Dehydroepiandrosterone: Difference between revisions
No edit summary |
No edit summary |
||
| Line 90: | Line 90: | ||
DHEA is transformed into DHEA-S by [[sulfation]] at the C3β position via the [[sulfotransferase]] [[enzyme]] [[SULT2A1]].<ref name="pmid17945481" /><ref name="Lash2005">{{cite book|author=Lawrence H Lash|title=Drug Metabolism and Transport: Molecular Methods and Mechanisms|url=https://books.google.com/books?id=-sK8NM_9UVsC&pg=PA353|year=2005|publisher=Springer Science & Business Media|isbn=978-1-59259-832-8|pages=353–}}</ref> This occurs naturally in the adrenal cortex and during [[first-pass metabolism]] in the [[liver]] and [[intestines]] when [[exogenous]] DHEA is administered orally.{{Citation needed|date=May 2017}} Levels of DHEA-S in circulation are approximately 250 to 300 times those of DHEA.<ref name="Weizman2008">{{cite book|author=Abraham Weizman|title=Neuroactive Steroids in Brain Function, Behavior and Neuropsychiatric Disorders: Novel Strategies for Research and Treatment|url=https://books.google.com/books?id=uABKkFdPjhkC&pg=PA229|date=1 February 2008|publisher=Springer Science & Business Media|isbn=978-1-4020-6854-6|pages=229–}}</ref> DHEA-S in turn can be converted back into DHEA in peripheral tissues via [[steroid sulfatase]] (STS).<ref name="Morfin2003">{{cite book|author=Robert Morfin|title=DHEA and the Brain|url=https://books.google.com/books?id=uZp62ctguF0C&pg=PA28|date=2 September 2003|publisher=CRC Press|isbn=978-0-203-30121-0|pages=28–}}</ref><ref name="Karasek2006">{{cite book|author=Michał Karasek|title=Aging and Age-related Diseases: The Basics|url=https://books.google.com/books?id=A_PN9oxKpP0C&pg=PA66|year=2006|publisher=Nova Publishers|isbn=978-1-59454-426-2|pages=66–}}</ref> |
DHEA is transformed into DHEA-S by [[sulfation]] at the C3β position via the [[sulfotransferase]] [[enzyme]] [[SULT2A1]].<ref name="pmid17945481" /><ref name="Lash2005">{{cite book|author=Lawrence H Lash|title=Drug Metabolism and Transport: Molecular Methods and Mechanisms|url=https://books.google.com/books?id=-sK8NM_9UVsC&pg=PA353|year=2005|publisher=Springer Science & Business Media|isbn=978-1-59259-832-8|pages=353–}}</ref> This occurs naturally in the adrenal cortex and during [[first-pass metabolism]] in the [[liver]] and [[intestines]] when [[exogenous]] DHEA is administered orally.{{Citation needed|date=May 2017}} Levels of DHEA-S in circulation are approximately 250 to 300 times those of DHEA.<ref name="Weizman2008">{{cite book|author=Abraham Weizman|title=Neuroactive Steroids in Brain Function, Behavior and Neuropsychiatric Disorders: Novel Strategies for Research and Treatment|url=https://books.google.com/books?id=uABKkFdPjhkC&pg=PA229|date=1 February 2008|publisher=Springer Science & Business Media|isbn=978-1-4020-6854-6|pages=229–}}</ref> DHEA-S in turn can be converted back into DHEA in peripheral tissues via [[steroid sulfatase]] (STS).<ref name="Morfin2003">{{cite book|author=Robert Morfin|title=DHEA and the Brain|url=https://books.google.com/books?id=uZp62ctguF0C&pg=PA28|date=2 September 2003|publisher=CRC Press|isbn=978-0-203-30121-0|pages=28–}}</ref><ref name="Karasek2006">{{cite book|author=Michał Karasek|title=Aging and Age-related Diseases: The Basics|url=https://books.google.com/books?id=A_PN9oxKpP0C&pg=PA66|year=2006|publisher=Nova Publishers|isbn=978-1-59454-426-2|pages=66–}}</ref> |
||
The [[terminal half-life]] of DHEA is short at only 15 to 30 minutes.<ref name="WhitePorterfield2013" /> In contrast, the terminal half-life of DHEA-S is far longer, at 7 to 10 hours.<ref name="WhitePorterfield2013" /> As DHEA-S can be converted back into DHEA, it serves as a circulating reservoir for DHEA, thereby extending the [[duration of action|duration]] of DHEA.<ref name="KalimiRegelson2000">{{cite book|author1=Mohammed Y. Kalimi|author2=William Regelson|title=Dehydroepiandrosterone (DHEA): Biochemical, Physiological and Clinical Aspects|url=https://books.google.com/books?id=Cn0tcGjTD8YC&pg=PA41|year=2000|publisher=Walter de Gruyter|isbn=978-3-11-016111-3|pages=41–}}</ref><ref name="Weizman2008" /> |
The [[terminal half-life]] of DHEA is short at only 15 to 30 minutes.<ref name="WhitePorterfield2013">{{cite book|author1=Bruce Alan White|author2=Susan P. Porterfield|title=Endocrine and Reproductive Physiology,Mosby Physiology Monograph Series (with Student Consult Online Access),4: Endocrine and Reproductive Physiology|url=https://books.google.com/books?id=zMb4uoiXzzcC&pg=PA164|year=2013|publisher=Elsevier Health Sciences|isbn=0-323-08704-3|pages=164–}}</ref> In contrast, the terminal half-life of DHEA-S is far longer, at 7 to 10 hours.<ref name="WhitePorterfield2013" /> As DHEA-S can be converted back into DHEA, it serves as a circulating reservoir for DHEA, thereby extending the [[duration of action|duration]] of DHEA.<ref name="KalimiRegelson2000">{{cite book|author1=Mohammed Y. Kalimi|author2=William Regelson|title=Dehydroepiandrosterone (DHEA): Biochemical, Physiological and Clinical Aspects|url=https://books.google.com/books?id=Cn0tcGjTD8YC&pg=PA41|year=2000|publisher=Walter de Gruyter|isbn=978-3-11-016111-3|pages=41–}}</ref><ref name="Weizman2008" /> |
||
[[Metabolite]]s of DHEA include DHEA-S, [[7α-hydroxy-DHEA]], [[7β-hydroxy-DHEA]], [[7-keto-DHEA]], [[7α-hydroxyepiandrosterone]], and [[7β-hydroxyepiandrosterone]], as well as [[5-androstenediol]] and [[4-androstenedione]].<ref name="pmid16524719" |
[[Metabolite]]s of DHEA include DHEA-S, [[7α-hydroxy-DHEA]], [[7β-hydroxy-DHEA]], [[7-keto-DHEA]], [[7α-hydroxyepiandrosterone]], and [[7β-hydroxyepiandrosterone]], as well as [[5-androstenediol]] and [[4-androstenedione]].<ref name="pmid16524719" /> |
||
====Pregnancy==== |
====Pregnancy==== |
||
| Line 122: | Line 122: | ||
DHEA and other adrenal androgens such as [[androstenedione]], although relatively weak androgens, are responsible for the androgenic effects of [[adrenarche]], such as early [[pubic hair|pubic]] and [[axillary hair]] growth, adult-type [[body odor]], increased oiliness of hair and skin, and mild [[acne]].<ref name="PescovitzEugster2004">{{cite book|author1=Ora Hirsch Pescovitz|author2=Erica A. Eugster|title=Pediatric Endocrinology: Mechanisms, Manifestations, and Management|url=https://books.google.com/books?id=9gvBlktAT6YC&pg=PA362|year=2004|publisher=Lippincott Williams & Wilkins|isbn=978-0-7817-4059-3|pages=362–}}</ref><ref name="Lifshitz2006">{{cite book|author=Fima Lifshitz|title=Pediatric Endocrinology: Growth, Adrenal, Sexual, Thyroid, Calcium, and Fluid Balance Disorders|url=https://books.google.com/books?id=1CTNBQAAQBAJ&pg=PA289|date=26 December 2006|publisher=CRC Press|isbn=978-1-4200-4272-6|pages=289–}}</ref><ref name="Salhan2011">{{cite book|author=Sudha Salhan|title=Textbook of Gynecology|url=https://books.google.com/books?id=YUYx1neUEIoC&pg=PA94|date=1 August 2011|publisher=JP Medical Ltd|isbn=978-93-5025-369-4|pages=94–}}</ref> Women with [[complete androgen insensitivity syndrome]] (CAIS), who have a non-functional [[androgen receptor]] (AR) and are immune to the androgenic effects of DHEA and other androgens, have absent or only sparse/scanty pubic and axillary hair and [[body hair]] in general, demonstrating the role of DHEA, [[testosterone]], and other androgens in body hair development at both adrenarche and [[pubarche]].<ref name="LaverySanfilippo2012">{{cite book|author1=J.P. Lavery|author2=J.S. Sanfilippo|title=Pediatric and Adolescent Obstetrics and Gynecology|url=https://books.google.com/books?id=l9XTBwAAQBAJ&pg=PA45|date=6 December 2012|publisher=Springer Science & Business Media|isbn=978-1-4612-5064-7|pages=45–}}</ref><ref name="NussbaumMcInnes2015">{{cite book|author1=Robert L. Nussbaum|author2=Roderick R. McInnes|author3=Huntington F Willard|title=Thompson & Thompson Genetics in Medicine|url=https://books.google.com/books?id=4yV1CQAAQBAJ&pg=PA102|date=28 April 2015|publisher=Elsevier Health Sciences|isbn=978-0-323-39206-8|pages=102–}}</ref><ref name="SetchellHudson2013">{{cite book|author1=Marcus E Setchell|author2=C. N. Hudson|title=Shaw's Textbook of Operative Gynaecology|url=https://books.google.com/books?id=XHcWNRVHWsEC&pg=PA129|date=4 April 2013|publisher=Elsevier Health Sciences|isbn=81-312-3481-9|pages=129–}}</ref><ref name="BissonnetteDalens2006">{{cite book|author1=Bruno Bissonnette|author2=Bernard Dalens|title=Syndromes: Rapid Recognition and Perioperative Implications|url=https://books.google.com/books?id=uRR1MYa-w5wC|date=20 July 2006|publisher=McGraw Hill Professional|isbn=978-0-07-135455-4|page=184}}</ref> |
DHEA and other adrenal androgens such as [[androstenedione]], although relatively weak androgens, are responsible for the androgenic effects of [[adrenarche]], such as early [[pubic hair|pubic]] and [[axillary hair]] growth, adult-type [[body odor]], increased oiliness of hair and skin, and mild [[acne]].<ref name="PescovitzEugster2004">{{cite book|author1=Ora Hirsch Pescovitz|author2=Erica A. Eugster|title=Pediatric Endocrinology: Mechanisms, Manifestations, and Management|url=https://books.google.com/books?id=9gvBlktAT6YC&pg=PA362|year=2004|publisher=Lippincott Williams & Wilkins|isbn=978-0-7817-4059-3|pages=362–}}</ref><ref name="Lifshitz2006">{{cite book|author=Fima Lifshitz|title=Pediatric Endocrinology: Growth, Adrenal, Sexual, Thyroid, Calcium, and Fluid Balance Disorders|url=https://books.google.com/books?id=1CTNBQAAQBAJ&pg=PA289|date=26 December 2006|publisher=CRC Press|isbn=978-1-4200-4272-6|pages=289–}}</ref><ref name="Salhan2011">{{cite book|author=Sudha Salhan|title=Textbook of Gynecology|url=https://books.google.com/books?id=YUYx1neUEIoC&pg=PA94|date=1 August 2011|publisher=JP Medical Ltd|isbn=978-93-5025-369-4|pages=94–}}</ref> Women with [[complete androgen insensitivity syndrome]] (CAIS), who have a non-functional [[androgen receptor]] (AR) and are immune to the androgenic effects of DHEA and other androgens, have absent or only sparse/scanty pubic and axillary hair and [[body hair]] in general, demonstrating the role of DHEA, [[testosterone]], and other androgens in body hair development at both adrenarche and [[pubarche]].<ref name="LaverySanfilippo2012">{{cite book|author1=J.P. Lavery|author2=J.S. Sanfilippo|title=Pediatric and Adolescent Obstetrics and Gynecology|url=https://books.google.com/books?id=l9XTBwAAQBAJ&pg=PA45|date=6 December 2012|publisher=Springer Science & Business Media|isbn=978-1-4612-5064-7|pages=45–}}</ref><ref name="NussbaumMcInnes2015">{{cite book|author1=Robert L. Nussbaum|author2=Roderick R. McInnes|author3=Huntington F Willard|title=Thompson & Thompson Genetics in Medicine|url=https://books.google.com/books?id=4yV1CQAAQBAJ&pg=PA102|date=28 April 2015|publisher=Elsevier Health Sciences|isbn=978-0-323-39206-8|pages=102–}}</ref><ref name="SetchellHudson2013">{{cite book|author1=Marcus E Setchell|author2=C. N. Hudson|title=Shaw's Textbook of Operative Gynaecology|url=https://books.google.com/books?id=XHcWNRVHWsEC&pg=PA129|date=4 April 2013|publisher=Elsevier Health Sciences|isbn=81-312-3481-9|pages=129–}}</ref><ref name="BissonnetteDalens2006">{{cite book|author1=Bruno Bissonnette|author2=Bernard Dalens|title=Syndromes: Rapid Recognition and Perioperative Implications|url=https://books.google.com/books?id=uRR1MYa-w5wC|date=20 July 2006|publisher=McGraw Hill Professional|isbn=978-0-07-135455-4|page=184}}</ref> |
||
As a [[neurosteroid]] and [[neurotrophin]], DHEA has important effects on the [[central nervous system]].<ref name="Weizman2008" |
As a [[neurosteroid]] and [[neurotrophin]], DHEA has important effects on the [[central nervous system]].<ref name="Weizman2008" /><ref name="GravanisMellon2011">{{cite book|author1=Achille G. Gravanis|author2=Synthia H. Mellon|title=Hormones in Neurodegeneration, Neuroprotection, and Neurogenesis|url=https://books.google.com/books?id=YmQAhOeaFtUC&pg=PT349|date=24 June 2011|publisher=John Wiley & Sons|isbn=978-3-527-63397-5|pages=349–}}</ref><ref>{{cite book|title=Sex difference in the human brain, their underpinnings and implications|url=https://books.google.com/books?id=JFpq6hYQRhQC&pg=PA127|date=3 December 2010|publisher=Elsevier|isbn=978-0-444-53631-0|pages=127–}}</ref> |
||
==Chemistry== |
==Chemistry== |
||
Revision as of 13:31, 30 May 2017
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Astenile, Cetovister, 17-Chetovis, Dastonil S, Deandros, Diandrone, Hormobago, 17-Hormoforin, 17-Ketovis, Mentalormon, Psicosterone[1] |
| Other names | Androst-5-en-3β-ol-17-one; 3β-Hydroxyandrost-5-en-17-one; 5,6-Didehydroepiandrosterone;[2] Dehydroisoepiandrosterone[1] |
| Routes of administration | By mouth, intramuscular injection (as prasterone enanthate) |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | 50%[3] |
| Metabolism | Hepatic[3] |
| Metabolites | • Androsterone[3] • Etiocholanolone[3] • DHEA sulfate[3] • Androstenedione[3] • Androstenediol[3] • Testosterone[3] • Androstanediol[3] |
| Elimination half-life | DHEA: 25 minutes[4] DHEA-S: 11 hours[4] |
| Excretion | Urinary |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.000.160 |
| Chemical and physical data | |
| Formula | C19H28O2 |
| Molar mass | 288.424 g/mol g·mol−1 |
| 3D model (JSmol) | |
| Melting point | 148.5 °C (299.3 °F) |
| |
| |
| (verify) | |
Dehydroepiandrosterone (DHEA), also known as androstenolone or as prasterone (INN), is an endogenous steroid hormone.[1][5] It is one of the most abundant circulating steroids in humans,[6] in whom it is produced in the adrenal glands,[7] the gonads, and the brain,[8] where it functions as a metabolic intermediate in the biosynthesis of the androgen and estrogen sex steroids.[5][9] However, DHEA also has a variety of potential biological effects in its own right, binding to an array of nuclear and cell surface receptors,[10] and acting as a neurosteroid and neurotrophin.[11]
Medical uses
In women with adrenal insufficiency and the healthy elderly there is insufficient evidence to support the use of DHEA.[12][13]
Menopause
DHEA is sometimes used as an androgen in hormone replacement therapy (HRT) for menopause. A long-lasting ester prodrug of DHEA, prasterone enanthate, is used in combination with estradiol valerate for this indication.[14][15][16][17][18][19]
Side effects
DHEA is produced naturally in the human body, but the long-term effects of its use are largely unknown.[20][21] In the short term, several studies have noted few adverse effects. In a study by Chang et al., DHEA was administered at a dose of 200 mg/day for 24 weeks with slight androgenic effects noted.[22] Another study utilized a dose up to 400 mg/day for 8 weeks with few adverse events reported.[23] A longer term study followed patients dosed with 50 mg of DHEA for 12 months with the number and severity of side effects reported to be small.[24] Another study delivered a dose of 50 mg of DHEA for 10 months with no serious adverse events reported.[25]
As a hormone precursor, there have been reports of side effects possibly caused by the hormone metabolites of DHEA.[21][26]
It is not known whether DHEA is safe for long-term use. Some researchers believe DHEA supplements might actually raise the risk of breast cancer, prostate cancer, heart disease, diabetes,[21] and stroke. DHEA may stimulate tumor growth in types of cancer that are sensitive to hormones, such as some types of breast, uterine, and prostate cancer.[21] DHEA may increase prostate swelling in men with benign prostatic hyperplasia (BPH), an enlarged prostate gland.[20]
DHEA is a steroid hormone. High doses may cause aggressiveness, irritability, trouble sleeping, and the growth of body or facial hair on women.[20] It also may stop menstruation and lower the levels of HDL ("good" cholesterol), which could raise the risk of heart disease.[20] Other reported side effects include acne, heart rhythm problems, liver problems, hair loss (from the scalp), and oily skin. It may also alter the body's regulation of blood sugar.[20]
DHEA may promote tamoxifen resistance.[20] Patients on hormone replacement therapy may have more estrogen-related side effects when taking DHEA. This supplement may also interfere with other medicines, and potential interactions between it and drugs and herbs are possible. [20]
DHEA is possibly unsafe for individuals experiencing pregnancy, breast-feeding, hormone sensitive conditions, liver problems, diabetes, depression or mood disorders, polycystic ovarian syndrome (PCOS), or cholesterol problems.[27]
Biochemistry
Biosynthesis
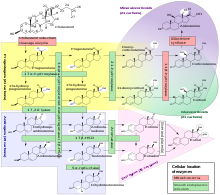
DHEA is produced in the zona reticularis of the adrenal cortex under the control of adrenocorticotropic hormone (ACTH) and by the gonads under the control of gonadotropin-releasing hormone (GnRH).[29][30] It is also produced in the brain.[31] DHEA is synthesized from cholesterol via the enzymes cholesterol side-chain cleavage enzyme (CYP11A1; P450scc) and 17α-hydroxylase/17,20-lyase (CYP17A1), with pregnenolone and 17α-hydroxypregnenolone as intermediates.[32] It is derived mostly from the adrenal cortex, with only about 10% being secreted from the gonads.[33][34][35] Approximately 50 to 70% of circulating DHEA originates from desulfation of DHEA sulfate (DHEA-S) in peripheral tissues.[33] DHEA-S itself originates almost exclusively from the adrenal cortex, with 95 to 100% being secreted from the adrenal cortex in women.[29][35]
Increasing endogenous production
Regular exercise is known to increase DHEA production in the body.[36][37] Calorie restriction has also been shown to increase DHEA in primates.[38] Some theorize that the increase in endogenous DHEA brought about by calorie restriction is partially responsible for the longer life expectancy known to be associated with calorie restriction.[39] Catalpol and a combination of acetyl-carnitine and propionyl-carnitine on 1:1 ratio also improves endogenous DHEA production and release due to direct cholinergic stimulation of CRH release and an increase of IGF-1 expression respectively.
Distribution
In the circulation, DHEA is mainly bound to albumin, with a small amount bound to sex hormone-binding globulin (SHBG).[40] The small remainder of DHEA is unbound and free in the circulation.[40]
DHEA easily crosses the blood–brain barrier into the central nervous system from the periphery.[31]
Metabolism
DHEA is transformed into DHEA-S by sulfation at the C3β position via the sulfotransferase enzyme SULT2A1.[32][41] This occurs naturally in the adrenal cortex and during first-pass metabolism in the liver and intestines when exogenous DHEA is administered orally.[citation needed] Levels of DHEA-S in circulation are approximately 250 to 300 times those of DHEA.[42] DHEA-S in turn can be converted back into DHEA in peripheral tissues via steroid sulfatase (STS).[43][44]
The terminal half-life of DHEA is short at only 15 to 30 minutes.[45] In contrast, the terminal half-life of DHEA-S is far longer, at 7 to 10 hours.[45] As DHEA-S can be converted back into DHEA, it serves as a circulating reservoir for DHEA, thereby extending the duration of DHEA.[46][42]
Metabolites of DHEA include DHEA-S, 7α-hydroxy-DHEA, 7β-hydroxy-DHEA, 7-keto-DHEA, 7α-hydroxyepiandrosterone, and 7β-hydroxyepiandrosterone, as well as 5-androstenediol and 4-androstenedione.[5]
Pregnancy
During pregnancy, DHEA-S is metabolized into the sulfates of 16α-hydroxy-DHEA and 15α-hydroxy-DHEA in the fetal liver as intermediates in the production of the estrogens estriol and estetrol.
Levels
Prior to puberty, DHEA and DHEA-S levels elevate upon differentiation of the zona reticularis of the adrenal cortex.[47] Peak levels of DHEA and DHEA-S are observed around age 20, which is followed by an age-dependent decline throughout life eventually back to prepubertal concentrations.[47] Plasma levels of DHEA in adult men are 10–25 nM, in premenopausal women are 5–30 nM, and in postmenopausal women are 2–20 nM.[47] Conversely, DHEA-S levels are an order of magnitude higher at 1–10 μM.[47] Levels of DHEA and DHEA-S decline to the lower nanomolar and micromolar ranges in men and women aged 60 to 80 years.[47]
Measurement
As almost all DHEA is derived from the adrenal glands, blood measurements of DHEA-S/DHEA are useful to detect excess adrenal activity as seen in adrenal cancer or hyperplasia, including certain forms of congenital adrenal hyperplasia. Women with polycystic ovary syndrome tend to have elevated levels of DHEA-S.[48]
Biological activity
Androgenic activity
Although it functions as an endogenous precursor to more potent androgens such as testosterone and DHT, DHEA has been found to possess some degree of androgenic activity in its own right, acting as a low affinity (Ki = 1 μM), weak partial agonist of the androgen receptor. However, its intrinsic activity at the receptor is quite weak, and on account of that, due to competition for binding with full agonists like testosterone, it can actually behave more like an antagonist depending on circulating testosterone and dihydrotestosterone (DHT) levels, and hence, like an antiandrogen. However, its affinity for the receptor is very low, and for that reason, is unlikely to be of much significance under normal circumstances.[49][50]
Estrogenic activity
In addition to its affinity for the androgen receptor, DHEA has also been found to bind to and activate the ERα and ERβ estrogen receptors with Ki values of 1.1 μM and 0.5 μM, respectively, and EC50 values of >1 μM and 200 nM, respectively. Though it was found to be a partial agonist of the ERα with a maximal efficacy of 30–70%, the concentrations required for this degree of activation make it unlikely that the activity of DHEA at this receptor is physiologically meaningful. Remarkably however, DHEA acts as a full agonist of the ERβ with a maximal response similar to or actually slightly greater than that of estradiol, and its levels in circulation and local tissues in the human body are high enough to activate the receptor to the same degree as that seen with circulating estradiol levels at somewhat higher than their maximal, non-ovulatory concentrations; indeed, when combined with estradiol with both at levels equivalent to those of their physiological concentrations, overall activation of the ERβ was doubled. As such, it has been proposed that DHEA may be an important and potentially major endogenous estrogen in the body.[10][49]
Neurotrophic activity
In 2011, the surprising discovery was made that DHEA, as well as DHEA-S, directly bind to and activate the TrkA and p75NTR, receptors of neurotrophins like nerve growth factor (NGF) and brain-derived neurotrophic factor (BDNF), with high affinity.[47][51] DHEA was subsequently also found to bind to the TrkB and TrkC with high affinity, though it notably activated the TrkC but not the TrkB.[47][52] DHEA and DHEA-S bound to these receptors with affinities that were in the low nanomolar range (around 5 nM), although the affinities were nonetheless approximately two orders of magnitude lower relative to highly potent polypeptide neurotrophins like NGF (0.01–0.1 nM).[47][51][52] In any case, DHEA and DHEA-S both circulate at requisite concentrations to activate these receptors and were thus identified as important endogenous neurotrophic factors.[47][51][51] They have since been labeled "steroidal microneurotrophins", due to their small-molecule and steroidal nature relative to their polypeptide neurotrophin counterparts.[53] Subsequent research has suggested that DHEA and/or DHEA-S may in fact be phylogenetically ancient "ancestral" ligands of the neurotrophin receptors from early on in the evolution of the nervous system.[47][52] The findings that DHEA binds to and potently activates neurotrophin receptors may explain the positive association between decreased circulating DHEA levels with age and age-related neurodegenerative diseases.[47][51]
Other activity
Unlike the case of the androgen and estrogen receptors, DHEA does not bind to or activate the progesterone, glucocorticoid, or mineralocorticoid receptors.[49][54]
Other nuclear receptor targets of DHEA include the PPARα, PXR, and CAR. In addition, it has been found to directly act on several membrane receptors, including the NMDA receptor as a positive allosteric modulator, the GABAA receptor as a negative allosteric modulator, and the σ1 receptor as an agonist. It is these actions that have conferred the label of a "neurosteroid" upon DHEA. Finally, DHEA is thought to regulate a handful of other proteins via indirect, genomic mechanisms, including the enzymes CYP2C11 and 11β-HSD1—the latter of which is essential for the biosynthesis of the glucocorticoids such as cortisol and has been suggested to be involved in the antiglucocorticoid effects of DHEA—and the carrier IGFBP1.[49][55]
Biological function
DHEA and other adrenal androgens such as androstenedione, although relatively weak androgens, are responsible for the androgenic effects of adrenarche, such as early pubic and axillary hair growth, adult-type body odor, increased oiliness of hair and skin, and mild acne.[56][57][58] Women with complete androgen insensitivity syndrome (CAIS), who have a non-functional androgen receptor (AR) and are immune to the androgenic effects of DHEA and other androgens, have absent or only sparse/scanty pubic and axillary hair and body hair in general, demonstrating the role of DHEA, testosterone, and other androgens in body hair development at both adrenarche and pubarche.[59][60][61][62]
As a neurosteroid and neurotrophin, DHEA has important effects on the central nervous system.[42][63][64]
Chemistry
DHEA is an androstane steroid and is known chemically as androst-5-en-3β-ol-17-one. It is the 5-dehydro analogue of epiandrosterone (5α-androstan-3β-ol-17-one) and is also known as 5-dehydroepiandrosterone or as δ5-epiandrosterone.
Isomers
The term "dehydroepiandrosterone" is ambiguous chemically because it does not include the specific positions within epiandrosterone at which hydrogen atoms are missing. DHEA itself is 5,6-didehydroepiandrosterone or 5-dehydroepiandrosterone. A number of naturally occurring isomers also exist and may have similar activities. Some isomers of DHEA are 1-dehydroepiandrosterone (1-androsterone) and 4-dehydroepiandrosterone. These isomers are also technically "DHEA", since they are dehydroepiandrosterones in which hydrogens are removed from the epiandrosterone skeleton.
Dehydroandrosterone (DHA) is the 3α-epimer of DHEA and is also an endogenous androgen.
Derivatives
DHEA is used medically as the C3β esters prasterone enanthate and prasterone sodium sulfate.[1]
Society and culture
Legality
United States
DHEA is legal to sell in the United States as a dietary supplement. It is currently grandfathered in as an "Old Dietary Ingredient" being on sale prior to 1994. DHEA is specifically exempted from the Anabolic Steroid Control Act of 1990 and 2004.[65] It is banned from use in athletic competition.
Canada
In Canada, DHEA is a Controlled Drug listed under Section 23 of Schedule IV of the Controlled Drugs and Substances Act[66] and as such is available by prescription only.
Australia
In Australia, a prescription is required to buy DHEA, where it is also comparatively expensive compared to off-the-shelf purchases in US supplement shops. Australian customs classify DHEA as an "anabolic steroid[s] or precursor[s]" and, as such, it is only possible to carry DHEA into the country through customs if one possesses an import permit which may be obtained if one has a valid prescription for the hormone.[67]
United Kingdom
DHEA (Prasterone) is listed as an anabolic steroid and is thus a class C controlled drug.
Sports and athletics
DHEA is a prohibited substance under the World Anti-Doping Code of the World Anti-Doping Agency,[68] which manages drug testing for Olympics and other sports. In January 2011, NBA player O. J. Mayo was given a 10-game suspension after testing positive for DHEA. Mayo termed his use of DHEA as "an honest mistake," saying the DHEA was in an over-the-counter supplement and that he was unaware the supplement was banned by the NBA.[69] Mayo is the seventh player to test positive for performance-enhancing drugs since the league began testing in 1999. Rashard Lewis, then with the Orlando Magic, tested positive for DHEA and was suspended 10 games before the start of the 2009-10 season.[70] 2008 Olympic 400 meter champion Lashawn Merritt has also tested positive for DHEA and was banned from the sport for 21 months.[71] Yulia Efimova, who holds the world record pace for both the 50-meter and 200-meter breaststroke, and won the bronze medal in the 200-meter breaststroke in the 2012 London Olympic Games, tested positive for DHEA in an out-of-competition doping test.[72] In 2016 MMA fighter Fabio Maldonado revealed he was taking DHEA during his time with the UFC.[73]
Marketing
In the United States, DHEA or DHEA-S have been advertised with claims that they may be beneficial for a wide variety of ailments. DHEA and DHEA-S are readily available in the United States, where they are marketed as over-the-counter dietary supplements.[74]
Research
DHEA has been studied in several conditions.
Anabolic uses
Body composition
A meta-analysis of intervention studies shows that DHEA supplementation in elderly men can induce a small but significant positive effect on body composition that is strictly dependent on DHEA conversion into its bioactive metabolites such as androgens or estrogens.[75]
Cancer
There is no evidence DHEA is of benefit in treating or preventing cancer.[20] Although DHEA is postulated as an inhibitor towards glucose-6-phosphate dehydrogenase (G6PD) and suppresses leukemia cell proliferation in vitro,[76][77] DHEA may enhance G6PD mRNA expression, confounding its inhibitory effects.[78]
Cardiovascular disease
A review in 2003 found the then-extant evidence sufficient to suggest that low serum levels of DHEA-S may be associated with coronary heart disease in men, but insufficient to determine whether DHEA supplementation would have any cardiovascular benefit.[79]
Drug addiction
A double-blind, placebo-controlled study in adult polydrug users in a detoxification program showed the efficacy of DHEA treatment combined with psychosocial enrichment and after-care. DHEA administration positively affected decision-making, mood and well-being as early as one month into treatment, and had a long-lasting preventive effect on relapse to drug use. In a 16-month follow-up, relapse rates of DHEA-treated subjects were only 11.5%. No adverse symptoms were found. These findings demonstrate the long-term effect of DHEA on drug relapse [80]
Lupus
There is some evidence of short-term benefit in those with systemic lupus erythematosus but little evidence of long-term benefit or safety.[81]
Memory
DHEA supplementation has not been found to be useful for memory function in normal middle aged or older adults.[82] It has been studied as a treatment for Alzheimer's disease, but there is no evidence that it is effective.[83]
Mood
A few small, short term clinical studies have found that DHEA improves mood but its long-term efficacy and safety, and how it compares to antidepressants, was unknown as of 2015.[84][85]
Strength
Evidence is inconclusive in regards to the effect of DHEA on strength in the elderly.[86]
In middle-aged men, no significant effect of DHEA supplementation on lean body mass, strength, or testosterone levels was found in a randomized placebo-controlled trial.[87]
See also
- 3α-Androstanediol
- Androsterone
- Etiocholanolone
- List of unproven and disproven cancer treatments
- Pregnenolone sulfate
References
- ^ a b c d J. Elks (14 November 2014). The Dictionary of Drugs: Chemical Data: Chemical Data, Structures and Bibliographies. Springer. pp. 641–. ISBN 978-1-4757-2085-3.
- ^ James Devillers (27 April 2009). Endocrine Disruption Modeling. CRC Press. pp. 339–. ISBN 978-1-4200-7636-3.
- ^ a b c d e f g h i Melanie Johns Cupp; Timothy S. Tracy (10 December 2002). Dietary Supplements: Toxicology and Clinical Pharmacology. Springer Science & Business Media. pp. 135–. ISBN 978-1-59259-303-3.
- ^ a b B.J. Oddens; A. Vermeulen (15 November 1996). Androgens and the Aging Male. CRC Press. pp. 5–. ISBN 978-1-85070-763-9.
- ^ a b c Mo Q, Lu SF, Simon NG (April 2006). "Dehydroepiandrosterone and its metabolites: differential effects on androgen receptor trafficking and transcriptional activity". J. Steroid Biochem. Mol. Biol. 99 (1): 50–8. doi:10.1016/j.jsbmb.2005.11.011. PMID 16524719.
- ^ William F Ganong MD, 'Review of Medical Physiology', 22nd Ed, McGraw Hill, 2005, p. 362.
- ^ The Merck Index, 13th Edition, 7798
- ^ Schulman, Robert A.; Dean, Carolyn (2007). Solve It With Supplements. New York City: Rodale, Inc. p. 100. ISBN 978-1-57954-942-8.
DHEA (Dehydroepiandrosterone) is a common hormone produced in the adrenal glands, the gonads, and the brain.
- ^ Thomas Scott (1996). Concise Encyclopedia Biology. Walter de Gruyter. p. 49. ISBN 978-3-11-010661-9. Retrieved 25 May 2012.
- ^ a b Webb SJ, Geoghegan TE, Prough RA, Michael Miller KK (2006). "The biological actions of dehydroepiandrosterone involves multiple receptors". Drug Metabolism Reviews. 38 (1–2): 89–116. doi:10.1080/03602530600569877. PMC 2423429. PMID 16684650.
- ^ Friess E, Schiffelholz T, Steckler T, Steiger A (December 2000). "Dehydroepiandrosterone--a neurosteroid". European Journal of Clinical Investigation. 30 Suppl 3: 46–50. doi:10.1046/j.1365-2362.2000.0300s3046.x. PMID 11281367.
- ^ Arlt, W (September 2004). "Dehydroepiandrosterone and ageing". Best practice & research. Clinical endocrinology & metabolism. 18 (3): 363–80. doi:10.1016/j.beem.2004.02.006. PMID 15261843.
- ^ Alkatib, AA; Cosma, M; Elamin, MB; Erickson, D; Swiglo, BA; Erwin, PJ; Montori, VM (October 2009). "A systematic review and meta-analysis of randomized placebo-controlled trials of DHEA treatment effects on quality of life in women with adrenal insufficiency". The Journal of Clinical Endocrinology and Metabolism. 94 (10): 3676–81. doi:10.1210/jc.2009-0672. PMID 19773400.
- ^ https://www.drugs.com/international/gynodian-depot.html
- ^ J. Horsky; J. Presl (6 December 2012). Ovarian Function and its Disorders: Diagnosis and Therapy. Springer Science & Business Media. pp. 146–. ISBN 978-94-009-8195-9.
- ^ D. Platt (6 December 2012). Geriatrics 3: Gynecology · Orthopaedics · Anesthesiology · Surgery · Otorhinolaryngology · Ophthalmology · Dermatology. Springer Science & Business Media. pp. 6–. ISBN 978-3-642-68976-5.
- ^ S. Campbell (6 December 2012). The Management of the Menopause & Post-Menopausal Years: The Proceedings of the International Symposium held in London 24–26 November 1975 Arranged by the Institute of Obstetrics and Gynaecology, The University of London. Springer Science & Business Media. pp. 395–. ISBN 978-94-011-6165-7.
- ^ Carrie Bagatell; William J. Bremner (27 May 2003). Androgens in Health and Disease. Springer Science & Business Media. pp. 277–. ISBN 978-1-59259-388-0.
- ^ Frigo P, Eppel W, Asseryanis E, Sator M, Golaszewski T, Gruber D, Lang C, Huber J (1995). "The effects of hormone substitution in depot form on the uterus in a group of 50 perimenopausal women--a vaginosonographic study". Maturitas. 21 (3): 221–5. doi:10.1016/0378-5122(94)00893-c. PMID 7616871.
- ^ a b c d e f g h Ades TB, ed. (2009). DHEA (2nd ed.). American Cancer Society. pp. 729–33. ISBN 9780944235713.
{{cite book}}:|work=ignored (help) - ^ a b c d Medscape (2010). "DHEA Oral". Drug Reference. WebMD LLC. Retrieved 18 February 2010.
- ^ Chang DM, Lan JL, Lin HY, Luo SF (2002). "Dehydroepiandrosterone treatment of women with mild-to-moderate systemic lupus erythematosus: a multicenter randomized, double-blind, placebo-controlled trial". Arthritis Rheum. 46 (11): 2924–27. doi:10.1002/art.10615. PMID 12428233.
- ^ Rabkin JG, McElhiney MC, Rabkin R, McGrath PJ, Ferrando SJ (2006). "Placebo-controlled trial of dehydroepiandrosterone (DHEA) for treatment of nonmajor depression in patients with HIV/AIDS". Am J Psychiatry. 163 (1): 59–66. doi:10.1176/appi.ajp.163.1.59. PMID 16390890.
- ^ Brooke AM, Kalingag LA, Miraki-Moud F, Camacho-Hübner C, Maher KT, Walker DM, Hinson JP, Monson JP (2006). "Dehydroepiandrosterone improves psychological well-being in male and female hypopituitary patients on maintenance growth hormone replacement". J Clin Endocrinol Metab. 91 (10): 3773–79. doi:10.1210/jc.2006-0316. PMID 16849414.
- ^ Villareal DT, Holloszy JO (2006). "DHEA enhances effects of weight training on muscle mass and strength in elderly women and men". Am J Physiol Endocrinol Metab. 291 (5): E1003–08. doi:10.1152/ajpendo.00100.2006.
- ^ Medline Plus. "DHEA". Drugs and Supplements Information. National Library of Medicine. Retrieved 18 February 2010.
- ^ "DHEA: Side effects and safety". WebMD. Retrieved 24 July 2012.
- ^ Häggström, Mikael; Richfield, David (2014). "Diagram of the pathways of human steroidogenesis". WikiJournal of Medicine. 1 (1). doi:10.15347/wjm/2014.005. ISSN 2002-4436.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ a b Risto Erkkola (2006). The Menopause. Elsevier. pp. 5–. ISBN 978-0-444-51830-9.
- ^ Bernhard Kleine; Winfried G. Rossmanith (11 February 2016). Hormones and the Endocrine System: Textbook of Endocrinology. Springer. pp. 264–265. ISBN 978-3-319-15060-4.
- ^ a b Joseph E. Pizzorno (2013). Textbook of Natural Medicine. Elsevier Health Sciences. pp. 711–. ISBN 1-4377-2333-0.
- ^ a b Rainey WE, Nakamura Y (February 2008). "Regulation of the adrenal androgen biosynthesis". J. Steroid Biochem. Mol. Biol. 108 (3–5): 281–86. doi:10.1016/j.jsbmb.2007.09.015. PMC 2699571. PMID 17945481.
- ^ a b Robert A. Adler (14 December 2009). Osteoporosis: Pathophysiology and Clinical Management. Springer Science & Business Media. pp. 387–. ISBN 978-1-934115-19-0.
- ^ Wolf-Bernhard Schill; Frank H. Comhaire; Timothy B. Hargreave (26 August 2006). Andrology for the Clinician. Springer Science & Business Media. pp. 243–. ISBN 978-3-540-33713-3.
- ^ a b Dimitrios A. Linos; Jon A. van Heerden (5 December 2005). Adrenal Glands: Diagnostic Aspects and Surgical Therapy. Springer Science & Business Media. pp. 161–. ISBN 978-3-540-26861-1.
- ^ Filaire, E; Duché, P; Lac, G (1998). "Effects of amount of training on the saliva concentrations of cortisol, dehydroepiandrosterone and on the dehydroepiandrosterone: Cortisol concentration ratio in women over 16 weeks of training". Eur. J. Appl. Physiol. Occup. Physiol. 78 (5): 466–71. doi:10.1007/s004210050447. PMID 9809849.
- ^ Copeland, J. L.; Consitt, L. A.; Tremblay, M. S. (2002). "Hormonal Responses to Endurance and Resistance Exercise in Females Aged 19–69 Years". J. Gerontol. A. Biol. Sci. Med. Sci. 57 (4): B158–65. doi:10.1093/gerona/57.4.B158.
- ^ Mattison, Julie A.; Lane, Mark A.; Roth, George S.; Ingram, Donald K. (2003). "Calorie restriction in rhesus monkeys". Experimental Gerontology. 38 (1–2): 35–46. doi:10.1016/S0531-5565(02)00146-8. PMID 12543259..
- ^ Roberts, E. (1999). "The importance of dehydroepiandrosterone sulfate in the blood of primates: a longer and healthier life?". Biochemical Pharmacology. 57 (4): 329–46. doi:10.1016/S0006-2952(98)00246-9. PMID 9933021..
- ^ a b Paul M. Coates; M. Coates Paul; Marc Blackman (29 December 2004). Encyclopedia of Dietary Supplements (Print). CRC Press. pp. 169–. ISBN 978-0-8247-5504-1.
{{cite book}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Lawrence H Lash (2005). Drug Metabolism and Transport: Molecular Methods and Mechanisms. Springer Science & Business Media. pp. 353–. ISBN 978-1-59259-832-8.
- ^ a b c Abraham Weizman (1 February 2008). Neuroactive Steroids in Brain Function, Behavior and Neuropsychiatric Disorders: Novel Strategies for Research and Treatment. Springer Science & Business Media. pp. 229–. ISBN 978-1-4020-6854-6.
- ^ Robert Morfin (2 September 2003). DHEA and the Brain. CRC Press. pp. 28–. ISBN 978-0-203-30121-0.
- ^ Michał Karasek (2006). Aging and Age-related Diseases: The Basics. Nova Publishers. pp. 66–. ISBN 978-1-59454-426-2.
- ^ a b Bruce Alan White; Susan P. Porterfield (2013). Endocrine and Reproductive Physiology,Mosby Physiology Monograph Series (with Student Consult Online Access),4: Endocrine and Reproductive Physiology. Elsevier Health Sciences. pp. 164–. ISBN 0-323-08704-3.
- ^ Mohammed Y. Kalimi; William Regelson (2000). Dehydroepiandrosterone (DHEA): Biochemical, Physiological and Clinical Aspects. Walter de Gruyter. pp. 41–. ISBN 978-3-11-016111-3.
- ^ a b c d e f g h i j k Prough RA, Clark BJ, Klinge CM (2016). "Novel mechanisms for DHEA action". J. Mol. Endocrinol. 56 (3): R139–55. doi:10.1530/JME-16-0013. PMID 26908835.
- ^ Banaszewska B, Spaczyński RZ, Pelesz M, Pawelczyk L (2003). "Incidence of elevated LH/FSH ratioin polycystic ovary syndrome women with normo- and hyperinsulinemia". Annales Academiae Medicae Bialostocensis. 48.
- ^ a b c d Chen F, Knecht K, Birzin E, et al. (November 2005). "Direct agonist/antagonist functions of dehydroepiandrosterone". Endocrinology. 146 (11): 4568–76. doi:10.1210/en.2005-0368. PMID 15994348.
- ^ Gao W, Bohl CE, Dalton JT (September 2005). "Chemistry and structural biology of androgen receptor". Chemical Reviews. 105 (9): 3352–70. doi:10.1021/cr020456u. PMC 2096617. PMID 16159155.
- ^ a b c d e Lazaridis I, Charalampopoulos I, Alexaki VI, Avlonitis N, Pediaditakis I, Efstathopoulos P, Calogeropoulou T, Castanas E, Gravanis A (2011). "Neurosteroid dehydroepiandrosterone interacts with nerve growth factor (NGF) receptors, preventing neuronal apoptosis". PLoS Biol. 9 (4): e1001051. doi:10.1371/journal.pbio.1001051. PMC 3082517. PMID 21541365.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ a b c Pediaditakis I, Iliopoulos I, Theologidis I, Delivanoglou N, Margioris AN, Charalampopoulos I, Gravanis A (2015). "Dehydroepiandrosterone: an ancestral ligand of neurotrophin receptors". Endocrinology. 156 (1): 16–23. doi:10.1210/en.2014-1596. PMID 25330101.
- ^ Gravanis A, Calogeropoulou T, Panoutsakopoulou V, Thermos K, Neophytou C, Charalampopoulos I (2012). "Neurosteroids and microneurotrophins signal through NGF receptors to induce prosurvival signaling in neuronal cells". Sci Signal. 5 (246): pt8. doi:10.1126/scisignal.2003387. PMID 23074265.
- ^ Lindschau C, Kirsch T, Klinge U, Kolkhof P, Peters I, Fiebeler A (September 2011). "Dehydroepiandrosterone-induced phosphorylation and translocation of FoxO1 depend on the mineralocorticoid receptor". Hypertension. 58 (3): 471–78. doi:10.1161/HYPERTENSIONAHA.111.171280. PMID 21747041.
- ^ Kalimi M, Shafagoj Y, Loria R, Padgett D, Regelson W (February 1994). "Anti-glucocorticoid effects of dehydroepiandrosterone (DHEA)". Molecular and Cellular Biochemistry. 131 (2): 99–104. doi:10.1007/BF00925945. PMID 8035785.
- ^ Ora Hirsch Pescovitz; Erica A. Eugster (2004). Pediatric Endocrinology: Mechanisms, Manifestations, and Management. Lippincott Williams & Wilkins. pp. 362–. ISBN 978-0-7817-4059-3.
- ^ Fima Lifshitz (26 December 2006). Pediatric Endocrinology: Growth, Adrenal, Sexual, Thyroid, Calcium, and Fluid Balance Disorders. CRC Press. pp. 289–. ISBN 978-1-4200-4272-6.
- ^ Sudha Salhan (1 August 2011). Textbook of Gynecology. JP Medical Ltd. pp. 94–. ISBN 978-93-5025-369-4.
- ^ J.P. Lavery; J.S. Sanfilippo (6 December 2012). Pediatric and Adolescent Obstetrics and Gynecology. Springer Science & Business Media. pp. 45–. ISBN 978-1-4612-5064-7.
- ^ Robert L. Nussbaum; Roderick R. McInnes; Huntington F Willard (28 April 2015). Thompson & Thompson Genetics in Medicine. Elsevier Health Sciences. pp. 102–. ISBN 978-0-323-39206-8.
- ^ Marcus E Setchell; C. N. Hudson (4 April 2013). Shaw's Textbook of Operative Gynaecology. Elsevier Health Sciences. pp. 129–. ISBN 81-312-3481-9.
- ^ Bruno Bissonnette; Bernard Dalens (20 July 2006). Syndromes: Rapid Recognition and Perioperative Implications. McGraw Hill Professional. p. 184. ISBN 978-0-07-135455-4.
- ^ Achille G. Gravanis; Synthia H. Mellon (24 June 2011). Hormones in Neurodegeneration, Neuroprotection, and Neurogenesis. John Wiley & Sons. pp. 349–. ISBN 978-3-527-63397-5.
- ^ Sex difference in the human brain, their underpinnings and implications. Elsevier. 3 December 2010. pp. 127–. ISBN 978-0-444-53631-0.
- ^ "Drug Scheduling Actions – 2005". Drug Enforcement Administration.
- ^ Health Canada, DHEA listing in the Ingredient Database
- ^ Therapeutic Goods Administration, Personal Importation Scheme
- ^ World Anti-Doping Agency
- ^ Memphis Grizzlies' O. J. Mayo gets 10-game drug suspension, ESPN, January 27, 2011.
- ^ Memphis Grizzlies' O. J. Mayo suspended 10 games for violating NBA anti-drug program
- ^ "US 400m star LaShawn Merritt fails drug test". BBC Sport. 22 April 2010.
- ^ Russian Olympic Medal-Winning Swimmer Efimova Fails Doping Test – Report
- ^ Fabio Maldonado plans to use DHEA for Fedor match, admits use in UFC
- ^ Calfee, R.; Fadale, P. (March 2006). "Popular ergogenic drugs and supplements in young athletes". Pediatrics. 117 (3): e577–89. doi:10.1542/peds.2005-1429. PMID 16510635.
In 2004, a new Steroid Control Act that placed androstenedione under Schedule III of controlled substances effective January 2005 was signed. DHEA was not included in this act and remains an over-the-counter nutritional supplement.
- ^ Corona, G; Rastrelli, G; Giagulli, VA; Sila, A; Sforza, A; Forti, G; Mannucci, E; Maggi, M (2013). "Dehydroepiandrosterone supplementation in elderly men: a meta-analysis study of placebo-controlled trials". J. Clin. Endocrinol. Metab. 98: 3615–26. doi:10.1210/jc.2013-1358. PMID 23824417.
- ^ Di Monaco M, Pizzini A, Gatto V, Leonardi L, Gallo M, Brignardello E, Boccuzzi G (1997). "Role of glucose-6-phosphate dehydrogenase inhibition in the antiproliferative effects of dehydroepiandrosterone on human breast cancer cells". Br J Cancer. 75: 589–92. doi:10.1038/bjc.1997.102. PMC 2063293. PMID 9052415.
- ^ Xu SN, Wang TS, Li X, Wang YP (Sep 2016). "SIRT2 activates G6PD to enhance NADPH production and promote leukaemia cell proliferation". Sci Rep. 6: 32734. doi:10.1038/srep32734. PMC 5009355. PMID 27586085.
- ^ Hecker PA, Leopold JA, Gupte SA, Recchia FA, Stanley WC (Feb 2013). "Impact of glucose-6-phosphate dehydrogenase deficiency on the pathophysiology of cardiovascular disease". Am J Physiol Heart Circ Physiol. 304: H491-500. doi:10.1152/ajpheart.00721.2012. PMC 3566485. PMID 23241320.
- ^ Thijs L, Fagard R, Forette F, Nawrot T, Staessen JA (October 2003). "Are low dehydroepiandrosterone sulphate levels predictive for cardiovascular diseases? A review of prospective and retrospective studies". Acta Cardiol. 58 (5): 403–10. doi:10.2143/AC.58.5.2005304. PMID 14609305.
- ^ Ohana, D; Maayan, R; Delayahu, Y; Roska, P; Ponizovsky, AM; Weizman, A; Yadid, G; Yechiam, E (March 2015). "Effect of dehydroepiandrosterone add-on therapy on mood, decision making and subsequent relapse of polydrug=Addiction Biology :". 21 (4): 885–94. PMID 25818161.
{{cite journal}}: Cite journal requires|journal=(help) - ^ Crosbie, D; Black, C; McIntyre, L; Royle, PL; Thomas, S (Oct 17, 2007). Crosbie, David (ed.). "Dehydroepiandrosterone for systemic lupus erythematosus". Cochrane database of systematic reviews (Online) (4): CD005114. doi:10.1002/14651858.CD005114.pub2. PMID 17943841.
- ^ Grimley Evans, J; Malouf, R; Huppert, F; van Niekerk, JK (Oct 18, 2006). Malouf, Reem (ed.). "Dehydroepiandrosterone (DHEA) supplementation for cognitive function in healthy elderly people". Cochrane database of systematic reviews (Online) (4): CD006221. doi:10.1002/14651858.CD006221. PMID 17054283.
- ^ Fuller, SJ; Tan, RS; Martins, RN (September 2007). "Androgens in the etiology of Alzheimer's disease in aging men and possible therapeutic interventions". Journal of Alzheimer's disease : JAD. 12 (2): 129–42. PMID 17917157.
- ^ Pluchino, N; Drakopoulos, P; Bianchi-Demicheli, F; Wenger, JM; Petignat, P; Genazzani, AR (January 2015). "Neurobiology of DHEA and effects on sexuality, mood and cognition". The Journal of steroid biochemistry and molecular biology. 145: 273–80. doi:10.1016/j.jsbmb.2014.04.012. PMID 24892797.
- ^ Maric, NP; Adzic, M (September 2013). "Pharmacological modulation of HPA axis in depression - new avenues for potential therapeutic benefits" (PDF). Psychiatria Danubina. 25 (3): 299–305. PMID 24048401.
- ^ Baker, WL; Karan, S; Kenny, AM (June 2011). "Effect of dehydroepiandrosterone on muscle strength and physical function in older adults: a systematic review". Journal of the American Geriatrics Society. 59 (6): 997–1002. doi:10.1111/j.1532-5415.2011.03410.x. PMID 21649617.
- ^ Wallace, M. B.; Lim, J.; Cutler, A.; Bucci, L. (1999). "Effects of dehydroepiandrosterone vs androstenedione supplementation in men". Medicine and Science in Sports and Exercise. 31 (12): 1788–92. doi:10.1097/00005768-199912000-00014. PMID 10613429.
External links
- Information on DHEA from the Mayo Clinic
- DHEA in elderly women and DHEA or testosterone in elderly men, published in the New England Journal of Medicine in 2006. "Neither DHEA nor low-dose testosterone replacement in elderly people has physiologically relevant beneficial effects on body composition, physical performance, insulin sensitivity, or quality of life."
- DHEA, from the Skeptic's Dictionary
- ChemSub Online: Dehydroepiandrosterone - DHEA
- Androgens and anabolic steroids
- Androstanes
- Estrogens
- Dietary supplements
- Hormones of the hypothalamus-pituitary-gonad axis
- GABAA receptor negative allosteric modulators
- Neurosteroids
- Neurotrophins
- NMDA receptor agonists
- Pheromones
- Pregnane X receptor agonists
- Sex hormones
- Sigma agonists
- World Anti-Doping Agency prohibited substances
