GPER: Difference between revisions
Citation bot (talk | contribs) m Alter: volume, pages, issue. Removed parameters. Formatted dashes. | You can use this bot yourself. Report bugs here. | User-activated. |
Modified the "Clinical Significance" section to be called "Roles in Cancer", which more accurately reflects the content of this section. This section was also updated with modern references to reflect an up-to-date understanding of the role of GPER in cancer. |
||
| Line 25: | Line 25: | ||
Female GPER [[knockout mouse|knockout mice]] display [[hyperglycemia]] and impaired [[glucose tolerance]], reduced body growth, and increased [[blood pressure]].<ref name="pmid18845638">{{cite journal |vauthors=Mårtensson UE, Salehi SA, Windahl S, Gomez MF, Swärd K, Daszkiewicz-Nilsson J, Wendt A, Andersson N, Hellstrand P, Grände PO, Owman C, Rosen CJ, Adamo ML, Lundquist I, Rorsman P, Nilsson BO, Ohlsson C, Olde B, Leeb-Lundberg LM | display-authors = 6 | title = Deletion of the G protein-coupled Receptor GPR30 Impairs Glucose Tolerance, Reduces Bone Growth, Increases Blood Pressure, and Eliminates Estradiol-stimulated Insulin Release in Female Mice | journal = Endocrinology | volume = 150| issue = 2| pages = 687–98| year = 2008 | pmid = 18845638 | doi = 10.1210/en.2008-0623 }}</ref> Male GPER knockout mice are observed to have increased growth, body fat, insulin resistance and glucose intolerance, dyslipidemia, increased [[osteoblast]] function (mineralization), resulting in higher bone mineral density and [[cancellous bone|trabecular bone]] volume, and persistent growth plate activity resulting in longer bones.<ref name="pmid20734455">{{cite journal |vauthors=Ford J, Hajibeigi A, Long M, Hahner L, Gore C, Hsieh JT, Clegg D, Zerwekh J, Oz OK | title = GPR30 deficiency causes increased bone mass, mineralization, and growth plate proliferative activity in male mice | journal = J Bone Miner Res | volume = 26| issue = 2| pages = 298–307|date=August 2010 | pmid = 20734455 | doi = 10.1002/jbmr.209 | pmc = 3179349}}</ref><ref>{{cite journal | vauthors = Sharma G, Hu C, Brigman JL, Zhu G, Hathaway HJ, Prossnitz ER | title = GPER deficiency in male mice results in insulin resistance, dyslipidemia, and a proinflammatory state | journal = Endocrinology | volume = 154 | issue = 11 | pages = 4136–45 | date = November 2013 | pmid = 23970785 | pmc = 3800768 | doi = 10.1210/en.2013-1357 }}</ref> |
Female GPER [[knockout mouse|knockout mice]] display [[hyperglycemia]] and impaired [[glucose tolerance]], reduced body growth, and increased [[blood pressure]].<ref name="pmid18845638">{{cite journal |vauthors=Mårtensson UE, Salehi SA, Windahl S, Gomez MF, Swärd K, Daszkiewicz-Nilsson J, Wendt A, Andersson N, Hellstrand P, Grände PO, Owman C, Rosen CJ, Adamo ML, Lundquist I, Rorsman P, Nilsson BO, Ohlsson C, Olde B, Leeb-Lundberg LM | display-authors = 6 | title = Deletion of the G protein-coupled Receptor GPR30 Impairs Glucose Tolerance, Reduces Bone Growth, Increases Blood Pressure, and Eliminates Estradiol-stimulated Insulin Release in Female Mice | journal = Endocrinology | volume = 150| issue = 2| pages = 687–98| year = 2008 | pmid = 18845638 | doi = 10.1210/en.2008-0623 }}</ref> Male GPER knockout mice are observed to have increased growth, body fat, insulin resistance and glucose intolerance, dyslipidemia, increased [[osteoblast]] function (mineralization), resulting in higher bone mineral density and [[cancellous bone|trabecular bone]] volume, and persistent growth plate activity resulting in longer bones.<ref name="pmid20734455">{{cite journal |vauthors=Ford J, Hajibeigi A, Long M, Hahner L, Gore C, Hsieh JT, Clegg D, Zerwekh J, Oz OK | title = GPR30 deficiency causes increased bone mass, mineralization, and growth plate proliferative activity in male mice | journal = J Bone Miner Res | volume = 26| issue = 2| pages = 298–307|date=August 2010 | pmid = 20734455 | doi = 10.1002/jbmr.209 | pmc = 3179349}}</ref><ref>{{cite journal | vauthors = Sharma G, Hu C, Brigman JL, Zhu G, Hathaway HJ, Prossnitz ER | title = GPER deficiency in male mice results in insulin resistance, dyslipidemia, and a proinflammatory state | journal = Endocrinology | volume = 154 | issue = 11 | pages = 4136–45 | date = November 2013 | pmid = 23970785 | pmc = 3800768 | doi = 10.1210/en.2013-1357 }}</ref> |
||
== |
== Role in cancer == |
||
Although GPER signaling was originally thought to be tumor-promoting in breast cancer <ref name="LappanoPisano2014">{{cite journal|last1=Lappano|first1=Rosamaria|last2=Pisano|first2=Assunta|last3=Maggiolini|first3=Marcello|title=GPER Function in Breast Cancer: An Overview|journal=Frontiers in Endocrinology|volume=5|year=2014|issn=1664-2392|doi=10.3389/fendo.2014.00066}}</ref>, subsequent reports suggest that nonclassical estrogen signaling is tumor suppressive in breast cancer <ref name="WeiChen2014">{{cite journal|last1=Wei|first1=W|last2=Chen|first2=Z-J|last3=Zhang|first3=K-S|last4=Yang|first4=X-L|last5=Wu|first5=Y-M|last6=Chen|first6=X-H|last7=Huang|first7=H-B|last8=Liu|first8=H-L|last9=Cai|first9=S-H|last10=Du|first10=J|last11=Wang|first11=H-S|title=The activation of G protein-coupled receptor 30 (GPR30) inhibits proliferation of estrogen receptor-negative breast cancer cells in vitro and in vivo|journal=Cell Death & Disease|volume=5|issue=10|year=2014|pages=e1428–e1428|issn=2041-4889|doi=10.1038/cddis.2014.398}}</ref><ref name="WeißenbornIgnatov2014">{{cite journal|last1=Weißenborn|first1=Christine|last2=Ignatov|first2=Tanja|last3=Ochel|first3=Hans-Joachim|last4=Costa|first4=Serban Dan|last5=Zenclussen|first5=Ana Claudia|last6=Ignatova|first6=Zoya|last7=Ignatov|first7=Atanas|title=GPER functions as a tumor suppressor in triple-negative breast cancer cells|journal=Journal of Cancer Research and Clinical Oncology|volume=140|issue=5|year=2014|pages=713–723|issn=0171-5216|doi=10.1007/s00432-014-1620-8}}</ref><ref name="WeißenbornIgnatov2014">{{cite journal|last1=Weißenborn|first1=Christine|last2=Ignatov|first2=Tanja|last3=Poehlmann|first3=Angela|last4=Wege|first4=Anja K.|last5=Costa|first5=Serban D.|last6=Zenclussen|first6=Ana Claudia|last7=Ignatov|first7=Atanas|title=GPER functions as a tumor suppressor in MCF-7 and SK-BR-3 breast cancer cells|journal=Journal of Cancer Research and Clinical Oncology|volume=140|issue=4|year=2014|pages=663–671|issn=0171-5216|doi=10.1007/s00432-014-1598-2}}</ref>. Consistent with this, recent studies showed that the presence of GPER protein in human breast cancer biopsies correlates with longer survival, suggesting a tumor suppressive role <ref name="MartinLebot2018">{{cite journal|last1=Martin|first1=Stewart G.|last2=Lebot|first2=Marie N.|last3=Sukkarn|first3=Bhudsaban|last4=Ball|first4=Graham|last5=Green|first5=Andrew R.|last6=Rakha|first6=Emad A.|last7=Ellis|first7=Ian O.|last8=Storr|first8=Sarah J.|title=Low expression of G protein-coupled oestrogen receptor 1 (GPER) is associated with adverse survival of breast cancer patients|journal=Oncotarget|volume=9|issue=40|year=2018|issn=1949-2553|doi=10.18632/oncotarget.25408}}</ref>. In line with findings in breast cancer, GPER signaling has also been shown to be tumor suppressive in adrenocortical carcinoma <ref name="ChimentoSirianni2015">{{cite journal|last1=Chimento|first1=Adele|last2=Sirianni|first2=Rosa|last3=Casaburi|first3=Ivan|last4=Zolea|first4=Fabiana|last5=Rizza|first5=Pietro|last6=Avena|first6=Paola|last7=Malivindi|first7=Rocco|last8=De Luca|first8=Arianna|last9=Campana|first9=Carmela|last10=Martire|first10=Emilia|last11=Domanico|first11=Francesco|last12=Fallo|first12=Francesco|last13=Carpinelli|first13=Giulia|last14=Cerquetti|first14=Lidia|last15=Amendola|first15=Donatella|last16=Stigliano|first16=Antonio|last17=Pezzi|first17=Vincenzo|title=GPER agonist G-1 decreases adrenocortical carcinoma (ACC) cell growth <i>in vitro</i> and <i>in vivo</i>|journal=Oncotarget|volume=6|issue=22|year=2015|issn=1949-2553|doi=10.18632/oncotarget.4241}}</ref>, colorectal cancer <ref name="LiuChen2017">{{cite journal|last1=Liu|first1=Qiao|last2=Chen|first2=Zhuojia|last3=Jiang|first3=Guanmin|last4=Zhou|first4=Yan|last5=Yang|first5=Xiangling|last6=Huang|first6=Hongbin|last7=Liu|first7=Huanliang|last8=Du|first8=Jun|last9=Wang|first9=Hongsheng|title=Epigenetic down regulation of G protein-coupled estrogen receptor (GPER) functions as a tumor suppressor in colorectal cancer|journal=Molecular Cancer|volume=16|issue=1|year=2017|issn=1476-4598|doi=10.1186/s12943-017-0654-3}}</ref>, endometrial cancer <ref name="SkrzypczakSchüler2013">{{cite journal|last1=Skrzypczak|first1=Maciej|last2=Schüler|first2=Susanne|last3=Lattrich|first3=Claus|last4=Ignatov|first4=Atanas|last5=Ortmann|first5=Olaf|last6=Treeck|first6=Oliver|title=G protein-coupled estrogen receptor (GPER) expression in endometrial adenocarcinoma and effect of agonist G-1 on growth of endometrial adenocarcinoma cell lines|journal=Steroids|volume=78|issue=11|year=2013|pages=1087–1091|issn=0039128X|doi=10.1016/j.steroids.2013.07.007}}</ref>, Leydig cell tumors <ref name="ChimentoCasaburi2013">{{cite journal|last1=Chimento|first1=A|last2=Casaburi|first2=I|last3=Bartucci|first3=M|last4=Patrizii|first4=M|last5=Dattilo|first5=R|last6=Avena|first6=P|last7=Andò|first7=S|last8=Pezzi|first8=V|last9=Sirianni|first9=R|title=Selective GPER activation decreases proliferation and activates apoptosis in tumor Leydig cells|journal=Cell Death & Disease|volume=4|issue=8|year=2013|pages=e747–e747|issn=2041-4889|doi=10.1038/cddis.2013.275}}</ref>, non-small cell lung cancer <ref name="ZhuHuang2016">{{cite journal|last1=Zhu|first1=Guangfa|last2=Huang|first2=Yan|last3=Wu|first3=Chunting|last4=Wei|first4=Dong|last5=Shi|first5=Yingxin|title=Activation of G-Protein-Coupled Estrogen Receptor Inhibits the Migration of Human Nonsmall Cell Lung Cancer Cells via IKK-β/NF-κB Signals|journal=DNA and Cell Biology|volume=35|issue=8|year=2016|pages=434–442|issn=1044-5498|doi=10.1089/dna.2016.3235}}</ref>, gastric cancer <ref name="TianZhan2019">{{cite journal|last1=Tian|first1=Shan|last2=Zhan|first2=Na|last3=Li|first3=Ruixue|last4=Dong|first4=Weiguo|title=Downregulation of G Protein-Coupled Estrogen Receptor (GPER) is Associated with Reduced Prognosis in Patients with Gastric Cancer|journal=Medical Science Monitor|volume=25|year=2019|pages=3115–3126|issn=1643-3750|doi=10.12659/MSM.913634}}</ref>, liver cancer <ref name="WeiChen2016">{{cite journal|last1=Wei|first1=Tao|last2=Chen|first2=Wei|last3=Wen|first3=Liang|last4=Zhang|first4=Jian|last5=Zhang|first5=Qi|last6=Yang|first6=Jiaqi|last7=Liu|first7=Hao|last8=Chen|first8=Bryan Wei|last9=Zhou|first9=Yue|last10=Feng|first10=Xinhua|last11=Yang|first11=Qi|last12=Bai|first12=Xueli|last13=Liang|first13=Tingbo|title=G protein-coupled estrogen receptor deficiency accelerates liver tumorigenesis by enhancing inflammation and fibrosis|journal=Cancer Letters|volume=382|issue=2|year=2016|pages=195–202|issn=03043835|doi=10.1016/j.canlet.2016.08.012}}</ref>, melanoma <ref name="RibeiroSantos2017">{{cite journal|last1=Ribeiro|first1=Mariana P.C.|last2=Santos|first2=Armanda E.|last3=Custódio|first3=José B.A.|title=The activation of the G protein-coupled estrogen receptor (GPER) inhibits the proliferation of mouse melanoma K1735-M2 cells|journal=Chemico-Biological Interactions|volume=277|year=2017|pages=176–184|issn=00092797|doi=10.1016/j.cbi.2017.09.017}}</ref>, osteosarcoma <ref name="WangChen2018">{{cite journal|last1=Wang|first1=Zhen|last2=Chen|first2=Xiao|last3=Zhao|first3=Yongqiang|last4=Jin|first4=Yi|last5=Zheng|first5=Jia|title=G-protein-coupled estrogen receptor suppresses the migration of osteosarcoma cells via post-translational regulation of Snail|journal=Journal of Cancer Research and Clinical Oncology|volume=145|issue=1|year=2018|pages=87–96|issn=0171-5216|doi=10.1007/s00432-018-2768-4}}</ref>, ovarian cancer <ref name="IgnatovModl2013">{{cite journal|last1=Ignatov|first1=Tanja|last2=Modl|first2=Saskia|last3=Thulig|first3=Maike|last4=Weißenborn|first4=Christine|last5=Treeck|first5=Oliver|last6=Ortmann|first6=Olaf|last7=Zenclussen|first7=AC|last8=Costa|first8=Serban|last9=Kalinski|first9=Thomas|last10=Ignatov|first10=Atanas|title=GPER-1 acts as a tumor suppressor in ovarian cancer|journal=Journal of Ovarian Research|volume=6|issue=1|year=2013|pages=51|issn=1757-2215|doi=10.1186/1757-2215-6-51}}</ref>, and prostate cancer <ref name="LamOuyang2014">{{cite journal|last1=Lam|first1=Hung-Ming|last2=Ouyang|first2=Bin|last3=Chen|first3=Jing|last4=Ying|first4=Jun|last5=Wang|first5=Jiang|last6=Wu|first6=Chin-Lee|last7=Jia|first7=Li|last8=Medvedovic|first8=Mario|last9=Vessella|first9=Robert L|last10=Ho|first10=Shuk-Mei|title=Targeting GPR30 with G-1: a new therapeutic target for castration-resistant prostate cancer|journal=Endocrine-Related Cancer|volume=21|issue=6|year=2014|pages=903–914|issn=1351-0088|doi=10.1530/ERC-14-0402}}</ref>. Together, these reports suggest that GPER is a tumor suppressor in a wide range of cancer types, and activation of GPER may represent a new therapeutic strategy in cancer. |
|||
GPER plays a role in breast cancer progression and [[tamoxifen]] resistance.<ref name="Lappano_2014">{{cite journal | vauthors = Lappano R, Pisano A, Maggiolini M | title = GPER Function in Breast Cancer: An Overview | journal = Frontiers in Endocrinology | volume = 5 | issue = | pages = 66 | year = 2014 | pmid = 24834064 | pmc = 4018520 | doi = 10.3389/fendo.2014.00066 | department = review }}</ref> GPER has also been proposed as a [[biomarker]] in [[triple-negative breast cancer]].<ref name="Lappano_2014"/> In patients with endometrial cancer GPER it is overexpressed and its associated with poor survival.<ref name="Filardo_2018">{{cite journal | vauthors = Filardo EJ | title = A role for G-protein coupled estrogen receptor (GPER) in estrogen-induced carcinogenesis: Dysregulated glandular homeostasis, survival and metastasis | journal = The Journal of Steroid Biochemistry and Molecular Biology | volume = 176 | issue = | pages = 38–48 | date = February 2018 | pmid = 28595943 | doi = 10.1016/j.jsbmb.2017.05.005 | department = review }}</ref> In other tumors, there is still a controversy over the role of GPER. For example in ovarian cancer, some studies indicate a link between GPER expression and poor prognosis, while other studies do not.<ref name="Filardo_2018" /> |
|||
==See also== |
==See also== |
||
Revision as of 19:51, 4 July 2019
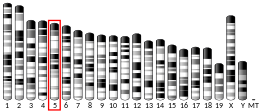
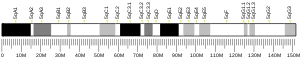
G protein-coupled estrogen receptor 1 (GPER), also known as G protein-coupled receptor 30 (GPR30), is a protein that in humans is encoded by the GPER gene.[5] GPER binds to and is activated by the female sex hormone estradiol and is responsible for some of the rapid effects that estradiol has on cells.
Discovery
The classical estrogen receptors first characterized in 1958[6] are water-soluble proteins located in the interior of cells that are activated by estrogenenic hormones such as estradiol and several of its metabolites such as estrone or estriol. These proteins belong to the nuclear hormone receptor class of transcription factors that regulate gene transcription. Since it takes time for genes to be transcribed into RNA and translated into protein, the effects of estrogens binding to these classical estrogen receptors is delayed. However, estrogens are also known to have effects that are too fast to be caused by regulation of gene transcription.[7] In 2005, it was discovered that a member of the G protein-coupled receptor (GPCR) family, GPR30 also binds with high affinity to estradiol and is responsible in part for the rapid non-genomic actions of estradiol. Based on its ability to bind estradiol, GPR30 was renamed as G protein-coupled estrogen receptor (GPER). Unlike the other members of the GPCR family, which reside in the outer membrane of cells, GPER is localized in the endoplasmic reticulum.[7]
Ligands
GPER binds estradiol though not other endogenous estrogens, such as estrone or estriol, nor for other endogenous steroids, including progesterone, testosterone, and cortisol.[8][9][10][11] Although potentially involved in signaling by aldosterone, GPER does not show any detectable binding towards aldosterone.[12][13] Niacin and nicotinamide bind to the receptor in vitro with very low affinity.[14][15] CCL18 has been identified as an endogenous antagonist of the GPER.[16]
Function
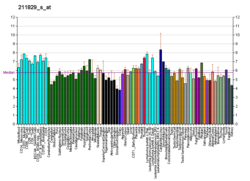
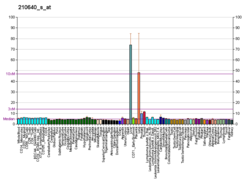
This protein is a member of the rhodopsin-like family of G protein-coupled receptors and is a multi-pass membrane protein that localizes to the endoplasmic reticulum. The protein binds estradiol, resulting in intracellular calcium mobilization and synthesis of phosphatidylinositol (3,4,5)-trisphosphate in the nucleus.[8] This protein therefore plays a role in the rapid nongenomic signaling events widely observed following stimulation of cells and tissues with estradiol.[17] The distribution of GPER is well established in the rodent, with high expression observed in the hypothalamus, pituitary gland, adrenal medulla, kidney medulla and developing follicles of the ovary.[18]
Animal studies
Reproductive tissue
GPER is expressed in the breasts, and activation by estradiol produces cell proliferation in both normal and malignant breast epithelial tissue.[19][20] However, GPER knockout mice show no overt mammary phenotype, unlike ERα knockout mice, but similarly to ERβ knockout mice.[19] This indicates that although GPER and ERβ play a modulatory role in breast development, ERα is the main receptor responsible for estrogen-mediated breast tissue growth.[19] GPER is expressed in germ cells and has been found to be essential for male fertility, specifically, in spermatogenesis.[21][22][23][24] GPER has been found to modulate gonadotropin-releasing hormone (GnRH) secretion in the hypothalamic-pituitary-gonadal (HPG) axis.[24]
Cardiovascular effects
GPER is expressed in the blood vessel endothelium and is responsible for vasodilation and as a result, blood pressure lowering effects of 17β-estradiol.[25] GPER also regulates components of the renin–angiotensin system, which also controls blood pressure,[26][27] and is required for superoxide-mediated cardiovascular function and aging.[28]
Central nervous system activity
GPER and ERα, but not ERβ, have been found to mediate the antidepressant-like effects of estradiol.[29][30][31] Contrarily, activation of GPER has been found to be anxiogenic in mice, while activation of ERβ has been found to be anxiolytic.[32] There is a high expression of GPER, as well as ERβ, in oxytocin neurons in various parts of the hypothalamus, including the paraventricular nucleus and the supraoptic nucleus.[31][33] It is speculated that activation of GPER may be the mechanism by which estradiol mediates rapid effects on the oxytocin system,[31][33] for instance, rapidly increasing oxytocin receptor expression.[34] Estradiol has also been found to increase oxytocin levels and release in the medial preoptic area and medial basal hypothalamus, actions that may be mediated by activation of GPER and/or ERβ.[34] Estradiol, as well as tamoxifen and fulvestrant, have been found to rapidly induce lordosis through activation of GPER in the arcuate nucleus of the hypothalamus of female rats.[35][36]
Metabolic roles
Female GPER knockout mice display hyperglycemia and impaired glucose tolerance, reduced body growth, and increased blood pressure.[37] Male GPER knockout mice are observed to have increased growth, body fat, insulin resistance and glucose intolerance, dyslipidemia, increased osteoblast function (mineralization), resulting in higher bone mineral density and trabecular bone volume, and persistent growth plate activity resulting in longer bones.[38][39]
Role in cancer
Although GPER signaling was originally thought to be tumor-promoting in breast cancer [40], subsequent reports suggest that nonclassical estrogen signaling is tumor suppressive in breast cancer [41][42][42]. Consistent with this, recent studies showed that the presence of GPER protein in human breast cancer biopsies correlates with longer survival, suggesting a tumor suppressive role [43]. In line with findings in breast cancer, GPER signaling has also been shown to be tumor suppressive in adrenocortical carcinoma [44], colorectal cancer [45], endometrial cancer [46], Leydig cell tumors [47], non-small cell lung cancer [48], gastric cancer [49], liver cancer [50], melanoma [51], osteosarcoma [52], ovarian cancer [53], and prostate cancer [54]. Together, these reports suggest that GPER is a tumor suppressor in a wide range of cancer types, and activation of GPER may represent a new therapeutic strategy in cancer.
See also
References
- ^ a b c GRCh38: Ensembl release 89: ENSG00000164850 – Ensembl, May 2017
- ^ a b c GRCm38: Ensembl release 89: ENSMUSG00000053647 – Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ O'Dowd BF, Nguyen T, Marchese A, Cheng R, Lynch KR, Heng HH, Kolakowski LF, George SR (January 1998). "Discovery of three novel G-protein-coupled receptor genes". Genomics. 47 (2): 310–3. doi:10.1006/geno.1998.5095. PMID 9479505.
- ^ Jensen E (2012). "A conversation with Elwood Jensen. Interview by David D. Moore". Annual Review of Physiology. 74: 1–11. doi:10.1146/annurev-physiol-020911-153327. PMID 21888507.
- ^ a b Vrtačnik P, Ostanek B, Mencej-Bedrač S, Marc J (2014). "The many faces of estrogen signaling". Biochemia Medica. 24 (3): 329–42. doi:10.11613/BM.2014.035. PMC 4210253. PMID 25351351.
- ^ a b Revankar CM, Cimino DF, Sklar LA, Arterburn JB, Prossnitz ER (March 2005). "A transmembrane intracellular estrogen receptor mediates rapid cell signaling". Science. 307 (5715): 1625–30. doi:10.1126/science.1106943. PMID 15705806.
- ^ Filardo EJ, Thomas P (October 2005). "GPR30: a seven-transmembrane-spanning estrogen receptor that triggers EGF release". Trends in Endocrinology and Metabolism. 16 (8): 362–7. doi:10.1016/j.tem.2005.08.005. PMID 16125968.
- ^ Manavathi B, Kumar R (June 2006). "Steering estrogen signals from the plasma membrane to the nucleus: two sides of the coin". Journal of Cellular Physiology. 207 (3): 594–604. doi:10.1002/jcp.20551. PMID 16270355.
- ^ Prossnitz ER, Arterburn JB, Sklar LA (February 2007). "GPR30: A G protein-coupled receptor for estrogen". Molecular and Cellular Endocrinology. 265–266: 138–42. doi:10.1016/j.mce.2006.12.010. PMC 1847610. PMID 17222505.
- ^ Wendler A, Albrecht C, Wehling M (August 2012). "Nongenomic actions of aldosterone and progesterone revisited". Steroids. 77 (10): 1002–6. doi:10.1016/j.steroids.2011.12.023. PMID 22285849.
- ^ Cheng SB, Dong J, Pang Y, LaRocca J, Hixon M, Thomas P, Filardo EJ (February 2014). "Anatomical location and redistribution of G protein-coupled estrogen receptor-1 during the estrus cycle in mouse kidney and specific binding to estrogens but not aldosterone". Molecular and Cellular Endocrinology. 382 (2): 950–9. doi:10.1016/j.mce.2013.11.005. PMID 24239983.
- ^ Santolla MF, De Francesco EM, Lappano R, Rosano C, Abonante S, Maggiolini M (July 2014). "Niacin activates the G protein estrogen receptor (GPER)-mediated signalling". Cell. Signal. 26 (7): 1466–1475. doi:10.1016/j.cellsig.2014.03.011. PMID 24662263.
Nicotinic acid, also known as niacin, is the water soluble vitamin B3 used for decades for the treatment of dyslipidemic diseases. Its action is mainly mediated by the G protein-coupled receptor (GPR) 109A; however, certain regulatory effects on lipid levels occur in a GPR109A-independent manner. The amide form of nicotinic acid, named nicotinamide, acts as a vitamin although neither activates the GPR109A nor exhibits the pharmacological properties of nicotinic acid. In the present study, we demonstrate for the first time that nicotinic acid and nicotinamide bind to and activate the GPER-mediated signalling in breast cancer cells and cancer-associated fibroblasts (CAFs)
- ^ Barton M (February 2016). "Not lost in translation: Emerging clinical importance of the G protein-coupled estrogen receptor GPER". Steroids. 111: 37–45. doi:10.1016/j.steroids.2016.02.016. PMID 26921679.
- ^ Catusse J, Wollner S, Leick M, Schröttner P, Schraufstätter I, Burger M (November 2010). "Attenuation of CXCR4 responses by CCL18 in acute lymphocytic leukemia B cells". J. Cell. Physiol. 225 (3): 792–800. doi:10.1002/jcp.22284. PMID 20568229.
- ^ "Entrez Gene: GPR30 G protein-coupled receptor 30".
- ^ Hazell GG, Yao ST, Roper JA, Prossnitz ER, O'Carroll AM, Lolait SJ (August 2009). "Localisation of GPR30, a novel G protein-coupled oestrogen receptor, suggests multiple functions in rodent brain and peripheral tissues". The Journal of Endocrinology. 202 (2): 223–36. doi:10.1677/JOE-09-0066. PMC 2710976. PMID 19420011.
- ^ a b c Scaling AL, Prossnitz ER, Hathaway HJ (2014). "GPER mediates estrogen-induced signaling and proliferation in human breast epithelial cells and normal and malignant breast". Horm Cancer. 5 (3): 146–60. doi:10.1007/s12672-014-0174-1. PMC 4091989. PMID 24718936.
- ^ Cite error: The named reference
Lappano_2014was invoked but never defined (see the help page). - ^ Carreau S, Bouraima-Lelong H, Delalande C (2011). "Estrogens: new players in spermatogenesis". Reprod Biol. 11 (3): 174–93. doi:10.1016/s1642-431x(12)60065-5. PMID 22139333.
- ^ Carreau S, Bois C, Zanatta L, Silva FR, Bouraima-Lelong H, Delalande C (2011). "Estrogen signaling in testicular cells". Life Sci. 89 (15–16): 584–7. doi:10.1016/j.lfs.2011.06.004. PMID 21703280.
- ^ Carreau S, Bouraima-Lelong H, Delalande C (2012). "Estrogen, a female hormone involved in spermatogenesis". Adv Med Sci. 57 (1): 31–6. doi:10.2478/v10039-012-0005-y. PMID 22440937.
- ^ a b Chimento A, Sirianni R, Casaburi I, Pezzi V (2014). "Role of estrogen receptors and g protein-coupled estrogen receptor in regulation of hypothalamus-pituitary-testis axis and spermatogenesis". Front Endocrinol (Lausanne). 5: 1. doi:10.3389/fendo.2014.00001. PMC 3893621. PMID 24474947.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Meyer MR, Amann K, Field AS, Hu C, Hathaway HJ, Kanagy NL, Walker MK, Barton M, Prossnitz ER (February 2012). "Deletion of G protein-coupled estrogen receptor increases endothelial vasoconstriction". Hypertension. 59 (2): 507–12. doi:10.1161/HYPERTENSIONAHA.111.184606. PMC 3266468. PMID 22203741.
The development of the GPER-selective agonist G-114 has facilitated studies that demonstrate GPER activation induces acute vasodilation and lowers blood pressure in rodents. We18 and others17,19 have shown that acute GPER-mediated vasodilator effects are at least partly endothelium- and NO-dependent.
- ^ Lindsey SH, Chappell MC (December 2011). "Evidence that the G protein-coupled membrane receptor GPR30 contributes to the cardiovascular actions of estrogen". Gender Medicine. 8 (6): 343–54. doi:10.1016/j.genm.2011.10.004. PMC 3240864. PMID 22153880.
- ^ Han G, Li F, Yu X, White RE (May 2013). "GPER: a novel target for non-genomic estrogen action in the cardiovascular system". Pharmacological Research. 71: 53–60. doi:10.1016/j.phrs.2013.02.008. PMID 23466742.
- ^ Meyer MR, Fredette NC, Daniel C, Sharma G, Amann K, Arterburn JB, Barton M, Prossnitz ER (November 2016). "Obligatory role for GPER in cardiovascular aging and disease". Science Signaling. 9 (452): ra105. doi:10.1126/scisignal.aag0240. PMC 5124501. PMID 27803283.
- ^ Estrada-Camarena E, López-Rubalcava C, Vega-Rivera N, Récamier-Carballo S, Fernández-Guasti A (2010). "Antidepressant effects of estrogens: a basic approximation". Behav Pharmacol. 21 (5–6): 451–64. doi:10.1097/FBP.0b013e32833db7e9. PMID 20700047.
- ^ Dennis MK, Burai R, Ramesh C, Petrie WK, Alcon SN, Nayak TK, Bologa CG, Leitao A, Brailoiu E, Deliu E, Dun NJ, Sklar LA, Hathaway HJ, Arterburn JB, Oprea TI, Prossnitz ER (2009). "In vivo effects of a GPR30 antagonist". Nat. Chem. Biol. 5 (6): 421–7. doi:10.1038/nchembio.168. PMC 2864230. PMID 19430488.
- ^ a b c Xu H, Qin S, Carrasco GA, Dai Y, Filardo EJ, Prossnitz ER, Battaglia G, Doncarlos LL, Muma NA (2009). "Extra-nuclear estrogen receptor GPR30 regulates serotonin function in rat hypothalamus". Neuroscience. 158 (4): 1599–607. doi:10.1016/j.neuroscience.2008.11.028. PMC 2747636. PMID 19095043.
- ^ Kastenberger I, Lutsch C, Schwarzer C (2012). "Activation of the G-protein-coupled receptor GPR30 induces anxiogenic effects in mice, similar to oestradiol". Psychopharmacology. 221 (3): 527–35. doi:10.1007/s00213-011-2599-3. PMC 3350630. PMID 22143579.
- ^ a b Choleris, Elena (11 April 2013). Oxytocin, Vasopressin and Related Peptides in the Regulation of Behavior. Cambridge University Press. pp. 10–. ISBN 978-0-521-19035-0.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ a b Blaustein, Jeffrey D. (8 December 2006). Handbook of Neurochemistry and Molecular Neurobiology: Behavioral Neurochemistry, Neuroendocrinology and Molecular Neurobiology. Springer Science & Business Media. pp. 165–. ISBN 978-0-387-30362-8.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Long N, Serey C, Sinchak K (September 2014). "17β-estradiol rapidly facilitates lordosis through G protein-coupled estrogen receptor 1 (GPER) via deactivation of medial preoptic nucleus μ-opioid receptors in estradiol primed female rats". Hormones and Behavior. 66 (4): 663–6. doi:10.1016/j.yhbeh.2014.09.008. PMC 4254307. PMID 25245158.
- ^ Long, Nathan; Long, Bertha; Mana, Asma; Le, Dream; Nguyen, Lam; Chokr, Sima; Sinchak, Kevin (1 March 2017). "Tamoxifen and ICI 182,780 activate hypothalamic G protein-coupled estrogen receptor 1 to rapidly facilitate lordosis in female rats". Hormones and Behavior. 89: 98–103. doi:10.1016/j.yhbeh.2016.12.013. PMC 5359066. PMID 28063803.
- ^ Mårtensson UE, Salehi SA, Windahl S, Gomez MF, Swärd K, Daszkiewicz-Nilsson J, et al. (2008). "Deletion of the G protein-coupled Receptor GPR30 Impairs Glucose Tolerance, Reduces Bone Growth, Increases Blood Pressure, and Eliminates Estradiol-stimulated Insulin Release in Female Mice". Endocrinology. 150 (2): 687–98. doi:10.1210/en.2008-0623. PMID 18845638.
- ^ Ford J, Hajibeigi A, Long M, Hahner L, Gore C, Hsieh JT, Clegg D, Zerwekh J, Oz OK (August 2010). "GPR30 deficiency causes increased bone mass, mineralization, and growth plate proliferative activity in male mice". J Bone Miner Res. 26 (2): 298–307. doi:10.1002/jbmr.209. PMC 3179349. PMID 20734455.
- ^ Sharma G, Hu C, Brigman JL, Zhu G, Hathaway HJ, Prossnitz ER (November 2013). "GPER deficiency in male mice results in insulin resistance, dyslipidemia, and a proinflammatory state". Endocrinology. 154 (11): 4136–45. doi:10.1210/en.2013-1357. PMC 3800768. PMID 23970785.
- ^ Lappano, Rosamaria; Pisano, Assunta; Maggiolini, Marcello (2014). "GPER Function in Breast Cancer: An Overview". Frontiers in Endocrinology. 5. doi:10.3389/fendo.2014.00066. ISSN 1664-2392.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Wei, W; Chen, Z-J; Zhang, K-S; Yang, X-L; Wu, Y-M; Chen, X-H; Huang, H-B; Liu, H-L; Cai, S-H; Du, J; Wang, H-S (2014). "The activation of G protein-coupled receptor 30 (GPR30) inhibits proliferation of estrogen receptor-negative breast cancer cells in vitro and in vivo". Cell Death & Disease. 5 (10): e1428–e1428. doi:10.1038/cddis.2014.398. ISSN 2041-4889.
- ^ a b Weißenborn, Christine; Ignatov, Tanja; Ochel, Hans-Joachim; Costa, Serban Dan; Zenclussen, Ana Claudia; Ignatova, Zoya; Ignatov, Atanas (2014). "GPER functions as a tumor suppressor in triple-negative breast cancer cells". Journal of Cancer Research and Clinical Oncology. 140 (5): 713–723. doi:10.1007/s00432-014-1620-8. ISSN 0171-5216. Cite error: The named reference "WeißenbornIgnatov2014" was defined multiple times with different content (see the help page).
- ^ Martin, Stewart G.; Lebot, Marie N.; Sukkarn, Bhudsaban; Ball, Graham; Green, Andrew R.; Rakha, Emad A.; Ellis, Ian O.; Storr, Sarah J. (2018). "Low expression of G protein-coupled oestrogen receptor 1 (GPER) is associated with adverse survival of breast cancer patients". Oncotarget. 9 (40). doi:10.18632/oncotarget.25408. ISSN 1949-2553.
- ^ Chimento, Adele; Sirianni, Rosa; Casaburi, Ivan; Zolea, Fabiana; Rizza, Pietro; Avena, Paola; Malivindi, Rocco; De Luca, Arianna; Campana, Carmela; Martire, Emilia; Domanico, Francesco; Fallo, Francesco; Carpinelli, Giulia; Cerquetti, Lidia; Amendola, Donatella; Stigliano, Antonio; Pezzi, Vincenzo (2015). "GPER agonist G-1 decreases adrenocortical carcinoma (ACC) cell growth in vitro and in vivo". Oncotarget. 6 (22). doi:10.18632/oncotarget.4241. ISSN 1949-2553.
- ^ Liu, Qiao; Chen, Zhuojia; Jiang, Guanmin; Zhou, Yan; Yang, Xiangling; Huang, Hongbin; Liu, Huanliang; Du, Jun; Wang, Hongsheng (2017). "Epigenetic down regulation of G protein-coupled estrogen receptor (GPER) functions as a tumor suppressor in colorectal cancer". Molecular Cancer. 16 (1). doi:10.1186/s12943-017-0654-3. ISSN 1476-4598.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Skrzypczak, Maciej; Schüler, Susanne; Lattrich, Claus; Ignatov, Atanas; Ortmann, Olaf; Treeck, Oliver (2013). "G protein-coupled estrogen receptor (GPER) expression in endometrial adenocarcinoma and effect of agonist G-1 on growth of endometrial adenocarcinoma cell lines". Steroids. 78 (11): 1087–1091. doi:10.1016/j.steroids.2013.07.007. ISSN 0039-128X.
- ^ Chimento, A; Casaburi, I; Bartucci, M; Patrizii, M; Dattilo, R; Avena, P; Andò, S; Pezzi, V; Sirianni, R (2013). "Selective GPER activation decreases proliferation and activates apoptosis in tumor Leydig cells". Cell Death & Disease. 4 (8): e747–e747. doi:10.1038/cddis.2013.275. ISSN 2041-4889.
- ^ Zhu, Guangfa; Huang, Yan; Wu, Chunting; Wei, Dong; Shi, Yingxin (2016). "Activation of G-Protein-Coupled Estrogen Receptor Inhibits the Migration of Human Nonsmall Cell Lung Cancer Cells via IKK-β/NF-κB Signals". DNA and Cell Biology. 35 (8): 434–442. doi:10.1089/dna.2016.3235. ISSN 1044-5498.
- ^ Tian, Shan; Zhan, Na; Li, Ruixue; Dong, Weiguo (2019). "Downregulation of G Protein-Coupled Estrogen Receptor (GPER) is Associated with Reduced Prognosis in Patients with Gastric Cancer". Medical Science Monitor. 25: 3115–3126. doi:10.12659/MSM.913634. ISSN 1643-3750.
- ^ Wei, Tao; Chen, Wei; Wen, Liang; Zhang, Jian; Zhang, Qi; Yang, Jiaqi; Liu, Hao; Chen, Bryan Wei; Zhou, Yue; Feng, Xinhua; Yang, Qi; Bai, Xueli; Liang, Tingbo (2016). "G protein-coupled estrogen receptor deficiency accelerates liver tumorigenesis by enhancing inflammation and fibrosis". Cancer Letters. 382 (2): 195–202. doi:10.1016/j.canlet.2016.08.012. ISSN 0304-3835.
- ^ Ribeiro, Mariana P.C.; Santos, Armanda E.; Custódio, José B.A. (2017). "The activation of the G protein-coupled estrogen receptor (GPER) inhibits the proliferation of mouse melanoma K1735-M2 cells". Chemico-Biological Interactions. 277: 176–184. doi:10.1016/j.cbi.2017.09.017. ISSN 0009-2797.
- ^ Wang, Zhen; Chen, Xiao; Zhao, Yongqiang; Jin, Yi; Zheng, Jia (2018). "G-protein-coupled estrogen receptor suppresses the migration of osteosarcoma cells via post-translational regulation of Snail". Journal of Cancer Research and Clinical Oncology. 145 (1): 87–96. doi:10.1007/s00432-018-2768-4. ISSN 0171-5216.
- ^ Ignatov, Tanja; Modl, Saskia; Thulig, Maike; Weißenborn, Christine; Treeck, Oliver; Ortmann, Olaf; Zenclussen, AC; Costa, Serban; Kalinski, Thomas; Ignatov, Atanas (2013). "GPER-1 acts as a tumor suppressor in ovarian cancer". Journal of Ovarian Research. 6 (1): 51. doi:10.1186/1757-2215-6-51. ISSN 1757-2215.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Lam, Hung-Ming; Ouyang, Bin; Chen, Jing; Ying, Jun; Wang, Jiang; Wu, Chin-Lee; Jia, Li; Medvedovic, Mario; Vessella, Robert L; Ho, Shuk-Mei (2014). "Targeting GPR30 with G-1: a new therapeutic target for castration-resistant prostate cancer". Endocrine-Related Cancer. 21 (6): 903–914. doi:10.1530/ERC-14-0402. ISSN 1351-0088.
External links
- "Estrogen (G protein coupled) Receptor". IUPHAR Database of Receptors and Ion Channels. International Union of Basic and Clinical Pharmacology.
- GPER+protein at the U.S. National Library of Medicine Medical Subject Headings (MeSH)
This article incorporates text from the United States National Library of Medicine, which is in the public domain.