Dehydroepiandrosterone sulfate: Difference between revisions
No edit summary |
|||
| Line 40: | Line 40: | ||
}} |
}} |
||
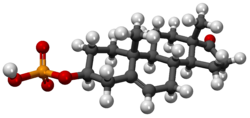
'''Dehydroepiandrosterone sulfate''', abbreviated as '''DHEA sulfate''' or '''DHEA-S''', also known as '''prasterone sulfate''', is an [[endogenous]] [[androstane]] [[steroid]] |
'''Dehydroepiandrosterone sulfate''', abbreviated as '''DHEA sulfate''' or '''DHEA-S''', also known as '''prasterone sulfate''', is an [[endogenous]] [[androstane]] [[steroid]] that is produced by the [[adrenal cortex]].<ref name="Erkkola2006" /> It is the the 3β-[[sulfate]] [[ester]] and a [[metabolite]] of [[dehydroepiandrosterone]] (DHEA) that circulates in far greater relative concentrations.<ref name="pmid26908835" /> The steroid is [[hormonal]]ly inert and is instead an important [[neurosteroid]] and [[neurotrophin]].<ref name="pmid26908835" /> as well as a [[metabolic intermediate]] in the [[biosynthesis]] of [[steroid hormone]]s like the [[androgen]]s and [[estrogen]]s.<ref name="pmid26908835" /> |
||
==Medical use== |
==Medical use== |
||
| Line 51: | Line 51: | ||
===Parturition=== |
===Parturition=== |
||
As the [[sodium salt]], [[prasterone sodium sulfate]], DHEA-S is used as a [[pharmaceutical drug]] in [[Japan]] in the treatment of insufficient [[cervical effacement|cervical ripening]] and [[cervical dilation]] during [[parturition]] (childbirth).<ref name="Elks2014">{{cite book|author=J. Elks|title=The Dictionary of Drugs: Chemical Data: Chemical Data, Structures and Bibliographies|url=https://books.google.com/books?id=0vXTBwAAQBAJ&pg=PA641|date=14 November 2014|publisher=Springer|isbn=978-1-4757-2085-3|pages=641–}}</ref><ref name="BluntMunro2007">{{cite book|author1=John W. Blunt|author2=Murray H. G. Munro|title=Dictionary of Marine Natural Products with CD-ROM|url=https://books.google.com/books?id=w1bLBQAAQBAJ&pg=PA1075|date=19 September 2007|publisher=CRC Press|isbn=978-0-8493-8217-8|pages=1075–}}</ref><ref name="KleemannEngel2014">{{cite book|author1=A. Kleemann|author2=J. Engel|author3=B. Kutscher |author4=D. Reichert|title=Pharmaceutical Substances, 5th Edition, 2009: Syntheses, Patents and Applications of the most relevant APIs|url=https://books.google.com/books?id=fO2IAwAAQBAJ&pg=PT2441|date=14 May 2014|publisher=Thieme|isbn=978-3-13-179525-0|pages=2441–2442}}</ref><ref name="NegwerScharnow2001">{{cite book|author1=Martin Negwer|author2=Hans-Georg Scharnow|title=Organic-chemical drugs and their synonyms: (an international survey)|url=https://books.google.com/books?id=zmpqAAAAMAAJ|year=2001|publisher=Wiley-VCH|isbn=978-3-527-30247-5|page=1831|quote=3β-Hydroxyandrost-5-en-17-one hydrogen sulfate = (3β)-3-(Sulfooxy)androst-5-en-17-one. R: Sodium salt (1099-87-2). S: Astenile, Dehydroepiandrosterone sulfate sodium, DHA-S, DHEAS, KYH 3102, Mylis, PB 005, Prasterone sodium sulfate, Teloin}}</ref><ref name="Jianqiu1992">Jianqiu, Y. (1992). Clinical Application of Prasterone Sodium Sulfate. ''Chinese Journal of New Drugs'', 5, 015.</ref><ref name="pmid1403604">{{cite journal | vauthors = Sakaguchi M, Sakai T, Adachi Y, Kawashima T, Awata N | title = The biological fate of sodium prasterone sulfate after vaginal administration. I. Absorption and excretion in rats | journal = J. Pharmacobio-dyn. | volume = 15 | issue = 2 | pages = 67–73 | year = 1992 | pmid = 1403604 | doi = | url = }}</ref><ref name="SakaiSakaguchi1992">Sakai, T., Sakaguchi, M., Adachi, Y., Kawashima, T., & Awata, N. (1992). The Biological Fate of Sodium Prasterone Sulfate after Vaginal Administration II: Distribution after Single and Multiple Administration to Pregnant Rats. 薬物動態, 7(1), 87-101.</ref> |
As the [[sodium salt]], [[prasterone sodium sulfate]], DHEA-S is used as a [[pharmaceutical drug]] in [[Japan]] in the treatment of insufficient [[cervical effacement|cervical ripening]] and [[cervical dilation]] during [[parturition]] (childbirth).<ref name="Elks2014">{{cite book|author=J. Elks|title=The Dictionary of Drugs: Chemical Data: Chemical Data, Structures and Bibliographies|url=https://books.google.com/books?id=0vXTBwAAQBAJ&pg=PA641|date=14 November 2014|publisher=Springer|isbn=978-1-4757-2085-3|pages=641–}}</ref><ref name="BluntMunro2007">{{cite book|author1=John W. Blunt|author2=Murray H. G. Munro|title=Dictionary of Marine Natural Products with CD-ROM|url=https://books.google.com/books?id=w1bLBQAAQBAJ&pg=PA1075|date=19 September 2007|publisher=CRC Press|isbn=978-0-8493-8217-8|pages=1075–}}</ref><ref name="KleemannEngel2014">{{cite book|author1=A. Kleemann|author2=J. Engel|author3=B. Kutscher |author4=D. Reichert|title=Pharmaceutical Substances, 5th Edition, 2009: Syntheses, Patents and Applications of the most relevant APIs|url=https://books.google.com/books?id=fO2IAwAAQBAJ&pg=PT2441|date=14 May 2014|publisher=Thieme|isbn=978-3-13-179525-0|pages=2441–2442}}</ref><ref name="NegwerScharnow2001">{{cite book|author1=Martin Negwer|author2=Hans-Georg Scharnow|title=Organic-chemical drugs and their synonyms: (an international survey)|url=https://books.google.com/books?id=zmpqAAAAMAAJ|year=2001|publisher=Wiley-VCH|isbn=978-3-527-30247-5|page=1831|quote=3β-Hydroxyandrost-5-en-17-one hydrogen sulfate = (3β)-3-(Sulfooxy)androst-5-en-17-one. R: Sodium salt (1099-87-2). S: Astenile, Dehydroepiandrosterone sulfate sodium, DHA-S, DHEAS, KYH 3102, Mylis, PB 005, Prasterone sodium sulfate, Teloin}}</ref><ref name="Jianqiu1992">Jianqiu, Y. (1992). Clinical Application of Prasterone Sodium Sulfate. ''Chinese Journal of New Drugs'', 5, 015.</ref><ref name="pmid1403604">{{cite journal | vauthors = Sakaguchi M, Sakai T, Adachi Y, Kawashima T, Awata N | title = The biological fate of sodium prasterone sulfate after vaginal administration. I. Absorption and excretion in rats | journal = J. Pharmacobio-dyn. | volume = 15 | issue = 2 | pages = 67–73 | year = 1992 | pmid = 1403604 | doi = | url = }}</ref><ref name="SakaiSakaguchi1992">Sakai, T., Sakaguchi, M., Adachi, Y., Kawashima, T., & Awata, N. (1992). The Biological Fate of Sodium Prasterone Sulfate after Vaginal Administration II: Distribution after Single and Multiple Administration to Pregnant Rats. 薬物動態, 7(1), 87-101.</ref> |
||
==Biological activity== |
|||
Similarly to other [[conjugation (biochemistry)|conjugated]] steroids, DHEA-S is devoid of [[hormone|hormonal]] activity, lacking [[affinity (pharmacology)|affinity]] for the [[steroid hormone receptor]]s.<ref name="Krause2008">{{cite book|author=Walter K.H. Krause|title=Cutaneous Manifestations of Endocrine Diseases|url=https://books.google.com/books?id=QymSmuV-fvUC&pg=PA79|date=30 November 2008|publisher=Springer Science & Business Media|isbn=978-3-540-88367-8|pages=79–}}</ref> However, DHEA-S retains activity as a [[neurosteroid]] and [[neurotrophin]].<ref name="pmid26908835">{{cite journal | vauthors = Prough RA, Clark BJ, Klinge CM | title = Novel mechanisms for DHEA action | journal = J. Mol. Endocrinol. | volume = 56 | issue = 3 | pages = R139–55 | year = 2016 | pmid = 26908835 | doi = 10.1530/JME-16-0013 | url = }}</ref> It has been found to act as a [[positive allosteric modulator]] of the [[NMDA receptor]] (50 nM–1 µM), [[negative allosteric modulator]] of the [[GABAA receptor|GABA<sub>A</sub> receptor]], and weak [[ligand (biochemistry)|ligand]] of the [[sigma-1 receptor]] (K<sub>d</sub> > 50 µM).<ref name="pmid26908835" /> In addition, DHEA-S has been found to directly bind to and activate the [[TrkA]] and [[p75NTR|p75<sup>NTR</sup>]] – receptors of neurotrophins like [[nerve growth factor]] (NGF) and [[brain-derived neurotrophic factor]] (BDNF) – with high affinity (around 5 nM).<ref name="pmid26908835" /><ref name="pmid21541365">{{cite journal | vauthors = Lazaridis I, Charalampopoulos I, Alexaki VI, Avlonitis N, Pediaditakis I, Efstathopoulos P, Calogeropoulou T, Castanas E, Gravanis A | title = Neurosteroid dehydroepiandrosterone interacts with nerve growth factor (NGF) receptors, preventing neuronal apoptosis | journal = PLoS Biol. | volume = 9 | issue = 4 | pages = e1001051 | year = 2011 | pmid = 21541365 | pmc = 3082517 | doi = 10.1371/journal.pbio.1001051 | url = }}</ref><ref name="pmid25330101">{{cite journal | vauthors = Pediaditakis I, Iliopoulos I, Theologidis I, Delivanoglou N, Margioris AN, Charalampopoulos I, Gravanis A | title = Dehydroepiandrosterone: an ancestral ligand of neurotrophin receptors | journal = Endocrinology | volume = 156 | issue = 1 | pages = 16–23 | year = 2015 | pmid = 25330101 | doi = 10.1210/en.2014-1596 | url = }}</ref><ref name="pmid23074265">{{cite journal | vauthors = Gravanis A, Calogeropoulou T, Panoutsakopoulou V, Thermos K, Neophytou C, Charalampopoulos I | title = Neurosteroids and microneurotrophins signal through NGF receptors to induce prosurvival signaling in neuronal cells | journal = Sci Signal | volume = 5 | issue = 246 | pages = pt8 | year = 2012 | pmid = 23074265 | doi = 10.1126/scisignal.2003387 | url = }}</ref> |
|||
Although DHEA-S itself is hormonally inert, it can be converted back into DHEA,<ref name="Morfin2003">{{cite book|author=Robert Morfin|title=DHEA and the Brain|url=https://books.google.com/books?id=uZp62ctguF0C&pg=PA28|date=2 September 2003|publisher=CRC Press|isbn=978-0-203-30121-0|pages=28–}}</ref> which is weakly [[androgen]]ic and [[estrogen]]ic, and DHEA in turn can be transformed into more potent androgens like [[testosterone]] and [[dihydrotestosterone]] (DHT) as well as estrogens like [[estradiol]].<ref name="pmid26908835" /><ref name="Erkkola2006" /> As such, DHEA-S is a [[prohormone]] with the potential for androgenic and estrogenic effects.<ref name="pmid26908835" /><ref name="Erkkola2006" /> |
|||
==Biochemistry== |
==Biochemistry== |
||
| Line 58: | Line 63: | ||
===Metabolism=== |
===Metabolism=== |
||
DHEA-S can be converted back |
DHEA-S can be converted back into DHEA via [[steroid sulfatase]] (STS).<ref name="Morfin2003" /> In [[premenopausal]] women, 40 to 75% of circulating testosterone is derived from peripheral [[metabolism]] of DHEA-S, and in [[postmenopausal]] women, over 90% of estrogens, mainly [[estrone]], are derived from peripheral metabolism of DHEA-S.<ref name="pmid26908835" /> |
||
===Levels=== |
===Levels=== |
||
| Line 144: | Line 149: | ||
{{Endogenous steroids}} |
{{Endogenous steroids}} |
||
| ⚫ | |||
{{GABA receptor modulators}} |
{{GABA receptor modulators}} |
||
| ⚫ | |||
{{Glutamate receptor modulators}} |
{{Glutamate receptor modulators}} |
||
{{Glycine receptor modulators}} |
{{Glycine receptor modulators}} |
||
{{ |
{{Growth factor receptor modulators}} |
||
{{Nuclear receptor modulators}} |
{{Nuclear receptor modulators}} |
||
Revision as of 11:49, 30 May 2017

| |
| |
| Names | |
|---|---|
| IUPAC name
[(3S,8R,9S,10R,13S,14S)-10,13-Dimethyl-17-oxo-1,2,3,4,7,8,9,11,12,14,15,16-dodecahydrocyclopenta[a]phenanthren-3-yl] hydrogen sulfate
| |
| Other names
Prasterone sulfate
| |
| Identifiers | |
3D model (JSmol)
|
|
| Abbreviations | DHEA sulfate; DHEA-S; DHEAS |
| ChemSpider | |
PubChem CID
|
|
CompTox Dashboard (EPA)
|
|
| |
| |
| Properties | |
| C19H28O5S | |
| Molar mass | 368.49 g/mol |
Except where otherwise noted, data are given for materials in their standard state (at 25 °C [77 °F], 100 kPa).
| |
Dehydroepiandrosterone sulfate, abbreviated as DHEA sulfate or DHEA-S, also known as prasterone sulfate, is an endogenous androstane steroid that is produced by the adrenal cortex.[1] It is the the 3β-sulfate ester and a metabolite of dehydroepiandrosterone (DHEA) that circulates in far greater relative concentrations.[2] The steroid is hormonally inert and is instead an important neurosteroid and neurotrophin.[2] as well as a metabolic intermediate in the biosynthesis of steroid hormones like the androgens and estrogens.[2]
Medical use
Hypoandrogenism
The Endocrine Society recommends against the therapeutic use of DHEA-S in both healthy women and those with adrenal insufficiency, as its role is not clear from studies performed so far.[3] The routine use of DHEA-S and other androgens is discouraged in the treatment of women with low androgen levels due to hypopituitarism, adrenal insufficiency, menopause due to ovarian surgery, glucocorticoid use, or other conditions associated with low androgen levels; this is because there are limited data supporting improvement in signs and symptoms with therapy and no long-term studies of risk.[3]
In otherwise elderly women, in whom an age-related fall of DHEA-S may be associated with menopausal symptoms and reduced libido, DHEA-S supplementation cannot currently be said to improve outcomes.[4]
Parturition
As the sodium salt, prasterone sodium sulfate, DHEA-S is used as a pharmaceutical drug in Japan in the treatment of insufficient cervical ripening and cervical dilation during parturition (childbirth).[5][6][7][8][9][10][11]
Biological activity
Similarly to other conjugated steroids, DHEA-S is devoid of hormonal activity, lacking affinity for the steroid hormone receptors.[12] However, DHEA-S retains activity as a neurosteroid and neurotrophin.[2] It has been found to act as a positive allosteric modulator of the NMDA receptor (50 nM–1 µM), negative allosteric modulator of the GABAA receptor, and weak ligand of the sigma-1 receptor (Kd > 50 µM).[2] In addition, DHEA-S has been found to directly bind to and activate the TrkA and p75NTR – receptors of neurotrophins like nerve growth factor (NGF) and brain-derived neurotrophic factor (BDNF) – with high affinity (around 5 nM).[2][13][14][15]
Although DHEA-S itself is hormonally inert, it can be converted back into DHEA,[16] which is weakly androgenic and estrogenic, and DHEA in turn can be transformed into more potent androgens like testosterone and dihydrotestosterone (DHT) as well as estrogens like estradiol.[2][1] As such, DHEA-S is a prohormone with the potential for androgenic and estrogenic effects.[2][1]
Biochemistry
Biosynthesis
DHEA and DHEA-S are produced in the zona reticularis of the adrenal cortex under the control of adrenocorticotropic hormone (ACTH).[1] DHEA is synthesized from cholesterol via the enzymes cholesterol side-chain cleavage enzyme (CYP11A1; P450scc) and 17α-hydroxylase/17,20-lyase (CYP17A1), with pregnenolone and 17α-hydroxypregnenolone as intermediates.[17] Then, DHEA-S is formed by sulfation of DHEA at the C3β position via the sulfotransferase enzyme SULT2A1.[17][18] Whereas DHEA is secreted primarily by the adrenal cortex but is also secreted to a lesser extent by the gonads, DHEA-S is almost exclusively produced and secreted by the adrenal cortex.[1]
Metabolism
DHEA-S can be converted back into DHEA via steroid sulfatase (STS).[16] In premenopausal women, 40 to 75% of circulating testosterone is derived from peripheral metabolism of DHEA-S, and in postmenopausal women, over 90% of estrogens, mainly estrone, are derived from peripheral metabolism of DHEA-S.[2]
Levels
| Tanner stage and average age | Lower limit | Upper limit | Unit | |
|---|---|---|---|---|
| Tanner stage I | >14 days | 16 | 96 | µg/dL |
| Tanner stage II | 10.5 years | 22 | 184 | |
| Tanner stage III | 11.6 years | <15 | 296 | |
| Tanner stage IV | 12.3 years | 17 | 343 | |
| Tanner stage V | 14.5 years | 44 | 332 | |
| 18–29 years | 44 | 332 | ||
| 30–39 years | 31 | 228 | ||
| 40–49 years | 18 | 244 | ||
| 50–59 years | <15 | 200 | ||
| > or =60 years | <15 | 157 | ||
| Tanner stage and average age | Lower limit | Upper limit | Unit | |
|---|---|---|---|---|
| Tanner stage I | >14 days | <15 | 120 | µg/dL |
| Tanner stage II | 11.5 years | <15 | 333 | |
| Tanner stage III | 13.6 years | <15 | 312 | |
| Tanner stage IV | 15.1 years | 29 | 412 | |
| Tanner stage V | 18.0 years | 89 | 457 | |
| 18–29 years | 89 | 457 | ||
| 30–39 years | 65 | 334 | ||
| 40–49 years | 48 | 244 | ||
| 50–59 years | 35 | 179 | ||
| > or =60 years | 25 | 131 | ||
Diagnostic use
DHEA-S levels above 1890 µM/L or 700-800 µg/dL are highly suggestive of adrenal dysfunction because DHEA-S is made by the adrenal glands[20][21] and also synthesized in the brain.[22] The presence of DHEA-S is therefore used to rule out ovarian or testicular origin of excess androgen.
See also
References
- ^ a b c d e Risto Erkkola (2006). The Menopause. Elsevier. pp. 5–. ISBN 978-0-444-51830-9.
- ^ a b c d e f g h i Prough RA, Clark BJ, Klinge CM (2016). "Novel mechanisms for DHEA action". J. Mol. Endocrinol. 56 (3): R139–55. doi:10.1530/JME-16-0013. PMID 26908835.
- ^ a b Wierman, Margaret E.; Arlt, Wiebke; Basson, Rosemary; Davis, Susan R.; Miller, Karen K.; Murad, Mohammad H.; Rosner, William; Santoro, Nanette. "Androgen Therapy in Women: A Reappraisal: An Endocrine Society Clinical Practice Guideline". The Journal of Clinical Endocrinology & Metabolism. 99 (10): 3489–510. doi:10.1210/jc.2014-2260. PMID 25279570.
- ^ Elraiyah, Tarig; Sonbol, Mohamad Bassam; Wang, Zhen; Khairalseed, Tagwa; Asi, Noor; Undavalli, Chaitanya; Nabhan, Mohammad; Altayar, Osama; Prokop, Larry; Montori, Victor M.; Murad, Mohammad Hassan. "The Benefits and Harms of Systemic Dehydroepiandrosterone (DHEA) in Postmenopausal Women With Normal Adrenal Function: A Systematic Review and Meta-analysis". The Journal of Clinical Endocrinology & Metabolism. 99 (10): 3536–42. doi:10.1210/jc.2014-2261. PMID 25279571.
- ^ J. Elks (14 November 2014). The Dictionary of Drugs: Chemical Data: Chemical Data, Structures and Bibliographies. Springer. pp. 641–. ISBN 978-1-4757-2085-3.
- ^ John W. Blunt; Murray H. G. Munro (19 September 2007). Dictionary of Marine Natural Products with CD-ROM. CRC Press. pp. 1075–. ISBN 978-0-8493-8217-8.
- ^ A. Kleemann; J. Engel; B. Kutscher; D. Reichert (14 May 2014). Pharmaceutical Substances, 5th Edition, 2009: Syntheses, Patents and Applications of the most relevant APIs. Thieme. pp. 2441–2442. ISBN 978-3-13-179525-0.
- ^ Martin Negwer; Hans-Georg Scharnow (2001). Organic-chemical drugs and their synonyms: (an international survey). Wiley-VCH. p. 1831. ISBN 978-3-527-30247-5.
3β-Hydroxyandrost-5-en-17-one hydrogen sulfate = (3β)-3-(Sulfooxy)androst-5-en-17-one. R: Sodium salt (1099-87-2). S: Astenile, Dehydroepiandrosterone sulfate sodium, DHA-S, DHEAS, KYH 3102, Mylis, PB 005, Prasterone sodium sulfate, Teloin
- ^ Jianqiu, Y. (1992). Clinical Application of Prasterone Sodium Sulfate. Chinese Journal of New Drugs, 5, 015.
- ^ Sakaguchi M, Sakai T, Adachi Y, Kawashima T, Awata N (1992). "The biological fate of sodium prasterone sulfate after vaginal administration. I. Absorption and excretion in rats". J. Pharmacobio-dyn. 15 (2): 67–73. PMID 1403604.
- ^ Sakai, T., Sakaguchi, M., Adachi, Y., Kawashima, T., & Awata, N. (1992). The Biological Fate of Sodium Prasterone Sulfate after Vaginal Administration II: Distribution after Single and Multiple Administration to Pregnant Rats. 薬物動態, 7(1), 87-101.
- ^ Walter K.H. Krause (30 November 2008). Cutaneous Manifestations of Endocrine Diseases. Springer Science & Business Media. pp. 79–. ISBN 978-3-540-88367-8.
- ^ Lazaridis I, Charalampopoulos I, Alexaki VI, Avlonitis N, Pediaditakis I, Efstathopoulos P, Calogeropoulou T, Castanas E, Gravanis A (2011). "Neurosteroid dehydroepiandrosterone interacts with nerve growth factor (NGF) receptors, preventing neuronal apoptosis". PLoS Biol. 9 (4): e1001051. doi:10.1371/journal.pbio.1001051. PMC 3082517. PMID 21541365.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Pediaditakis I, Iliopoulos I, Theologidis I, Delivanoglou N, Margioris AN, Charalampopoulos I, Gravanis A (2015). "Dehydroepiandrosterone: an ancestral ligand of neurotrophin receptors". Endocrinology. 156 (1): 16–23. doi:10.1210/en.2014-1596. PMID 25330101.
- ^ Gravanis A, Calogeropoulou T, Panoutsakopoulou V, Thermos K, Neophytou C, Charalampopoulos I (2012). "Neurosteroids and microneurotrophins signal through NGF receptors to induce prosurvival signaling in neuronal cells". Sci Signal. 5 (246): pt8. doi:10.1126/scisignal.2003387. PMID 23074265.
- ^ a b Robert Morfin (2 September 2003). DHEA and the Brain. CRC Press. pp. 28–. ISBN 978-0-203-30121-0.
- ^ a b Rainey WE, Nakamura Y (February 2008). "Regulation of the adrenal androgen biosynthesis". J. Steroid Biochem. Mol. Biol. 108 (3–5): 281–86. doi:10.1016/j.jsbmb.2007.09.015. PMC 2699571. PMID 17945481.
- ^ Lawrence H Lash (2005). Drug Metabolism and Transport: Molecular Methods and Mechanisms. Springer Science & Business Media. pp. 353–. ISBN 978-1-59259-832-8.
- ^ a b Dehydroepiandrosterone Sulfate (DHEA-S), Serum at Mayo Foundation For Medical Education And Research. Retrieved July 2012
- ^ Somani N, Harrison S, Bergfeld WF (2008). "The clinical evaluation of hirsutism". Dermatologic therapy. 21 (5): 376–91. doi:10.1111/j.1529-8019.2008.00219.x. PMID 18844715.
- ^ "Polycystic Ovarian Syndrome Workup". eMedicine. 25 October 2011. Retrieved 19 November 2011.
- ^ Vaudry H, Do Rego J-L, Burel D, et al. Neurosteroid Biosynthesis in the Brain of Amphibians. Frontiers in Endocrinology. 2011;2:79. doi:10.3389/fendo.2011.00079.
