Halothane
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Fluothane |
| AHFS/Drugs.com | FDA Professional Drug Information |
| License data | |
| Routes of administration | Inhalation |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Metabolism | Hepatic (CYP2E1[4]) |
| Excretion | Kidney, respiratory |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.005.270 |
| Chemical and physical data | |
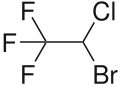
| Formula | C2HBrClF3 |
| Molar mass | 197.38 g·mol−1 |
| 3D model (JSmol) | |
| Density | 1.871 g/cm3 (at 20 °C) |
| Melting point | −118 °C (−180 °F) |
| Boiling point | 50.2 °C (122.4 °F) |
| |
| |
| (verify) | |
Halothane, sold under the brand name Fluothane among others, is a general anaesthetic.[5] It can be used to induce or maintain anaesthesia.[5] One of its benefits is that it does not increase the production of saliva, which can be particularly useful in those who are difficult to intubate.[5] It is given by inhalation.[5]
Side effects include an irregular heartbeat, respiratory depression, and hepatotoxicity.[5] Like all volatile anesthetics, it should not be used in people with a personal or family history of malignant hyperthermia.[5] It appears to be safe in porphyria.[6] It is unclear whether its usage during pregnancy is harmful to the fetus, and its use during a C-section is generally discouraged.[7] Halothane is a chiral molecule that is used as a racemic mixture.[8]
Halothane was discovered in 1951.[9] It was approved for medical use in the United States in 1958.[3] It is on the World Health Organization's List of Essential Medicines.[10] Its use in developed countries has been mostly replaced by newer anesthetic agents such as sevoflurane.[11] It is no longer commercially available in the United States.[7] Halothane also contributes to ozone depletion.[12][13]
Medical uses
[edit]
It is a potent anesthetic with a minimum alveolar concentration (MAC) of 0.74%.[14] Its blood/gas partition coefficient of 2.4 makes it an agent with moderate induction and recovery time.[15] It is not a good analgesic and its muscle relaxation effect is moderate.[16]
Halothane is colour-coded red on anaesthetic vaporisers.[17]

Side effects
[edit]Side effects include irregular heartbeat, respiratory depression, and hepatotoxicity.[5] It appears to be safe in porphyria.[6] It is unclear whether use during pregnancy is harmful to the baby, and it is not generally recommended for use during a C-section.[7] In rare cases, repeated exposure to halothane in adults was noted to result in severe liver injury. This occurred in about one in 10,000 exposures. The resulting syndrome was referred to as halothane hepatitis, immunoallergic in origin,[18] and is thought to result from the metabolism of halothane to trifluoroacetic acid via oxidative reactions in the liver. About 20% of inhaled halothane is metabolized by the liver and these products are excreted in the urine. The hepatitis syndrome had a mortality rate of 30% to 70%.[19] Concern for hepatitis resulted in a dramatic reduction in the use of halothane for adults and it was replaced in the 1980s by enflurane and isoflurane.[20][21] By 2005, the most common volatile anesthetics used were isoflurane, sevoflurane, and desflurane. Since the risk of halothane hepatitis in children was substantially lower than in adults, halothane continued to be used in pediatrics in the 1990s as it was especially useful for inhalation induction of anesthesia.[22][23] However, by 2000, sevoflurane, excellent for inhalation induction, had largely replaced the use of halothane in children.[24]
Halothane sensitises the heart to catecholamines, so it is liable to cause cardiac arrhythmia, occasionally fatal, particularly if hypercapnia has been allowed to develop. This seems to be especially problematic in dental anesthesia.[25]
Like all the potent inhalational anaesthetic agents, it is a potent trigger for malignant hyperthermia.[5] Similarly, in common with the other potent inhalational agents, it relaxes uterine smooth muscle and this may increase blood loss during delivery or termination of pregnancy.[26]
Occupational safety
[edit]People can be exposed to halothane in the workplace by breathing it in as waste anaesthetic gas, skin contact, eye contact, or swallowing it.[27] The National Institute for Occupational Safety and Health (NIOSH) has set a recommended exposure limit (REL) of 2 ppm (16.2 mg/m3) over 60 minutes.[28]
Pharmacology
[edit]The exact mechanism of the action of general anaesthetics has not been delineated.[29] Halothane activates GABAA and glycine receptors.[30][31] It also acts as an NMDA receptor antagonist,[31] inhibits nACh and voltage-gated sodium channels,[30][32] and activates 5-HT3 and twin-pore K+ channels.[30][33] It does not affect the AMPA or kainate receptors.[31]
Chemical and physical properties
[edit]Halothane (2-bromo-2-chloro-1,1,1-trifluoroethane) is a dense, highly volatile, clear, colourless, nonflammable liquid with a chloroform-like sweet odour. It is very slightly soluble in water and miscible with various organic solvents. Halothane can decompose to hydrogen fluoride, hydrogen chloride and hydrogen bromide in the presence of light and heat.[34]
| Boiling point: | 50.2 °C | (at 101.325 kPa) |
| Density: | 1.871 g/cm3 | (at 20 °C) |
| Molecular Weight: | 197.4 u | |
| Vapor pressure: | 244 mmHg (32kPa) | (at 20 °C) |
| 288 mmHg (38kPa) | (at 24 °C) | |
| MAC: | 0.75 | vol % |
| Blood:gas partition coefficient: | 2.3 | |
| Oil:gas partition coefficient: | 224 |
Chemically, halothane is an alkyl halide (not an ether like many other anesthetics).[4] The structure has one stereocenter, so (R)- and (S)-optical isomers occur.[citation needed]
Synthesis
[edit]The commercial synthesis of halothane starts from trichloroethylene, which is reacted with hydrogen fluoride in the presence of antimony trichloride at 130 °C to form 2-chloro-1,1,1-trifluoroethane. This is then reacted with bromine at 450 °C to produce halothane.[35]
Related substances
[edit]Attempts to find anesthetics with less metabolism led to halogenated ethers such as enflurane and isoflurane. The incidence of hepatic reactions with these agents is lower. The exact degree of hepatotoxic potential of enflurane is debated, although it is minimally metabolized. Isoflurane is essentially not metabolized and reports of associated liver injury are quite rare.[36] Small amounts of trifluoroacetic acid can be formed from both halothane and isoflurane metabolism and possibly accounts for cross sensitization of patients between these agents.[37][38]
The main advantage of the more modern agents is lower blood solubility, resulting in faster induction of and recovery from anaesthesia.[39]
History
[edit]
Halothane was first synthesized by C. W. Suckling of Imperial Chemical Industries in 1951 at the ICI Widnes Laboratory and was first used clinically by M. Johnstone in Manchester in 1956. Initially, many pharmacologists and anaesthesiologists had doubts about the safety and efficacy of the new drug. But halothane, which required specialist knowledge and technologies for safe administration, also afforded British anaesthesiologists the opportunity to remake their speciality as a profession during a period, when the newly established National Health Service needed more specialist consultants.[40] In this context, halothane eventually became popular as a nonflammable general anesthetic replacing other volatile anesthetics such as trichloroethylene, diethyl ether and cyclopropane. In many parts of the world it has been largely replaced by newer agents since the 1980s but is still widely used in developing countries because of its lower cost.[41]

Halothane was given to many millions of people worldwide from its introduction in 1956 through the 1980s.[42] Its properties include cardiac depression at high levels, cardiac sensitization to catecholamines such as norepinephrine, and potent bronchial relaxation. Its lack of airway irritation made it a common inhalation induction agent in pediatric anesthesia.[43][44] Its use in developed countries has been mostly replaced by newer anesthetic agents such as sevoflurane.[45] It is not commercially available in the United States.[7]
Society and culture
[edit]Availability
[edit]It is on the World Health Organization's List of Essential Medicines.[10] It is available as a volatile liquid, at 30, 50, 200, and 250 ml per container but in many developed nations is not available having been displaced by newer agents.[46]
It is the only inhalational anesthetic containing bromine, which makes it radiopaque.[47] It is colorless and pleasant-smelling, but unstable in light. It is packaged in dark-colored bottles and contains 0.01% thymol as a stabilizing agent.[20]
Greenhouse gas
[edit]Owing to the presence of covalently bonded fluorine, halothane absorbs in the atmospheric window and is therefore a greenhouse gas. However, it is much less potent than most other chlorofluorocarbons and bromofluorocarbons due to its short atmospheric lifetime, estimated at only one year vis-à-vis over 100 years for many perfluorocarbons.[48] Despite its short lifespan, halothane still has a global warming potential 47 times that of carbon dioxide, although this is over 100 times smaller than the most abundant fluorinated gases, and about 800 times smaller than the GWP of sulfur hexafluoride over 500 years.[49] Halothane is believed to make a negligible contribution to global warming.[48]
Ozone depletion
[edit]Halothane is an ozone depleting substance with an ODP of 1.56 and it is calculated to be responsible for 1% of total stratospheric ozone layer depletion.[12][13]
References
[edit]- ^ Anvisa (31 March 2023). "RDC Nº 784 — Listas de Substâncias Entorpecentes, Psicotrópicas, Precursoras e Outras sob Controle Especial" [Collegiate Board Resolution No. 784 — Lists of Narcotic, Psychotropic, Precursor, and Other Substances under Special Control] (in Brazilian Portuguese). Diário Oficial da União (published 4 April 2023). Archived from the original on 3 August 2023. Retrieved 16 August 2023.
- ^ "Halothane, USP". DailyMed. 18 September 2013. Retrieved 11 February 2022.
- ^ a b "Fluothane: FDA-Approved Drugs". U.S. Food and Drug Administration. Retrieved 12 February 2022.
- ^ a b "Halothane". DrugBank. DB01159.
- ^ a b c d e f g h World Health Organization (2009). Stuart MC, Kouimtzi M, Hill SR (eds.). WHO Model Formulary 2008. World Health Organization. pp. 17–8. hdl:10665/44053. ISBN 978-92-4-154765-9.
- ^ a b James MF, Hift RJ (July 2000). "Porphyrias". British Journal of Anaesthesia. 85 (1): 143–53. doi:10.1093/bja/85.1.143. PMID 10928003.
- ^ a b c d "Halothane — FDA prescribing information, side effects and uses". www.drugs.com. June 2005. Archived from the original on 21 December 2016. Retrieved 13 December 2016.
- ^ Bricker S (17 June 2004). The Anaesthesia Science Viva Book. Cambridge University Press. p. 161. ISBN 978-0-521-68248-0. Archived from the original on 10 September 2017 – via Google Books.
- ^ Walker SR (2012). Trends and Changes in Drug Research and Development. Springer. p. 109. ISBN 978-94-009-2659-2. Archived from the original on 10 September 2017.
- ^ a b World Health Organization (2023). The selection and use of essential medicines 2023: web annex A: World Health Organization model list of essential medicines: 23rd list (2023). Geneva: World Health Organization. hdl:10665/371090. WHO/MHP/HPS/EML/2023.02.
- ^ Yentis SM, Hirsch NP, Ip J (2013). Anaesthesia and Intensive Care A-Z: An Encyclopedia of Principles and Practice (5th ed.). Elsevier Health Sciences. p. 264. ISBN 978-0-7020-5375-7. Archived from the original on 10 September 2017.
- ^ a b Kümmerer K (2013). Pharmaceuticals in the Environment: Sources, Fate, Effects and Risks. Springer. p. 33. ISBN 978-3-662-09259-0.
- ^ a b Langbein T, Sonntag H, Trapp D, Hoffmann A, Malms W, Röth EP, et al. (January 1999). "Volatile anaesthetics and the atmosphere: atmospheric lifetimes and atmospheric effects of halothane, enflurane, isoflurane, desflurane and sevoflurane". British Journal of Anaesthesia. 82 (1): 66–73. doi:10.1093/bja/82.1.66. PMID 10325839.
- ^ Lobo SA, Ojeda J, Dua A, Singh K, Lopez J (2022). Minimum Alveolar Concentration. StatPearls. Treasure Island (FL): StatPearls Publishing. PMID 30422569. NBK532974.
- ^ Bezuidenhout E (November 2020). "The blood–gas partition coefficient". Southern African Journal of Anaesthesia and Analgesia. 1 (3): 3. doi:10.36303/SAJAA.2020.26.6.S3.2528. eISSN 2220-1173. ISSN 2220-1181.
- ^ "Halothane". Anesthesia General. 31 October 2010. Archived from the original on 16 February 2011.
- ^ Subrahmanyam M, Mohan S (September 2013). "Safety features in anaesthesia machine". Indian J Anaesth. 57 (5): 472–480. doi:10.4103/0019-5049.120143. PMC 3821264. PMID 24249880.
- ^ Habibollahi P, Mahboobi N, Esmaeili S, Safari S, Dabbagh A, Alavian SM (January 2018). Halothane. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. PMID 31643481. NBK548151.
- ^ Wark H, Earl J, Chau DD, Overton J (April 1990). "Halothane metabolism in children". British Journal of Anaesthesia. 64 (4): 474–481. doi:10.1093/bja/64.4.474. PMID 2334622.
- ^ a b Gyorfi MJ, Kim PY (2022). Halothane Toxicity. StatPearls. Treasure Island (FL): StatPearls Publishing. PMID 31424865. NBK545281.
- ^ Hankins DC, Kharasch ED (9 May 1997). "Determination of the halothane metabolites trifluoroacetic acid and bromide in plasma and urine by ion chromatography". Journal of Chromatography B: Biomedical Sciences and Applications. 692 (2): 413–8. doi:10.1016/S0378-4347(96)00527-0. ISSN 0378-4347. PMID 9188831.
- ^ Okuno T, Koutsogiannaki S, Hou L, Bu W, Ohto U, Eckenhoff RG, et al. (December 2019). "Volatile anesthetics isoflurane and sevoflurane directly target and attenuate Toll-like receptor 4 system". FASEB Journal. 33 (12): 14528–41. doi:10.1096/fj.201901570R. PMC 6894077. PMID 31675483.
- ^ Sakai EM, Connolly LA, Klauck JA (December 2005). "Inhalation anesthesiology and volatile liquid anesthetics: focus on isoflurane, desflurane, and sevoflurane". Pharmacotherapy. 25 (12): 1773–88. doi:10.1592/phco.2005.25.12.1773. PMID 16305297. S2CID 40873242.
- ^ Patel SS, Goa KL (April 1996). "Sevoflurane. A review of its pharmacodynamic and pharmacokinetic properties and its clinical use in general anaesthesia". Drugs. 51 (4): 658–700. doi:10.2165/00003495-199651040-00009. PMID 8706599. S2CID 265731583.
- ^ Paris ST, Cafferkey M, Tarling M, Hancock P, Yate PM, Flynn PJ (September 1997). "Comparison of sevoflurane and halothane for outpatient dental anaesthesia in children". British Journal of Anaesthesia. 79 (3): 280–4. doi:10.1093/bja/79.3.280. PMID 9389840.
- ^ Satuito M, Tom J (2016). "Potent Inhalational Anesthetics for Dentistry". Anesthesia Progress. 63 (1): 42–8, quiz 49. doi:10.2344/0003-3006-63.1.42. PMC 4751520. PMID 26866411.
- ^ "Common Name: Halothene" (PDF). Hazardous Substance Fact Sheet (PDF). 969 (1). 1999 – via New Jersey Department of Health and Senior Services.
- ^ "Halothane". NIOSH Pocket Guide to Chemical Hazards. (NIOSH) National Institute for Occupational Safety and Health, Centers for Disease Control. Archived from the original on 8 December 2015. Retrieved 3 November 2015.
- ^ Perkins B (7 February 2005). "How does anesthesia work?". Scientific American. Retrieved 30 June 2016.
- ^ a b c Hemmings HC, Hopkins PM (2006). Foundations of Anesthesia: Basic Sciences for Clinical Practice. Elsevier Health Sciences. pp. 292–. ISBN 978-0-323-03707-5. Archived from the original on 30 April 2016.
- ^ a b c Barash P, Cullen BF, Stoelting RK, Cahalan M, Stock CM, Ortega R (7 February 2013). Clinical Anesthesia, 7e: Print + Ebook with Multimedia. Lippincott Williams & Wilkins. pp. 116–. ISBN 978-1-4698-3027-8. Archived from the original on 17 June 2016.
- ^ Schüttler J, Schwilden H (8 January 2008). Modern Anesthetics. Springer. pp. 70–. ISBN 978-3-540-74806-9. Archived from the original on 1 May 2016.
- ^ Bowery NG (19 June 2006). Allosteric Receptor Modulation in Drug Targeting. CRC Press. pp. 143–. ISBN 978-1-4200-1618-5. Archived from the original on 10 May 2016.
- ^ Lewis, R.J. Sax's Dangerous Properties of Industrial Materials. 9th ed. Volumes 1-3. New York, NY: Van Nostrand Reinhold, 1996., p. 1761
- ^ Suckling et al.,"PROCESS FOR THE PREPARATION OF 1,1,1-TRIFLUORO-2-BROMO-2-CHLOROETHANE", US patent 2921098, granted January 1960 , assigned to Imperial Chemical Industries
- ^ Halogenated Anesthetics. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. January 2018. PMID 31644158. NBK548851.
- ^ Ma TG, Ling YH, McClure GD, Tseng MT (October 1990). "Effects of trifluoroacetic acid, a halothane metabolite, on C6 glioma cells". Journal of Toxicology and Environmental Health. 31 (2): 147–158. Bibcode:1990JTEH...31..147M. doi:10.1080/15287399009531444. PMID 2213926.
- ^ Biermann JS, Rice SA, Fish KJ, Serra MT (September 1989). "Metabolism of halothane in obese Fischer 344 rats". Anesthesiology. 71 (3): 431–7. doi:10.1097/00000542-198909000-00020. PMID 2774271.
- ^ Eger EI (1984). "The pharmacology of isoflurane". British Journal of Anaesthesia. 56 (Suppl 1): 71S–99S. PMID 6391530.
- ^ Mueller LM (March 2021). "Medicating Anaesthesiology: Pharmaceutical Change, Specialisation and Healthcare Reform in Post-War Britain". Social History of Medicine. 34 (4): 1343–65. doi:10.1093/shm/hkaa101.
- ^ Bovill JG (2008). "Inhalation Anaesthesia: From Diethyl Ether to Xenon". Modern Anesthetics. Handbook of Experimental Pharmacology. Vol. 182. pp. 121–142. doi:10.1007/978-3-540-74806-9_6. ISBN 978-3-540-72813-9. PMID 18175089.
- ^ Niedermeyer E, da Silva FH (2005). Electroencephalography: Basic Principles, Clinical Applications, and Related Fields. Lippincott Williams & Wilkins. p. 1156. ISBN 978-0-7817-5126-1. Archived from the original on 9 May 2016.
- ^ Himmel HM (2008). "Mechanisms involved in cardiac sensitization by volatile anesthetics: general applicability to halogenated hydrocarbons?". Critical Reviews in Toxicology. 38 (9): 773–803. doi:10.1080/10408440802237664. PMID 18941968. S2CID 12906139.
- ^ Chavez CA, Ski CF, Thompson DR (July 2014). "Psychometric properties of the Cardiac Depression Scale: a systematic review". Heart, Lung & Circulation. 23 (7): 610–8. doi:10.1016/j.hlc.2014.02.020. PMID 24709392.
- ^ Yentis SM, Hirsch NP, Ip J (2013). Anaesthesia and Intensive Care A-Z: An Encyclopedia of Principles and Practice (5th ed.). Elsevier Health Sciences. p. 264. ISBN 978-0-7020-5375-7. Archived from the original on 10 September 2017.
- ^ National formulary of India (4th ed.). New Delhi, India: Indian Pharmacopoeia Commission. 2011. p. 411.
- ^ Miller AL, Theodore D, Widrich J (2022). Inhalational Anesthetic. StatPearls. Treasure Island (FL): StatPearls Publishing. PMID 32119427. NBK554540.
- ^ a b Hodnebrog Ø, Etminan M, Fuglestvedt JS, Marston G, Myhre G, Nielsen CJ, et al. (24 April 2013). "Global warming potentials and radiative efficiencies of halocarbons and related compounds: A comprehensive review" (PDF). Reviews of Geophysics. 51 (2): 300–378. Bibcode:2013RvGeo..51..300H. doi:10.1002/rog.20013.
- ^ Hodnebrog Ø, Aamaas B, Fuglestvedt JS, Marston G, Myhre G, Nielsen CJ, et al. (September 2020). "Updated Global Warming Potentials and Radiative Efficiencies of Halocarbons and Other Weak Atmospheric Absorbers". Reviews of Geophysics. 58 (3): e2019RG000691. Bibcode:2020RvGeo..5800691H. doi:10.1029/2019RG000691. PMC 7518032. PMID 33015672.
- 5-HT3 agonists
- GABAA receptor positive allosteric modulators
- General anesthetics
- Glycine receptor agonists
- Hepatitis
- Hepatotoxins
- Nicotinic antagonists
- NMDA receptor antagonists
- Organobromides
- Organochlorides
- Organofluorides
- Trifluoromethyl compounds
- Withdrawn drugs
- World Health Organization essential medicines
- Ozone depletion
- Racemic mixtures

