Testosterone
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Androderm, Delatestryl |
| AHFS/Drugs.com | Monograph |
| Pregnancy category |
|
| Routes of administration | Intramuscular injection, transdermal (cream, gel, or patch), sub-'Q' pellet |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | low (due to extensive first pass metabolism) |
| Metabolism | Liver, Testis and Prostate |
| Elimination half-life | 2–4 h |
| Excretion | Urine (90%), feces (6%) |
| Identifiers | |
| |
| CAS Number |
|
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.000.336 |
| Chemical and physical data | |
| Formula | C19H28O2 |
| Molar mass | 288.42 g·mol−1 |
| 3D model (JSmol) | |
| Specific rotation | +110.2° |
| Melting point | 155 °C (311 °F) |
| |
| |
| | |
Testosterone is a steroid hormone from the androgen group and is found in mammals, reptiles,[2] birds,[3] and other vertebrates. In mammals, testosterone is secreted primarily in the testicles of males and the ovaries of females, although small amounts are also secreted by the adrenal glands. It is the principal male sex hormone and an anabolic steroid.
In men, testosterone plays a key role in the development of male reproductive tissues such as the testis and prostate as well as promoting secondary sexual characteristics such as increased muscle, bone mass, and the growth of body hair.[4] In addition, testosterone is essential for health and well-being[5] as well as the prevention of osteoporosis.[6]
On average, in adult males, levels of testosterone are about 7–8 times as great as the in adult females,[7] but, as the metabolic consumption of testosterone in males is greater, the daily production is about 20 times greater in men.[8][9] Females are also more sensitive to the hormone.[10] Testosterone is observed in most vertebrates. Fish make a slightly different form called 11-ketotestosterone.[11] Its counterpart in insects is ecdysone.[12] These ubiquitous steroids suggest that sex hormones have an ancient evolutionary history.[13]
Health effects
In general, androgens promote protein synthesis and growth of those tissues with androgen receptors. Testosterone effects can be classified as virilizing and anabolic, though the distinction is somewhat artificial, as many of the effects can be considered both.
- Anabolic effects include growth of muscle mass and strength, increased bone density and strength, and stimulation of linear growth and bone maturation.
- Androgenic effects include maturation of the sex organs, particularly the penis and the formation of the scrotum in the fetus, and after birth (usually at puberty) a deepening of the voice, growth of the beard and axillary hair. Many of these fall into the category of male secondary sex characteristics.
Testosterone effects can also be classified by the age of usual occurrence. For postnatal effects in both males and females, these are mostly dependent on the levels and duration of circulating free testosterone.
Before birth
The prenatal androgen effects occur during two different stages. Between 4 and 6 weeks of the gestation.
- Genital virilization (midline fusion, phallic urethra, scrotal thinning and rugation, phallic enlargement); although the role of testosterone is far smaller than that of dihydrotestosterone.
- Development of prostate and seminal vesicles.
During the second trimester, androgen level is associated with gender formation.[14] This period affects the femininization or masculinization of the fetus and can be a better predictor of feminine or mascular behaviours such as sex typed behaviour than an adult's own levels. A mother's testosterone level during pregnancy is correlated with her daughter's sex-typical behavior as an adult, and the correlation is even stronger than with the daughter's own adult testosterone level.[15]
Early infancy
Early infancy androgen effects are the least understood. In the first weeks of life for male infants, testosterone levels rise. The levels remain in a pubertal range for a few months, but usually reach the barely detectable levels of childhood by 4–6 months of age.[16][17] The function of this rise in humans is unknown. It has been speculated that "brain masculinization" is occurring since no significant changes have been identified in other parts of the body.[18] It is interesting to note that the male brain is masculinized by the aromatization of testosterone into estrogen, which crosses the blood–brain barrier and enters the male brain, whereas female fetuses have alpha-fetoprotein, which binds the estrogen so that female brains are not affected.[19]
Pre-peripubertal
Pre- Peripubertal effects are the first observable effects of rising androgen levels at the end of childhood, occurring in both boys and girls.
- Adult-type body odor
- Increased oiliness of skin and hair, acne
- Pubarche (appearance of pubic hair)
- Axillary hair
- Growth spurt, accelerated bone maturation
- Hair on upper lip and sideburns.
Pubertal
Pubertal effects begin to occur when androgen has been higher than normal adult female levels for months or years. In males, these are usual late pubertal effects, and occur in women after prolonged periods of heightened levels of free testosterone in the blood.
- Enlargement of sebaceous glands. This might cause acne.
- Phallic enlargement or clitoromegaly
- Increased libido and frequency of erection or clitoral engorgement
- Pubic hair extends to thighs and up toward umbilicus
- Facial hair (sideburns, beard, moustache)
- Loss of scalp hair (Androgenetic alopecia)
- Chest hair, periareolar hair, perianal hair
- Leg hair
- Axillary hair
- Subcutaneous fat in face decreases
- Increased muscle strength and mass[20]
- Deepening of voice
- Growth of the Adam's apple
- Growth of spermatogenic tissue in testicles, male fertility
- Growth of jaw, brow, chin, nose, and remodeling of facial bone contours
- Shoulders become broader and rib cage expands
- Completion of bone maturation and termination of growth. This occurs indirectly via estradiol metabolites and hence more gradually in men than women.
Adult
Adult testosterone effects are more clearly demonstrable in males than in females, but are likely important to both sexes. Some of these effects may decline as testosterone levels decrease in the later decades of adult life.

Biological uses
- Testosterone is necessary for normal sperm development. It activates genes in Sertoli cells, which promote differentiation of spermatogonia.
- Regulates acute HPA (Hypothalamic–pituitary–adrenal axis) response under dominance challenge[21]
- Regulator of cognitive and physical energy
- Maintenance of muscle trophism
- Testosterone regulates the population of thromboxane A2 receptors on megakaryocytes and platelets and hence platelet aggregation in humans[22][23]
- High androgen levels are associated with menstrual cycle irregularities in both clinical populations and healthy women.[24] See libido.
Cancer prevention and health risks
- Testosterone does not cause or produce deleterious effects on prostate cancer. In people who have undergone testosterone deprivation therapy, testosterone increases beyond the castrate level have been shown to increase the rate of spread of an existing prostate cancer.[25][26][27]
- Recent studies have shown conflicting results concerning the importance of testosterone in maintaining cardiovascular health.[28][29] Nevertheless, maintaining normal testosterone levels in elderly men has been shown to improve many parameters that are thought to reduce cardiovascular disease risk, such as increased lean body mass, decreased visceral fat mass, decreased total cholesterol, and glycemic control.[30]
- Under dominance challenge, may play a role in the regulation of the fight-or-flight response[31]
- Men whose testosterone levels are slightly above average are less likely to have high blood pressure, less likely to experience a heart attack, less likely to be obese, and less likely to rate their own health as fair or poor. However, high testosterone men are more likely to report one or more injuries, more likely to consume five or more alcoholic drinks in a day, more likely to have had a sexually transmitted infection, and more likely to smoke.[32]
Romantic relationships and fatherhood
Falling in love decreases men's testosterone levels while increasing women's testosterone levels. There has been speculation that these changes in testosterone result in the temporary reduction of differences in behavior between the sexes.[33] However, it is suggested that after the "honeymoon phase" ends—some one to three years into a relationship—this change in testosterone levels is no longer apparent.[33] Fatherhood also decreases testosterone levels in men, suggesting that the resulting emotional and behavioral changes promote paternal care.[34] Men who produce less testosterone are more likely to be in a relationship[35] and/or married,[36] and men who produce more testosterone are more likely to divorce;[36] however, causality cannot be determined in this relationship. Marriage or commitment could cause a decrease in testosterone levels.[37] Single men who have not had relationship experience have lower testosterone levels than single men with experience. It is suggested that these single men with prior experience are in a more competitive state than their non-experienced counterparts.[38] Married men who engage in bond-maintenance activities such as spending the day with their spouse/and or child have no different testosterone levels compared to times when they do not engage in such activities. Collectively, these results suggest that the presence of competitive activities rather than bond-maintenance activities are more relevant to changes in testosterone levels.[39]
Men who produce more testosterone are more likely to engage in extramarital sex.[36] Testosterone levels do not rely on physical presence of a partner for men engaging in relationships (same-city vs. long-distance), men have similar testosterone levels across the board.[35] Physical presence may be required for women who are in relationships for the testosterone–partner interaction, where same-city partnered women have lower testosterone levels than long-distance partnered women.[40]
Testosterone and sexual arousal
It has been found that when testosterone and endorphins in ejaculated semen meet the cervical wall after sexual intercourse, females receive a spike in testosterone, endorphin, and oxytocin levels, and males after orgasm during copulation experience an increase in endorphins and a marked increase in oxytocin levels. This adds to the hospitable physiological environment in the female internal reproductive tract for conceiving, and later for nurturing the conceptus in the pre-embryonic stages, and stimulates feelings of love, desire, and paternal care in the male (this is the only time male oxytocin levels rival a female's).[33]
Testosterone levels follow a nyctohemeral rhythm that peaks early each day, regardless of sexual activity.[41]
There are positive correlations between positive orgasm experience in women and testosterone levels where relaxation was a key perception of the experience. There is no correlation between testosterone and men's perceptions of their orgasm experience, and also no correlation between higher testosterone levels and greater sexual assertiveness in either sex.[42]
An increase in testosterone levels has also been found to occur in both men and women who have masturbation-induced orgasms.[43][44]
Mammalian studies
Studies conducted on rats have indicated that their degree of sexual arousal is sensitive to reductions in testosterone. When testosterone-deprived rats were given medium levels of testosterone, their sexual behaviors (copulation, partner preference, etc.) resumed, but not when given low amounts of the same hormone. Therefore, these mammals may provide a model for studying clinical populations among humans suffering from sexual arousal deficits such as hypoactive sexual desire disorder.[45]
In one study, almost every mammalian species examined demonstrated a marked increase in a male's testosterone level upon encountering a novel female. P.J. James et al. investigated the role of genotype on such so-called reflexive testosterone increases in male mice. They also concluded that this response is related to the male's initial level of sexual arousal.[46]
In non-human primates it has been suggested that testosterone in puberty stimulates sexual motivation, which allows the primate to increasingly seek out sexual experiences with females and thus creates a sexual preference for females.[47] Some research has also indicated that if testosterone is eliminated in an adult male human or other adult male primate's system, its sexual motivation decreases, but there is no corresponding decrease in ability to engage in sexual activity (mounting, ejaculating, etc.).[47]
Male sexual arousal
Higher levels of testosterone were associated with periods of sexual activity within subjects, but between subjects testosterone levels were higher for less sexually active individuals.[48] Men who have sexual encounters with unfamiliar or multiple partners experience large increases of testosterone the morning after.[49]
Men who watch a sexually explicit movie have an average increase of 35% in testosterone, peaking at 60–90 minutes after the end of the film, but no increase is seen in men who watch sexually neutral films.[50] Men who watch sexually explicit films also report increased optimism and decreased exhaustion.[51] Previous research has found a link between relaxation following sexual arousal and testosterone levels.[52]
A 2002 study found that testosterone increased in heterosexual men after having had a brief conversation with a woman, and stayed the same after a conversation with a man. The increase in testosterone levels was associated with the degree that the women thought the men were trying to impress them.[53]
Men's levels of testosterone, a hormone known to affect men's mating behaviour, changes depending on whether they are exposed to an ovulating or nonovulating woman's body odour. Men who are exposed to scents of ovulating women maintained a stable testosterone level that was higher than the testosterone level of men exposed to nonovulation cues. Testosterone levels and sexual arousal in men are heavily aware of hormone cycles in females.[54] This may be linked to the ovulatory shift hypothesis,[55] where males are adapted to respond to the ovulation cycles of females by sensing when they are most fertile and whereby females look for preferred male mates when they are the most fertile; both actions may be driven by hormones.
In a 1991 study, males were exposed to either visual or auditory erotic stimuli and asked to complete a cognitive task, where the number of errors on the task indicated how distracted the participant was by the stimuli. It concluded that men with lower thresholds for sexual arousal have a greater likelihood to attend to sexual information and that testosterone may have an impact by enhancing their attention to the relevant stimuli.[56]
Sperm competition theory: Testosterone levels are shown to increase as a response to previously neutral stimuli when conditioned to become sexual in male rats.[57] This reaction engages penile reflexes (such as erection and ejaculation) that aid in sperm competition when more than one male is present in mating encounters, allowing for more production of successful sperm and a higher chance of reproduction.
Female sexual arousal
Androgens may modulate the physiology of vaginal tissue and contribute to female genital sexual arousal.[58] Women's level of testosterone is higher when measured pre-intercourse vs pre-cuddling, as well as post-intercourse vs post-cuddling.[59] There is a time lag effect when testosterone is administered, on genital arousal in women. In addition, a continuous increase in vaginal sexual arousal may result in higher genital sensations and sexual appetitive behaviors.[60]
When females have a higher baseline level of testosterone, they have higher increases in sexual arousal levels but smaller increases in testosterone, indicating a ceiling effect on testosterone levels in females. Sexual thoughts also change the level of testosterone but not level of cortisol in the female body, and hormonal contraceptives may have an impact on the variation in testosterone response to sexual thoughts.[61]
Testosterone may prove to be an effective treatment in female sexual arousal disorders.[62] Currently there is no FDA approved androgen preparation for the treatment of androgen insufficiency, however it has been used off-label to treat low libido and sexual dysfunction in older women. Testosterone may be a treatment for postmenopausal women as long as they are effectively estrogenized.[62]
Behavior and personality
Testosterone levels play a major role in risk-taking during financial decisions.[63][64]
A 2009 study of 25 male subjects found that men with artificially raised testosterone were 27% less generous while playing a test game than they were at their normal testosterone level. The authors concluded that "What we have found is that T[estosterone] appears to play a role inducing men to change from being selfless to being selfish."[65]
Brain
As testosterone affects the entire body (often by enlarging; males have bigger hearts, lungs, liver, etc.), the brain is also affected by this "sexual" differentiation;[14] the enzyme aromatase converts testosterone into estradiol that is responsible for masculinization of the brain in male mice. In humans, masculinization of the fetal brain appears, by observation of gender preference in patients with congenital diseases of androgen formation or androgen receptor function, to be associated with functional androgen receptors.[66]
There are some differences between a male and female brain (possibly the result of different testosterone levels), one of them being size: the male human brain is, on average, larger.[67] In a Danish study from 2003, men were found to have a total myelinated fiber length of 176,000 km at the age of 20, whereas in women the total length was 149,000 km (approx. 15% less).[68]
A study conducted in 1996 found no immediate short term effects on mood or behavior from the administration of supraphysiologic doses of testosterone for 10 weeks on 43 healthy men.[20] Another study found a correlation between testosterone and risk tolerance in career choice among women.[69][70]
The literature suggests that attention, memory, and spatial ability are key cognitive functions affected by testosterone in humans. Preliminary evidence suggests that low testosterone levels may be a risk factor for cognitive decline and possibly for dementia of the Alzheimer's type,[71][72][73][74] a key argument in life extension medicine for the use of testosterone in anti-aging therapies. Much of the literature, however, suggests a curvilinear or even quadratic relationship between spatial performance and circulating testosterone,[75] where both hypo- and hypersecretion (deficient- and excessive-secretion) of circulating androgens have negative effects on cognition.
Aggression and criminality
The "evolutionary neuroandrogenic theory" focuses on the hormone testosterone as a factor influencing aggression and criminality and being evolutionarily beneficial during certain forms of competition. In most species, males are more aggressive than females. Castration of males usually has a pacifying effect on their aggressive behavior. In humans, males engage in crime and especially violent crime more than females. Their involvement in crime usually rises in the early teens to mid teens, at the same time as testosterone levels rise. Research on the relationship between testosterone and aggression is difficult, since the only reliable measurement of brain testosterone is by a lumbar puncture that is not done for research purposes. Studies therefore have often instead used more unreliable measurements from blood or saliva. [citation needed]
Most studies support a link between adult criminality and testosterone, although the relationship is modest if examined separately for each sex. Nearly all studies of juvenile delinquency and testosterone are not significant. Most studies have also found testosterone to be associated with behaviors or personality traits linked with criminality such as antisocial behavior and alcoholism. Many studies have also been done on the relationship between more general aggressive behavior/feelings and testosterone. About half the studies have found a relationship and about half no relationship.[76]
The testosterone derivative estradiol (an estrogen) is known to correlate with aggression in male mice.[77] Moreover, the conversion of testosterone to estradiol regulates male aggression in sparrows during breeding season.[78]
Medical uses
The original and primary use of testosterone is for the treatment of males with too little or no natural endogenous testosterone production—males with hypogonadism. Appropriate use for this purpose is legitimate hormone replacement therapy (testosterone replacement therapy [TRT]), which maintains serum testosterone levels in the normal range.
Testosterone has also been given for many other conditions and purposes besides replacement. Examples include reducing infertility, correcting lack of libido or erectile dysfunction, correcting osteoporosis, encouraging penile enlargement, encouraging height growth, encouraging bone marrow stimulation and reversing the effects of anemia, and even appetite stimulation. By the late 1940s, testosterone was being touted as an anti-aging wonder drug (e.g., see Paul de Kruif's The Male Hormone).[79] Decline of testosterone production with age has led to interest in androgen replacement therapy.[80]
To take advantage of its virilizing effects, testosterone is often administered to transsexual men as part of the hormone replacement therapy,[81] with a "target level" of the normal male testosterone level. Likewise, transsexual women are sometimes prescribed anti-androgens to decrease the level of testosterone in the body and allow for the effects of estrogen to develop.
Testosterone patches are effective at treating low libido in post-menopausal women.[82] Low libido may also occur as a symptom or outcome of hormonal contraceptive use. Women may also use testosterone therapies to treat or prevent loss of bone density and muscle mass and to treat certain kinds of depression and low energy state. Women on testosterone therapies may experience an increase in body weight without an increase in body fat due to changes in bone and muscle density. The undesired effects of testosterone therapy in women are typically controlled with symptomatic treatments, such as hair removal and topical acne therapy. There is a theoretical risk that testosterone therapy increases the risk of breast or gynaecological cancers, and further research is needed to define any such risks more clearly.[82]
Appropriate testosterone therapy may improve the management of type 2 diabetes.[83] Low testosterone has been associated with the development of Alzheimer's disease.[73][74] A small trial in 2005 showed mixed results in using testosterone to combat the effects of aging.[84]
Large-scale trials to assess the efficiency and long-term safety of testosterone are still lacking.[85]
Hormone replacement therapy
Testosterone levels decline gradually with age in human beings. The clinical significance of this decrease is debated (see andropause). There is disagreement about when to treat aging men with testosterone replacement therapy. The American Society of Andrology's position is that "testosterone replacement therapy in aging men is indicated when both clinical symptoms and signs suggestive of androgen deficiency and decreased testosterone levels are present."[86] The American Association of Clinical Endocrinologists says "Hypogonadism is defined as a free testosterone level that is below the lower limit of normal for young adult control subjects. Previously, age-related decreases in free testosterone were once accepted as normal. Currently, they are not considered normal. Patients with borderline testosterone levels warrant a clinical trial of testosterone."[87]
There is not total agreement on the threshold of testosterone value below which a man would be considered hypogonadal. (Currently, there are no standards as to when to treat women.) Testosterone can be measured as "free" (that is, bioavailable and unbound) or, more commonly, "total" (including the percentage that is chemically bound and unavailable). In the United States, male total testosterone levels below 300 ng/dL from a morning serum sample are generally considered low.[88] Identification of inadequate testosterone in an aging male by symptoms alone can be difficult.
Adverse effects of testosterone supplementation include minor side-effects such as acne and oily skin, and more significant complications such as increased hematocrit, which can require venipuncture in order to treat, exacerbation of sleep apnea and acceleration of pre-existing prostate cancer growth in individuals having undergone androgen deprivation. Another adverse effect may be significant hair loss and/or thinning of the hair. This may be prevented with 5-alpha reductase inhibitors ordinarily used for the treatment of benign prostatic hyperplasia such as finasteride or dutasteride. Exogenous testosterone also causes suppression of spermatogenesis and can lead to infertility.[89]
Insufficiency
Testosterone insufficiency (also termed hypotestosteronism or hypotestosteronemia) is an abnormally low testosterone production. It may occur because of testicular dysfunction (primary hypogonadism) or hypothalamic-pituitary dysfunction (secondary hypogonadism) and may be congenital or acquired.[90] An acquired form of hypotestosteronism is the decline in testosterone levels that occurs by aging, sometimes called "andropause" in men, as a comparison to the decline in estrogen that comes with menopause in women. In Western countries, average testosterone levels are receding in men of all ages.[91][92] Several theories, from increases in obesity, to exposure to endocrine disruptors have been proposed as an explanation for this reduction.[93]
Recreational use
Athletics
Testosterone can be used by an athlete in order to improve performance, but it is considered to be a form of doping in most sports. There are several application methods for testosterone, including intramuscular injections, transdermal gels and patches, and implantable pellets. Supplement of the hormone results in lower metabolic production via the Farquharson phenomenon, creating long-term dependence for improved performance level.[citation needed]
Anabolic steroids (including testosterone) have also been taken to enhance muscle development, strength, or endurance. They do so directly by increasing the muscles' protein synthesis. As a result, muscle fibers become larger and repair faster than the average person's. After a series of scandals and publicity in the 1980s (such as Ben Johnson's improved performance at the 1988 Summer Olympics), prohibitions of anabolic steroid use were renewed or strengthened by many sports organizations. Testosterone and other anabolic steroids were designated a "controlled substance" by the United States Congress in 1990, with the Anabolic Steroid Control Act.[94] The use is seen as being a seriously problematic issue in modern sport, particularly given the lengths to which athletes and professional laboratories go to in trying to conceal such abuse from sports regulators. Steroid abuse once again came into the spotlight recently as a result of the Chris Benoit double murder-suicide in 2007, however, there has been no evidence indicating steroid use as a contributing factor.[citation needed]
Detection of abuse
A number of methods for detecting testosterone use by athletes have been employed, most based on a urine test. These include the testosterone/epitestosterone ratio (normally less than 6), the testosterone/luteinizing hormone ratio and the carbon-13 / carbon-12 ratio (pharmaceutical testosterone contains less carbon-13 than endogenous testosterone). In some testing programs, an individual's own historical results may serve as a reference interval for interpretation of a suspicious finding. Another approach being investigated is the detection of the administered form of testosterone, usually an ester, in hair.[95][96][97][98]
Adverse effects
Testosterone is contraindicated in pregnancy and not recommended during breastfeeding.[99]
Whether or not testosterone therapy in men causes important adverse effects is unclear.[100] Up to the year 2010, studies had not shown an affect on the risk of death, prostate cancer or cardiovascular disease.;[100][101] two more recent studies, however, do raise concern.[102] It does increase hemoglobin levels and decrease HDL cholesterol levels but it is not clear if these changes are meaningful.[100] In the New York Times, Dr. Brad Anwalt, University of Washington, was quoted by reporter Roni Caryn Rabin as "For people with truly low testosterone levels, the benefits outweigh the risks,...But for millions of others, it's in the same category as snake oil...There are what I would label testosterone factories out there, and it's terrifying because we don't know what the long-term safety profile is."; February 14 2014, The New York Times: "A high price for vigor".
Testosterone in the presence of a slow-growing cancer is assumed to increase its growth rate. However the association between testosterone supplementation and the development of prostate cancer is unproven.[103] Nevertheless physicians are cautioned about the cancer risk associated with testosterone supplementation.[104]
Fluoxymesterone and methyltestosterone are synthetic derivatives of testosterone. Methyltestosterone and fluoxymesterone are no longer prescribed by physicians, given their poor safety record.
Ethnic groups have different rates of prostate cancer.[105] Differences in sex hormones including testosterone have been suggested as an explanation for these differences.[105] This apparent paradox can be resolved by noting that prostate cancer is very common. In autopsies, 80% of 80-year-old men have prostate cancer.[106]
Biochemistry
Biosynthesis

Like other steroid hormones, testosterone is derived from cholesterol (see figure to the left).[107] The first step in the biosynthesis involves the oxidative cleavage of the sidechain of cholesterol by CYP11A, a mitochondrial cytochrome P450 oxidase with the loss of six carbon atoms to give pregnenolone. In the next step, two additional carbon atoms are removed by the CYP17A enzyme in the endoplasmic reticulum to yield a variety of C19 steroids.[108] In addition, the 3-hydroxyl group is oxidized by 3-β-HSD to produce androstenedione. In the final and rate limiting step, the C-17 keto group androstenedione is reduced by 17-β hydroxysteroid dehydrogenase to yield testosterone.
The largest amounts of testosterone (>95%) are produced by the testes in men.[4] It is also synthesized in far smaller quantities in women by the thecal cells of the ovaries, by the placenta, as well as by the zona reticularis of the adrenal cortex and even skin[109] in both sexes. In the testes, testosterone is produced by the Leydig cells.[110] The male generative glands also contain Sertoli cells, which require testosterone for spermatogenesis. Like most hormones, testosterone is supplied to target tissues in the blood where much of it is transported bound to a specific plasma protein, sex hormone-binding globulin (SHBG).
Regulation

In males, testosterone is synthesized primarily in Leydig cells. The number of Leydig cells in turn is regulated by luteinizing hormone (LH) and follicle-stimulating hormone (FSH). In addition, the amount of testosterone produced by existing Leydig cells is under the control of LH, which regulates the expression of 17-β hydroxysteroid dehydrogenase.[111]
The amount of testosterone synthesized is regulated by the hypothalamic–pituitary–testicular axis (see figure to the right).[112] When testosterone levels are low, gonadotropin-releasing hormone (GnRH) is released by the hypothalamus, which in turn stimulates the pituitary gland to release FSH and LH. These latter two hormones stimulate the testis to synthesize testosterone. Finally, increasing levels of testosterone through a negative feedback loop act on the hypothalamus and pituitary to inhibit the release of GnRH and FSH/LH, respectively.
Environmental factors affecting testosterone levels include:
- Weight loss may result in an increase in testosterone levels. Fat cells synthesize the enzyme aromatase, which converts testosterone, the male sex hormone, into estradiol, the female sex hormone.[113]
- The secosteroid vitamin D in levels of 400–1000 IU/d (10–25 mcg/d) raises testosterone levels.[114]
- Zinc deficiency lowers testosterone levels[115] but over supplementation has no effect on serum testosterone.[116]
- Dominance challenges can, in some cases, stimulate increased testosterone release in men.[117]
- Aging reduces testosterone release.[118]
- Hypogonadism
- Sleep (REM dream) increases nocturnal testosterone levels.[119]
- Resistance training increases testosterone levels,[120] however, in older men, that increase can be avoided by protein ingestion.[121]
- Licorice. The active ingredient in licorice root, glycyrrhizinic acid has been linked to small, clinically non-significant decreases in testosterone levels.[122] In contrast, a more recent study found that licorice administration produced a substantial testosterone decrease in a small, female-only sample.[123]
- Natural or man-made antiandrogens including spearmint tea reduce testosterone levels.[124][125][126]
Metabolism
Approximately 7% of testosterone is reduced to 5α-dihydrotestosterone (DHT) by the cytochrome P450 enzyme 5α-reductase,[127] an enzyme highly expressed in male sex organs and hair follicles.[4] Approximately 0.3% of testosterone is converted into estradiol by aromatase (CYP19A1)[128] an enzyme expressed in the brain, liver, and adipose tissues.[4]
DHT is a more potent form of testosterone while estradiol has completely different activities (feminization) compared to testosterone (masculinization). Also, testosterone and DHT may be deactivated or cleared by enzymes that hydroxylate at the 6, 7, 15 or 16 positions.[129]
Mechanism of action
The effects of testosterone in humans and other vertebrates occur by way of two main mechanisms: by activation of the androgen receptor (directly or as DHT), and by conversion to estradiol and activation of certain estrogen receptors.[130][131]
Free testosterone (T) is transported into the cytoplasm of target tissue cells, where it can bind to the androgen receptor, or can be reduced to 5α-dihydrotestosterone (DHT) by the cytoplasmic enzyme 5-alpha reductase. DHT binds to the same androgen receptor even more strongly than testosterone, so that its androgenic potency is about 5 times that of T.[132] The T-receptor or DHT-receptor complex undergoes a structural change that allows it to move into the cell nucleus and bind directly to specific nucleotide sequences of the chromosomal DNA. The areas of binding are called hormone response elements (HREs), and influence transcriptional activity of certain genes, producing the androgen effects.
Androgen receptors occur in many different vertebrate body system tissues, and both males and females respond similarly to similar levels. Greatly differing amounts of testosterone prenatally, at puberty, and throughout life account for a share of biological differences between males and females.
The bones and the brain are two important tissues in humans where the primary effect of testosterone is by way of aromatization to estradiol. In the bones, estradiol accelerates ossification of cartilage into bone, leading to closure of the epiphyses and conclusion of growth. In the central nervous system, testosterone is aromatized to estradiol. Estradiol rather than testosterone serves as the most important feedback signal to the hypothalamus (especially affecting LH secretion).[citation needed] In many mammals, prenatal or perinatal "masculinization" of the sexually dimorphic areas of the brain by estradiol derived from testosterone programs later male sexual behavior.[citation needed]
Synthetic analogs
A number of synthetic analogs of testosterone have been developed with improved bioavailability and metabolic half life relative to testosterone. Many of these analogs have an alkyl group introduced at the C-17 position in order to prevent conjugation and hence improve oral bioavailability. These are the so-called "17-aa" (17-alkyl androgen) family of androgens such as fluoxymesterone and methyltestosterone.
Related drugs
Some drugs indirectly target testosterone as a way of treating certain conditions. For example, 5-alpha-reductase inhibitors such as finasteride inhibit the conversion of testosterone into dihydrotestosterone (DHT), a metabolite more potent than testosterone.[133] These 5-alpha-reductase inhibitors have been used to treat various conditions associated with androgens, such as androgenetic alopecia (male-pattern baldness), hirsutism, benign prostatic hyperplasia (BPH), and prostate cancer.[133] In contrast, GnRH antagonists bind to GnRH receptors in the pituitary gland, blocking the release of luteinising hormone (LH) and follicle-stimulating hormone (FSH) from the pituitary.[134] In men, the reduction in LH subsequently leads to rapid suppression of testosterone release from the testes. GnRH antagonists have been used for the treatment of prostate cancer.
Routes of administration

There are many routes of administration for testosterone. Forms of testosterone for human administration currently available include injectable (such as testosterone cypionate or testosterone enanthate in oil),[135] oral, buccal,[136] transdermal skin patches, transdermal creams, gels,[137][138] and implantable pellets.[139] Roll-on methods and nasal sprays are currently under development.
History
A testicular action was linked to circulating blood fractions – now understood to be a family of androgenic hormones – in the early work on castration and testicular transplantation in fowl by Arnold Adolph Berthold (1803–1861).[140] Research on the action of testosterone received a brief boost in 1889, when the Harvard professor Charles-Édouard Brown-Séquard (1817–1894), then in Paris, self-injected subcutaneously a "rejuvenating elixir" consisting of an extract of dog and guinea pig testicle. He reported in The Lancet that his vigor and feeling of well-being were markedly restored but the effects were transient,[141] and Brown-Séquard's hopes for the compound were dashed. Suffering the ridicule of his colleagues, he abandoned his work on the mechanisms and effects of androgens in human beings.
In 1927, the University of Chicago's Professor of Physiologic Chemistry, Fred C. Koch, established easy access to a large source of bovine testicles — the Chicago stockyards — and recruited students willing to endure the tedious work of extracting their isolates. In that year, Koch and his student, Lemuel McGee, derived 20 mg of a substance from a supply of 40 pounds of bovine testicles that, when administered to castrated roosters, pigs and rats, remasculinized them.[142] The group of Ernst Laqueur at the University of Amsterdam purified testosterone from bovine testicles in a similar manner in 1934, but isolation of the hormone from animal tissues in amounts permitting serious study in humans was not feasible until three European pharmaceutical giants—Schering (Berlin, Germany), Organon (Oss, Netherlands) and Ciba (Basel, Switzerland)—began full-scale steroid research and development programs in the 1930s.

The Organon group in the Netherlands were the first to isolate the hormone, identified in a May 1935 paper "On Crystalline Male Hormone from Testicles (Testosterone)".[143] They named the hormone testosterone, from the stems of testicle and sterol, and the suffix of ketone. The structure was worked out by Schering's Adolf Butenandt.[144][145]
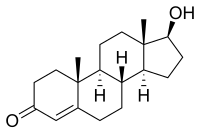
The chemical synthesis of testosterone from cholesterol was achieved in August that year by Butenandt and Hanisch.[146] Only a week later, the Ciba group in Zurich, Leopold Ruzicka (1887–1976) and A. Wettstein, published their synthesis of testosterone.[147] These independent partial syntheses of testosterone from a cholesterol base earned both Butenandt and Ruzicka the joint 1939 Nobel Prize in Chemistry.[145][148] Testosterone was identified as 17β-hydroxyandrost-4-en-3-one (C19H28O2), a solid polycyclic alcohol with a hydroxyl group at the 17th carbon atom. This also made it obvious that additional modifications on the synthesized testosterone could be made, i.e., esterification and alkylation.
The partial synthesis in the 1930s of abundant, potent testosterone esters permitted the characterization of the hormone's effects, so that Kochakian and Murlin (1936) were able to show that testosterone raised nitrogen retention (a mechanism central to anabolism) in the dog, after which Allan Kenyon's group[149] was able to demonstrate both anabolic and androgenic effects of testosterone propionate in eunuchoidal men, boys, and women. The period of the early 1930s to the 1950s has been called "The Golden Age of Steroid Chemistry",[150] and work during this period progressed quickly. Research in this golden age proved that this newly synthesized compound—testosterone—or rather family of compounds (for many derivatives were developed from 1940 to 1960), was a potent multiplier of muscle, strength, and well-being.[79]
Synthesis
Preparation of testosterone from the abundant starting compound dehydroepiandrosterone () in essence involves interchanging oxidation states between C3 and C17, a process that would involve juggling protecting groups. The selectivity with which manganese dioxide oxidizes allylic hydroxyl groups simplifies that transformation.
Thus, reduction of androst-5-ene-1,17-dione () with lithium aluminum hydride reduced both 3- and 17-carbonyl groups, that atC17 cleanly to the b-epimer and the ketone at C3 to a mixture of epimers (). Treatment of the mixture of epimers with manganese dioxide oxidizes the allylic alcohol at C3, leaving that at C17 untouched, affording testosterone ().
References
- ^ "FDA-sourced list of all drugs with black box warnings (Use Download Full Results and View Query links.)". nctr-crs.fda.gov. FDA. Retrieved 22 Oct 2023.
- ^ Cox RM, John-Alder HB (December 2005). "Testosterone has opposite effects on male growth in lizards (Sceloporus spp.) with opposite patterns of sexual size dimorphism". J. Exp. Biol. 208 (Pt 24): 4679–87. doi:10.1242/jeb.01948. PMID 16326949.
- ^ Reed WL, Clark ME, Parker PG, Raouf SA, Arguedas N, Monk DS, Snajdr E, Nolan V, Ketterson ED (May 2006). "Physiological effects on demography: a long-term experimental study of testosterone's effects on fitness". Am. Nat. 167 (5): 667–83. doi:10.1086/503054. PMID 16671011.
{{cite journal}}: Unknown parameter|laysource=ignored (help); Unknown parameter|layurl=ignored (help)CS1 maint: multiple names: authors list (link) - ^ a b c d Mooradian AD, Morley JE, Korenman SG (February 1987). "Biological actions of androgens". Endocr. Rev. 8 (1): 1–28. doi:10.1210/edrv-8-1-1. PMID 3549275.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Bassil N, Alkaade S, Morley JE (June 2009). "The benefits and risks of testosterone replacement therapy: a review". Ther Clin Risk Manag. 5 (3): 427–48. PMC 2701485. PMID 19707253.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Tuck SP, Francis RM (2009). "Testosterone, bone and osteoporosis". Front Horm Res. Frontiers of Hormone Research. 37: 123–32. doi:10.1159/000176049. ISBN 978-3-8055-8622-1. PMID 19011293.
- ^ Torjesen PA, Sandnes L (March 2004). "Serum testosterone in women as measured by an automated immunoassay and a RIA". Clin. Chem. 50 (3): 678, author reply 678–9. doi:10.1373/clinchem.2003.027565. PMID 14981046.
- ^ Southren AL, Gordon GG, Tochimoto S, Pinzon G, Lane DR, Stypulkowski W (May 1967). "Mean plasma concentration, metabolic clearance and basal plasma production rates of testosterone in normal young men and women using a constant infusion procedure: effect of time of day and plasma concentration on the metabolic clearance rate of testosterone". J. Clin. Endocrinol. Metab. 27 (5): 686–94. doi:10.1210/jcem-27-5-686. PMID 6025472.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Southren AL, Tochimoto S, Carmody NC, Isurugi K (November 1965). "Plasma production rates of testosterone in normal adult men and women and in patients with the syndrome of feminizing testes". J. Clin. Endocrinol. Metab. 25 (11): 1441–50. doi:10.1210/jcem-25-11-1441. PMID 5843701.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Dabbs M, Dabbs JM (2000). Heroes, rogues, and lovers: testosterone and behavior. New York: McGraw-Hill. ISBN 0-07-135739-4.
- ^ Nelson, Randy F. (2005). An introduction to behavioral endocrinology. Sunderland, Mass: Sinauer Associates. p. 143. ISBN 0-87893-617-3.
- ^ De Loof A (October 2006). "Ecdysteroids: the overlooked sex steroids of insects? Males: the black box". Insect Science. 13 (5): 325–338. doi:10.1111/j.1744-7917.2006.00101.x.
- ^ Mechoulam R, Brueggemeier RW, Denlinger DL (September 1984). "Estrogens in insects". Journal Cellular and Molecular Life Sciences. 40 (9): 942–944. doi:10.1007/BF01946450.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Swaab DF, Garcia-Falgueras A (2009). "Sexual differentiation of the human brain in relation to gender identity and sexual orientation". Funct. Neurol. 24 (1): 17–28. PMID 19403051.
- ^ Browne KR (2002). Biology at work: rethinking sexual equality. New Brunswick, N.J: Rutgers University Press. p. 112. ISBN 0-8135-3053-9.
- ^ Forest MG, Cathiard AM, Bertrand JA (July 1973). "Evidence of testicular activity in early infancy". J. Clin. Endocrinol. Metab. 37 (1): 148–51. doi:10.1210/jcem-37-1-148. PMID 4715291.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Corbier P, Edwards DA, Roffi J (1992). "The neonatal testosterone surge: a comparative study". Arch Int Physiol Biochim Biophys. 100 (2): 127–31. doi:10.3109/13813459209035274. PMID 1379488.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Dakin CL, Wilson CA, Kalló I, Coen CW, Davies DC (May 2008). "Neonatal stimulation of 5-HT(2) receptors reduces androgen receptor expression in the rat anteroventral periventricular nucleus and sexually dimorphic preoptic area". Eur. J. Neurosci. 27 (9): 2473–80. doi:10.1111/j.1460-9568.2008.06216.x. PMID 18445234.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Kalat JW (2009). "Reproductive behaviors". Biological psychology. Belmont, Calif: Wadsworth, Cengage Learning. p. 321. ISBN 0-495-60300-7.
{{cite book}}: External link in|chapterurl=|chapterurl=ignored (|chapter-url=suggested) (help) - ^ a b Bhasin S, Storer TW, Berman N, Callegari C, Clevenger B, Phillips J, Bunnell TJ, Tricker R, Shirazi A, Casaburi R (July 1996). "The effects of supraphysiologic doses of testosterone on muscle size and strength in normal men". N. Engl. J. Med. 335 (1): 1–7. doi:10.1056/NEJM199607043350101. PMID 8637535.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Mehta PH, Jones AC, Josephs RA (June 2008). "The social endocrinology of dominance: basal testosterone predicts cortisol changes and behavior following victory and defeat" (PDF). J Pers Soc Psychol. 94 (6): 1078–93. doi:10.1037/0022-3514.94.6.1078. PMID 18505319.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Ajayi AA, Halushka PV (May 2005). "Castration reduces platelet thromboxane A2 receptor density and aggregability". QJM. 98 (5): 349–56. doi:10.1093/qjmed/hci054. PMID 15820970.
- ^ Ajayi AA, Mathur R, Halushka PV (June 1995). "Testosterone increases human platelet thromboxane A2 receptor density and aggregation responses". Circulation. 91 (11): 2742–7. doi:10.1161/01.CIR.91.11.2742. PMID 7758179.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Van Anders SM, Watson NV (2006). "Menstrual cycle irregularities are associated with testosterone levels in healthy premenopausal women". Am. J. Hum. Biol. 18 (6): 841–4. doi:10.1002/ajhb.20555. PMID 17039468.
- ^ Morgentaler A, Schulman C (2009). "Testosterone and prostate safety". Front Horm Res. Frontiers of Hormone Research. 37: 197–203. doi:10.1159/000176054. ISBN 978-3-8055-8622-1. PMID 19011298.
- ^ Rhoden, E.L., M.A. Averbeck, and P.E. Teloken (2008). "Androgen replacement in men undergoing treatment for prostate cancer". J Sex Med. 5 (9): 2202–8. doi:10.1111/j.1743-6109.2008.00925.x. PMID 18638000.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Morgentaler, A. and A.M. Traish (2009). "Shifting the paradigm of testosterone and prostate cancer: the saturation model and the limits of androgen-dependent growth". Eur Urol. 55 (2): 310–20. doi:10.1016/j.eururo.2008.09.024. PMID 18838208.
- ^ Haddad RM, Kennedy CC, Caples SM, Tracz MJ, Boloña ER, Sideras K, Uraga MV, Erwin PJ, Montori VM (January 2007). "Testosterone and cardiovascular risk in men: a systematic review and meta-analysis of randomized placebo-controlled trials". Mayo Clin. Proc. 82 (1): 29–39. doi:10.4065/82.1.29. PMID 17285783.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Jones TH, Saad F (April 2009). "The effects of testosterone on risk factors for, and the mediators of, the atherosclerotic process". Atherosclerosis. 207 (2): 318–27. doi:10.1016/j.atherosclerosis.2009.04.016. PMID 19464009.
- ^ Stanworth RD, Jones TH (2008). "Testosterone for the aging male; current evidence and recommended practice". Clin Interv Aging. 3 (1): 25–44. PMC 2544367. PMID 18488876.
- ^ Mehta PH, Josephs RA (December 2006). "Testosterone change after losing predicts the decision to compete again". Horm Behav. 50 (5): 684–92. doi:10.1016/j.yhbeh.2006.07.001. PMID 16928375.
- ^ Booth A, Johnson DR, Granger DA (February 1999). "Testosterone and men's health". J Behav Med. 22 (1): 1–19. doi:10.1023/A:1018705001117. PMID 10196726.
{{cite journal}}: Unknown parameter|laysource=ignored (help); Unknown parameter|layurl=ignored (help)CS1 maint: multiple names: authors list (link) - ^ a b c Marazziti D, Canale D (August 2004). "Hormonal changes when falling in love". Psychoneuroendocrinology. 29 (7): 931–6. doi:10.1016/j.psyneuen.2003.08.006. PMID 15177709.
- ^ Berg SJ, Wynne-Edwards KE (2001). "Changes in testosterone, cortisol, and estradiol levels in men becoming fathers". Mayo Clinic Proceedings. 76 (1): 582–592. doi:10.4065/76.6.582.
- ^ a b van Anders SM, Watson NV (July 2006). "Relationship status and testosterone in North American heterosexual and non-heterosexual men and women: cross-sectional and longitudinal data". Psychoneuroendocrinology. 31 (6): 715–23. doi:10.1016/j.psyneuen.2006.01.008. PMID 16621328.
- ^ a b c Booth A, Dabbs JM (1993). "Testosterone and Men's Marriages". Social Forces. 72 (2): 463–477. doi:10.1093/sf/72.2.463.
- ^ Mazur A, Michalek J (1998). "Marriage, Divorce, and Male Testosterone". Social Forces. 77 (1): 315–330. doi:10.1093/sf/77.1.315.
- ^ Gray PB, Chapman JF, Burnham TC, McIntyre MH, Lipson SF, Ellison PT (2004). "Human male pair bonding and testosterone". Human Nature. 15 (2): 119–131. doi:10.1007/s12110-004-1016-6.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Gray PB, Campbell BC, Marlowe FW, Lipson SF, Ellison PT (October 2004). "Social variables predict between-subject but not day-to-day variation in the testosterone of US men". Psychoneuroendocrinology. 29 (9): 1153–62. doi:10.1016/j.psyneuen.2004.01.008. PMID 15219639.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ van Anders SM, Watson NV (February 2007). "Testosterone levels in women and men who are single, in long-distance relationships, or same-city relationships". Horm Behav. 51 (2): 286–91. doi:10.1016/j.yhbeh.2006.11.005. PMID 17196592.
- ^ Fox CA, Ismail AA, Love DN, Kirkham KE, Loraine JA (January 1972). "Studies on the relationship between plasma testosterone levels and human sexual activity". J. Endocrinol. 52 (1): 51–8. doi:10.1677/joe.0.0520051. PMID 5061159.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ van Anders SM, Dunn EJ (August 2009). "Are gonadal steroids linked with orgasm perceptions and sexual assertiveness in women and men?". Horm Behav. 56 (2): 206–13. doi:10.1016/j.yhbeh.2009.04.007. PMID 19409392.
- ^ Exton MS, Bindert A, Krüger T, Scheller F, Hartmann U, Schedlowski M (1999). "Cardiovascular and endocrine alterations after masturbation-induced orgasm in women". Psychosom Med. 61 (3): 280–9. PMID 10367606.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Purvis K, Landgren BM, Cekan Z, Diczfalusy E (September 1976). "Endocrine effects of masturbation in men". J. Endocrinol. 70 (3): 439–44. doi:10.1677/joe.0.0700439. PMID 135817.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Harding SM, Velotta JP (May 2011). "Comparing the relative amount of testosterone required to restore sexual arousal, motivation, and performance in male rats". Horm Behav. 59 (5): 666–73. doi:10.1016/j.yhbeh.2010.09.009. PMID 20920505.
- ^ James PJ, Nyby JG, Saviolakis GA (September 2006). "Sexually stimulated testosterone release in male mice (Mus musculus): roles of genotype and sexual arousal". Horm Behav. 50 (3): 424–31. doi:10.1016/j.yhbeh.2006.05.004. PMID 16828762.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Wallen K (September 2001). "Sex and context: hormones and primate sexual motivation". Horm Behav. 40 (2): 339–57. doi:10.1006/hbeh.2001.1696. PMID 11534996.
- ^ Kraemer HC, Becker HB, Brodie HK, Doering CH, Moos RH, Hamburg DA (March 1976). "Orgasmic frequency and plasma testosterone levels in normal human males". Arch Sex Behav. 5 (2): 125–32. doi:10.1007/BF01541869. PMID 1275688.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Hirschenhauser K, Frigerio D, Grammer K, Magnusson MS (September 2002). "Monthly patterns of testosterone and behavior in prospective fathers". Horm Behav. 42 (2): 172–81. doi:10.1006/hbeh.2002.1815. PMID 12367570.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Pirke KM, Kockott G, Dittmar F (November 1974). "Psychosexual stimulation and plasma testosterone in man". Arch Sex Behav. 3 (6): 577–84. doi:10.1007/BF01541140. PMID 4429441.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Hellhammer DH, Hubert W, Schürmeyer T (1985). "Changes in saliva testosterone after psychological stimulation in men". Psychoneuroendocrinology. 10 (1): 77–81. doi:10.1016/0306-4530(85)90041-1. PMID 4001279.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Rowland DL, Heiman JR, Gladue BA, Hatch JP, Doering CH, Weiler SJ (1987). "Endocrine, psychological and genital response to sexual arousal in men". Psychoneuroendocrinology. 12 (2): 149–58. doi:10.1016/0306-4530(87)90045-X. PMID 3602262.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Roney JR, Mahler SV, Maestripieri D (2003). "Behavioral and hormonal responses of men to brief interactions with women". Evolution and Human Behavior. 24 (6): 365–375. doi:10.1016/S1090-5138(03)00053-9.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Miller SL, Maner JK (February 2010). "Scent of a woman: men's testosterone responses to olfactory ovulation cues". Psychol Sci. 21 (2): 276–83. doi:10.1177/0956797609357733. PMID 20424057.
- ^ Gangestead SW, Thornhill R, Garver-Apgar CE (2005). "Adaptations to Ovulation: Implications for Sexual and Social Behavior". Current Directions in Psychological Science. 14 (6): 312–316. doi:10.1111/j.0963-7214.2005.00388.x.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Alexander GM, Sherwin BB (September 1991). "The association between testosterone, sexual arousal, and selective attention for erotic stimuli in men". Horm Behav. 25 (3): 367–81. doi:10.1016/0018-506X(91)90008-6. PMID 1937428.
- ^ Hart BL (December 1983). "Role of testosterone secretion and penile reflexes in sexual behavior and sperm competition in male rats: a theoretical contribution". Physiol. Behav. 31 (6): 823–7. doi:10.1016/0031-9384(83)90279-2. PMID 6665072.
- ^ Traish AM, Kim N, Min K, Munarriz R, Goldstein I (April 2002). "Role of androgens in female genital sexual arousal: receptor expression, structure, and function". Fertil. Steril. 77 Suppl 4: S11–8. PMID 12007897.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ van Anders SM, Hamilton LD, Schmidt N, Watson NV (April 2007). "Associations between testosterone secretion and sexual activity in women". Horm Behav. 51 (4): 477–82. doi:10.1016/j.yhbeh.2007.01.003. PMID 17320881.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Tuiten A, Van Honk J, Koppeschaar H, Bernaards C, Thijssen J, Verbaten R (February 2000). "Time course of effects of testosterone administration on sexual arousal in women". Arch. Gen. Psychiatry. 57 (2): 149–53, discussion 155–6. doi:10.1001/archpsyc.57.2.149. PMID 10665617.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Goldey KL, van Anders SM (May 2011). "Sexy thoughts: effects of sexual cognitions on testosterone, cortisol, and arousal in women". Horm Behav. 59 (5): 754–64. doi:10.1016/j.yhbeh.2010.12.005. PMID 21185838.
- ^ a b Bolour S, Braunstein G (2005). "Testosterone therapy in women: a review". Int. J. Impot. Res. 17 (5): 399–408. doi:10.1038/sj.ijir.3901334. PMID 15889125.
- ^ Sapienza P, Zingales L, Maestripieri D (September 2009). "Gender differences in financial risk aversion and career choices are affected by testosterone". Proc. Natl. Acad. Sci. U.S.A. 106 (36): 15268–73. Bibcode:2009PNAS..10615268S. doi:10.1073/pnas.0907352106. PMC 2741240. PMID 19706398.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Apicella CL, Dreber A, Campbell B, Gray PB, Hoffman M, Little AC (November 2008). "Testosterone and financial risk preferences". Evolution and Human Behavior. 29 (6): 384–390. doi:10.1016/j.evolhumbehav.2008.07.001.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Zak PJ, Kurzban R, Ahmadi S, Swerdloff RS, Park J, Efremidze L, Redwine K, Morgan K, Matzner W (2009). Aleman, André (ed.). "Testosterone administration decreases generosity in the ultimatum game". PLoS ONE. 4 (12): e8330. Bibcode:2009PLoSO...4.8330Z. doi:10.1371/journal.pone.0008330. PMC 2789942. PMID 20016825.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - ^ Wilson JD (September 2001). "Androgens, androgen receptors, and male gender role behavior". Horm Behav. 40 (2): 358–66. doi:10.1006/hbeh.2001.1684. PMID 11534997.
- ^ Cosgrove KP, Mazure CM, Staley JK (October 2007). "Evolving knowledge of sex differences in brain structure, function, and chemistry". Biol. Psychiatry. 62 (8): 847–55. doi:10.1016/j.biopsych.2007.03.001. PMC 2711771. PMID 17544382.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Marner L, Nyengaard JR, Tang Y, Pakkenberg B (July 2003). "Marked loss of myelinated nerve fibers in the human brain with age". J. Comp. Neurol. 462 (2): 144–52. doi:10.1002/cne.10714. PMID 12794739.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Paola Sapienzaa, Luigi Zingales and Dario Maestripieri (2009). "Gender differences in financial risk aversion and career choices are affected by testosterone". PNAS. 106 (36): 15268–15273. Bibcode:2009PNAS..10615268S. doi:10.1073/pnas.0907352106. PMC 2741240. PMID 19706398.
- ^ "Testosterone Affects Some Women's Career Choices". NPR. August 28, 2009.
- ^ Hogervorst E, Bandelow S, Combrinck M, Smith AD (2004). "Low free testosterone is an independent risk factor for Alzheimer's disease". Exp. Gerontol. 39 (11–12): 1633–9. doi:10.1016/j.exger.2004.06.019. PMID 15582279.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Moffat SD, Zonderman AB, Metter EJ, Kawas C, Blackman MR, Harman SM, Resnick SM (January 2004). "Free testosterone and risk for Alzheimer disease in older men". Neurology. 62 (2): 188–93. doi:10.1212/WNL.62.2.188. PMID 14745052.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Pike CJ, Rosario ER, Nguyen TV (April 2006). "Androgens, aging, and Alzheimer's disease". Endocrine. 29 (2): 233–41. doi:10.1385/ENDO:29:2:233. PMID 16785599.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Rosario ER, Chang L, Stanczyk FZ, Pike CJ (September 2004). "Age-related testosterone depletion and the development of Alzheimer disease". JAMA. 292 (12): 1431–2. doi:10.1001/jama.292.12.1431-b. PMID 15383512.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Moffat SD, Hampson E (April 1996). "A curvilinear relationship between testosterone and spatial cognition in humans: possible influence of hand preference". Psychoneuroendocrinology. 21 (3): 323–37. doi:10.1016/0306-4530(95)00051-8. PMID 8817730.
- ^ Wright J, Ellis L, Beaver K (2009). Handbook of crime correlates. San Diego: Academic Press. pp. 208–210. ISBN 0-12-373612-9.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ^ Soma KK, Scotti MA, Newman AE, Charlier TD, Demas GE (October 2008). "Novel mechanisms for neuroendocrine regulation of aggression". Front Neuroendocrinol. 29 (4): 476–89. doi:10.1016/j.yfrne.2007.12.003. PMID 18280561.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Soma KK, Sullivan KA, Tramontin AD, Saldanha CJ, Schlinger BA, Wingfield JC (2000). "Acute and chronic effects of an aromatase inhibitor on territorial aggression in breeding and nonbreeding male song sparrows". J. Comp. Physiol. A. 186 (7–8): 759–69. doi:10.1007/s003590000129. PMID 11016791.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b de Kruif P (1945). The Male Hormone. New York: Harcourt, Brace.
- ^ Myers JB, Meacham RB (2003). "Androgen Replacement Therapy in the Aging Male". Rev Urol. 5 (4): 216–26. PMC 1508369. PMID 16985841.
- ^ "Gender dysphoria - Treatment". NHS Gov.uk. Page last reviewed: 21/05/2012. Retrieved 31 October 2013.
{{cite web}}: Check date values in:|date=(help) - ^ a b Davis SR, Moreau M, Kroll R, Bouchard C, Panay N, Gass M, Braunstein GD, Hirschberg AL, Rodenberg C, Pack S, Koch H, Moufarege A, Studd J (November 2008). "Testosterone for low libido in postmenopausal women not taking estrogen". N. Engl. J. Med. 359 (19): 2005–17. doi:10.1056/NEJMoa0707302. PMID 18987368.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Traish AM, Saad F, Guay A (2009). "The dark side of testosterone deficiency: II. Type 2 diabetes and insulin resistance". J. Androl. 30 (1): 23–32. doi:10.2164/jandrol.108.005751. PMID 18772488.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Emmelot-Vonk MH, Verhaar HJ, Nakhai Pour HR, Aleman A, Lock TM, Bosch JL, Grobbee DE, van der Schouw YT (January 2008). "Effect of testosterone supplementation on functional mobility, cognition, and other parameters in older men: a randomized controlled trial". JAMA. 299 (1): 39–52. doi:10.1001/jama.2007.51. PMID 18167405.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Cunningham GR (2008-06-25). "Testosterone treatment in aging men". EndocrineToday.com. Retrieved 2009-07-17.
- ^ "Testosterone replacement therapy for male aging: ASA position statement". J. Androl. 27 (2): 133–4. 2006. PMID 16474019.
- ^ Guay AT, Spark RF, Bansal S, Cunningham GR, Goodman NF, Nankin HR, Petak SM, Perez JB (2003). "American Association of Clinical Endocrinologists medical guidelines for clinical practice for the evaluation and treatment of male sexual dysfunction: a couple's problem—2003 update" (PDF). Endocr Pract. 9 (1): 77–95. doi:10.4158/EP.9.1.77. PMID 12917096.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Holt EH, Zieve D (2008-03-18). "Testosterone". MedlinePlus Medical Encyclopedia. U.S. National Library of Medicine. Retrieved 2009-07-17.
{{cite web}}: Cite has empty unknown parameter:|coauthors=(help) - ^ "Contraceptive efficacy of testosterone-induced azoospermia in normal men. World Health Organization Task Force on methods for the regulation of male fertility". Lancet. 336 (8721): 955–9. October 1990. doi:10.1016/0140-6736(90)92416-F. PMID 1977002.
- ^ Gould DC, Petty R (August 2000). "The male menopause: does it exist?: For: Some men need investigation and testosterone treatment". West. J. Med. 173 (2): 76–8. doi:10.1136/ewjm.173.2.76. PMC 1070997. PMID 10924412.
- ^ Travison TG, Araujo AB, O'Donnell AB, Kupelian V, McKinlay JB (January 2007). "A population-level decline in serum testosterone levels in American men". J. Clin. Endocrinol. Metab. 92 (1): 196–202. doi:10.1210/jc.2006-1375. PMID 17062768.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Dindyal S (2007). "The sperm count has been decreasing steadily for many years in Western industrialised countries: Is there an endocrine basis for this decrease?". The Internet Journal of Urology. 2 (1): 1–21.
- ^ Bhasin S (January 2007). "Secular decline in male reproductive function: Is manliness threatened?". J. Clin. Endocrinol. Metab. 92 (1): 44–5. doi:10.1210/jc.2006-2438. PMID 17209224.
- ^ "Anabolic Steroid Control Act" (PDF). United States Sentencing Commission. 1990.
- ^ Strahm E, Emery C, Saugy M, Dvorak J, Saudan C (December 2009). "Detection of testosterone administration based on the carbon isotope ratio profiling of endogenous steroids: international reference populations of professional soccer players". Br J Sports Med. 43 (13): 1041–4. doi:10.1136/bjsm.2009.058669. PMC 2784500. PMID 19549614.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Kicman AT, Cowan DA (January 2009). "Subject-based profiling for the detection of testosterone administration in sport". Drug Test Anal. 1 (1): 22–4. doi:10.1002/dta.14. PMID 20355155.
- ^ Pozo OJ, Deventer K, Van Eenoo P, Rubens R, Delbeke FT (August 2009). "Quantification of testosterone undecanoate in human hair by liquid chromatography-tandem mass spectrometry". Biomed. Chromatogr. 23 (8): 873–80. doi:10.1002/bmc.1199. PMID 19353724.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Baselt RC (2008). Disposition of Toxic Drugs & Chemicals in Man (8th ed.). Foster City, Calif: Biomedical Publications. pp. 1501–1504. ISBN 978-0-9626523-7-0.
- ^ "Testosterone Pregnancy and Breastfeeding Warnings". Retrieved 1 February 2014.
- ^ a b c Fernández-Balsells, MM (June 2010). "Clinical review 1: Adverse effects of testosterone therapy in adult men: a systematic review and meta-analysis". The Journal of Clinical Endocrinology and Metabolism. 95 (6): 2560–75. doi:10.1210/jc.2009-2575. PMID 20525906.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Haddad, RM (January 2007). "Testosterone and cardiovascular risk in men: a systematic review and meta-analysis of randomized placebo-controlled trials". Mayo Clinic proceedings. Mayo Clinic. 82 (1): 29–39. doi:10.4065/82.1.29. PMID 17285783.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ "Testosterone Products: Drug Safety Communication - FDA Investigating Risk of Cardiovascular Events". FDA. Jan 31,2014. Retrieved 3 February 2014.
{{cite web}}: Check date values in:|date=(help) - ^ Rhoden EL, Averbeck MA (November 2009). "Testosterone therapy and prostate carcinoma". Curr Urol Rep. 10 (6): 453–9. doi:10.1007/s11934-009-0072-1. PMID 19863857.
- ^ Gaylis FD, Lin DW, Ignatoff JM, Amling CL, Tutrone RF, Cosgrove DJ (August 2005). "Prostate cancer in men using testosterone supplementation". J. Urol. 174 (2): 534–8, discussion 538. doi:10.1097/01.ju.0000165166.36280.60. PMID 16006887.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Calistro Alvarado L (2010). "Population differences in the testosterone levels of young men are associated with prostate cancer disparities in older men". Am. J. Hum. Biol. 22 (4): 449–55. doi:10.1002/ajhb.21016. PMID 20087895.
- ^ Bostwick DG, Burke HB, Djakiew D, Euling S, Ho SM, Landolph J, Morrison H, Sonawane B, Shifflett T, Waters DJ, Timms B (November 2004). "Human prostate cancer risk factors". Cancer. 101 (10 Suppl): 2371–490. doi:10.1002/cncr.20408. PMID 15495199.
{{cite journal}}: Unknown parameter|laysource=ignored (help); Unknown parameter|layurl=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Waterman MR, Keeney DS (1992). "Genes involved in androgen biosynthesis and the male phenotype". Horm. Res. 38 (5–6): 217–21. doi:10.1159/000182546. PMID 1307739.
- ^ Zuber MX, Simpson ER, Waterman MR (December 1986). "Expression of bovine 17 alpha-hydroxylase cytochrome P-450 cDNA in nonsteroidogenic (COS 1) cells". Science. 234 (4781): 1258–61. Bibcode:1986Sci...234.1258Z. doi:10.1126/science.3535074. PMID 3535074.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Zouboulis CC, Degitz K (2004). "Androgen action on human skin – from basic research to clinical significance". Exp. Dermatol. 13 Suppl 4: 5–10. doi:10.1111/j.1600-0625.2004.00255.x. PMID 15507105.
- ^ Brooks RV (November 1975). "Androgens". Clin Endocrinol Metab. 4 (3): 503–20. doi:10.1016/S0300-595X(75)80045-4. PMID 58744.
- ^ Payne AH, O'Shaughnessy P (1996). "Structure, function, and regulation of steroidogenic enzymes in the Leydig cell". In Payne AH, Hardy MP, Russell LD (ed.). Leydig Cell. Vienna [Il]: Cache River Press. pp. 260–285. ISBN 0-9627422-7-9.
{{cite book}}: CS1 maint: multiple names: editors list (link) - ^ Swerdloff RS, Wang C, Bhasin S (April 1992). "Developments in the control of testicular function". Baillieres Clin. Endocrinol. Metab. 6 (2): 451–83. doi:10.1016/S0950-351X(05)80158-2. PMID 1377467.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Håkonsen LB, Thulstrup AM, Aggerholm AS, Olsen J, Bonde JP, Andersen CY, Bungum M, Ernst EH, Hansen ML, Ernst EH, Ramlau-Hansen CH (2011). "Does weight loss improve semen quality and reproductive hormones? Results from a cohort of severely obese men". Reprod Health. 8: 24. doi:10.1186/1742-4755-8-24. PMC 3177768. PMID 21849026.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - ^ Pilz S, Frisch S, Koertke H, Kuhn J, Dreier J, Obermayer-Pietsch B, Wehr E, Zittermann A (March 2011). "Effect of vitamin D supplementation on testosterone levels in men". Horm. Metab. Res. 43 (3): 223–5. doi:10.1055/s-0030-1269854. PMID 21154195.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Prasad AS, Mantzoros CS, Beck FW, Hess JW, Brewer GJ (May 1996). "Zinc status and serum testosterone levels of healthy adults". Nutrition. 12 (5): 344–8. doi:10.1016/S0899-9007(96)80058-X. PMID 8875519.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Koehler K, Parr MK, Geyer H, Mester J, Schänzer W (January 2009). "Serum testosterone and urinary excretion of steroid hormone metabolites after administration of a high-dose zinc supplement". Eur J Clin Nutr. 63 (1): 65–70. doi:10.1038/sj.ejcn.1602899. PMID 17882141.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Schultheiss OC, Campbell KL, McClelland DC (December 1999). "Implicit power motivation moderates men's testosterone responses to imagined and real dominance success". Horm Behav. 36 (3): 234–41. doi:10.1006/hbeh.1999.1542. PMID 10603287.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Liu PY, Pincus SM, Takahashi PY, Roebuck PD, Iranmanesh A, Keenan DM, Veldhuis JD (January 2006). "Aging attenuates both the regularity and joint synchrony of LH and testosterone secretion in normal men: analyses via a model of graded GnRH receptor blockade". Am. J. Physiol. Endocrinol. Metab. 290 (1): E34–E41. doi:10.1152/ajpendo.00227.2005. PMID 16339924.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Andersen ML, Tufik S (October 2008). "The effects of testosterone on sleep and sleep-disordered breathing in men: its bidirectional interaction with erectile function" (PDF). Sleep Med Rev. 12 (5): 365–79. doi:10.1016/j.smrv.2007.12.003. PMID 18519168.
- ^ Marin DP, Figueira AJ Junior, Pinto LG (2006). "One session of resistance training may increase serum testosterone and triiodetironine in young men". Medicine & Science in Sports & Exercise. 38 (5): S285. doi:10.1249/00005768-200605001-01235.
{{cite journal}}: Cite has empty unknown parameter:|month=(help)CS1 maint: multiple names: authors list (link) - ^ Hulmi JJ, Ahtiainen JP, Selänne H, Volek JS, Häkkinen K, Kovanen V, Mero AA (May 2008). "Androgen receptors and testosterone in men—effects of protein ingestion, resistance exercise and fiber type". J. Steroid Biochem. Mol. Biol. 110 (1–2): 130–7. doi:10.1016/j.jsbmb.2008.03.030. PMID 18455389.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Josephs RA, Guinn JS, Harper ML, Askari F (November 2001). "Liquorice consumption and salivary testosterone concentrations". Lancet. 358 (9293): 1613–4. doi:10.1016/S0140-6736(01)06664-8. PMID 11716893.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Armanini D, Mattarello MJ, Fiore C, Bonanni G, Scaroni C, Sartorato P, Palermo M (2004). "Licorice reduces serum testosterone in healthy women". Steroids. 69 (11–12): 763–6. doi:10.1016/j.steroids.2004.09.005. PMID 15579328.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Akdoğan M, Tamer MN, Cüre E, Cüre MC, Köroğlu BK, Delibaş N (May 2007). "Effect of spearmint (Mentha spicata Labiatae) teas on androgen levels in women with hirsutism". Phytother Res. 21 (5): 444–7. doi:10.1002/ptr.2074. PMID 17310494.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Kumar V, Kural MR, Pereira BM, Roy P (December 2008). "Spearmint induced hypothalamic oxidative stress and testicular anti-androgenicity in male rats – altered levels of gene expression, enzymes and hormones". Food Chem. Toxicol. 46 (12): 3563–70. doi:10.1016/j.fct.2008.08.027. PMID 18804513.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Grant P (February 2010). "Spearmint herbal tea has significant anti-androgen effects in polycystic ovarian syndrome. A randomized controlled trial". Phytother Res. 24 (2): 186–8. doi:10.1002/ptr.2900. PMID 19585478.
- ^ Randall VA (April 1994). "Role of 5 alpha-reductase in health and disease". Baillieres Clin. Endocrinol. Metab. 8 (2): 405–31. doi:10.1016/S0950-351X(05)80259-9. PMID 8092979.
- ^ Meinhardt U, Mullis PE (August 2002). "The essential role of the aromatase/p450arom". Semin. Reprod. Med. 20 (3): 277–84. doi:10.1055/s-2002-35374. PMID 12428207.
- ^ Trager L (1977). Steroidhormone: Biosynthese, Stoffwechsel, Wirkung (in German). Springer-Verlag. p. 349. ISBN 0-387-08012-0.
- ^ Hiipakka RA, Liao S (October 1998). "Molecular mechanism of androgen action". Trends Endocrinol. Metab. 9 (8): 317–24. doi:10.1016/S1043-2760(98)00081-2. PMID 18406296.
- ^ McPhaul MJ, Young M (September 2001). "Complexities of androgen action". J. Am. Acad. Dermatol. 45 (3 Suppl): S87–94. doi:10.1067/mjd.2001.117429. PMID 11511858.
- ^ Breiner M, Romalo G, Schweikert HU (August 1986). "Inhibition of androgen receptor binding by natural and synthetic steroids in cultured human genital skin fibroblasts". Klin. Wochenschr. 64 (16): 732–7. doi:10.1007/BF01734339. PMID 3762019.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Bratoeff E, Cabeza M, Ramirez E, Heuze Y, Flores E (2005). "Recent advances in the chemistry and pharmacological activity of new steroidal antiandrogens and 5 alpha-reductase inhibitors". Curr. Med. Chem. 12 (8): 927–43. doi:10.2174/0929867053507306. PMID 15853706.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Engel JB, Schally AV (February 2007). "Drug Insight: clinical use of agonists and antagonists of luteinizing-hormone-releasing hormone". Nat Clin Pract Endocrinol Metab. 3 (2): 157–67. doi:10.1038/ncpendmet0399. PMID 17237842.
- ^ "Testosterone Information". Drugs.com.
{{cite web}}: Cite has empty unknown parameter:|coauthors=(help) - ^ "Striant Official FDA information, side effects and uses". Drugs.com.
{{cite web}}: Cite has empty unknown parameter:|coauthors=(help) - ^ "AndroGel Official FDA information, side effects and uses". Drugs.com.
{{cite web}}: Cite has empty unknown parameter:|coauthors=(help) - ^ "Testim (patches and gel) medical facts". Drugs.com.
{{cite web}}: Cite has empty unknown parameter:|coauthors=(help) - ^ "Testopel Pellets". www.slatepharma.com.
- ^ Berthold AA (1849). "Transplantation der Hoden". Arch. Anat. Physiol. Wissensch. (in German). 16: 42–6.
{{cite journal}}: Cite has empty unknown parameter:|month=(help); Unknown parameter|trans_title=ignored (|trans-title=suggested) (help) - ^ Brown-Sequard CE (1889). "The effects produced on man by subcutaneous injections of liquid obtained from the testicles of animals". Lancet. 2 (3438): 105. doi:10.1016/S0140-6736(00)64118-1.
{{cite journal}}: Cite has empty unknown parameter:|month=(help) - ^ Gallagher TF, Koch FC (November 1929). "The testicular hormone". J. Biol. Chem. 84 (2): 495–500.
- ^ David KG., Dingemanse E, Freud J. Laqueur E (May 1935). "Über krystallinisches mannliches Hormon aus Hoden (Testosteron) wirksamer als aus harn oder aus Cholesterin bereitetes Androsteron". Hoppe Seylers Z Physiol Chem (in German). 233 (5–6): 281. doi:10.1515/bchm2.1935.233.5-6.281.
{{cite journal}}: Unknown parameter|trans_title=ignored (|trans-title=suggested) (help)CS1 maint: multiple names: authors list (link) - ^ Butenandt A, Hanisch G (1935). "Umwandlung des Dehydroandrosterons in Androstendiol und Testosterone; ein Weg zur Darstellung des Testosterons aus Cholestrin". Hoppe Seylers Z Physiol Chem (in German). 237 (2): 89. doi:10.1515/bchm2.1935.237.1-3.89.
{{cite journal}}: Cite has empty unknown parameter:|month=(help); Unknown parameter|trans_title=ignored (|trans-title=suggested) (help) - ^ a b Freeman ER, Bloom DA, McGuire EJ (February 2001). "A brief history of testosterone". J. Urol. 165 (2): 371–3. doi:10.1097/00005392-200102000-00004. PMID 11176375.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Butenandt A, Hanisch G (1935). "Uber die Umwandlung des Dehydroandrosterons in Androstenol-(17)-one-(3) (Testosterone); um Weg zur Darstellung des Testosterons auf Cholesterin (Vorlauf Mitteilung). [The conversion of dehydroandrosterone into androstenol-(17)-one-3 (testosterone); a method for the production of testosterone from cholesterol (preliminary communication)]". Chemische Berichte (in German). 68: 1859–1862.
- ^ Ruzicka L, Wettstein A (1935). "Uber die kristallinische Herstellung des Testikelhormons, Testosteron (Androsten-3-ol-17-ol) [The crystalline production of the testicle hormone, testosterone (Androsten-3-ol-17-ol)]". Helvetica Chimica Acta (in German). 18: 1264–1275. doi:10.1002/hlca.193501801176.
- ^ Hoberman JM, Yesalis CE (February 1995). "The history of synthetic testosterone". Sci. Am. 272 (2): 76–81. doi:10.1038/scientificamerican0295-76. PMID 7817189.
- ^ Kenyon AT, Knowlton K, Sandiford I, Koch FC, Lotwin,G (February 1940). "A comparative study of the metabolic effects of testosterone propionate in normal men and women and in eunuchoidism". Endocrinology. 26 (1): 26–45. doi:10.1210/Endo-26-1-26.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Schwarz S, Onken D, Schubert A (July 1999). "The steroid story of Jenapharm: from the late 1940s to the early 1970s". Steroids. 64 (7): 439–45. doi:10.1016/S0039-128X(99)00003-3. PMID 10443899.
{{cite journal}}: CS1 maint: multiple names: authors list (link)
External links
- Testosterone bound to proteins in the PDB
- Testosterone - Lab Tests Online

