P-glycoprotein
ABCB1 at EBI Gene Expression Atlas
| ||
| ABCB1 is differentially expressed in 97 experiments [93 up/106 dn]: 26 organism parts: kidney [2 up/0 dn], bone marrow [0 up/2 dn], ...; 29 disease states: normal [10 up/3 dn], glioblastoma [0 up/2 dn], ...; 30 cell types, 22 cell lines, 11 compound treatments and 16 other conditions. | ||
| Factor Value | Factor | Up/Down |
| Legend: | ||
| Normal | Disease state | 10/3 |
| None | Compound treatment | 3/0 |
| Stromal cell | Cell type | 1/2 |
| Kidney | Cell type | 2/0 |
| MDA-MB-231 | Cell line | 0/2 |
| Glioblastoma | Disease state | 0/2 |
| Epithelial cell | Cell type | 0/2 |
| HeLa | Cell line | 0/2 |
| Primary | Disease staging | 2/0 |
| Bone marrow | Organism part | 0/2 |
| ABCB1 expression data in ATLAS | ||
P-glycoprotein 1 (permeability glycoprotein, abbreviated as P-gp or Pgp) also known as multidrug resistance protein 1 (MDR1) or ATP-binding cassette sub-family B member 1 (ABCB1) or cluster of differentiation 243 (CD243) is an important protein of the cell membrane that pumps many foreign substances out of cells. More formally, it is an ATP-dependent efflux pump with broad substrate specificity. It exists in animals, fungi and bacteria and likely evolved as a defense mechanism against harmful substances.
P-gp is extensively distributed and expressed in the intestinal epithelium where it pumps xenobiotics (such as toxins or drugs) back into the intestinal lumen, in liver cells where it pumps them into bile ducts, in the cells of the proximal tubule of the kidney where it pumps them into urine-conducting ducts, and in the capillary endothelial cells composing the blood–brain barrier and blood-testis barrier, where it pumps them back into the capillaries.
P-gp is a glycoprotein that in humans is encoded by the ABCB1 gene.[4] P-gp is a well-characterized ABC-transporter (which transports a wide variety of substrates across extra- and intracellular membranes) of the MDR/TAP subfamily.[5] The normal excretion of xenobiotics back into the gut lumen by P-gp pharmacokinetically reduces the efficacy of some pharmaceutical drugs (which are said to be P-gp substrates). In addition, some cancer cells also express large amounts of P-gp, further amplifying that effect and rendering these cancers multidrug resistant. Many drugs inhibit P-gp, typically incidentally rather than as their main mechanism of action; some foods do as well. Any such substance can sometimes be called a P-gp inhibitor.
P-gp was discovered in 1971 by Victor Ling.
Function
The protein belongs to the superfamily of ATP-binding cassette (ABC) transporters. ABC proteins transport various molecules across extra- and intra-cellular membranes. ABC genes are divided into seven distinct subfamilies (ABC1, MDR/TAP, MRP, ALD, OABP, GCN20, White). This protein is a member of the MDR/TAP subfamily. Members of the MDR/TAP subfamily are involved in multidrug resistance. P-gp is an ATP-dependent drug efflux pump for xenobiotic compounds with broad substrate specificity. It is responsible for decreased drug accumulation in multidrug-resistant cells and often mediates the development of resistance to anticancer drugs. This protein also functions as a transporter in the blood–brain barrier.[6]
P-gp transports various substrates across the cell membrane including:
- Drugs such as colchicine, tacrolimus and quinidine
- Chemotherapeutic agents such as etoposide, doxorubicin, and vinblastine
- Lipids
- Steroids
- Xenobiotics
- Peptides
- Bilirubin
- Cardiac glycosides like digoxin
- Immunosuppressive agents
- Glucocorticoids like dexamethasone
- HIV-type 1 antiretroviral therapy agents like protease inhibitors and nonnucleoside reverse transcriptase inhibitors.
Its ability to transport the above substrates accounts for the many roles of P-gp including:
- Regulating the distribution and bioavailability of drugs
- Increased intestinal expression of P-glycoprotein can reduce the absorption of drugs that are substrates for P-glycoprotein. Thus, there is a reduced bioavailability, and therapeutic plasma concentrations are not attained. On the other hand, supratherapeutic plasma concentrations and drug toxicity may result because of decreased P-glycoprotein expression
- Active cellular transport of antineoplastics resulting in multidrug resistance to these drugs
- The removal of toxic metabolites and xenobiotics from cells into urine, bile, and the intestinal lumen
- The transport of compounds out of the brain across the blood–brain barrier
- Digoxin uptake
- Prevention of ivermectin and loperamide entry into the central nervous system
- The migration of dendritic cells
- Protection of hematopoietic stem cells from toxins.[5]
It is inhibited by many drugs, such as Amiodarone, Azithromycin, Captopril, Clarithromycin, Cyclosporine, Piperine, Quercetin, Quinidine, Quinine, Reserpine, Ritonavir, Tariquidar, and Verapamil[7].
Structure
P-gp is a 170 kDa transmembrane glycoprotein, which includes 10-15 kDa of N-terminal glycosylation. The N-terminal half of the molecule contains 6 transmembrane domains, followed by a large cytoplasmic domain with an ATP-binding site, and then a second section with 6 transmembrane domains and an ATP-binding site that shows over 65% of amino acid similarity with the first half of the polypeptide.[8] In 2009, the first structure of a mammalian P-glycoprotein was solved (3G5U).[9] The structure was derived from the mouse MDR3 gene product heterologously expressed in Pichia pastoris yeast. The structure of mouse P-gp is similar to structures of the bacterial ABC transporter MsbA (3B5W and 3B5X)[10] that adopt an inward facing conformation that is believed to be important for binding substrate along the inner leaflet of the membrane. Additional structures (3G60 and 3G61) of P-gp were also solved revealing the binding site(s) of two different cyclic peptide substrate/inhibitors. The promiscuous binding pocket of P-gp is lined with aromatic amino acid side chains. However, the murine P-gp structure is incomplete, missing an intermediate linker sequence proved to be essential for substrate recognition and ATP hydrolysis. Through Molecular Dynamic (MD) simulations, this sequence was proved to have a direct impact in the transporter's structural stability (in the nucleotide-binding domains) and defining a lower boundary for the internal drug-binding pocket.[11]
Mechanism of action
Substrate enters P-gp either from an opening within the inner leaflet of the membrane or from an opening at the cytoplasmic side of the protein. ATP binds at the cytoplasmic side of the protein. Following binding of each, ATP hydrolysis shifts the substrate into a position to be excreted from the cell. Release of the phosphate (from the original ATP molecule) occurs concurrently with substrate excretion. ADP is released, and a new molecule of ATP binds to the secondary ATP-binding site. Hydrolysis and release of ADP and a phosphate molecule resets the protein, so that the process can start again...
Tissue distribution
P-gp is expressed primarily in certain cell types in the liver, pancreas, kidney, colon, and jejunum.[12] P-gp is also found in brain capillary endothelial cells.[13]
Detecting the activity of the transporter
Radioactive verapamil can be used for measuring P-gp function with positron emission tomography.[14]
P-gp is also used to differentiate transitional B-cells from naive B-cells. Dyes such as Rhodamine123 and MitoTracker Dyes from Invitrogen can be used to make this differentiation.[15]
History
P-gp was first cloned and characterized in 1976. It was shown to be responsible for conferring multidrug resistance upon mutant cultured cancer cells that had developed resistance to cytotoxic drugs.[5][16]
The structure of P-gp was resolved by x-ray crystallography in 2009.[9]
References
- ^ a b c GRCm38: Ensembl release 89: ENSMUSG00000040584 – Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ Ueda K, Clark DP, Chen CJ, Roninson IB, Gottesman MM, Pastan I (Jan 1987). "The human multidrug resistance (mdr1) gene. cDNA cloning and transcription initiation". The Journal of Biological Chemistry. 262 (2): 505–8. PMID 3027054.
- ^ a b c Dean, Michael (2002-11-01). "The Human ATP-Binding Cassette (ABC) Transporter Superfamily". National Library of Medicine (US), NCBI. Archived from the original on 2006-02-12. Retrieved 2008-03-02.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ "Entrez Gene: ABCB1".
- ^ "Drug Development and Drug Interactions: Table of Substrates, Inhibitors and Inducers".
- ^ Franck Viguié (1998-03-01). "ABCB1". Atlas of Genetics and Cytogenetics in Oncology and Haematology. Retrieved 2008-03-02.
- ^ a b Aller SG, Yu J, Ward A, Weng Y, Chittaboina S, Zhuo R, Harrell PM, Trinh YT, Zhang Q, Urbatsch IL, Chang G (Mar 2009). "Structure of P-glycoprotein reveals a molecular basis for poly-specific drug binding". Science. 323 (5922). Science: 1718–22. doi:10.1126/science.1168750. PMC 2720052. PMID 19325113.
- ^ Ward A, Reyes CL, Yu J, Roth CB, Chang G (Nov 2007). "Flexibility in the ABC transporter MsbA: Alternating access with a twist". Proceedings of the National Academy of Sciences of the United States of America. 104 (48): 19005–10. doi:10.1073/pnas.0709388104. PMC 2141898. PMID 18024585.
- ^ Ferreira RJ, Ferreira MJ, Dos Santos DJ (Jun 2012). "Insights on P-Glycoprotein's Efflux Mechanism Obtained by Molecular Dynamics Simulations". Journal of Chemical Theory and Computation. 8 (6): 1853–64. doi:10.1021/ct300083m. PMID 26593820.
- ^ Thiebaut F, Tsuruo T, Hamada H, Gottesman MM, Pastan I, Willingham MC (Nov 1987). "Cellular localization of the multidrug-resistance gene product P-glycoprotein in normal human tissues". Proceedings of the National Academy of Sciences of the United States of America. 84 (21): 7735–8. doi:10.1073/pnas.84.21.7735. PMC 299375. PMID 2444983.
- ^ Schinkel AH (Apr 1999). "P-Glycoprotein, a gatekeeper in the blood-brain barrier". Advanced Drug Delivery Reviews. 36 (2–3): 179–194. doi:10.1016/S0169-409X(98)00085-4. PMID 10837715.
- ^ Luurtsema G, Windhorst AD, Mooijer MP, Herscheid A, Lammertsma AA, Franssen EJ (2002). "Fully automated high yield synthesis of (R)- and (S)-[C-11]verapamil for measuring P-glycoprotein function with positron emission tomography". Journal of Labelled Compounds & Radiopharmaceuticals. 45 (14): 1199–1207. doi:10.1002/jlcr.632.
- ^ Wirths S, Lanzavecchia A (Dec 2005). "ABCB1 transporter discriminates human resting naive B cells from cycling transitional and memory B cells". European Journal of Immunology. 35 (12): 3433–41. doi:10.1002/eji.200535364. PMID 16259010.
- ^ Juliano RL, Ling V (Nov 1976). "A surface glycoprotein modulating drug permeability in Chinese hamster ovary cell mutants". Biochimica et Biophysica Acta. 455 (1): 152–62. doi:10.1016/0005-2736(76)90160-7. PMID 990323.
Further reading
- Ling V (1997). "Multidrug resistance: molecular mechanisms and clinical relevance". Cancer Chemotherapy and Pharmacology. 40 Suppl (7): S3-8. doi:10.1007/s002800051053. PMID 9272126.
- Kerb R, Hoffmeyer S, Brinkmann U (Feb 2001). "ABC drug transporters: hereditary polymorphisms and pharmacological impact in MDR1, MRP1 and MRP2". Pharmacogenomics. 2 (1): 51–64. doi:10.1517/14622416.2.1.51. PMID 11258197.
- Akiyama S (Dec 2001). "[Mechanisms of drug resistance and reversal of the resistance]". Human Cell. 14 (4): 257–60. PMID 11925925.
- Brinkmann U (2002). "Functional polymorphisms of the human multidrug resistance (MDR1) gene: correlation with P glycoprotein expression and activity in vivo". Novartis Foundation Symposium. Novartis Foundation Symposia. 243: 207–10, discussion 210–2, 231–5. doi:10.1002/0470846356.ch15. ISBN 978-0-470-84635-3. PMID 11990778.
- Váradi A, Szakács G, Bakos E, Sarkadi B (2002). "P glycoprotein and the mechanism of multidrug resistance". Novartis Foundation Symposium. Novartis Foundation Symposia. 243: 54–65, discussion 65–8, 180–5. doi:10.1002/0470846356.ch5. ISBN 978-0-470-84635-3. PMID 11990782.
- Hegedus T, Orfi L, Seprodi A, Váradi A, Sarkadi B, Kéri G (Jul 2002). "Interaction of tyrosine kinase inhibitors with the human multidrug transporter proteins, MDR1 and MRP1". Biochimica et Biophysica Acta. 1587 (2–3): 318–25. doi:10.1016/s0925-4439(02)00095-9. PMID 12084474.
- Pallis M, Turzanski J, Higashi Y, Russell N (Jun 2002). "P-glycoprotein in acute myeloid leukaemia: therapeutic implications of its association with both a multidrug-resistant and an apoptosis-resistant phenotype". Leukemia & Lymphoma. 43 (6): 1221–8. doi:10.1080/10428190290026277. PMID 12152989.
- Schaich M, Illmer T (Jul 2002). "Mdr1 gene expression and mutations in Ras proto-oncogenes in acute myeloid leukemia". Leukemia & Lymphoma. 43 (7): 1345–54. doi:10.1080/10428190290033279. PMID 12389613.
- Fromm MF (Nov 2002). "The influence of MDR1 polymorphisms on P-glycoprotein expression and function in humans". Advanced Drug Delivery Reviews. 54 (10): 1295–310. doi:10.1016/S0169-409X(02)00064-9. PMID 12406646.
- Ambudkar SV, Kimchi-Sarfaty C, Sauna ZE, Gottesman MM (Oct 2003). "P-glycoprotein: from genomics to mechanism". Oncogene. 22 (47): 7468–85. doi:10.1038/sj.onc.1206948. PMID 14576852.
- Jamroziak K, Robak T (Apr 2004). "Pharmacogenomics of MDR1/ABCB1 gene: the influence on risk and clinical outcome of haematological malignancies". Hematology. 9 (2): 91–105. doi:10.1080/10245330310001638974. PMID 15203864.
- Ishikawa T, Onishi Y, Hirano H, Oosumi K, Nagakura M, Tarui S (Jul 2004). "Pharmacogenomics of drug transporters: a new approach to functional analysis of the genetic polymorphisms of ABCB1 (P-glycoprotein/MDR1)". Biological & Pharmaceutical Bulletin. 27 (7): 939–48. doi:10.1248/bpb.27.939. PMID 15256718.
- Lee W, Lockhart AC, Kim RB, Rothenberg ML (Feb 2005). "Cancer pharmacogenomics: powerful tools in cancer chemotherapy and drug development". The Oncologist. 10 (2): 104–11. doi:10.1634/theoncologist.10-2-104. PMID 15709212.
- Gambrelle J, Labialle S, Dayan G, Gayet L, Barakat S, Michaud M, Grange JD, Baggetto LG (Jun 2005). "[Multidrug resistance in uveal melanoma]". Journal Français d'Ophtalmologie. 28 (6): 652–9. doi:10.1016/s0181-5512(05)81112-x. PMID 16141933.
- Al-Shawi MK, Omote H (Dec 2005). "The remarkable transport mechanism of P-glycoprotein: a multidrug transporter". Journal of Bioenergetics and Biomembranes. 37 (6): 489–96. doi:10.1007/s10863-005-9497-5. PMC 1459968. PMID 16691488.
- Ferreira RJ, Ferreira MJ, Dos Santos DJ (Jun 2012). "Insights on P-Glycoprotein's Efflux Mechanism Obtained by Molecular Dynamics Simulations". Journal of Chemical Theory and Computation. 8 (6): 1853–64. doi:10.1021/ct300083m. PMID 26593820.
- Orlowski S, Martin S, Escargueil A (May 2006). "P-glycoprotein and 'lipid rafts': some ambiguous mutual relationships (floating on them, building them or meeting them by chance?)". Cellular and Molecular Life Sciences. 63 (9): 1038–59. doi:10.1007/s00018-005-5554-9. PMID 16721513.
- Annese V, Valvano MR, Palmieri O, Latiano A, Bossa F, Andriulli A (Jun 2006). "Multidrug resistance 1 gene in inflammatory bowel disease: a meta-analysis". World Journal of Gastroenterology. 12 (23): 3636–44. doi:10.3748/wjg.v12.i23.3636. PMID 16773678.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - Sekine I, Minna JD, Nishio K, Tamura T, Saijo N (Jan 2006). "A literature review of molecular markers predictive of clinical response to cytotoxic chemotherapy in patients with lung cancer". Journal of Thoracic Oncology. 1 (1): 31–7. doi:10.1097/01243894-200601000-00008. PMID 17409824.
- Kumar YS, Adukondalu D, Sathish D, Vishnu YV, Ramesh G, Latha AB, Reddy PC, Sarangapani M, Rao YM (2010). "P-Glycoprotein- and cytochrome P-450-mediated herbal drug interactions". Drug Metabolism and Drug Interactions. 25 (1–4): 3–16. doi:10.1515/DMDI.2010.006. PMID 21417789.
- Shityakov S, Förster C (2013). "Multidrug resistance protein P-gp interaction with nanoparticles (fullerenes and carbon nanotube) to assess their drug delivery potential: a theoretical molecular docking study". International Journal of Computational Biology and Drug Design. 6 (4): 343–57. doi:10.1504/IJCBDD.2013.056801. PMID 24088267.
- Shityakov S, Förster C (2014). "In silico structure-based screening of versatile P-glycoprotein inhibitors using polynomial empirical scoring functions". Advances and Applications in Bioinformatics and Chemistry. 7 (7): 1–9. doi:10.2147/AABC.S56046. PMC 3969253. PMID 24711707.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - Schinkel AH (Apr 1999). "P-Glycoprotein, a gatekeeper in the blood-brain barrier". Advanced Drug Delivery Reviews. 36 (2–3): 179–194. doi:10.1016/S0169-409X(98)00085-4. PMID 10837715.
External links
- P-Glycoprotein at the U.S. National Library of Medicine Medical Subject Headings (MeSH)
- Jessica R Oesterheld (2002-05-01). "P-glycoprotein". Mental Health Connections, Inc. Archived from the original on 2008-02-07. Retrieved 2008-03-02.
- P-glycoprotein substrate prediction
- NextBio.com
- PharmGKB.org
- The role of MDR1-MDCK in permeability studies The performance of MDR1-MDCK permeability studies for P-glycoprotein substrate identification.
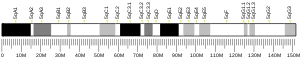
- ABCB1 human gene location in the UCSC Genome Browser.
- ABCB1 human gene details in the UCSC Genome Browser.
This article incorporates text from the United States National Library of Medicine, which is in the public domain.