |
||
| GLS-5310 GeneOne Life Science Inc. |
South Korea | DNA | Phase I–II (345) Multicenter, Randomized, Combined Phase I Dose-escalation and Phase IIa Double-blind. Dec 2020 – Jul 2022, South Korea |
Preclinical |
||
| Covigenix VAX-001 Entos Pharmaceuticals Inc. |
Canada | DNA | Phase I–II (72) Placebo-controlled, randomized, observer-blind, dose ranging adaptive. Mar – Aug 2021, Canada |
Preclinical |
||
| COH04S1 City of Hope Medical Center |
United States | Viral vector | Phase I (129) Dose Escalation Study. Dec 2020 – Nov 2022, California |
Preclinical |
||
| FAKHRAVAC (MIVAC) Organization of Defensive Innovation and Research |
Iran | Inactivated SARS‑CoV‑2 | Phase I (135) Randomized, double blind, controlled trial with factorial design. Mar – Apr 2021, Iran |
Preclinical |
||
| NBP2001 SK Bioscience Co. Ltd. |
South Korea | DNA | Phase I (50) Placebo-controlled, Randomized, Observer-blinded, Dose-escalation. Dec 2020 – Apr 2021, South Korea |
Preclinical |
||
| CoVac-1 University Hospital Tuebingen |
Germany | Subunit | Phase I (36) Placebo-controlled, Randomized, Observer-blinded, Dose-escalation. Nov 2020 – Sep 2021, Germany |
Preclinical |
||
| bacTRL-Spike Symvivo |
Canada | DNA | Phase I (24) Randomized, observer-blind, placebo-controlled. Nov 2020 – Feb 2022, Australia |
Preclinical |
||
| Razi Cov Pars Razi Vaccine and Serum Research Institute |
Iran | Subunit | Phase I (133) Randomized, double blind, placebo controlled. Jan – Mar 2021, Iran |
Preclinical |
||
| CORVax12 Providence Health & Services |
United States | DNA | Phase I (36) Open-label. Dec 2020 – May 2021, United States |
Preclinical |
||
| ChAdV68-S NIAID, Gritstone Oncology |
United States | Viral vector | Phase I (130) Open-label, dose and age escalation, parallel design. Mar 2021 – Sep 2022, United States |
Preclinical |
||
| AdCOVID Altimmune Inc. |
United States | Viral vector | Phase I (180) Double-blind, randomized, placebo-controlled, first-in-Human. Feb 2021 – Feb 2022, United States |
Preclinical |
||
| VXA-CoV2-1 Vaxart |
United States | Viral vector | Phase I (35) Double-blind, randomized, placebo-controlled, first-in-Human. Sep – Dec 2020, United States |
Preclinical |
||
| AdCLD-CoV19 Cellid Co |
South Korea | Viral vector | Phase I (150) Phase I: Dose Escalation, Single Center, Open. Phase IIa: Multicenter, Randomized, Open. Dec 2020 – Mar 2021, South Korea |
Preclinical |
||
| SpFN COVID-19 Vaccine United States Army Medical Research and Development Command |
United States | Subunit | Phase I (72) Randomized, double-blind, placebo-controlled. Apr 2021 – Oct 2022, United States |
Preclinical |
||
| MVA-SARS-2-S University Medical Center Hamburg-Eppendorf |
Germany | Viral vector | Phase I (30) Open, Single-center. Oct 2020 – May 2021, Germany |
Preclinical |
||
| LNP-nCoVsaRNA MRC clinical trials unit at Imperial College London |
United Kingdom | RNA | Terminated (105) Randomized trial, with dose escalation study (15) and expanded safety study (at least 200) Jun 2020 – Jul 2021, United Kingdom |
? |
||
| COVID-19-101 Institut Pasteur |
France | Viral vector | Terminated (90) Randomized, Placebo-controlled. Aug – Nov 2020, Belgium, France |
? |
||
| SARS-CoV-2 Sclamp/V451 UQ, Syneos Health, CEPI, Seqirus |
Australia | Subunit (molecular clamp stabilized spike protein with MF59) | Terminated (120) Randomised, double-blind, placebo-controlled, dose-ranging. False positive HIV test found among participants. Jul–Oct 2020, Brisbane |
? |
||
| V590[413] and V591/MV-SARS-CoV-2[414] Merck & Co. (Themis BIOscience), Institut Pasteur, University of Pittsburgh's Center for Vaccine Research (CVR), CEPI | United States, France | Vesicular stomatitis virus vector[415] / Measles virus vector[416] | Terminated In phase I, immune responses were inferior to those seen following natural infection and those reported for other SARS-CoV-2/COVID-19 vaccines.[417] |
- ^ Storage temperature for the frozen Gam-COVID-Vac formulation. The lyophilised Gam-COVID-Vac-Lyo formulation can be stored at 2-8°C.[181]
- ^ Serum Institute of India will be producing the ChAdOx1 nCoV-19 vaccine for India[190] and other low- and middle-income countries.[191]
- ^ Oxford name: ChAdOx1 nCoV-19. Manufacturing in Brazil to be carried out by Oswaldo Cruz Foundation.[192]
- ^ a b Recommended interval. The second dose of the Pfizer–BioNTech and Moderna vaccines can be administered up to 6 weeks after the first dose to alleviate a shortage of supplies.[199][200]
- ^ Long-term storage temperature. The Pfizer–BioNTech COVID-19 vaccine can be kept between −25 and −15 °C (−13 and 5 °F) for up to two weeks before use, and between 2 and 8 °C (36 and 46 °F) for up to five days before use.[201][202]
- ^ Latest Phase with published results.
- ^ Virus-like particles grown in Nicotiana benthamiana[302]
- ^ Phase I–IIa in South Korea in parallel with Phase II–III in the US
Formulation
As of September 2020[update], eleven of the vaccine candidates in clinical development use adjuvants to enhance immunogenicity.[23] An immunological adjuvant is a substance formulated with a vaccine to elevate the immune response to an antigen, such as the COVID‑19 virus or influenza virus.[418] Specifically, an adjuvant may be used in formulating a COVID‑19 vaccine candidate to boost its immunogenicity and efficacy to reduce or prevent COVID‑19 infection in vaccinated individuals.[418][419] Adjuvants used in COVID‑19 vaccine formulation may be particularly effective for technologies using the inactivated COVID‑19 virus and recombinant protein-based or vector-based vaccines.[419] Aluminum salts, known as "alum", were the first adjuvant used for licensed vaccines, and are the adjuvant of choice in some 80% of adjuvanted vaccines.[419] The alum adjuvant initiates diverse molecular and cellular mechanisms to enhance immunogenicity, including release of proinflammatory cytokines.[418][419]
Deployment
| Location | Vaccinated[a] | Percent[b] | |
|---|---|---|---|
| World[c][d] | 5,645,247,500 | 70.70% | |
| China[e] | 1,318,026,800 | 92.48% | |
| India | 1,027,438,900 | 72.08% | |
| European Union[f] | 338,481,060 | 75.43% | |
| United States[g] | 270,227,170 | 79.12% | |
| Indonesia | 204,419,400 | 73.31% | |
| Brazil | 189,643,420 | 90.17% | |
| Pakistan | 165,567,890 | 67.94% | |
| Bangladesh | 151,507,170 | 89.45% | |
| Japan | 104,740,060 | 83.79% | |
| Mexico | 97,179,496 | 75.56% | |
| Nigeria | 93,829,430 | 42.05% | |
| Vietnam | 90,497,670 | 90.79% | |
| Russia | 89,081,600 | 61.19% | |
| Philippines | 82,684,776 | 72.55% | |
| Iran | 65,199,830 | 72.83% | |
| Germany | 64,876,300 | 77.15% | |
| Turkey | 57,941,052 | 66.55% | |
| Thailand | 57,005,496 | 79.47% | |
| Egypt | 56,907,320 | 50.53% | |
| France | 54,677,680 | 82.50% | |
| United Kingdom | 53,806,964 | 78.92% | |
| Ethiopia | 52,489,510 | 41.86% | |
| Italy[h] | 50,936,720 | 85.44% | |
| South Korea | 44,764,956 | 86.45% | |
| Colombia | 43,012,176 | 83.13% | |
| Myanmar | 41,551,930 | 77.30% | |
| Argentina | 41,529,056 | 91.46% | |
| Spain | 41,351,230 | 86.46% | |
| Canada | 34,742,936 | 89.49% | |
| Tanzania | 34,434,932 | 53.21% | |
| Peru | 30,563,708 | 91.30% | |
| Malaysia | 28,138,564 | 81.10% | |
| Nepal | 27,883,196 | 93.83% | |
| Saudi Arabia | 27,041,364 | 84.04% | |
| Morocco | 25,020,168 | 67.03% | |
| South Africa | 24,210,952 | 38.81% | |
| Poland | 22,984,544 | 59.88% | |
| Mozambique | 22,869,646 | 70.03% | |
| Australia | 22,231,734 | 84.85% | |
| Venezuela | 22,157,232 | 78.54% | |
| Uzbekistan | 22,094,470 | 63.24% | |
| Taiwan | 21,899,240 | 93.51% | |
| Uganda | 20,033,188 | 42.34% | |
| Afghanistan | 19,151,368 | 47.20% | |
| Chile | 18,088,516 | 92.51% | |
| Sri Lanka | 17,143,760 | 75.08% | |
| Democratic Republic of the Congo | 17,045,720 | 16.65% | |
| Angola | 16,550,642 | 46.44% | |
| Ukraine | 16,267,198 | 39.63% | |
| Ecuador | 15,345,791 | 86.10% | |
| Cambodia | 15,316,670 | 89.04% | |
| Sudan | 15,207,452 | 30.79% | |
| Kenya | 14,494,372 | 26.72% | |
| Ghana | 13,864,186 | 41.82% | |
| Ivory Coast | 13,568,372 | 44.64% | |
| Netherlands | 12,582,081 | 70.27% | |
| Zambia | 11,711,565 | 58.11% | |
| Iraq | 11,332,925 | 25.72% | |
| Rwanda | 10,884,714 | 79.74% | |
| Kazakhstan | 10,858,101 | 54.20% | |
| Cuba | 10,805,570 | 97.70% | |
| United Arab Emirates | 9,991,089 | 97.55% | |
| Portugal | 9,821,414 | 94.28% | |
| Belgium | 9,261,641 | 79.55% | |
| Somalia | 8,972,167 | 50.40% | |
| Guatemala | 8,937,923 | 50.08% | |
| Tunisia | 8,896,848 | 73.41% | |
| Guinea | 8,715,641 | 62.01% | |
| Greece | 7,938,031 | 76.24% | |
| Algeria | 7,840,131 | 17.24% | |
| Sweden | 7,775,726 | 74.14% | |
| Zimbabwe | 7,525,882 | 46.83% | |
| Dominican Republic | 7,367,193 | 65.60% | |
| Bolivia | 7,361,008 | 60.95% | |
| Israel | 7,055,466 | 77.51% | |
| Czech Republic | 6,982,006 | 65.42% | |
| Hong Kong | 6,920,057 | 92.69% | |
| Austria | 6,899,873 | 76.12% | |
| Honduras | 6,596,213 | 63.04% | |
| Belarus | 6,536,392 | 71.25% | |
| Hungary | 6,420,354 | 66.30% | |
| Nicaragua | 6,404,524 | 95.15% | |
| Niger | 6,248,483 | 24.69% | |
| Switzerland | 6,096,911 | 69.34% | |
| Burkina Faso | 6,089,089 | 27.05% | |
| Laos | 5,888,649 | 77.90% | |
| Sierra Leone | 5,676,123 | 68.58% | |
| Romania | 5,474,507 | 28.56% | |
| Malawi | 5,433,538 | 26.42% | |
| Azerbaijan | 5,373,253 | 52.19% | |
| Tajikistan | 5,328,277 | 52.33% | |
| Singapore | 5,287,005 | 93.58% | |
| Chad | 5,147,667 | 27.89% | |
| Jordan | 4,821,579 | 42.83% | |
| Denmark | 4,746,522 | 80.41% | |
| El Salvador | 4,659,970 | 74.20% | |
| Costa Rica | 4,650,636 | 91.52% | |
| Turkmenistan | 4,614,869 | 63.83% | |
| Finland | 4,524,288 | 81.24% | |
| Mali | 4,354,292 | 18.87% | |
| Norway | 4,346,995 | 79.66% | |
| South Sudan | 4,315,127 | 39.15% | |
| New Zealand | 4,302,330 | 83.84% | |
| Republic of Ireland | 4,112,237 | 80.47% | |
| Paraguay | 3,995,915 | 59.11% | |
| Liberia | 3,903,802 | 72.65% | |
| Cameroon | 3,753,733 | 13.58% | |
| Panama | 3,746,041 | 85.12% | |
| Benin | 3,697,190 | 26.87% | |
| Kuwait | 3,457,498 | 75.33% | |
| Serbia | 3,354,075 | 49.39% | |
| Syria | 3,295,630 | 14.67% | |
| Oman | 3,279,632 | 69.33% | |
| Uruguay | 3,010,464 | 88.78% | |
| Qatar | 2,852,178 | 98.61% | |
| Slovakia | 2,840,017 | 51.89% | |
| Lebanon | 2,740,227 | 47.70% | |
| Madagascar | 2,710,365 | 8.90% | |
| Senegal | 2,684,696 | 15.21% | |
| Central African Republic | 2,600,389 | 51.01% | |
| Croatia | 2,323,025 | 59.46% | |
| Libya | 2,316,327 | 32.07% | |
| Mongolia | 2,284,018 | 67.45% | |
| Togo | 2,255,579 | 24.81% | |
| Bulgaria | 2,155,863 | 31.58% | |
| Mauritania | 2,103,754 | 43.15% | |
| Palestine | 2,012,767 | 37.94% | |
| Lithuania | 1,958,299 | 69.52% | |
| Botswana | 1,951,054 | 79.96% | |
| Kyrgyzstan | 1,736,541 | 24.97% | |
| Georgia | 1,654,504 | 43.60% | |
| Albania | 1,349,255 | 47.72% | |
| Latvia | 1,346,184 | 71.57% | |
| Slovenia | 1,265,802 | 59.84% | |
| Bahrain | 1,241,174 | 80.94% | |
| Armenia | 1,150,915 | 39.95% | |
| Mauritius | 1,123,773 | 88.06% | |
| Moldova | 1,109,524 | 36.50% | |
| Yemen | 1,050,202 | 2.75% | |
| Lesotho | 1,014,073 | 44.36% | |
| Bosnia and Herzegovina | 943,394 | 29.44% | |
| Kosovo | 906,858 | 52.79% | |
| Timor-Leste | 886,838 | 64.77% | |
| Estonia | 870,202 | 64.46% | |
| Jamaica | 859,773 | 30.28% | |
| North Macedonia | 854,570 | 46.44% | |
| Trinidad and Tobago | 754,399 | 50.43% | |
| Guinea-Bissau | 747,057 | 35.48% | |
| Fiji | 712,025 | 77.44% | |
| Bhutan | 699,116 | 89.52% | |
| Republic of the Congo | 695,760 | 11.53% | |
| Macau | 679,703 | 96.50% | |
| Gambia | 674,314 | 25.58% | |
| Cyprus | 671,193 | 71.37% | |
| Namibia | 629,767 | 21.79% | |
| Eswatini | 526,050 | 43.16% | |
| Haiti | 521,396 | 4.53% | |
| Guyana | 497,550 | 60.56% | |
| Luxembourg | 481,957 | 73.77% | |
| Malta | 478,953 | 90.68% | |
| Brunei | 451,149 | 99.07% | |
| Comoros | 438,825 | 52.60% | |
| Djibouti | 421,573 | 37.07% | |
| Maldives | 399,308 | 76.19% | |
| Papua New Guinea | 382,020 | 3.74% | |
| Cabo Verde | 356,734 | 68.64% | |
| Solomon Islands | 343,821 | 44.02% | |
| Gabon | 311,244 | 12.80% | |
| Iceland | 309,770 | 81.44% | |
| Northern Cyprus | 301,673 | 78.80% | |
| Montenegro | 292,783 | 47.63% | |
| Equatorial Guinea | 270,109 | 14.98% | |
| Suriname | 267,820 | 42.98% | |
| Belize | 258,473 | 64.18% | |
| New Caledonia | 192,375 | 67.00% | |
| Samoa | 191,403 | 88.91% | |
| French Polynesia | 190,908 | 68.09% | |
| Vanuatu | 176,624 | 56.42% | |
| Bahamas | 174,810 | 43.97% | |
| Barbados | 163,853 | 58.04% | |
| Sao Tome and Principe | 140,256 | 61.97% | |
| Curaçao | 108,601 | 58.59% | |
| Kiribati | 100,900 | 77.33% | |
| Aruba | 90,546 | 84.00% | |
| Seychelles | 88,520 | 70.52% | |
| Tonga | 87,375 | 83.17% | |
| Jersey | 84,365 | 81.52% | |
| Isle of Man | 69,560 | 82.67% | |
| Antigua and Barbuda | 64,290 | 69.24% | |
| Cayman Islands | 62,113 | 86.74% | |
| Saint Lucia | 60,140 | 33.64% | |
| Andorra | 57,913 | 72.64% | |
| Guernsey | 54,223 | 85.06% | |
| Bermuda | 48,554 | 74.96% | |
| Grenada | 44,241 | 37.84% | |
| Gibraltar | 42,175 | 112.08% | |
| Faroe Islands | 41,715 | 77.19% | |
| Greenland | 41,227 | 73.60% | |
| Saint Vincent and the Grenadines | 37,532 | 36.77% | |
| Burundi | 36,909 | 0.28% | |
| Saint Kitts and Nevis | 33,794 | 72.32% | |
| Dominica | 32,995 | 49.36% | |
| Turks and Caicos Islands | 32,815 | 71.54% | |
| Sint Maarten | 29,788 | 70.65% | |
| Monaco | 28,875 | 74.14% | |
| Liechtenstein | 26,771 | 68.06% | |
| San Marino | 26,357 | 77.26% | |
| British Virgin Islands | 19,466 | 50.77% | |
| Caribbean Netherlands | 19,109 | 66.69% | |
| Cook Islands | 15,112 | 102.48% | |
| Nauru | 13,106 | 110.87% | |
| Anguilla | 10,858 | 76.45% | |
| Tuvalu | 9,763 | 97.51% | |
| Wallis and Futuna | 7,150 | 62.17% | |
| Saint Helena, Ascension and Tristan da Cunha | 4,361 | 81.23% | |
| Falkland Islands | 2,632 | 74.88% | |
| Tokelau | 2,203 | 95.29% | |
| Montserrat | 2,104 | 47.01% | |
| Niue | 1,638 | 88.83% | |
| Pitcairn Islands | 47 | 100.00% | |
| North Korea | 0 | 0.00% | |
| |||
As of 12 August 2024[update], 13.53 billion COVID-19 vaccine doses have been administered worldwide, with 70.6 percent of the global population having received at least one dose.[421][422] While 4.19 million vaccines were then being administered daily, only 22.3 percent of people in low-income countries had received at least a first vaccine by September 2022, according to official reports from national health agencies, which are collated by Our World in Data.[423]
During a pandemic on the rapid timeline and scale of COVID-19 cases in 2020, international organizations like the World Health Organization (WHO) and Coalition for Epidemic Preparedness Innovations (CEPI), vaccine developers, governments, and industry evaluated the distribution of the eventual vaccine(s).[424] Individual countries producing a vaccine may be persuaded to favor the highest bidder for manufacturing or provide first-class service to their own country.[425][426][427] Experts emphasize that licensed vaccines should be available and affordable for people at the frontlines of healthcare and in most need.[425][427]
In April 2020, it was reported that the UK agreed to work with 20 other countries and global organizations, including France, Germany, and Italy, to find a vaccine and share the results, and that UK citizens would not get preferential access to any new COVID‑19 vaccines developed by taxpayer-funded UK universities.[428] Several companies planned to initially manufacture a vaccine at artificially low prices, then increase prices for profitability later if annual vaccinations are needed and as countries build stock for future needs.[427]
The WHO had set out the target to vaccinate 40% of the population of all countries by the end of 2021 and 70% by mid-2022,[429] but many countries missed the 40% target at the end of 2021.[430][431]Liability
The examples and perspective in this section may not represent a worldwide view of the subject. (December 2020) |
On 4 February 2020, US Secretary of Health and Human Services Alex Azar published a notice of declaration under the Public Readiness and Emergency Preparedness Act for medical countermeasures against COVID‑19, covering "any vaccine, used to treat, diagnose, cure, prevent, or mitigate COVID‑19, or the transmission of SARS-CoV-2 or a virus mutating therefrom", and stating that the declaration precludes "liability claims alleging negligence by a manufacturer in creating a vaccine, or negligence by a health care provider in prescribing the wrong dose, absent willful misconduct".[432] The declaration is effective in the United States through 1 October 2024.[432]
In the European Union, the COVID‑19 vaccines are licensed under a Conditional Marketing Authorisation which does not exempt manufacturers from civil and administrative liability claims.[433] While the purchasing contracts with vaccine manufacturers remain secret, they do not contain liability exemptions even for side-effects not known at the time of licensure.[434]
Pfizer has been criticised for demanding far-reaching liability waivers and other guarantees from countries such as Argentina and Brazil, which go beyond what was expected from other countries such as the US (above).[435][436]
Society and culture
Access
Nations pledged to buy doses of COVID-19 vaccine before the doses were available. Though high-income nations represent only 14% of the global population, as of 15 November 2020, they had contracted to buy 51% of all pre-sold doses. Some high-income nations bought more doses than would be necessary to vaccinate their entire populations.[437]
On 18 January 2021, WHO Director-General Tedros Adhanom Ghebreyesus warned of problems with equitable distribution: "More than 39 million doses of vaccine have now been administered in at least 49 higher-income countries. Just 25 doses have been given in one lowest-income country. Not 25 million; not 25 thousand; just 25."[438]
Some nations involved in long-standing territorial disputes have reportedly had their access to vaccines blocked by competing nations; Palestine has accused Israel blocking vaccine delivery to Gaza, while Taiwan has suggested that China has hampered its efforts to procure vaccine doses.[439][440][441]
A single dose of the COVID-19 vaccine by AstraZeneca would cost 47 Egyptian pounds (EGP) and the authorities are selling it between 100 and 200 EGP. A report by Carnegie Endowment for International Peace cited the current poverty rate in Egypt as around 29.7 percent, which constitutes approximately 30.5 million people, and claimed that about 15 million of the Egyptians would be unable to gain access to the luxury of vaccination. A human rights lawyer, Khaled Ali launched a lawsuit against the government, forcing them to provide vaccination free of cost to all members of the public.[442]
According to immunologist Dr. Anthony Fauci, mutant strains of virus and limited vaccine distribution pose continuing risks and he said: "we have to get the entire world vaccinated, not just our own country."[443] Edward Bergmark and Arick Wierson are calling for an global vaccination effort and wrote that the wealthier nations' "me-first" mentality could ultimately backfire, because the spread of the virus in poorer countries would lead to more variants, against which current vaccines could be less effective.[444]
On 10 March 2021, the United States, Britain, European Union nations and other WTO members, blocked a push by over 80 developing countries to waive COVID-19 vaccine patent rights in an effort to boost production of vaccines for poor nations.[445]
Misinformation
Vaccine hesitancy
Some 10% of the public perceives vaccines as unsafe or unnecessary, refusing vaccination – a global health threat called vaccine hesitancy[446] – which increases the risk of further viral spread that could lead to COVID‑19 outbreaks.[37] As of May 2020, estimates from two surveys were that 67% or 80% of people in the U.S. would accept a new vaccination against COVID‑19, with wide disparity by education level, employment status, ethnicity, and geography.[447] As of March 2021, 19% of US adults claim to have been vaccinated and 50% of US adults plan to get vaccinated.[448][449]
In an effort to demonstrate the vaccine's safety, prominent politicians have received it on camera, with others pledging to do so.[450][451][452]
Encouragement by public figures and celebrities
Due to vaccine hesitancy caused by COVID vaccine conspiracy theories many public figures and celebrities have publicly declared and they have been vaccinated and encouraged people to have COVID vaccines, many documented themselves getting vaccinated.[453]
Politicians and heads of state
Several heads of state and government ministers have released photographs of their vaccinations, encouraging others to be vaccinated including Kyriakos Mitsotakis, Zdravko Marić, Olivier Véran, US President Joe Biden, Former US Presidents Barack Obama, George W. Bush and Bill Clinton, the Dalai Lama, all nine US Supreme Court Justices, Alexandria Ocasio-Cortez, Nancy Pelosi and Kamala Harris.[454][455][456]
Elizabeth II and Prince Phillip announced they had had the vaccine, breaking from protocol of keeping the British royal family's health private.[453] Pope Francis and ex Pope Benedict both announced they had been vaccinated.[453]
Musicians
Dolly Parton recorded herself getting vaccinated with the Moderna vaccine she helped fund, she encouraged people to get vaccinated and created a new version of her song "Jolene" called "Vaccine".[453] Patti Smith, Yo-Yo Ma, Carole King, Tony Bennett, Mavis Staples, Brian Wilson, Joel Grey, Loretta Lynn, Willie Nelson, and Paul Stanley have all released photographs of them being vaccinated and encouraged others to do so.[457] Grey stated "I got the vaccine because I want to be safe. We've lost so many people to COVID. I've lost a few friends. It's heartbreaking. Frightening."[454]
Actresses and actors
Amy Schumer, Rosario Dawson, Arsinio Hall, Danny Trejo, Mandy Patinkin, Magic Johnson, Samuel L. Jackson, Arnold Schwarzenegger, Buzz Aldrin, Sharon Stone, Kate Mulgrew, Jeff Goldblum, Jane Fonda, Anthony Hopkins, Bette Midler, Kim Catrell, Isabella Rosselini, Christie Brinkley, Cameran Eubanks, Hugh Bonneville, Alan Alda, David Harbour, Sean Penn, Johnathan Van Ness, Dan Rather, Al Roker, Amanda Kloots, Kareem Abdul Jabbar, Martha Stewart, Ian McKellen and Patrick Stewart have released photographs of themselves getting vaccinated and encouraging others to do the same.[453][458]
Stephen Fry was photographed being vaccinated, described it as a "wonderful moment, but you feel that it's not only helpful for your own health, but you know that you're likely to be less contagious if you yourself happen to carry it... It's a symbol of being part of society, part of the group that we all want to protect each other and get this thing over and done with."[453] Dame Judi Dench, Sir David Attenborough, Joan Collins have announced they have been vaccinated.[453]
Specific communities
Romesh Ranganathan, Meera Syal, Adil Ray, Sadiq Khan and others produced a video specifically encouraging ethnic minority communities in the UK to be vaccinated including addressing conspiracy theories stating 'there is no scientific evidence to suggest it will work differently on people from ethnic minorities and that it does not include pork or any material of fetal or animal origin'.[459]
Oprah Winfrey and Whoopi Goldberg have spoken about being vaccinated for COVID and encouraged black Americans to be vaccinated.[460][461] Stephanie Elam volunteered to be a trial volunteer stating "a large part of the reason why I wanted to volunteer for this COVID-19 vaccine research — more Black people and more people of color need to be part of these trials so more diverse populations can reap the benefits of this medical research."[454]
See also
References
- ^ Li YD, Chi WY, Su JH, Ferrall L, Hung CF, Wu TC (December 2020). "Coronavirus vaccine development: from SARS and MERS to COVID-19". Journal of Biomedical Science. 27 (1): 104. doi:10.1186/s12929-020-00695-2. PMC 7749790. PMID 33341119.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Padilla T (24 February 2021). "No one is safe unless everyone is safe". BusinessWorld. Retrieved 24 February 2021.
- ^ a b c d e f "COVID-19 vaccine development pipeline (Refresh URL to update)". Vaccine Centre, London School of Hygiene and Tropical Medicine. 1 March 2021. Retrieved 10 March 2021.
- ^ Beaumont P (18 November 2020). "Covid-19 vaccine: who are countries prioritising for first doses?". The Guardian. ISSN 0261-3077. Retrieved 26 December 2020.
- ^ "Coronavirus (COVID-19) Vaccinations – Statistics and Research". Our World in Data. Retrieved 7 February 2021.
- ^ "Which companies will likely produce the most COVID-19 vaccine in 2021?". Pharmaceutical Processing World. 5 February 2021. Retrieved 1 March 2021.
- ^ "China can hit 500-mln-dose annual capacity of CanSinoBIO COVID-19 vaccine this year". Yahoo! Sport. Retrieved 1 March 2021.
- ^ Mullard A (November 2020). "How COVID vaccines are being divvied up around the world". Nature. doi:10.1038/d41586-020-03370-6. PMID 33257891. S2CID 227246811.
- ^ So AD, Woo J (December 2020). "Reserving coronavirus disease 2019 vaccines for global access: cross sectional analysis". BMJ. 371: m4750. doi:10.1136/bmj.m4750. PMC 7735431. PMID 33323376.
- ^ a b c Gates B (30 April 2020). "The vaccine race explained: What you need to know about the COVID-19 vaccine". The Gates Notes. Archived from the original on 14 May 2020. Retrieved 2 May 2020.
- ^ Cavanagh D (December 2003). "Severe acute respiratory syndrome vaccine development: experiences of vaccination against avian infectious bronchitis coronavirus". Avian Pathology. 32 (6): 567–82. doi:10.1080/03079450310001621198. PMC 7154303. PMID 14676007.
- ^ Gao W, Tamin A, Soloff A, D'Aiuto L, Nwanegbo E, Robbins PD, et al. (December 2003). "Effects of a SARS-associated coronavirus vaccine in monkeys". Lancet. 362 (9399): 1895–6. doi:10.1016/S0140-6736(03)14962-8. PMC 7112457. PMID 14667748.
- ^ Kim E, Okada K, Kenniston T, Raj VS, AlHajri MM, Farag EA, et al. (October 2014). "Immunogenicity of an adenoviral-based Middle East Respiratory Syndrome coronavirus vaccine in BALB/c mice". Vaccine. 32 (45): 5975–82. doi:10.1016/j.vaccine.2014.08.058. PMC 7115510. PMID 25192975.
- ^ Greenough TC, Babcock GJ, Roberts A, Hernandez HJ, Thomas WD, Coccia JA, et al. (February 2005). "Development and characterization of a severe acute respiratory syndrome-associated coronavirus-neutralizing human monoclonal antibody that provides effective immunoprophylaxis in mice". The Journal of Infectious Diseases. 191 (4): 507–14. doi:10.1086/427242. PMC 7110081. PMID 15655773.
- ^ Tripp RA, Haynes LM, Moore D, Anderson B, Tamin A, Harcourt BH, et al. (September 2005). "Monoclonal antibodies to SARS-associated coronavirus (SARS-CoV): identification of neutralizing and antibodies reactive to S, N, M and E viral proteins". Journal of Virological Methods. 128 (1–2): 21–8. doi:10.1016/j.jviromet.2005.03.021. PMC 7112802. PMID 15885812.
- ^ Roberts A, Thomas WD, Guarner J, Lamirande EW, Babcock GJ, Greenough TC, et al. (March 2006). "Therapy with a severe acute respiratory syndrome-associated coronavirus-neutralizing human monoclonal antibody reduces disease severity and viral burden in golden Syrian hamsters". The Journal of Infectious Diseases. 193 (5): 685–92. doi:10.1086/500143. PMC 7109703. PMID 16453264.
- ^ a b Jiang S, Lu L, Du L (January 2013). "Development of SARS vaccines and therapeutics is still needed". Future Virology. 8 (1): 1–2. doi:10.2217/fvl.12.126. PMC 7079997. PMID 32201503.
- ^ "SARS (severe acute respiratory syndrome)". National Health Service. 5 March 2020. Archived from the original on 9 March 2020. Retrieved 31 January 2020.
- ^ Shehata MM, Gomaa MR, Ali MA, Kayali G (June 2016). "Middle East respiratory syndrome coronavirus: a comprehensive review". Frontiers of Medicine. 10 (2): 120–36. doi:10.1007/s11684-016-0430-6. PMC 7089261. PMID 26791756.
- ^ Butler D (October 2012). "SARS veterans tackle coronavirus". Nature. 490 (7418): 20. Bibcode:2012Natur.490...20B. doi:10.1038/490020a. PMID 23038444.
- ^ Modjarrad K, Roberts CC, Mills KT, Castellano AR, Paolino K, Muthumani K, et al. (September 2019). "Safety and immunogenicity of an anti-Middle East respiratory syndrome coronavirus DNA vaccine: a phase 1, open-label, single-arm, dose-escalation trial". The Lancet. Infectious Diseases. 19 (9): 1013–1022. doi:10.1016/S1473-3099(19)30266-X. PMC 7185789. PMID 31351922.
- ^ Yong CY, Ong HK, Yeap SK, Ho KL, Tan WS (2019). "Recent Advances in the Vaccine Development Against Middle East Respiratory Syndrome-Coronavirus". Frontiers in Microbiology. 10: 1781. doi:10.3389/fmicb.2019.01781. PMC 6688523. PMID 31428074.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ a b c d e f g h Le TT, Cramer JP, Chen R, Mayhew S (October 2020). "Evolution of the COVID-19 vaccine development landscape". Nature Reviews. Drug Discovery. 19 (10): 667–668. doi:10.1038/d41573-020-00151-8. PMID 32887942. S2CID 221503034.
- ^ a b c d e Thanh Le T, Andreadakis Z, Kumar A, Gómez Román R, Tollefsen S, Saville M, Mayhew S (May 2020). "The COVID-19 vaccine development landscape". Nature Reviews. Drug Discovery. 19 (5): 305–306. doi:10.1038/d41573-020-00073-5. PMID 32273591.
- ^ Simpson S, Kaufmann MC, Glozman V, Chakrabarti A (May 2020). "Disease X: accelerating the development of medical countermeasures for the next pandemic". The Lancet. Infectious Diseases. 20 (5): e108–e115. doi:10.1016/S1473-3099(20)30123-7. PMC 7158580. PMID 32197097.
- ^ a b c d Sanger DE, Kirkpatrick DD, Zimmer C, Thomas K, Wee SL (2 May 2020). "With Pressure Growing, Global Race for a Vaccine Intensifies". The New York Times. ISSN 0362-4331. Archived from the original on 11 May 2020. Retrieved 2 May 2020.
- ^ a b c d Steenhuysen J, Eisler P, Martell A, Nebehay S (27 April 2020). "Special Report: Countries, companies risk billions in race for coronavirus vaccine". Reuters. Archived from the original on 15 May 2020. Retrieved 2 May 2020.
- ^ Jeong-ho L, Zheng W, Zhou L (26 January 2020). "Chinese scientists race to develop vaccine as coronavirus death toll jumps". South China Morning Post. Archived from the original on 26 January 2020. Retrieved 28 January 2020.
- ^ Wee SL (4 May 2020). "China's coronavirus vaccine drive empowers a troubled industry". The New York Times. ISSN 0362-4331. Archived from the original on 4 May 2020. Retrieved 4 May 2020.
- ^ a b c Diamond MS, Pierson TC (May 2020). "The Challenges of Vaccine Development against a New Virus during a Pandemic". Cell Host & Microbe. 27 (5): 699–703. doi:10.1016/j.chom.2020.04.021. PMC 7219397. PMID 32407708.
- ^ Thorp HH (March 2020). "Underpromise, overdeliver". Science. 367 (6485): 1405. Bibcode:2020Sci...367.1405T. doi:10.1126/science.abb8492. PMID 32205459.
- ^ Blackwell T (20 April 2020). "COVID-19 vaccine researchers say pandemic lockdown placing many serious obstacles to their work". National Post. Archived from the original on 1 November 2020. Retrieved 3 May 2020.
- ^ Chen J (4 May 2020). "Covid-19 has shuttered labs. It could put a generation of researchers at risk". Stat. Archived from the original on 6 May 2020. Retrieved 4 May 2020.
- ^ a b c "Vaccine Safety – Vaccines". vaccines.gov. US Department of Health and Human Services. Archived from the original on 22 April 2020. Retrieved 13 April 2020.
- ^ a b c d "The drug development process". U.S. Food and Drug Administration (FDA). 4 January 2018. Archived from the original on 22 February 2020. Retrieved 12 April 2020.
- ^ a b Cohen J (June 2020). "Pandemic vaccines are about to face the real test". Science. 368 (6497): 1295–1296. Bibcode:2020Sci...368.1295C. doi:10.1126/science.368.6497.1295. PMID 32554572.
- ^ a b Dubé E, Laberge C, Guay M, Bramadat P, Roy R, Bettinger J (August 2013). "Vaccine hesitancy: an overview". Human Vaccines & Immunotherapeutics. 9 (8): 1763–73. doi:10.4161/hv.24657. PMC 3906279. PMID 23584253.
- ^ Howard J, Stracqualursi V (18 June 2020). "Fauci warns of 'anti-science bias' being a problem in US". CNN. Archived from the original on 21 June 2020. Retrieved 21 June 2020.
- ^ "Vaccines: The Emergency Authorisation Procedure". European Medicines Agency. 2020. Archived from the original on 24 September 2020. Retrieved 21 August 2020.
- ^ Byrne J (19 October 2020). "Moderna COVID-19 vaccine under rolling review process in Canada, EU". BioPharma-Reporter.com, William Reed Business Media Ltd. Retrieved 25 November 2020.
- ^ Dangerfield K (20 November 2020). "Pfizer files for emergency use of coronavirus vaccine in U.S. – what about in Canada?". Global News. Retrieved 25 November 2020.
- ^ "G20 launches initiative for health tools needed to combat the coronavirus". The Globe and Mail. 25 April 2020.
- ^ "Access to COVID-19 Tools (ACT) Accelerator" (PDF). World Health Organization (WHO). 24 April 2020.
- ^ "The ACT-Accelerator: frequently asked questions (FAQ)". World Health Organization (WHO). 2020. Retrieved 16 December 2020.
- ^ "Update on WHO Solidarity Trial – Accelerating a safe and effective COVID-19 vaccine". World Health Organization (WHO). 27 April 2020. Archived from the original on 30 April 2020. Retrieved 2 May 2020.
It is vital that we evaluate as many vaccines as possible as we cannot predict how many will turn out to be viable. To increase the chances of success (given the high level of attrition during vaccine development), we must test all candidate vaccines until they fail. [The] WHO is working to ensure that all of them have the chance of being tested at the initial stage of development. The results for the efficacy of each vaccine are expected within three to six months and this evidence, combined with data on safety, will inform decisions about whether it can be used on a wider scale.
- ^ Abedi M (23 March 2020). "Canada to spend $192M on developing COVID-19 vaccine". Global News. Archived from the original on 9 April 2020. Retrieved 24 March 2020.
- ^ "Government of Canada's research response to COVID-19". Government of Canada. 23 April 2020. Archived from the original on 13 May 2020. Retrieved 4 May 2020.
- ^ Takada N, Satake M (2 May 2020). "US and China unleash wallets in race for coronavirus vaccine". Nikkei Asian Review. Archived from the original on 10 May 2020. Retrieved 3 May 2020.
- ^ Morriss E (22 April 2020). "Government launches coronavirus vaccine taskforce as human clinical trials start". Pharmafield. Archived from the original on 17 June 2020. Retrieved 3 May 2020.
- ^ Kuznia R, Polglase K, Mezzofiore G (1 May 2020). "In quest for vaccine, US makes 'big bet' on company with unproven technology". CNN. Archived from the original on 13 May 2020. Retrieved 2 May 2020.
- ^ Cohen J (May 2020). "U.S. 'Warp Speed' vaccine effort comes out of the shadows". Science. 368 (6492): 692–693. Bibcode:2020Sci...368..692C. doi:10.1126/science.368.6492.692. PMID 32409451.
- ^ "Trump introduces 'Warp Speed' leaders to hasten COVID-19 vaccine". Bloomberg. 15 May 2020. Archived from the original on 21 May 2020. Retrieved 15 May 2020.
{{cite news}}: Unknown parameter|authors=ignored (help) - ^ "World Health Organization timeline – COVID-19". World Health Organization (WHO). 27 April 2020. Archived from the original on 29 April 2020. Retrieved 2 May 2020.
- ^ a b c Thanh Le T, Andreadakis Z, Kumar A, Gómez Román R, Tollefsen S, Saville M, Mayhew S (May 2020). "The COVID-19 vaccine development landscape". Nature Reviews. Drug Discovery. 19 (5): 305–306. doi:10.1038/d41573-020-00073-5. PMID 32273591.
- ^ a b Gates B (February 2020). "Responding to Covid-19: A once-in-a-century pandemic?". The New England Journal of Medicine. 382 (18): 1677–79. doi:10.1056/nejmp2003762. PMID 32109012.
- ^ Fauci AS, Lane HC, Redfield RR (March 2020). "Covid-19: Navigating the uncharted". The New England Journal of Medicine. 382 (13): 1268–69. doi:10.1056/nejme2002387. PMC 7121221. PMID 32109011.
- ^ a b Le TT, Cramer JP, Chen R, Mayhew S (October 2020). "Evolution of the COVID-19 vaccine development landscape". Nature Reviews. Drug Discovery. 19 (10): 667–668. doi:10.1038/d41573-020-00151-8. PMID 32887942. S2CID 221503034.
- ^ Weintraub, Rebecca; Yadav, Prashant; Berkley, Seth (2 April 2020). "A COVID-19 vaccine will need equitable, global distribution". Harvard Business Review. ISSN 0017-8012. Archived from the original on 9 June 2020. Retrieved 9 June 2020.
- ^ "COVID-19 pandemic reveals the risks of relying on private sector for life-saving vaccines, says expert". CBC Radio. 8 May 2020. Archived from the original on 13 May 2020. Retrieved 8 June 2020.
- ^ Ahmed, Darius D. (4 June 2020). "Oxford, AstraZeneca COVID-19 deal reinforces 'vaccine sovereignty'". Stat. Archived from the original on 12 June 2020. Retrieved 8 June 2020.
- ^ Grenfell, Rob; Drew, Trevor (14 February 2020). "Here's why the WHO says a coronavirus vaccine is 18 months away". Business Insider. Archived from the original on 5 December 2020. Retrieved 11 November 2020.
- ^ Offit, Paul (13 February 2021). "TWiV 720: With vaccines, Offit is on it". This Week in Virology Podcast. Vincent Racaniello Youtube Channel. Archived from the original on 25 May 2021. Retrieved 14 July 2021.
- ^ "Update on WHO Solidarity Trial – Accelerating a safe and effective COVID-19 vaccine". World Health Organization (WHO). 27 April 2020. Archived from the original on 30 April 2020. Retrieved 2 May 2020.
It is vital that we evaluate as many vaccines as possible as we cannot predict how many will turn out to be viable. To increase the chances of success (given the high level of attrition during vaccine development), we must test all candidate vaccines until they fail. [The] WHO is working to ensure that all of them have the chance of being tested at the initial stage of development. The results for the efficacy of each vaccine are expected within three to six months and this evidence, combined with data on safety, will inform decisions about whether it can be used on a wider scale.
- ^ Yamey G, Schäferhoff M, Hatchett R, Pate M, Zhao F, McDade KK (May 2020). "Ensuring global access to COVID‑19 vaccines". Lancet. 395 (10234): 1405–06. doi:10.1016/S0140-6736(20)30763-7. PMC 7271264. PMID 32243778.
CEPI estimates that developing up to three vaccines in the next 12–18 months will require an investment of at least US$2 billion. This estimate includes Phase 1 clinical trials of eight vaccine candidates, progression of up to six candidates through Phase 2 and 3 trials, completion of regulatory and quality requirements for at least three vaccines, and enhancing global manufacturing capacity for three vaccines.
- ^ "WHO 'backed China's emergency use' of experimental Covid-19 vaccines". South China Morning Post. 25 September 2020. Archived from the original on 26 September 2020. Retrieved 26 September 2020.
- ^ Kramer, Andrew E. (19 September 2020). "Russia Is Slow to Administer Virus Vaccine Despite Kremlin's Approval". The New York Times. ISSN 0362-4331. Archived from the original on 27 September 2020. Retrieved 28 September 2020.
- ^ "Pfizer and BioNTech to Submit Emergency Use Authorization Request Today to the U.S. FDA for COVID-19 Vaccine". Pfizer (Press release). 20 November 2020. Archived from the original on 29 January 2021. Retrieved 20 November 2020.
- ^ Park, Alice (20 November 2020). "Exclusive: Pfizer CEO Discusses Submitting the First COVID-19 Vaccine Clearance Request to the FDA". Time. Archived from the original on 29 January 2021. Retrieved 20 November 2020.
- ^ "Information for Healthcare Professionals on Pfizer/BioNTech COVID-19 vaccine". Medicines & Healthcare products Regulatory Agency (MHRA). 8 December 2020. Archived from the original on 15 March 2021. Retrieved 13 December 2020.
- ^ "Conditions of Authorisation for Pfizer/BioNTech COVID-19 vaccine". Medicines and Healthcare products Regulatory Agency (MHRA). 3 December 2020. Archived from the original on 26 February 2021. Retrieved 19 December 2020.
- ^ "UK medicines regulator gives approval for first UK COVID-19 vaccine". Medicines and Healthcare Products Regulatory Agency, Government of the UK. 2 December 2020. Archived from the original on 17 March 2021. Retrieved 2 December 2020.
- ^ Mueller, Benjamin (2 December 2020). "U.K. Approves Pfizer Coronavirus Vaccine, a First in the West". The New York Times. Archived from the original on 28 January 2021. Retrieved 2 December 2020.
- ^ Roberts, Michelle (2 December 2020). "Covid Pfizer vaccine approved for use next week in UK". BBC News Online. Archived from the original on 2 December 2020. Retrieved 2 December 2020.
- ^ "Questions and Answers: COVID-19 vaccination in the EU". European Commission. 21 December 2020. Archived from the original on 29 January 2021. Retrieved 21 December 2020.
- ^ "Bahrain second in the world to approve the Pfizer/BioNTech Covid-19 vaccine". Bahrain News Agency. 4 December 2020. Archived from the original on 17 December 2020. Retrieved 9 December 2020.
- ^ "UAE: Ministry of Health announces 86 per cent vaccine efficacy". Gulf News. Archived from the original on 24 December 2020. Retrieved 9 December 2020.
- ^ Thomas K, LaFraniere S, Weiland N, Goodnough A, Haberman M (12 December 2020). "F.D.A. Clears Pfizer Vaccine, and Millions of Doses Will Be Shipped Right Away". The New York Times. Archived from the original on 12 December 2020. Retrieved 12 December 2020.
- ^ "FDA Takes Additional Action in Fight Against COVID-19 By Issuing Emergency Use Authorization for Second COVID-19 Vaccine". U.S. Food and Drug Administration (FDA) (Press release). Archived from the original on 17 March 2021. Retrieved 18 December 2020.
- ^ Oliver SE, Gargano JW, Marin M, Wallace M, Curran KG, Chamberland M, McClung N, Campos-Outcalt D, Morgan RL, Mbaeyi S, Romero JR, Talbot HK, Lee GM, Bell BP, Dooling K (January 2021). "The Advisory Committee on Immunization Practices' Interim Recommendation for Use of Moderna COVID-19 Vaccine - United States, December 2020" (PDF). MMWR. Morbidity and Mortality Weekly Report. 69 (5152): 1653–56. doi:10.15585/mmwr.mm695152e1. PMC 9191904. PMID 33382675. S2CID 229945697. Archived (PDF) from the original on 9 February 2021. Retrieved 18 January 2021.
- ^ Lovelace Jr B (19 December 2020). "FDA approves second Covid vaccine for emergency use as it clears Moderna's for U.S. distribution". CNBC. Archived from the original on 26 January 2021. Retrieved 19 December 2020.
- ^ Corum J, Zimmer C (17 December 2020). "How the Oxford-AstraZeneca Vaccine Works". The New York Times. Archived from the original on 5 January 2022. Retrieved 2 May 2021.
- ^ Tétrault-Farber M, Vasilyeva G (31 March 2021). "Russia registers world's first COVID-19 vaccine for animals". Reuters. Archived from the original on 17 December 2021. Retrieved 4 April 2021.
- ^ "В России зарегистрировали первую в мире вакцину против COVID-19 для животных" [The world's first COVID-19 vaccine for animals was registered in Russia]. TASS (in Russian). Moscow. 31 March 2021. Archived from the original on 19 May 2021. Retrieved 19 May 2021.
- ^ MORITSUGU, KEN (26 October 2022). "Afraid of needles? China using inhalable COVID-19 vaccine". AP NEWS. Retrieved 2 November 2022.
- ^ Hotez PJ, Bottazzi ME (January 2022). "Whole Inactivated Virus and Protein-Based COVID-19 Vaccines". Annual Review of Medicine. 73 (1): 55–64. doi:10.1146/annurev-med-042420-113212. PMID 34637324. S2CID 238747462.
- ^ Ye Y, Zhang Q, Wei X, Cao Z, Yuan HY, Zeng DD (February 2022). "Equitable access to COVID-19 vaccines makes a life-saving difference to all countries". Nature Human Behaviour. 6 (2): 207–216. doi:10.1038/s41562-022-01289-8. PMC 8873023. PMID 35102361.
- ^ Krammer F (October 2020). "SARS-CoV-2 vaccines in development". Nature. 586 (7830): 516–527. Bibcode:2020Natur.586..516K. doi:10.1038/s41586-020-2798-3. PMID 32967006. S2CID 221887746.
- ^ Park KS, Sun X, Aikins ME, Moon JJ (February 2021). "Non-viral COVID-19 vaccine delivery systems". Advanced Drug Delivery Reviews. 169: 137–151. doi:10.1016/j.addr.2020.12.008. PMC 7744276. PMID 33340620.
- ^ Kowalski PS, Rudra A, Miao L, Anderson DG (April 2019). "Delivering the Messenger: Advances in Technologies for Therapeutic mRNA Delivery". Molecular Therapy. 27 (4): 710–728. doi:10.1016/j.ymthe.2019.02.012. PMC 6453548. PMID 30846391.
- ^ Verbeke R, Lentacker I, De Smedt SC, Dewitte H (October 2019). "Three decades of messenger RNA vaccine development". Nano Today. 28: 100766. doi:10.1016/j.nantod.2019.100766.
- ^ "COVID-19 ACIP Vaccine Recommendations". Centers for Disease Control and Prevention (CDC). Retrieved 18 February 2021.
- ^ "Safe COVID-19 vaccines for Europeans". European Commission – European Commission. Retrieved 19 February 2021.
- ^ a b c "Regulatory Decision Summary – Pfizer-BioNTech COVID-19 Vaccine". Health Canada, Government of Canada. 9 December 2020. Retrieved 9 December 2020.
- ^ a b "Study to Describe the Safety, Tolerability, Immunogenicity, and Efficacy of RNA Vaccine Candidates Against COVID-19 in Healthy Adults". ClinicalTrials.gov. United States National Library of Medicine. 30 April 2020. NCT04368728. Archived from the original on 11 October 2020. Retrieved 14 July 2020.
- ^ a b "A Multi-site Phase I/II, 2-Part, Dose-Escalation Trial Investigating the Safety and Immunogenicity of four Prophylactic SARS-CoV-2 RNA Vaccines Against COVID-19 Using Different Dosing Regimens in Healthy Adults". EU Clinical Trials Register. European Union. 14 April 2020. EudraCT 2020-001038-36. Archived from the original on 22 April 2020. Retrieved 22 April 2020.
- ^ a b "A Study to Evaluate Efficacy, Safety, and Immunogenicity of mRNA-1273 Vaccine in Adults Aged 18 Years and Older to Prevent COVID-19". ClinicalTrials.gov. United States National Library of Medicine. 14 July 2020. NCT04470427. Archived from the original on 11 October 2020. Retrieved 27 July 2020.
- ^ a b Palca J (27 July 2020). "COVID-19 vaccine candidate heads to widespread testing in U.S." NPR. Archived from the original on 11 October 2020. Retrieved 27 July 2020.
- ^ a b "EMA starts rolling review of CureVac's COVID-19 vaccine (CVnCoV)". European Medicines Agency (EMA) (Press release). 1 December 2020. Retrieved 12 February 2021.
- ^ a b c Moghimi SM (2021). "Allergic Reactions and Anaphylaxis to LNP-Based COVID-19 Vaccines". Molecular Therapy. 29 (3): 898–900. doi:10.1016/j.ymthe.2021.01.030. PMC 7862013. PMID 33571463.
- ^ a b "What are viral vector-based vaccines and how could they be used against COVID-19?". GAVI. 2020. Retrieved 26 January 2021.
- ^ a b c "Investigating a Vaccine Against COVID-19". ClinicalTrials.gov. United States National Library of Medicine. 26 May 2020. NCT04400838. Archived from the original on 11 October 2020. Retrieved 14 July 2020.
- ^ a b "A Phase 2/3 study to determine the efficacy, safety and immunogenicity of the candidate Coronavirus Disease (COVID-19) vaccine ChAdOx1 nCoV-19". EU Clinical Trials Register. European Union. 21 April 2020. EudraCT 2020-001228-32. Archived from the original on 5 October 2020. Retrieved 3 August 2020.
- ^ a b O'Reilly P (26 May 2020). "A Phase III study to investigate a vaccine against COVID-19". ISRCTN. doi:10.1186/ISRCTN89951424. ISRCTN89951424.
- ^ Corum J, Carl Z (8 January 2021). "How Gamaleya's Vaccine Works". The New York Times. Retrieved 27 January 2021.
- ^ a b "A Study of Ad26.COV2.S in Adults". ClinicalTrials.gov. 4 August 2020. Archived from the original on 16 September 2020. Retrieved 23 August 2020.
- ^ a b "A Study of Ad26.COV2.S for the Prevention of SARS-CoV-2-Mediated COVID-19 in Adult Participants". ClinicalTrials.gov. US National Library of Medicine. Archived from the original on 26 September 2020.
- ^ Johnson C, McGinley L. "Johnson & Johnson seeks emergency FDA authorization for single-shot coronavirus vaccine". The Washington Post.
- ^ "It's not just Johnson & Johnson: China has a single-dose COVID-19 vaccine that's 65% effective". Fortune. Retrieved 28 February 2021.
- ^ Petrovsky N, Aguilar JC (October 2004). "Vaccine adjuvants: current state and future trends". Immunology and Cell Biology. 82 (5): 488–96. doi:10.1111/j.0818-9641.2004.01272.x. PMID 15479434. S2CID 154670.
- ^ a b c "Safety and Immunogenicity Study of Inactivated Vaccine for Prevention of SARS-CoV-2 Infection (COVID-19) (Renqiu)". ClinicalTrials.gov. United States National Library of Medicine. 12 May 2020. NCT04383574. Archived from the original on 11 October 2020. Retrieved 14 July 2020.
- ^ a b "Clinical Trial of Efficacy and Safety of Sinovac's Adsorbed COVID-19 (Inactivated) Vaccine in Healthcare Professionals (PROFISCOV)". ClinicalTrials.gov. United States National Library of Medicine. 2 July 2020. NCT04456595. Archived from the original on 11 October 2020. Retrieved 3 August 2020.
- ^ a b PT. Bio Farma (10 August 2020). "A Phase III, observer-blind, randomized, placebo-controlled study of the efficacy, safety, and immunogenicity of SARS-COV-2 inactivated vaccine in healthy adults aged 18–59 years in Indonesia". Registri Penyakit Indonesia. Retrieved 15 August 2020.
- ^ a b c Chen W, Al Kaabi N (18 July 2020). "A Phase III clinical trial for inactivated novel coronavirus pneumonia (COVID-19) vaccine (Vero cells)". Chinese Clinical Trial Registry. Retrieved 15 August 2020.
- ^ https://www.reuters.com/article/us-health-coronavirus-russia-vaccine-idUSKBN2AK07H
- ^ a b "VLA2001 COVID-19 Vaccine". Precision Vaccinations. 31 December 2020. Retrieved 11 January 2021.
- ^ a b "Dose Finding Study to Evaluate Safety, Tolerability and Immunogenicity of an Inactiviated Adjuvanted Sars-Cov-2 Virus Vaccine Candidate Against Covid-19 in Healthy Adults". clinicaltrials.gov. U.S. National Library of Medicine. 30 December 2020. Retrieved 11 January 2021.
- ^ "Module 2 – Subunit vaccines". WHO Vaccine Safety Basics.
- ^ "Study of the Safety, Reactogenicity and Immunogenicity of "EpiVacCorona" Vaccine for the Prevention of COVID-19 (EpiVacCorona)". ClinicalTrials.gov. United States National Library of Medicine. 22 September 2020. NCT04368988. Retrieved 16 November 2020.
- ^ a b "Evaluation of the Safety and Immunogenicity of a SARS-CoV-2 rS (COVID-19) Nanoparticle Vaccine With/Without Matrix-M Adjuvant". ClinicalTrials.gov. United States National Library of Medicine. 30 April 2020. NCT04368988. Archived from the original on 14 July 2020. Retrieved 14 July 2020.
- ^ a b "A Study on the Safety, Tolerability and Immune Response of SARS-CoV-2 Sclamp (COVID-19) Vaccine in Healthy Adults". ClinicalTrials.gov. United States National Library of Medicine. 3 August 2020. NCT04495933. Archived from the original on 11 October 2020. Retrieved 4 August 2020.
- ^ a b "UQ-CSL V451 Vaccine". precisionvaccinations.com. Retrieved 11 December 2020.
- ^ a b "A prospective, randomized, adaptive, phase I/II clinical study to evaluate the safety and immunogenicity of Novel Corona Virus −2019-nCov vaccine candidate of M/s Cadila Healthcare Limited by intradermal route in healthy subjects". ctri.nic.in. Clinical Trials Registry India. 15 December 2020. CTRI/2020/07/026352. Archived from the original on 22 November 2020.
- ^ a b "Safety, Tolerability and Immunogenicity of INO-4800 for COVID-19 in Healthy Volunteers". ClinicalTrials.gov. United States National Library of Medicine. 7 April 2020. NCT04336410. Archived from the original on 11 October 2020. Retrieved 14 July 2020.
- ^ a b "IVI, INOVIO, and KNIH to partner with CEPI in a Phase I/II clinical trial of INOVIO's COVID-19 DNA vaccine in South Korea". International Vaccine Institute. 16 April 2020. Retrieved 23 April 2020.
- ^ a b "Study of COVID-19 DNA Vaccine (AG0301-COVID19)". ClinicalTrials.gov. United States National Library of Medicine. 9 July 2020. NCT04463472. Archived from the original on 11 October 2020. Retrieved 14 July 2020.
- ^ a b "Safety and Immunogenicity Study of GX-19, a COVID-19 Preventive DNA Vaccine in Healthy Adults". ClinicalTrials.gov. United States National Library of Medicine. 24 June 2020. NCT04445389. Archived from the original on 11 October 2020. Retrieved 14 July 2020.
- ^ a b "S. Korea's Genexine begins human trial of coronavirus vaccine". Reuters. 19 June 2020. Archived from the original on 11 October 2020. Retrieved 25 June 2020.
- ^ a b "Safety and Immunity of Covid-19 aAPC Vaccine". ClinicalTrials.gov. United States National Library of Medicine. 9 March 2020. NCT04299724. Archived from the original on 11 October 2020. Retrieved 14 July 2020.
- ^ a b "Immunity and Safety of Covid-19 Synthetic Minigene Vaccine". ClinicalTrials.gov. United States National Library of Medicine. 19 February 2020. NCT04276896. Archived from the original on 11 October 2020. Retrieved 14 July 2020.
- ^ a b "A Phase I/II Randomized, Multi-Center, Placebo-Controlled, Dose-Escalation Study to Evaluate the Safety, Immunogenicity and Potential Efficacy of an rVSV-SARS-CoV-2-S Vaccine (IIBR-100) in Adults". ClinicalTrials.gov. United States National Library of Medicine. 1 November 2020. NCT04608305.
- ^ Johnson CY, Mufson S. "Can old vaccines from science's medicine cabinet ward off coronavirus?". The Washington Post. ISSN 0190-8286. Retrieved 31 December 2020.
- ^ "Bacille Calmette-Guérin (BCG) vaccination and COVID-19". World Health Organization (WHO). 12 April 2020. Archived from the original on 30 April 2020. Retrieved 1 May 2020.
- ^ "FDA Briefing Document: Pfizer-BioNTech COVID-19 Vaccine" (PDF). U.S. Food and Drug Administration. 10 December 2020. Retrieved 1 January 2021.
- ^ a b c Zimmer C (20 November 2020). "2 Companies Say Their Vaccines Are 95% Effective. What Does That Mean? You might assume that 95 out of every 100 people vaccinated will be protected from Covid-19. But that's not how the math works". The New York Times. Retrieved 21 November 2020.
- ^ Branswell H (2 February 2021). "Comparing three Covid-19 vaccines: Pfizer, Moderna, J&J". Stat. Retrieved 28 February 2021.
- ^ Randolph HE, Barreiro LB (May 2020). "Herd Immunity: Understanding COVID-19". Immunity. 52 (5): 737–741. doi:10.1016/j.immuni.2020.04.012. PMC 7236739. PMID 32433946.
- ^ "The FDA's cutoff for Covid-19 vaccine effectiveness is 50 percent. What does that mean?". NBC News. Retrieved 8 January 2021.
- ^ "EMA sets 50% efficacy goal – with flexibility – for COVID vaccines". raps.org. Retrieved 8 January 2021.
- ^ Bartsch SM, O'Shea KJ, Ferguson MC, Bottazzi ME, Wedlock PT, Strych U, et al. (October 2020). "Vaccine Efficacy Needed for a COVID-19 Coronavirus Vaccine to Prevent or Stop an Epidemic as the Sole Intervention". American Journal of Preventive Medicine. 59 (4): 493–503. doi:10.1016/j.amepre.2020.06.011. PMC 7361120. PMID 32778354.
- ^ Dean N, Madewell Z (5 March 2021). "Understanding the spectrum of vaccine efficacy measures". The BMJ Opinion. Retrieved 10 March 2021.
- ^ "Moderna COVID-19 Vaccine – cx-024414 injection, suspension". DailyMed. U.S. National Institutes of Health. Retrieved 20 December 2020.
{{cite web}}: CS1 maint: url-status (link) - ^ "Pfizer-BioNTech COVID-19 Vaccine – rna ingredient bnt-162b2 injection, suspension". DailyMed. U.S. National Institutes of Health. Retrieved 14 December 2020.
{{cite web}}: CS1 maint: url-status (link) - ^ a b Logunov DY, Dolzhikova IV, Shcheblyakov DV, Tukhvatulin AI, Zubkova OV, Dzharullaeva AS, et al. (February 2021). "Safety and efficacy of an rAd26 and rAd5 vector-based heterologous prime-boost COVID-19 vaccine: an interim analysis of a randomised controlled phase 3 trial in Russia". Lancet. 397 (10275): 671–681. doi:10.1016/S0140-6736(21)00234-8. PMC 7852454. PMID 33545094.
- ^ a b Voysey M, Costa Clemens SA, Madhi SA, Weckx LY, Folegatti PM, Aley PK, et al. (March 2021). "Single-dose administration and the influence of the timing of the booster dose on immunogenicity and efficacy of ChAdOx1 nCoV-19 (AZD1222) vaccine: a pooled analysis of four randomised trials". Lancet. 397 (10277): 881–891. doi:10.1016/S0140-6736(21)00432-3. PMC 7894131. PMID 33617777.
- ^ "AZD1222 US Phase III primary analysis confirms safety and efficacy". Retrieved 25 March 2021.
- ^ Wadman M, Cohen J (28 January 2021). "Novavax vaccine delivers 89% efficacy against COVID-19 in UK – but is less potent in South Africa". Science. doi:10.1126/science.abg8101.
- ^ "Novavax COVID-19 Vaccine Demonstrates 89.3% Efficacy in UK Phase 3 Trial | Novavax Inc. - IR Site". ir.novavax.com. Retrieved 3 March 2021.
- ^ a b "UAE says Sinopharm vaccine has 86% efficacy against COVID-19". Reuters. Dubai. 9 December 202. Retrieved 10 March 2021.
- ^ Wee SL, Qin A (30 December 2020). "A Chinese Covid-19 Vaccine Has Proved Effective, Its Maker Says". The New York Times. Retrieved 30 December 2020.
- ^ "Sinovac says COVID-19 vaccine effective in preventing hospitalization, death". Reuters. 5 February 2021. Retrieved 10 March 2021.
- ^ "Sinovac's Covid Shot Proves 78% Effective in Brazil Trial". Bloomberg. 7 January 2021. Retrieved 7 January 2021.
- ^ "Chile Approves Chinese Coronavirus Vaccine". Barron's. Agence France-Presse. 20 January 2021. Retrieved 10 March 2021.
- ^ a b "Janssen COVID-19 Vaccine - ad26.cov2.s injection, suspension". DailyMed. U.S. National Institutes of Health. Retrieved 15 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "Bharat Biotech's Covaxin found 81% effective in interim phase 3 trials". mint. 3 March 2021.
- ^ "Bharat Biotech Announces Phase 3 Results of COVAXIN: India's First COVID-19 Vaccine Demonstrates Interim Clinical Efficacy of 81%" (PDF) (Press release). Hyderabad: Bharat Biotech. 3 March 2021. Retrieved 10 March 2021.
- ^ a b c d Peshimam G, Farooq U (8 February 2021). "CanSinoBIO's COVID-19 vaccine 65.7% effective in global trials, Pakistan official says". Reuters. Islamabad. Retrieved 5 March 2021.
its single-dose regimen and normal refrigerator storage requirement could make it a favourable option for many countries
- ^ Amir Tal and Elizabeth Cohen (29 January 2021). "Israel's health data suggests Pfizer and Moderna vaccines may be more effective than we thought". CNN. Retrieved 27 March 2021.
- ^ "Interim Estimates of Vaccine Effectiveness of BNT162b2 and mRNA-1273 COVID-19 Vaccines in Preventing SARS-CoV-2 Infection Among Health Care Personnel, First Responders, and Other Essential and Frontline Workers — Eight U.S. Locations, December 2020–March 2021". cdc.gov. 29 March 2021.
- ^ a b Office of the Commissioner (23 February 2021). "Coronavirus (COVID-19) Update: FDA Issues Policies to Guide Medical Product Developers Addressing Virus Variants". FDA. Retrieved 7 March 2021.
- ^ Mahase E (March 2021). "Covid-19: Where are we on vaccines and variants?". BMJ. 372: n597. doi:10.1136/bmj.n597. PMID 33653708. S2CID 232093175.
- ^ "Inside the B.1.1.7 Coronavirus Variant". The New York Times. 18 January 2021. Retrieved 29 January 2021.
- ^ Muik A, Wallisch AK, Sänger B, Swanson KA, Mühl J, Chen W, et al. (March 2021). "Neutralization of SARS-CoV-2 lineage B.1.1.7 pseudovirus by BNT162b2 vaccine-elicited human sera". Science. 371 (6534): 1152–1153. doi:10.1126/science.abg6105. PMID 33514629.
- ^ a b Wang P, Nair MS, Liu L, Iketani S, Luo Y, Guo Y, et al. (March 2021). "Antibody Resistance of SARS-CoV-2 Variants B.1.351 and B.1.1.7". Nature. doi:10.1038/s41586-021-03398-2.
- ^ Emary KR, Golubchik T, Aley PK, Ariani CV, Angus BJ, Bibi S, et al. (2021). "Efficacy of ChAdOx1 nCoV-19 (AZD1222) Vaccine Against SARS-CoV-2 VOC 202012/01 (B.1.1.7)". SSRN Electronic Journal. doi:10.2139/ssrn.3779160. ISSN 1556-5068.
- ^ Mahase E (February 2021). "Covid-19: Novavax vaccine efficacy is 86% against UK variant and 60% against South African variant". BMJ. 372: n296. doi:10.1136/bmj.n296. PMID 33526412. S2CID 231730012.
- ^ Kuchler H (25 January 2021). "Moderna develops new vaccine to tackle mutant Covid strain". Financial Times. Retrieved 30 January 2021.
- ^ Liu Y, Liu J, Xia H, Zhang X, Fontes-Garfias CR, Swanson KA, et al. (February 2021). "Neutralizing Activity of BNT162b2-Elicited Serum - Preliminary Report". The New England Journal of Medicine. doi:10.1056/nejmc2102017. PMID 33596352.
- ^ a b Hoffmann M, Arora P, Gross R, Seidel A, Hoernich BF, Hahn AS, et al. (March 2021). "1 SARS-CoV-2 variants B.1.351 and P.1 escape from neutralizing antibodies". Cell. doi:10.1016/j.cell.2021.03.036.
- ^ "Johnson & Johnson Announces Single-Shot Janssen COVID-19 Vaccine Candidate Met Primary Endpoints in Interim Analysis of its Phase 3 ENSEMBLE Trial" (Press release). Johnson & Johnson. 29 January 2021. Retrieved 29 January 2021.
- ^ Francis D, Andy B (6 February 2021). "Oxford/AstraZeneca COVID shot less effective against South African variant: study". Reuters. Retrieved 8 February 2021.
- ^ "South Africa halts AstraZeneca jab over new strain". BBC News. 7 February 2021. Retrieved 8 February 2021.
- ^ Booth W, Johnson CY (7 February 2021). "South Africa suspends Oxford-AstraZeneca vaccine rollout after researchers report 'minimal' protection against coronavirus variant". The Washington Post. London. Retrieved 8 February 2021.
South Africa will suspend use of the coronavirus vaccine being developed by Oxford University and AstraZeneca after researchers found it provided "minimal protection" against mild to moderate coronavirus infections caused by the new variant first detected in that country.
- ^ "Covid: South Africa halts AstraZeneca vaccine rollout over new variant". BBC News. 8 February 2021. Retrieved 12 February 2021.
- ^ "How flu vaccine effectiveness and efficacy are measured". Centers for Disease Control and Prevention, National Center for Immunization and Respiratory Diseases, US Department of Health and Human Services. 29 January 2016. Archived from the original on 7 May 2020. Retrieved 6 May 2020.
- ^ "Principles of epidemiology, Section 8: Concepts of disease occurrence". Centers for Disease Control and Prevention, Center for Surveillance, Epidemiology, and Laboratory Services, US Department of Health and Human Services. 18 May 2012. Archived from the original on 6 April 2020. Retrieved 6 May 2020.
- ^ a b Pallmann P, Bedding AW, Choodari-Oskooei B, Dimairo M, Flight L, Hampson LV, et al. (February 2018). "Adaptive designs in clinical trials: why use them, and how to run and report them". BMC Medicine. 16 (1): 29. doi:10.1186/s12916-018-1017-7. PMC 5830330. PMID 29490655.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ "Adaptive designs for clinical trials of drugs and biologics: Guidance for industry" (PDF). U.S. Food and Drug Administration (FDA). 1 November 2019. Archived from the original on 13 December 2019. Retrieved 3 April 2020.
- ^ "An international randomised trial of candidate vaccines against COVID-19: Outline of Solidarity vaccine trial" (PDF). World Health Organization (WHO). 9 April 2020. Archived (PDF) from the original on 12 May 2020. Retrieved 9 May 2020.
- ^ "An Open Study of the Safety, Tolerability and Immunogenicity of the Drug "Gam-COVID-Vac" Vaccine Against COVID-19". ClinicalTrials.gov. United States National Library of Medicine. 17 June 2020. NCT04436471. Retrieved 5 March 2021.
- ^ Jones I, Roy P (February 2021). "Sputnik V COVID-19 vaccine candidate appears safe and effective". Lancet. 397 (10275): 642–643. doi:10.1016/S0140-6736(21)00191-4. PMC 7906719. PMID 33545098.
- ^ Sagdiev R, Ivanova P (16 November 2020). "Russia focuses on freeze-dried vaccine doses as transport fix". Reuters. Moscow. Retrieved 5 March 2021.
- ^ "Clinical Trial of Efficacy, Safety, and Immunogenicity of Gam-COVID-Vac Vaccine Against COVID-19". ClinicalTrials.gov. Archived from the original on 12 September 2020. Retrieved 11 September 2020.
- ^ "Clinical Trial of Efficacy, Safety, and Immunogenicity of Gam-COVID-Vac Vaccine Against COVID-19 in Belarus". ClinicalTrials.gov. Health Ministry of the Russian Federation. 25 September 2020. Retrieved 18 January 2021.
- ^ Kumar S (1 December 2020). "Sputnik-V from Russia arrives in India for clinal trials". Hindustan Times.
- ^ "Clinical trial: 17 volunteers given Russia's Sputnik V Covid-19 vaccine in Pune". The Indian Express. 6 December 2020.
- ^ "Clinical Trial of the Immunogenicity, Safety, and Efficacy of the Gam-COVID-Vac Vaccine Against COVID-19 in Venezuela". ClinicalTrials.gov. Health Ministry of the Russian Federation. 24 November 2020. Retrieved 18 January 2021.
- ^ "Clinical Trial of the Immunogenicity, Safety, and Efficacy of the Gam-COVID-Vac Vaccine Against COVID-19 in Venezuela". ClinicalTrials.gov. Health Ministry of the Russian Federation. 24 November 2020. Retrieved 18 January 2021.
- ^ "UAE begins trials of Russia's Sputnik V Covid-19 vaccine". Clinical Trials Arena. 8 January 2021.
- ^ "Vaxzevria (previously COVID-19 Vaccine AstraZeneca) EPAR". European Medicines Agency (EMA).
- ^ "AstraZeneca & Serum Institute of India sign licensing deal for 1 million doses of Oxford vaccine". The Economic Times. Retrieved 15 June 2020.
- ^ "Covid-19 vaccine: Serum Institute signs up for 100 million doses of vaccines for India, low and middle-income countries". The Financial Express. 7 August 2020.
- ^ Walsh N, Shelley J, Duwe E, Bonnett W (27 July 2020). "The world's hopes for a coronavirus vaccine may run in these health care workers' veins". São Paulo: CNN. Archived from the original on 3 August 2020. Retrieved 3 August 2020.
- ^ Gallagher J, Triggle N (30 December 2020). "Covid-19: Oxford-AstraZeneca vaccine approved for use in UK". BBC. Retrieved 5 March 2020.
- ^ AstraZeneca COVID-19 Vaccine (PDF) (Product Monograph). AstraZeneca. 26 February 2021. 244627. Retrieved 5 March 2021.
- ^ "A Phase III Randomized, Double-blind, Placebo-controlled Multicenter Study in Adults to Determine the Safety, Efficacy, and Immunogenicity of AZD1222, a Non-replicating ChAdOx1 Vector Vaccine, for the Prevention of COVID-19". ClinicalTrials.gov. United States National Library of Medicine. 12 May 2020. NCT04383574. Archived from the original on 23 August 2020. Retrieved 26 August 2020.
- ^ "Trial of Oxford COVID-19 vaccine starts in Brazil". Jenner Institute. Archived from the original on 9 September 2020. Retrieved 26 August 2020.
- ^ "Oxford COVID-19 vaccine final trials will be held in these 17 hospitals in India". mint. 19 August 2020.
- ^ Farge E, Revill J (5 January 2021). "WHO recommends two doses of Pfizer COVID-19 vaccine within 21–28 days". Reuters. Geneva. Retrieved 5 March 2021.
- ^ Keaten J (8 January 2021). "WHO: Amid short supplies, vaccine doses can be 6 weeks apart". Associated Press. Geneva. Retrieved 6 March 2021.
- ^ "COVID vaccine: Moderna shots can be 6 weeks apart, WHO says". Deutsche Welle. 26 January 2021. Retrieved 6 March 2021.
- ^ "Coronavirus (COVID-19) Update: FDA Allows More Flexible Storage, Transportation Conditions for Pfizer-BioNTech COVID-19 Vaccine" (Press release). Food and Drug Administration (FDA). 25 February 2021. Retrieved 5 March 2021.
- ^ "Pfizer-BioNTech COVID-19 Vaccine EUA Fact Sheet for Healthcare Providers" (PDF). Pfizer. 25 February 2021. Retrieved 25 February 2021.
- ^ "Pfizer and BioNTech Conclude Phase 3 Study of COVID-19 Vaccine Candidate, Meeting All Primary Efficacy Endpoints" (Press release). Pfizer. 18 November 2020.
- ^ Polack FP, Thomas SJ, Kitchin N, Absalon J, Gurtman A, Lockhart S, et al. (December 2020). "Safety and Efficacy of the BNT162b2 mRNA Covid-19 Vaccine". The New England Journal of Medicine. 383 (27): 2603–2615. doi:10.1056/NEJMoa2034577. PMC 7745181. PMID 33301246.
- ^ FDA Review of Efficacy and Safety of Pfizer-BioNTech COVID-19 Vaccine Emergency Use Authorization Request (PDF). U.S. Food and Drug Administration (FDA) (Report). 10 December 2020. Retrieved 11 December 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ Erman M (18 November 2020). "Pfizer ends COVID-19 trial with 95% efficacy, to seek emergency-use authorization". Reuters. Retrieved 18 November 2020.
- ^ Xia S, Zhang Y, Wang Y, Wang H, Yang Y, Gao GF, et al. (January 2021). "Safety and immunogenicity of an inactivated SARS-CoV-2 vaccine, BBIBP-CorV: a randomised, double-blind, placebo-controlled, phase 1/2 trial". The Lancet. Infectious Diseases. 21 (1): 39–51. doi:10.1016/S1473-3099(20)30831-8. PMC 7561304. PMID 33069281.
- ^ Elbahrawy F, Lyu D, Omar A, Che C, Paton J (9 December 2020). "China State-Backed Covid Vaccine Has 86% Efficacy, UAE Says". Bloomberg News. Retrieved 5 March 2020.
CNBG's vaccine can be transported and stored at normal refrigerated temperatures.
- ^ Wee SL, Qin A (30 December 2020). "A Chinese Covid-19 Vaccine Has Proved Effective, Its Maker Says". The New York Times. Retrieved 30 December 2020.
- ^ Yang Y. "A Study to Evaluate The Efficacy, Safety and Immunogenicity of Inactivated SARS-CoV-2 Vaccines (Vero Cell) in Healthy Population Aged 18 Years Old and Above". ClinicalTrials.gov. Archived from the original on 14 September 2020. Retrieved 15 September 2020.
- ^ "Clinical Trial to Evaluate the Efficacy, Immunogenicity and Safety of the Inactivated SARS-CoV-2 Vaccine (COVID-19)". ClinicalTrials.gov. Retrieved 28 September 2020.
- ^ "A Phase III clinical trial for inactivated novel coronavirus pneumonia (COVID-19) vaccine (Vero cells)". chictr.org.cn. Chinese Clinical Trial Register (ChiCTR). Retrieved 15 December 2020.
- ^ "Bahrain allows Sinopharm COVID-19 vaccine candidate use in frontline workers". MSN. Reuters. Retrieved 3 November 2020.
- ^ "Sinovac says COVID-19 vaccine effective in preventing hospitalization, death". Reuters. 5 February 2021. Retrieved 5 March 2021.
- ^ Tan Y (14 January 2021). "Covid: What do we know about China's coronavirus vaccines?". BBC. Retrieved 5 March 2020.
- ^ Daily Sabah with Agencies (25 December 2020). "Turkey set to receive 'effective' COVID-19 vaccine amid calls for inoculation". Daily Sabah. Retrieved 12 February 2021.
- ^ Soeriaatmadja W (11 January 2021). "Indonesia grants emergency use approval to Sinovac's vaccine, local trials show 65% efficacy". The Straits Times. Retrieved 11 January 2021.
- ^ "Sinovac: Brazil results show Chinese vaccine 50.4% effective". BBC News. 13 January 2021. Retrieved 12 February 2021.
- ^ "Tests show coronavirus vaccine by China's Sinovac is safe, says Brazil's Butantan Institute". Archived from the original on 29 October 2020. Retrieved 29 October 2020.
- ^ "Chile initiates clinical study for COVID-19 vaccine". Archived from the original on 11 October 2020. Retrieved 29 October 2020.
- ^ "Randomized, Double-Blind, Placebo-Controlled Phase III Clinical Trial For Evaluation of Efficacy and Safety of SARS-CoV-2 Vaccine (Vero Cell), Inactivated". ClinicalTrials.gov. 8 October 2020. Archived from the original on 20 October 2020. Retrieved 22 October 2020.
- ^ "Safety and Immunogenicity Study of 2019-nCoV Vaccine (mRNA-1273) for Prophylaxis of SARS-CoV-2 Infection (COVID-19)". ClinicalTrials.gov. United States National Library of Medicine. 16 March 2020. NCT04283461. Retrieved 5 March 2021.
- ^ "WHO experts issue recommendations on Moderna COVID-19 vaccine". Reuters. Geneva. 26 January 2021. Retrieved 5 March 2021.
- ^ Fact Sheet for Healthcare Providers Administering Vaccine (Fact sheet). Food and Drug Administration. December 2020. Retrieved 5 March 2021.
- ^ "Promising Interim Results from Clinical Trial of NIH-Moderna COVID-19 Vaccine". National Institutes of Health (NIH). 15 November 2020.
- ^ Baden LR, El Sahly HM, Essink B, Kotloff K, Frey S, Novak R, et al. (February 2021). "Efficacy and Safety of the mRNA-1273 SARS-CoV-2 Vaccine". The New England Journal of Medicine. 384 (5): 403–416. doi:10.1056/NEJMoa2035389. PMC 7787219. PMID 33378609.
- ^ Janssen Ad26.COV2.S Vaccine for the Prevention of COVID-19 (Briefing). Food and Drug Administration. 26 February 2021. p. 6. Retrieved 6 March 2021.
The vaccine, known as Ad26.COV2.S, is a replication-incompetent adenovirus type 26 (Ad26) vectored vaccine encoding a stabilized variant of the SARS-CoV-2 S protein.
- ^ a b Ledford H (January 2021). "J&J's one-shot COVID vaccine offers hope for faster protection". Nature. doi:10.1038/d41586-021-00119-7. PMID 33526898.
- ^ "Johnson & Johnson Announces Single-Shot Janssen COVID-19 Vaccine Candidate Met Primary Endpoints in Interim Analysis of its Phase 3 ENSEMBLE Trial" (Press release). Johnson & Johnson. 29 January 2021. Retrieved 29 January 2021.
- ^ Zhu FC, Guan XH, Li YH, Huang JY, Jiang T, Hou LH, et al. (August 2020). "Immunogenicity and safety of a recombinant adenovirus type-5-vectored COVID-19 vaccine in healthy adults aged 18 years or older: a randomised, double-blind, placebo-controlled, phase 2 trial". Lancet. 396 (10249): 479–488. doi:10.1016/s0140-6736(20)31605-6. PMC 7836858. PMID 32702299.
{{cite journal}}: Unknown parameter|lay-url=ignored (help) - ^ "Clinical Trial of Recombinant Novel Coronavirus Vaccine (Adenovirus Type 5 Vector) Against COVID-19". ClinicalTrials.gov. United States National Library of Medicine. 13 November 2020. NCT04540419. Retrieved 17 November 2020.
- ^ Lazcano P (15 November 2020). "Así funcionan las cuatro vacunas que se probarán en Chile". La Tercera. Retrieved 15 December 2020.
- ^ Martinez AI (3 November 2020). "CanSino Biologics delivers COVID-19 vaccine to Mexico for late-stage trial". Reuters. Retrieved 4 November 2020.
- ^ Ng E (28 October 2020). "China's CanSino trials Covid-19 vaccine in 'high disease burden' nations". South China Morning Post. Retrieved 4 November 2020.
- ^ Nafisa E (9 August 2020). "CanSino to start Phase III trial of COVID-19 vaccine in Saudi". Reuters. Retrieved 4 November 2020.
- ^ Gou J. "Phase III Trial of A COVID-19 Vaccine of Adenovirus Vector in Adults 18 Years Old and Above". ClinicalTrials.gov. Archived from the original on 18 September 2020. Retrieved 17 September 2020.
- ^ "Whole-Virion Inactivated SARS-CoV-2 Vaccine (BBV152) for COVID-19 in Healthy Volunteers". ClinicalTrials.gov. NCT04471519.
- ^ a b "Covishield and Covaxin: What we know about India's Covid-19 vaccines". BBC. 4 March 2021. Retrieved 5 March 2020.
The two doses are given four weeks apart. The vaccine can be stored at 2C to 8C.
- ^ "An Efficacy and Safety Clinical Trial of an Investigational COVID-19 Vaccine (BBV152) in Adult Volunteers". ClinicalTrials.gov. NCT04641481. Retrieved 26 November 2020.
- ^ "Bharat Biotech Recruits 23,000 Volunteers For Covaxin's Phase 3 Clinical Trial". NDTV.com. 28 December 2020. Retrieved 3 January 2021.
- ^ https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(21)00070-0/fulltext
- ^ "Covaxin showed 81% interim efficacy: Bharat Biotech on Phase 3 results". Business Standard India. 3 March 2021.
- ^ a b c Ryzhikov AB, Ryzhikov EA, Bogryantseva MP, Usova SV, Danilenko ED, Nechaeva EA, Pyankov OV, Pyankova OG, Gudymo AS, Bodnev SA, Onkhonova GS, Sleptsova ES, Kuzubov VI, Ryndyuk NN, Ginko ZI, Petrov VN, Moiseeva AA, Torzhkova PY, Pyankov SA, Tregubchak TV, Antonec DV, Gavrilova EV, Maksyutov RA (2021). "A single blind, placebo-controlled randomized study of the safety, reactogenicity and immunogenicity of the "EpiVacCorona" Vaccine for the prevention of COVID-19, in volunteers aged 18–60 years (phase I–II)". Russian Journal of Infection and Immunity. 11 (2): 283–296. doi:10.15789/2220-7619-ASB-1699.
- ^ Benedyczak J (12 February 2021). Russia's Problems in the Vaccine Race (Bulletin). Polish Institute of International Affairs. Retrieved 6 March 2021.
the Sputnik V and EpiVacCorona can be transported and stored at temperatures of +2 to + 8° C
- ^ "Russian EpiVacCorona Vaccine Has No Adverse Effects". Oreanda News. 13 January 2021.
- ^ a b "A Phase III Clinical Trial to Determine the Safety and Efficacy of ZF2001 for Prevention of COVID-19". ClinicalTrials.gov.
- ^ "China's CAS COVID-19 vaccine induces immune response in mid-stage tests". Reuters. Beijing. 23 December 2020. Retrieved 8 March 2021.
- ^ Pinghui Z (20 November 2020). "Fifth Chinese Covid-19 vaccine candidate ready to enter phase 3 trials". South China Morning Post. Retrieved 26 December 2020.
- ^ Ying TP (7 December 2020). "MYEG to conduct phase 3 clinical trial for China's Covid-19 vaccine in Msia". New Straits Times. Retrieved 28 December 2020.
- ^ "Briefing with Deputy Prime Minister Tatyana Golikova, Health Minister Mikhail Murashko and Head of Rospotrebnadzor Anna Popova". Government of Russia. 18 January 2021. Retrieved 20 February 2021.
- ^ Ryumin A (20 February 2021). "Russia registers its third COVID-19 vaccine CoviVac". TASS. Moscow. Retrieved 6 March 2021.
- ^ a b Ivanova P (8 February 2021). "Russia approves its third COVID-19 vaccine, CoviVac". Reuters. Moscow. Retrieved 5 March 2021.
The CoviVac shot is given in two doses, 14 days apart. It is transported and stored at normal fridge temperatures, of 2 to 8 degrees Celsius (35.6 to 46.4 Fahrenheit), Deputy Prime Minister Tatiana Golikova said in a government briefing in January.
- ^ "COVID-19 vaccine tracker (Choose vaccines tab, apply filters to view select data)". Milken Institute. 8 December 2020. Retrieved 11 December 2020.
{{cite web}}: Unknown parameter|lay-url=ignored (help) - ^ "Draft landscape of COVID 19 candidate vaccines". World Health Organization (WHO). 10 December 2020. Retrieved 11 December 2020.
- ^ "Hope to launch Covovax by September, says Serum Institute CEO". mint. 27 March 2021. Retrieved 28 March 2021.
- ^ Wadman M (November 2020). "The long shot". Science. 370 (6517): 649–653. Bibcode:2020Sci...370..649W. doi:10.1126/science.370.6517.649. PMID 33154120.
- ^ Wadman M (28 December 2020). "Novavax launches pivotal U.S. trial of dark horse COVID-19 vaccine after manufacturing delays". Science. doi:10.1126/science.abg3441.
- ^ Parekh N (24 July 2020). "Novavax: A SARS-CoV-2 Protein Factory to Beat COVID-19". Archived from the original on 22 November 2020. Retrieved 24 July 2020.
- ^ Chung YH, Beiss V, Fiering SN, Steinmetz NF (October 2020). "COVID-19 Vaccine Frontrunners and Their Nanotechnology Design". ACS Nano. 14 (10): 12522–12537. doi:10.1021/acsnano.0c07197. PMC 7553041. PMID 33034449.
- ^ Moitra P, Alafeef M, Dighe K, Frieman MB, Pan D (June 2020). "Selective Naked-Eye Detection of SARS-CoV-2 Mediated by N Gene Targeted Antisense Oligonucleotide Capped Plasmonic Nanoparticles". ACS Nano. 14 (6): 7617–7627. doi:10.1021/acsanm.0c01978. PMC 7482545.
- ^ "A Study Looking at the Effectiveness, Immune Response, and Safety of a COVID-19 Vaccine in Adults in the United Kingdom". ClinicalTrials.gov. Retrieved 22 November 2020.
- ^ "A Study Looking at the Efficacy, Immune Response, and Safety of a COVID-19 Vaccine in Adults at Risk for SARS-CoV-2". ClinicalTrials.gov. Retrieved 30 December 2020.
- ^ "Covovax trials begin in India, launch hopefully in September: Adar Poonawalla". India Today. 27 March 2021. Retrieved 28 March 2021.
- ^ Keech C, Albert G, Cho I, Robertson A, Reed P, Neal S, et al. (December 2020). "Phase 1-2 Trial of a SARS-CoV-2 Recombinant Spike Protein Nanoparticle Vaccine". The New England Journal of Medicine. 383 (24): 2320–2332. doi:10.1056/NEJMoa2026920. PMC 7494251. PMID 32877576.
- ^ https://www.bloomberg.com/news/articles/2021-02-02/trudeau-signs-deal-to-make-novavax-covid-19-vaccine-in-canada
- ^ "EMA starts rolling review of Novavax's COVID-19 vaccine (NVX-CoV2373)". European Medicines Agency (EMA) (Press release). 1 December 2020. Retrieved 12 February 2021.
- ^ "Ukraine secures 12 million AstraZeneca, Novavax COVID-19 vaccine doses". Reuters. 5 February 2021. Retrieved 24 February 2021.
- ^ "COVID-19: Ukraine set to launch coronavirus vaccination programme". euronews. 8 February 2021. Retrieved 24 February 2021.
- ^ https://www.nbcchicago.com/news/coronavirus/astrazeneca-and-novavax-covid-vaccines-what-we-know-so-far/2460531/
- ^ https://www.cityam.com/uk-secures-deal-to-bottle-60m-novavax-vaccine-doses-in-the-north-east/
- ^ https://www.raps.org/news-and-articles/news-articles/2021/1/novavax-covid-vaccine-takes-first-step-toward-aust
- ^ https://www.biopharma-reporter.com/Article/2020/12/17/New-Zealand-secures-COVID-19-vaccines-from-Novavax-and-AstraZeneca
- ^ "COVID-19". CureVac. Retrieved 21 December 2020.
- ^ "COVID-19: A Phase 2b/3, Randomized, Observer-Blinded, Placebo Controlled, Multicenter Clinical Study Evaluating the Efficacy and Safety of Investigational SARS-CoV-2 mRNA Vaccine CVnCoV in Adults 18 Years of Age and Older". EU Clinical Trials Register. 19 November 2020. 2020-003998-22. Retrieved 19 December 2020.
- ^ "A Study to Evaluate the Safety and Immunogenicity of Vaccine CVnCoV in Healthy Adults in Germany for COVID-19". clinicaltrials.gov. United States National Library of Medicine. Retrieved 23 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "A Study to Evaluate the Safety, Reactogenicity and Immunogenicity of Vaccine CVnCoV in Healthy Adults". ClinicalTrials.gov. 26 June 2020. NCT04449276. Archived from the original on 11 October 2020. Retrieved 14 July 2020.
- ^ "A Dose-Confirmation Study to Evaluate the Safety, Reactogenicity and Immunogenicity of Vaccine CVnCoV in Healthy Adults". ClinicalTrials.gov. 17 August 2020. NCT04515147. Archived from the original on 23 August 2020. Retrieved 28 August 2020.
- ^ "ABDALA Clinical Study - Phase III". rpcec.sld.cu. Registro Público Cubano de Ensayos Clínicos. Retrieved 22 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "ABDALA Clinical Study". rpcec.sld.cu. Registro Público Cubano de Ensayos Clínicos. Retrieved 21 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ Held S (4 March 2021). "Cuba's Soberana 02 SARS-CoV-2 vaccine candidate moves to phase III trials". Bioworld. Retrieved 10 March 2021.
- ^ "SOBERANA 02-FaseIII". Registro Público Cubano de Ensayos Clínicos. RPCEC00000354.
- ^ "SOBERANA 02". Registro Público Cubano de Ensayos Clínicos. 27 October 2020. Retrieved 22 January 2021.
- ^ "SOBERANA 02A". Registro Público Cubano de Ensayos Clínicos. 17 December 2020. Retrieved 22 January 2021.
- ^ https://www.bmj.com/content/372/bmj.n171/rr-0
- ^ "Study of Recombinant Protein Vaccine with Adjuvant against COVID-19 in Adults 18 Years of Age and Older". pactr.samrc.ac.za. Pan African Clinical Trials Registry. Retrieved 24 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "Study of Recombinant Protein Vaccine Formulations Against COVID-19 in Healthy Adults 18 Years of Age and Older". clinicaltrials.gov. United States National Library of Medicine. Retrieved 11 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "Study of Recombinant Protein Vaccine With Adjuvant Against COVID-19 in Adults 18 Years of Age and Older (VAT00002)". clinicaltrials.gov. United States National Library of Medicine. Retrieved 11 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ https://www.gsk.com/en-gb/media/press-releases/sanofi-and-gsk-confirm-agreement-with-european-union-to-supply-up-to-300-million-doses-of-adjuvanted-covid-19-vaccine/
- ^ https://www.gsk.com/en-gb/media/press-releases/sanofi-and-gsk-sign-agreements-with-the-government-of-canada-to-supply-up-to-72-million-doses-of-adjuvanted-covid-19-vaccine/
- ^ https://www.bloomberg.com/news/articles/2020-05-13/u-s-to-get-sanofi-covid-vaccine-first-if-it-succeeds-ceo-says
- ^ https://www.bbc.com/news/business-53577637
- ^ "Safety and Immunogenicity Study of an Inactivated SARS-CoV-2 Vaccine for Preventing Against COVID-19". ClinicalTrials.gov. United States National Library of Medicine. 2 June 2020. NCT04412538. Archived from the original on 11 October 2020. Retrieved 14 July 2020.
- ^ "The Efficacy, Safety and Immunogenicity Study of Inactivated SARS-CoV-2 Vaccine for Preventing Against COVID-19". ClinicalTrials.gov. United States National Library of Medicine. NCT04659239. Retrieved 10 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ Yergaliyeva A (20 December 2020). "Kazakhstan Begins Vaccinating 3,000 Volunteers With Self-Made QazCovid-in". The Astana Times. Retrieved 2 March 2021.
- ^ a b "Immunogenicity, Efficacy and Safety of QazCovid-in® COVID-19 Vaccine - Full Text View - ClinicalTrials.gov". clinicaltrials.gov.
- ^ "Reactogenicity, Safety and Immunogenicity of QazCovid-in® COVID-19 Vaccine - Full Text View - ClinicalTrials.gov". clinicaltrials.gov.
- ^ "Coronavirus | Zydus Cadila gets DCGI nod to initiate Phase-3 clinical trials for COVID-19 vaccine". The Hindu. 3 January 2021.
- ^ a b Thacker T. "Zydus Cadila to test ZyCoV-D on 30,000 patients in Phase-3 trials". The Economic Times. Retrieved 16 December 2020.
- ^ "DBT-BIRAC supported indigenously developed DNA Vaccine Candidate by Zydus Cadila, approved for Phase III clinical trials" (Press release). Press Information Bureau. 3 January 2021.
- ^ Rawat K, Kumari P, Saha L (February 2021). "COVID-19 vaccine: A recent update in pipeline vaccines, their design and development strategies". European Journal of Pharmacology. 892: 173751. doi:10.1016/j.ejphar.2020.173751. PMC 7685956. PMID 33245898.
- ^ "GSK, Medicago launch phase 2/3 clinical trials of plant-derived COVID-19 vaccine". PMLive. 13 November 2020. Retrieved 16 November 2020.
- ^ Chander V (14 July 2020). "Canada's Medicago begins human trials of plant-based COVID-19 vaccine". National Post. Reuters. Archived from the original on 1 November 2020. Retrieved 14 July 2020.
- ^ Medicago (18 November 2020). "Randomized, Observer-Blind, Placebo-Controlled, Phase 2/3 Study to Assess the Safety, Efficacy, and Immunogenicity of a Recombinant Coronavirus-Like Particle COVID-19 Vaccine in Adults 18 Years of Age or Older". Clinical Trials. Retrieved 26 November 2020.
- ^ "Safety, Tolerability and Immunogenicinity of a Coronavirus-Like Particle COVID-19 Vaccine in Adults Aged 18-55 Years". clinicaltrials.gov. United States National Library of Medicine. Retrieved 17 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ https://www.medicago.com/en/media-room/medicago-signs-agreements-with-the-government-of-canada-to-supply-up-to-76-million-doses-of-its-recombinant-plant-derived-covid-19-vaccine/
- ^ "SCB-2019 as COVID-19 Vaccine". ClinicalTrials.gov. United States National Library of Medicine. 28 May 2020. NCT04405908. Archived from the original on 11 October 2020. Retrieved 14 July 2020.
- ^ "Clover Biopharmaceuticals starts Phase I Covid-19 vaccine trial". Clinical Trials Arena. 20 June 2020. Archived from the original on 11 October 2020. Retrieved 25 June 2020.
- ^ "About Us". Clover Biopharmaceuticals. Archived from the original on 11 October 2020. Retrieved 1 August 2020.
- ^ "A Controlled Phase 2/3 Study of Adjuvanted Recombinant SARS-CoV-2 Trimeric S-protein Vaccine (SCB-2019) for the Prevention of COVID-19 (SCB-2019)". United States National Library of Medicine. NCT04672395. Retrieved 10 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "COVIran Barakat: Iran launches human trials of its COVID vaccine". aljazeera. 29 December 2019.
- ^ "A double-blind, randomized, placebo-controlled Phase II/III Clinical trial to evaluate the safety and efficacy of COVID-19 inactivated vaccine (Shifa-Pharmed) in a population aged 18 to 75 years". Iranian Registry of Clinical Trials. Retrieved 27 March 2021.
- ^ "A double-blinded, randomized, placebo-controlled Phase I Clinical trial to evaluate the safety and immunogenicity of COVID-19 inactivated vaccine (Shif-Pharmed) in a healthy population". Iranian Registry of Clinical Trials. Retrieved 20 March 2021.
- ^ "A Study to Evaluate UB-612 COVID-19 Vaccine in Adolescent, Younger and Elderly Adult Volunteers". clinicaltrials.gov. United States National Library of Medicine. Retrieved 20 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "A Study to Evaluate the Safety, Immunogenicity, and Efficacy of UB-612 COVID-19 Vaccine". clinicaltrials.gov. United States National Library of Medicine. Retrieved 20 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "A Study to Evaluate the Safety, Tolerability, and Immunogenicity of UB-612 COVID-19 Vaccine". clinicaltrials.gov. United States National Library of Medicine. Retrieved 20 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "GRAd-COV2 Vaccine Against COVID-19". ClinicalTrials.gov. United States National Library of Medicine. 7 January 2021. NCT04528641.
- ^ "ReiThera Announces its GRAd-COV2 COVID-19 Vaccine Candidate is Well Tolerated and Induces Clear Immune Responses in Healthy Subjects Aged 18–55 Years". ReiThera Srl. Yahoo! Finance. 24 November 2020. Retrieved 12 January 2021.
- ^ "Study of GRAd-COV2 for the Prevention of COVID-19 in Adults (COVITAR)". clinicaltrials.gov. United States National Library of Medicine. Retrieved 20 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "REITHERA'S COVID-19 VACCINE CANDIDATE ENTERS PHASE 2/3 CLINICAL STUDY". Reithera. 18 March 2021. Retrieved 20 March 2021.
- ^ "New ReiThera vaccine safe, response peak at 4 wks". ANSA. 5 January 2021.
- ^ "A Phase Ⅱ Clinical Trial of Recombinant Corona Virus Disease-19 (COVID-19) Vaccine (Sf9 Cells)". clinicaltrials.gov. United States National Library of Medicine. Retrieved 20 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "Phase IIb Clinical Trial of Recombinant Novel Coronavirus Pneumonia (COVID-19) Vaccine (Sf9 Cells)". clinicaltrials.gov. United States National Library of Medicine. Retrieved 20 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "Phase I Trial of a Recombinant SARS-CoV-2 Vaccine (Sf9 Cell)". clinicaltrials.gov. United States National Library of Medicine. Retrieved 20 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "A Study to Evaluate MVC-COV1901 Vaccine Against COVID-19 in Adult (COVID-19)". clinicaltrials.gov. United States National Library of Medicine. Retrieved 11 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "A Study to Evaluate the Safety and Immunogenicity of MVC-COV1901 Against COVID-19". clinicaltrials.gov. United States National Library of Medicine. Retrieved 11 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "A Study to Evaluate Safety and Immunogenicity of Inactivated SARS-CoV-2 Vaccine (Vero Cells) in Healthy Population Aged 18 Years and Above(COVID-19)". clinicaltrials.gov. United States National Library of Medicine. Retrieved 21 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "A Safety and Immunogenicity Study of Inactivated SARS-CoV-2 Vaccine (Vero Cells) in Healthy Population Aged 18 Years and Above(COVID-19)". clinicaltrials.gov. United States National Library of Medicine. Retrieved 21 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "A Phase II Clinical Trial of Influenza virus Vector COVID-19 Vaccine for intranasal Spray (DelNS1-2019-nCoV-RBD-OPT1)". chictr.org.cn. Chinese Clinical Trial Registry. Retrieved 24 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "A Phase I Clinical Trial of Influenza virus Vector COVID-19 Vaccine for intranasal Spray (DelNS1-2019-nCoV-RBD-OPT1)". chictr.org.cn. Chinese Clinical Trial Registry. Retrieved 24 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ a b "VN starts injection of homegrown COVID-19 vaccine in first-stage human trial". Viet Nam News. 17 December 2020.
- ^ "Draft landscape and tracker of COVID-19 candidate vaccines". WHO. 26 February 2021.
- ^ "How much does first Made-in Vietnam COVID-19 vaccine cost?". Voice of Vietnam. 11 December 2020.
- ^ Le C, Thu A (26 February 2021). "Vietnam enters second phase of Covid-19 vaccine trials". VnExpress.
- ^ "A Phase I clinical trial to evaluate the safety, tolerance and preliminary immunogenicity of different doses of a SARS-CoV-2 mRNA vaccine in population aged 18–59 years and 60 years and above". Chinese Clinical Trial Register. 24 June 2020. ChiCTR2000034112. Archived from the original on 11 October 2020. Retrieved 6 July 2020.
- ^ "Company introduction". Walvax Biotechnology. Archived from the original on 11 October 2020. Retrieved 1 August 2020.
- ^ "A Phase II clinical trial to evaluate the immunogenicity and safety of different doses of a novel coronavirus pneumonia (COVID-19) mRNA vaccine in population aged 18-59 years". chictr.org.cn. Chinese Clinical Trial Registry. Retrieved 20 March 2020.
- ^ "Safety, Immunogenicity, and Efficacy of INO-4800 for COVID-19 in Healthy Seronegative Adults at High Risk of SARS-CoV-2 Exposure". clinicaltrials.gov. United States National Library of Medicine. Retrieved 12 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "A Phase II, Randomized, Double-Blinded, Placebo-Controlled, Dose-Finding Clinical Trial to Evaluate the Safety and Immunogenicity of Different Doses of COVID-19 DNA Vaccine INO-4800 Administered Intradermally Followed by Electroporation in Healthy Adult and Elderly Volunteers". chictr.org.cn. Chinese Clinical Trial Registry. Retrieved 27 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "Safety, Tolerability and Immunogenicity of INO-4800 Followed by Electroporation in Healthy Volunteers for COVID19". clinicaltrials.gov. United States National Library of Medincine. Retrieved 12 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "Study of COVID-19 DNA Vaccine (AG0302-COVID19)". clinicaltrials.gov. United States National Library of Medicine. Retrieved 11 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "About AnGes – Introduction". AnGes, Inc. Archived from the original on 11 October 2020. Retrieved 1 August 2020.
- ^ "Phase II / III Study of COVID-19 DNA Vaccine (AG0302-COVID19)". clinicaltrials.gov. United States National Library of Medicine. Retrieved 11 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "As Israel goes vaccine-wild, will the homegrown version lose its shot?". The Times of Israel. 29 December 2020. Retrieved 1 January 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "CTI and Arcturus Therapeutics Announce Initiation of Dosing of COVID-19 STARR™ mRNA Vaccine Candidate, LUNAR-COV19 (ARCT-021) in a Phase 1/2 study". UK BioIndustry Association. 13 August 2020. Archived from the original on 11 October 2020. Retrieved 23 August 2020.
- ^ "Ascending Dose Study of Investigational SARS-CoV-2 Vaccine ARCT-021 in Healthy Adult Subjects". clinicaltrials.gov. Archived from the original on 11 October 2020. Retrieved 23 August 2020.
- ^ "Open Label Extension Study to Assess the Safety and Long-Term Immunogenicity of ARCT-021". clinicaltrials.gov. United States National Library of Medicine. Retrieved 13 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "A Trial Evaluating the Safety and Effects of an RNA Vaccine ARCT-021 in Healthy Adults". clinicaltrials.gov. United States National Library of Medicine. Retrieved 10 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "VBI Vaccines Announces Initiation of Enrollment in Adaptive Phase 1/2 Study of Prophylactic COVID-19 Vaccine Candidate, VBI-2902". VBI Vaccines. 9 March 2021. Retrieved 22 March 2021.
- ^ "Safety, Tolerability, and Immunogenicity of the COVID-19 Vaccine Candidate (VBI-2902a)". clinicaltrials.gov. United States National Library of Medicine. Retrieved 15 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "Sanofi and Translate Bio initiate Phase 1/2 clinical trial of mRNA COVID-19 vaccine candidate". Sanofi. 12 March 2021. Retrieved 20 March 2021.
- ^ "Study of mRNA Vaccine Formulation Against COVID-19 in Healthy Adults 18 Years of Age and Older (VAW00001)". United States National Library of Medicine. Retrieved 20 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "Safety, Tolerance and Immunogenicity of EuCorVac-19 for the Prevention of COVID-19 in Healthy Adults". clinicaltrials.gov. United States National Library of Medicine. Retrieved 20 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "Trial registered on ANZCTR". anzctr.org.au. Australian New Zealand Clinical Trials Registry. Retrieved 24 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "Safety and Immunogenicity Study of GX-19N, a COVID-19 Preventive DNA Vaccine in Healthy Adults". clinicaltrials.gov. United States National Library of Medicine. Retrieved 16 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "Genexine consortium's Covid-19 vaccine acquires approval for clinical trails in Korea". 11 June 2020. Retrieved 1 August 2020.
- ^ "Phase I-II Trial of Dendritic Cell Vaccine to Prevent COVID-19 in Adults". United States National Library of Medicine. Retrieved 23 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "Dendritic Cell Vaccine to Prevent COVID-19". United States National Library of Medicine. Retrieved 23 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "Start of a Japanese Clinical Study of TAK-919, Moderna's COVID-19 Vaccine Candidate". Takeda. 21 January 2021. Retrieved 11 March 2021.
- ^ "A Study of TAK-919 in Healthy Japanese Adults (COVID-19)". United States National Library of Medicine. Retrieved 11 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "Takeda Provides Updates on Phase 1/2 Clinical Trials of Novavax' and Moderna's COVID-19 Vaccine Candidates in Japan". Takeda. 24 February 2021. Retrieved 11 March 2021.
- ^ "A Study of TAK-019 in Healthy Japanese Adults (COVID-19)". United States National Library of Medicine. Retrieved 10 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "Safety and Immunogenicity of COVID-eVax, a Candidate Plasmid DNA Vaccine for COVID-19, in Healthy Adult Volunteers". United States National Library of Medicine. Retrieved 21 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "ChulaCov19 mRNA Vaccine in Healthy Adults". United States National Library of Medicine. Retrieved 21 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ a b "About Us". Shenzhen Genoimmune Medical Institute. Archived from the original on 11 October 2020. Retrieved 1 August 2020.
- ^ "COVID-19 Vaccination Using a 2nd Generation (E1/E2B/E3-Deleted) Adenoviral Platform in Healthy South African Adults". United States National Library of Medicine. Retrieved 23 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "COVID-19 Oral and Subcutaneous Vaccination Using a 2nd Generation (E1/E2B/E3-Deleted) Adenovirus Platform in Healthy Volunteers in USA". United States National Library of Medicine. Retrieved 23 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "COVID-19 Vaccination Using a 2nd Generation (E1/E2B/E3-Deleted) Adenoviral-COVID-19 in Normal Healthy Volunteers". United States National Library of Medicine. Retrieved 23 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "Monovalent Recombinant COVID19 Vaccine (COVAX19)". ClinicalTrials.gov. United States National Library of Medicine. 1 July 2020. NCT04453852. Archived from the original on 11 October 2020. Retrieved 14 July 2020.
- ^ "Vaxine". Archived from the original on 11 October 2020. Retrieved 1 August 2020.
- ^ "Indigenous mRNA vaccine candidate supported by DBT gets Drug Controller nod to initiate Human clinical trials" (Press release). Press Information Bureau. Retrieved 13 January 2021.
- ^ "mRNA Vaccines – HGC019". Gennova Biopharmaceuticals Limited. Retrieved 13 January 2021.
- ^ Raghavan P (15 December 2020). "Pune-based Gennova to begin human trials of its Covid vaccine 'soon'". The Indian Express.
- ^ "A prospective open label randomised phase-I seamlessly followed by phase-II study to assess the safety, reactogenicity and immunogenicity of Biological E's novel Covid-19 vaccine containing Receptor Binding Domain of SARS-CoV-2 for protection against Covid-19 disease when administered intramuscularly in a two dose schedule (0, 28D) to healthy volunteers". ctri.nic.in. Clinical Trials Registry India. 13 January 2021. CTRI/2020/11/029032. Archived from the original on 12 November 2020.
- ^ "CEPI partners with Biological E Limited to advance development and manufacture of COVID-19 vaccine candidate". cepi.net. CEPI. Retrieved 5 March 2021.
- ^ Chui M (16 November 2020). "Biological E. Limited and Baylor COVID-19 vaccine begins clinical trial in India". Baylor College of Medicine.
- ^ Leo L (16 November 2020). "Biological E initiates human trials of vaccine". Mint.
- ^ a b "Bangavax Vaccine: Permission sought for clinical trial". The Daily Star. 18 January 2021.
- ^ "Bangladesh joins global COVID-19 vaccine race with Bongavax set for clinical trial". arabnews.com. Arab News. 8 January 2021.
- ^ "Globe Biotech applies for approval to run clinical trial of COVID vaccine". bdnews24.com. Bdnews24.com. 17 January 2021.
- ^ "Globe Biotech seeks approval for vaccine trials". New Age. 17 January 2021.
- ^ a b "Made-in-Canada coronavirus vaccine starts human clinical trials". Canadian Broadcasting Corporation. 26 January 2021.
- ^ a b "VIDO COVID-19 vaccine moves to Phase 1 clinical testing". globalnews.ca. 10 February 2021.
- ^ "Safety and Immunogenicity of COVI-VAC, a Live Attenuated Vaccine Against COVID-19". clinicaltrials.gov. United States National Library of Medicine.
{{cite web}}: CS1 maint: url-status (link) - ^ "A Study of the Safety of and Immune Response to Varying Doses of a Vaccine Against COVID-19 in Healthy Adults". clinicaltrials.gov. United States National Library of Medicine.
{{cite web}}: CS1 maint: url-status (link) - ^ "The Safety and Immunogenicity of a DNA-based Vaccine (COVIGEN) in Healthy Volunteers (COVALIA)". clinicaltrials.gov. United States National Library of Medicine.
{{cite web}}: CS1 maint: url-status (link) - ^ a b "Safety and Immunogenicity of an Intranasal SARS-CoV-2 Vaccine (BBV154) for COVID-19". ClinicalTrials.gov. United States National Library of Medicine. 5 February 2021. NCT04751682. Archived from the original on 24 February 2021. Retrieved 5 February 2021.
- ^ "Intranasal Vaccine For Covid-19 | Bharat Biotech". www.bharatbiotech.com. Retrieved 5 March 2021.
- ^ "Meissa Announces IND Clearance for Phase 1 Study of Intranasal Live Attenuated Vaccine Candidate for COVID-19". Business Wire. 16 March 2021. Retrieved 20 March 2021.
- ^ "Safety and Immunogenicity of an Intranasal RSV Vaccine Expressing SARS-CoV-2 Spike Protein (COVID-19 Vaccine) in Adults". clinicaltrials.gov. United States National Library of Medicine. Retrieved 20 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "Safety and Immunogenicity of an Intranasal RSV Vaccine Expressing SARS-CoV-2 Spike Protein (COVID-19 Vaccine) in Adults". jrct.niph.go.jp. Japan Registry of Clinical Trials. Retrieved 21 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "Safety and Immunogenicity Study of SARS-CoV-2 Nanoparticle Vaccine (GBP510) Adjuvanted With or Without AS03 (COVID-19)". clinicaltrials.gov. United States National Library of Medicine. Retrieved 21 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "KBP-201 COVID-19 Vaccine Trial in Healthy Volunteers". clinicaltrials.gov. United States National Library of Medicine. Retrieved 21 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "A Study to Evaluate the Safety and Immunogenicity of COVID-19 (AdimrSC-2f) Vaccine". clinicaltrials.gov. United States National Library of Medicine. Retrieved 21 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "Safety and Immunogenicity of Two Different Strengths of the Inactivated COVID-19 Vaccine ERUCOV-VAC (ERUCOV-VAC)". clinicaltrials.gov. United States National Library of Medicine. Retrieved 21 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "Anti-COVID19 AKS-452 - ACT Study (ACT)". clinicaltrials.gov. United States National Library of Medicine. Retrieved 21 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "GLS-5310 Vaccine for the Prevention of SARS-CoV-2 (COVID-19)". clinicaltrials.gov. United States National Library of Medicine. Retrieved 21 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "A Clinical Trial of a Plasmid DNA Vaccine for COVID-19 [Covigenix VAX-001] in Adults". clinicaltrials.gov. United States National Library of Medicine. Retrieved 21 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "A Synthetic MVA-based SARS-CoV-2 Vaccine, COH04S1, for the Prevention of COVID-19". clinicaltrials.gov. United States National Library of Medicine. Retrieved 21 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "Phase 1, safety, immunogenicity and dose finding for two strengths of 0.5 × 10^6 and 2.5 × 10^6 (TCID50) inactivated SARS-CoV-2 vaccine FAKHRAVAC (MIVAC) injected in two schedules of two doses, 2 and 3 weeks apart in healthy adults aged 18-55 years: a randomized, double blind, placebo controlled, clinical trial". en.irct.ir. Iran Registry of Clinical Trials. Retrieved 21 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "Safety and Immunogenicity of a SARS-CoV-2 Vaccine (NBP2001) in Healthy Adults (COVID-19)". clinicaltrials.gov. United States National Library of Medicine. Retrieved 21 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "Safety and Immunogenicity Trial of Multi-peptide Vaccination to Prevent COVID-19 Infection in Adults (pVAC)". clinicaltrials.gov. United States National Library of Medicine. Retrieved 21 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "Evaluating the Safety, Tolerability and Immunogenicity of bacTRL-Spike Vaccine for Prevention of COVID-19". clinicaltrials.gov. United States National Library of Medicine. Retrieved 21 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "Phase I, Safety and Immunogenicity of Razi SARS-CoV-2 recombinant Spike protein vaccine (Razi Cov Pars), in healthy adults aged 18-55 years; parallel 4 arms design (adjuvant only and three vaccine doses of 5, 10, and 20 µg/200µl); a Randomised, double blind, clinical trial". irct.ir. Iranian Registry of Clinical Trials. Retrieved 21 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "CORVax12: SARS-CoV-2 Spike (S) Protein Plasmid DNA Vaccine Trial for COVID-19 (SARS-CoV-2) (CORVax12)". clinicaltrials.gov. United States National Library of Medicine. Retrieved 21 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "Chimpanzee Adenovirus and Self-Amplifying mRNA Prime-Boost Prophylactic Vaccines Against SARS-CoV-2 in Healthy Adults". clinicaltrials.gov. United States National Library of Medicine. Retrieved 22 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "Safety and Immunogenicity of AdCOVID in Healthy Adults (COVID-19 Vaccine Study)". clinicaltrials.gov. United States National Library of Medicine. Retrieved 22 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "Safety and Immunogenicity Trial of an Oral SARS-CoV-2 Vaccine (VXA-CoV2-1) for Prevention of COVID-19 in Healthy Adults". clinicaltrials.gov. United States National Library of Medicine. Retrieved 22 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "Safety and Immunogenicity Study of AdCLD-CoV19: A COVID-19 Preventive Vaccine in Healthy Volunteers". clinicaltrials.gov. United States National Library of Medicine. Retrieved 23 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "SARS-COV-2-Spike-Ferritin-Nanoparticle (SpFN) Vaccine With ALFQ Adjuvant for Prevention of COVID-19 in Healthy Adults". clinicaltrials.gov. United States National Library of Medicine. Retrieved 24 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "Safety, Tolerability and Immunogenicity of the Candidate Vaccine MVA-SARS-2-S Against COVID-19". clinicaltrials.gov. United States National Library of Medicine. Retrieved 24 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ Ward D, McCormack S (22 May 2020). "Clinical trial to assess the safety of a coronavirus vaccine in healthy men and women". ISRCTN. doi:10.1186/ISRCTN17072692. ISRCTN17072692.
- ^ "Clinical Trial to Evaluate the Safety and Immunogenicity of the COVID-19 Vaccine (COVID-19-101)". clinicaltrials.gov. United States National Library of Medicine. Retrieved 23 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "Dose Ranging Trial to Assess Safety and Immunogenicity of V590 (COVID-19 Vaccine) in Healthy Adults (V590-001)". ClinicalTrials.gov. 30 September 2020. Retrieved 26 January 2021.
- ^ "A Study to Assess Safety, Tolerability, and Immunogenicity of V591 (COVID-19 Vaccine) in Healthy Participants (V591-001)". ClinicalTrials.gov. 4 August 2020. Retrieved 26 January 2021.
- ^ "Participant Enrollment Begins for Phase I Trial of IAVI-Merck COVID-19 Vaccine Candidate". IAVI. Retrieved 14 March 2021.
- ^ "V591 SARS-CoV-2 Vaccine". www.precisionvaccinations.com. Retrieved 14 March 2021.
- ^ "Merck Discontinues Development of SARS-CoV-2/COVID-19 Vaccine Candidates; Continues Development of Two Investigational Therapeutic Candidates". Merck (Press release). 25 January 2021. Retrieved 25 January 2021.
- ^ a b c Tregoning JS, Russell RF, Kinnear E (March 2018). "Adjuvanted influenza vaccines". Human Vaccines & Immunotherapeutics. 14 (3): 550–564. doi:10.1080/21645515.2017.1415684. PMC 5861793. PMID 29232151.
- ^ a b c d Wang J, Peng Y, Xu H, Cui Z, Williams RO (August 2020). "The COVID-19 Vaccine Race: Challenges and Opportunities in Vaccine Formulation". AAPS PharmSciTech. 21 (6): 225. doi:10.1208/s12249-020-01744-7. PMC 7405756. PMID 32761294.
- ^ Mathieu, Edouard; Ritchie, Hannah; Rodés-Guirao, Lucas; Appel, Cameron; Giattino, Charlie; Hasell, Joe; Macdonald, Bobbie; Dattani, Saloni; Beltekian, Diana; Ortiz-Ospina, Esteban; Roser, Max (2020–2024). "Coronavirus Pandemic (COVID-19)". Our World in Data. Retrieved 27 October 2024.
- ^ Mathieu E, Ritchie H, Rodés-Guirao L, Appel C, Giattino C, Hasell J, Macdonald B, Dattani S, Beltekian D, Ortiz-Ospina E, Roser M (2020). "Coronavirus Pandemic (COVID-19)". Our World in Data. Retrieved 14 November 2023.
- ^ Mathieu E, Ritchie H, Ortiz-Ospina E, Roser M, Hasell J, Appel C, Giattino C, Rodés-Guirao L (2021). "A global database of COVID-19 vaccinations". Nature Human Behaviour. 5 (7): 947–953. doi:10.1038/s41562-021-01122-8. PMID 33972767.
- ^ Richie H, Ortiz-Ospina E, Beltekian D, Methieu E, Hasell J, Macdonald B, Giattino C, Appel C, Rodes-Guirao L, Roser M (1 September 2021). "Coronavirus (COVID-19) Vaccinations - Statistics and Research". Our World in Data. Archived from the original on 10 March 2021. Retrieved 26 January 2021.
- ^ "Update on WHO Solidarity Trial – Accelerating a safe and effective COVID-19 vaccine". World Health Organization (WHO). 27 April 2020. Archived from the original on 30 April 2020. Retrieved 2 May 2020.
It is vital that we evaluate as many vaccines as possible as we cannot predict how many will turn out to be viable. To increase the chances of success (given the high level of attrition during vaccine development), we must test all candidate vaccines until they fail. The World Health Organization (WHO) is working to ensure that all of them have the chance of being tested at the initial stage of development. The results for the efficacy of each vaccine are expected within three to six months and this evidence, combined with data on safety, will inform decisions about whether it can be used on a wider scale.
- ^ a b Gates B (April 2020). "Responding to Covid-19 - A Once-in-a-Century Pandemic?". The New England Journal of Medicine. 382 (18): 1677–1679. doi:10.1056/nejmp2003762. PMID 32109012.
- ^ Weintraub R, Yadav P, Berkley S (2 April 2020). "A COVID-19 vaccine will need equitable, global distribution". Harvard Business Review. ISSN 0017-8012. Archived from the original on 9 June 2020. Retrieved 9 June 2020.
- ^ a b c Steenhuysen J, Eisler P, Martell A, Nebehay S (27 April 2020). "Special Report: Countries, companies risk billions in race for coronavirus vaccine". Reuters. Archived from the original on 15 May 2020. Retrieved 2 May 2020.
- ^ Gartner A, Roberts L (3 May 2020). "How close are we to a coronavirus vaccine? Latest news on UK trials". The Telegraph. ISSN 0307-1235. Archived from the original on 4 May 2020. Retrieved 3 May 2020.
- ^ "WHO, UN set out steps to meet world COVID vaccination targets". World Health Organization (WHO). 7 October 2021. Archived from the original on 31 December 2021. Retrieved 31 December 2021.
- ^ "COVID-19: WHO calls on countries to vaccinate 70% of their population by mid-2022". 29 December 2021. Archived from the original on 31 December 2021. Retrieved 31 December 2021.
- ^ "Covid-19 vaccinations: African nations miss WHO target". BBC. 31 December 2021. Archived from the original on 31 December 2021. Retrieved 31 December 2021.
- ^ a b Azar A (4 February 2020). "Notice of Declaration under the Public Readiness and Emergency Preparedness Act for medical countermeasures against COVID-19". Archived from the original on 25 April 2020. Retrieved 22 April 2020.
- ^ "Questions and Answers: Conditional Marketing Authorisation of COVID-19 Vaccines in the EU". European Commission. 11 December 2020. Question: What is the difference in liability between EU Conditional Marketing Authorisation vs Emergency Use Authorisations?. Retrieved 29 December 2020.
- ^ Haahr T (7 September 2020). "COVID-19: MEPs want safe vaccines, full transparency and liability for companies". European Parliament. Ms. Gallina stressed negotiations with companies had been difficult but underlined that those companies developing and manufacturing COVID-19 vaccines would indeed be liable according to current laws and if something goes wrong they could be taken to court. This also goes for compensation for hidden defects. Retrieved 29 December 2020.
- ^ "How Pfizer tried to bully Argentina and Brazil in exchange for vaccines". WIONews. 24 February 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "'Held to ransom': Pfizer plays hardball in Covid-19 vaccine negotiations with Latin American countries". STAT news. 23 February 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ So AD, Woo J (December 2020). "Reserving coronavirus disease 2019 vaccines for global access: cross sectional analysis". BMJ. 371: m4750. doi:10.1136/bmj.m4750. PMC 7735431. PMID 33323376.
- ^ Adhanom Ghebreyesus T (18 January 2021). "WHO Director-General's opening remarks at 148th session of the Executive Board". World Health Organization. Retrieved 25 January 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ Holmes O (16 February 2021). "Israel blocked Covid vaccines from entering Gaza, say Palestinians". The Guardian. Retrieved 17 February 2021.
- ^ Rasgon A (4 February 2021). "Israel's Vaccine Success Unleashes a Debate on Palestinian Inequities". The New York Times. Retrieved 17 February 2021.
- ^ Horton C (17 February 2021). "Taiwan Concerned China May Have Blocked Vaccine Purchase". Bloomberg. Retrieved 17 February 2021.
- ^ "Playing Politics with Poverty: Sisi's COVID-19 Vaccine Strategy". Carnegie Endowment for International Peace. Retrieved 25 February 2021.
- ^ Strazewski L (9 February 2021). "Dr. Fauci: Variants reveal COVID-19 vaccination as global job". American Medical Association. Retrieved 4 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ Bergmark E, Wierson A (26 February 2021). "Opinion: Without a global vaccine plan, coronavirus variants could lead to untold number of deaths". CNN. Retrieved 4 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ Lim P (11 March 2021). "Rich countries block push by developing nations to waive COVID vaccine patents rights". www.euractiv.com. Retrieved 13 March 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "Ten health issues WHO will tackle this year". World Health Organization (WHO). 2019. Archived from the original on 11 November 2019. Retrieved 26 May 2020.
- ^ Malik AA, McFadden SM, Elharake J, Omer SB (September 2020). "Determinants of COVID-19 vaccine acceptance in the US". EClinicalMedicine. 26: 100495. doi:10.1016/j.eclinm.2020.100495. PMC 7423333. PMID 32838242.
- ^ "More in U.S. Embrace Covid Vaccines, Pew Poll Shows". The New York Times. 5 March 2021. Retrieved 8 March 2021.
- ^ Funk C (5 March 2021). "Growing Share of Americans Say They Plan To Get a COVID-19 Vaccine – or Already Have" (PDF). Pew Research Center Science & Society. Retrieved 8 March 2021.
{{cite web}}: Unknown parameter|lay-url=ignored (help) - ^ Bekiempis V (21 December 2020). "'I'm ready': Joe Biden receives coronavirus vaccine live on TV". The Guardian. Retrieved 26 December 2020.
- ^ Aratani L (18 December 2020). "Mike Pence receives Covid-19 vaccine on live TV: 'I didn't feel a thing'". The Guardian. Retrieved 26 December 2020.
- ^ Gabbatt A (3 December 2020). "Obama, Clinton and Bush pledge to take Covid vaccine on TV to show its safety". The Guardian. Retrieved 26 December 2020.
- ^ a b c d e f g "COVID-19: Celebrities who have had the coronavirus vaccination". Sky News. Retrieved 31 March 2021.
- ^ a b c "See Amy Schumer, Oprah Winfrey and More Celebs and Politicians Who've Gotten Their COVID-19 Vaccines". PEOPLE.com. Retrieved 31 March 2021.
- ^ "Why are male politicians in love with topless vaccine selfies? | Priya Elan". the Guardian. 12 March 2021. Retrieved 31 March 2021.
- ^ "See Amy Schumer, Oprah Winfrey and More Celebs and Politicians Who've Gotten Their COVID-19 Vaccines". PEOPLE.com. Retrieved 31 March 2021.
- ^ "See Amy Schumer, Oprah Winfrey and More Celebs and Politicians Who've Gotten Their COVID-19 Vaccines". PEOPLE.com. Retrieved 31 March 2021.
- ^ "See Amy Schumer, Oprah Winfrey and More Celebs and Politicians Who've Gotten Their COVID-19 Vaccines". PEOPLE.com. Retrieved 31 March 2021.
- ^ "COVID-19 vaccine: Stars bust myths in video urging people from ethnic minority communities to get the jab". Sky News. Retrieved 31 March 2021.
- ^ "See Amy Schumer, Oprah Winfrey and More Celebs and Politicians Who've Gotten Their COVID-19 Vaccines". PEOPLE.com. Retrieved 31 March 2021.
- ^ "See Amy Schumer, Oprah Winfrey and More Celebs and Politicians Who've Gotten Their COVID-19 Vaccines". PEOPLE.com. Retrieved 31 March 2021.
Further reading
- Funk CD, Laferrière C, Ardakani A (2020). "A Snapshot of the Global Race for Vaccines Targeting SARS-CoV-2 and the COVID-19 Pandemic". Frontiers in Pharmacology. 11: 937. doi:10.3389/fphar.2020.00937. PMC 7317023. PMID 32636754.
- Development and Licensure of Vaccines to Prevent COVID-19: Guidance for Industry (Report). U.S. Food and Drug Administration. June 2020.
- Khandekar, Gauri, Otero-Iglesias Miguel (1 March 2021). "How to quickly ramp up global vaccine production" Politico.
- Ramsay M, ed. (2020). "Chapter 14a: COVID-19". Immunisation against infectious disease. Public Health England.
- Levine H (23 September 2020). "The 5 Stages of COVID-19 Vaccine Development: What You Need to Know About How a Clinical Trial Works". Johnson & Johnson.
- Ware G (18 February 2021). "How patent laws get in the way of the global coronavirus vaccine rollou". The Conversation.
- Zimmer C, Sheikh K, Weiland N (20 May 2020). "A New Entry in the Race for a Coronavirus Vaccine: Hope". The New York Times.
Vaccine protocols
- "Protocol mRNA-1273-P301" (PDF). Moderna.
- "Protocol C4591001 PF-07302048 (BNT162 RNA-Based COVID-19 Vaccines)" (PDF). Pfizer.
- "Protocol AZD1222 – D8110C00001" (PDF). AstraZeneca.
- "Protocol VAC31518COV3001; Phase 3 (ENSEMBLE)" (PDF). Janssen Vaccines & Prevention.
- "Protocol VAC31518COV3009; Phase 3 (ENSEMBLE 2)" (PDF). Janssen Vaccines & Prevention.
External links
- "The COVID-19 candidate vaccine landscape". World Health Organization (WHO).
- COVID‑19 Vaccine Tracker. Regulatory Focus
- "STAT's Covid-19 Drugs and Vaccines Tracker". Stat.
- "COVID-19 vaccines: development, evaluation, approval and monitoring". European Medicines Agency.
- "Vaccine Development – 101". U.S. Food and Drug Administration.
- "Coronavirus Variants and Mutations". The New York Times.
- M.I.T. Lecture 10: Kizzmekia Corbett, Vaccines" on YouTube