Imipramine
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Tofranil, Tofranil-PM, others |
| Other names | Melipramine; G-22355 |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682389 |
| License data |
|
| Pregnancy category |
|
| Routes of administration | By mouth, intramuscular injection |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 94–96%[3] |
| Protein binding | 86%[4] |
| Metabolism | Liver (CYP1A2, CYP2C19, CYP2D6)[4] |
| Metabolites | Desipramine[4] |
| Elimination half-life | 20 hours[4] |
| Excretion | Kidney (80%), fecal (20%)[4] |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| PDB ligand | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.000.039 |
| Chemical and physical data | |
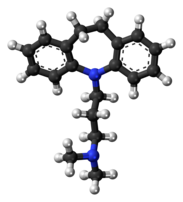
| Formula | C19H24N2 |
| Molar mass | 280.415 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| (verify) | |
Imipramine, sold under the brand name Tofranil, among others, is a tricyclic antidepressant (TCA) mainly used in the treatment of depression. It is also effective in treating anxiety and panic disorder. Imipramine is taken by mouth.
Common side effects of imipramine include dry mouth, drowsiness, dizziness, low blood pressure, rapid heart rate, urinary retention, and electrocardiogram changes. Overdose of the medication can result in death. Imipramine appears to work by increasing levels of serotonin and norepinephrine and by blocking certain serotonin, adrenergic, histamine, and cholinergic receptors.
Imipramine was discovered in 1951 and was introduced for medical use in 1957. It was the first TCA to be marketed. Imipramine and the other TCAs (besides amitriptyline, which, at least in the U.K., remains at least just as commonly-prescribed as SSRIs) have decreased in use in recent decades, due to the introduction of the selective serotonin reuptake inhibitors (SSRIs), which, although generally significantly less potent in terms of clinical efficacy per-se, have fewer inherent side effects and are far safer in overdose. Irrespective of these caveats, however, imipramine has an invaluable place in psychiatry and other fields of medicine (e.g., with childhood enuresis), and is considered the "gold standard" for panic disorder.[5][6]
Medical uses
[edit]Imipramine is primarily used for the treatment of depression and certain anxiety disorders, including acute post-traumatic stress reactions. A significant amount of research regarding its efficacy on acute post-traumatic stress in children and adolescents has focused on trauma resulting from burn-injuries.[7][8][9] Although evidence for its efficacy in the treatment of chronic post-traumatic stress disorder appears to be less robust,[10] it remains a viable treatment.[11] Here, it may act fairly similarly to monoamine oxidase inhibitor phenelzine.
Caution is needed in prescribing imipramine (and its commercially-available metabolite, desipramine) in children and youth/adolescents (whether they suffer with, e.g., bed-wetting, recurrent panic attacks, acute trauma or, in the case of desipramine,[12][13] ADHD), owing to possibility of certain side-effects which may be of particular concern in those under a certain age.[14][15]
In the treatment of depression, it has demonstrated similar efficacy to the MAOI moclobemide.[16] It has also been used to treat nocturnal enuresis because of its ability to shorten the time of delta wave stage sleep, where wetting occurs. In veterinary medicine, imipramine is used with xylazine to induce pharmacologic ejaculation in stallions. It is also used for separation anxiety in dogs and cats. Blood levels between 150 and 250 ng/mL of imipramine plus its metabolite desipramine generally correspond to antidepressant efficacy.[17]
Contraindications
[edit]Combining it with alcohol consumption may cause more drowsiness, necessitating greater caution when drinking.[18] It may be unsafe during pregnancy.[1]
Many MAOIs are known to have serious interactions with imipramine. It is often contraindicated during their use or in the two weeks following their discontinuation. This category includes medications such as isocarboxazid, linezolid, methylene blue, phenelzine, selegiline, moclobemide, procarbazine, rasagiline, safinamide, and tranylcypromine.[18][19]
Side effects
[edit]These side effects can be contributed to the multiple receptors that imipramine targets such as serotonin, norepinephrine, dopamine, acetylcholine, epinephrine, histamine. Those listed in italics below denote common side effects, separated by the organ systems that are affected.[20] Some side effects may be beneficial in some cases, e.g. reduction of hyperactive gag reflex; reduced random or physical strain-linked urinary leakage.
- Central nervous system: dizziness, drowsiness, confusion, seizures, headache, anxiety, tremors, stimulation, weakness, insomnia, nightmares, extrapyramidal symptoms in geriatric patients, increased psychiatric symptoms, paresthesia
- Cardiovascular: orthostatic hypotension, ECG changes, tachycardia, hypertension, palpitations, dysrhythmias
- Eyes, ears, nose and throat: blurred vision, tinnitus, mydriasis
- Gastrointestinal: dry mouth, nausea, vomiting, paralytic ileus, increased appetite, cramps, epigastric distress, jaundice, hepatitis, stomatitis, constipation, taste change
- Genitourinary: urinary retention
- Hematological: agranulocytosis, thrombocytopenia, eosinophilia, leukopenia
- Skin: rash, urticaria, diaphoresis, pruritus, photosensitivity
Overdose
[edit]Interactions
[edit]Like other tricyclic antidepressants, imipramine has many medication interactions. Many MAOIs have serious interactions with this medication. Other categories of medications that may interact with imipramine include blood thinners, antihistamines, muscle relaxants, sleeping pills, thyroid medications, and tranquilizers. Some medications used for various conditions such as high blood pressure, mental illness, nausea, Parkinson's disease, asthma, colds, or allergies.[18]
Certain medications increase the risk of serotonin syndrome, including selective serotonin reuptake inhibitors (SSRIs), St. John's Wort, and drugs such as ecstasy. Other prescription drugs decrease the body's ability to eliminate imipramine. These include barbiturates, some antiarrhythmic medications, some antiepileptic drugs, and certain HIV drugs (protease inhibitors). Others may cause changes in the heart rhythm, such as QT prolongation.[19]
Alcohol and tobacco may interact with imipramine. Tobacco may decrease the medication's effectiveness.[18]
Pharmacology
[edit]Pharmacodynamics
[edit]| Site | IMI | DSI | Species | Ref |
|---|---|---|---|---|
| SERT | 1.3–1.4 | 17.6–163 | Human | [23][24] |
| NET | 20–37 | 0.63–3.5 | Human | [23][24] |
| DAT | 8,500 | 3,190 | Human | [23] |
| 5-HT1A | ≥5,800 | ≥6,400 | Human | [25][26][27] |
| 5-HT2A | 80–150 | 115–350 | Human | [25][27] |
| 5-HT2C | 120 | 244–748 | Human/rat | [28][29][26] |
| 5-HT3 | 970–3,651 | ≥2,500 | Rodent | [26][30] |
| 5-HT6 | 190–209 | ND | Rat | [31] |
| 5-HT7 | >1,000 | >1,000 | Rat | [32] |
| α1 | 32 | 23–130 | Human | [25][33][24] |
| α2 | 3,100 | ≥1,379 | Human | [25][33][24] |
| β | >10,000 | ≥1,700 | Rat | [34][35][36] |
| D1 | >10,000 | 5,460 | Human | [26][37] |
| D2 | 620–726 | 3,400 | Human | [37][26][33] |
| D3 | 387 | ND | Human | [26] |
| H1 | 7.6–37 | 60–110 | Human | [25][33][38] |
| H2 | 550 | 1,550 | Human | [38] |
| H3 | >100,000 | >100,000 | Human | [38] |
| H4 | 24,000 | 9,550 | Human | [38] |
| mACh | 46 | 66–198 | Human | [25][33] |
| M1 | 42 | 110 | Human | [39] |
| M2 | 88 | 540 | Human | [39] |
| M3 | 60 | 210 | Human | [39] |
| M4 | 112 | 160 | Human | [39] |
| M5 | 83 | 143 | Human | [39] |
| α3β4 | 410–970 | ND | Human | [40] |
| σ1 | 332–520 | 1,990–4,000 | Rodent | [41][42][43] |
| σ2 | 327–2,100 | ≥1,611 | Rat | [21][42][43] |
| hERG | 3,400 | ND | Human | [44] |
| Values are Ki (nM). The smaller the value, the more strongly the drug binds to the site. | ||||
Imipramine affects numerous neurotransmitter systems known to be involved in the etiology of depression, anxiety, attention-deficit hyperactivity disorder (ADHD), enuresis and numerous other mental and physical conditions. Imipramine is similar in structure to some muscle relaxants, and has a significant analgesic effect and, thus, is very useful in some pain conditions.
The mechanisms of imipramine's actions include, but are not limited to, effects on:
- Serotonin: very strong reuptake inhibition. Imipramine is a tertiary TCA, and is a potent inhibitor of serotonin reuptake, and to a greater extent than secondary amine TCAs such as nortriptyline and despiramine.[45]
- Norepinephrine: strong reuptake inhibition. Desipramine has more affinity to norepinephrine transporter than imipramine.
- Dopamine: imipramine blocks D2 receptors.[46] Imipramine, and its metabolite desipramine, have no appreciable affinity for the dopamine transporter (Ki = 8,500 and >10,000 nM, respectively).[47]
- Acetylcholine: imipramine is, to a certain extent, an antimuscarinic, specifically a relative antagonist of the muscarinic acetylcholine receptors. The attendant side-effects (e.g., blurry vision, dry mouth, constipation), however, are somewhat less common with imipramine than amitriptyline and protriptyline, which tend to cause antimuscarinic side-effects more often. All-in-all, however, it is prescribed with caution to the elderly and with extreme caution to those with psychosis, as the general brain activity enhancement in combination with the "dementing" effects of anticholinergics increases the potential of imipramine to cause hallucinations, confusion and delirium in this population. "Anti-cholinergic" side-effects, including urinary hesitancy/retention, may be treated/reversed with bethanechol and/or other acetylcholine-agonists.[48][49][50]
Bethanechol may also be able to alleviate the sexual-dysfunction symptoms which may occur in the context of tricyclic-antidepressant treatment.[51][52][53]
- Epinephrine: imipramine antagonizes adrenergic receptors, thus sometimes causing orthostatic hypotension.
- Sigma receptor: activity on sigma receptors is present, but it is very weak (Ki = 520 nM) and it is about half that of amitriptyline (Ki = 300 nM).[citation needed]
- Histamine: imipramine is an antagonist of the histamine H1 receptors.
- BDNF: BDNF is implicated in neurogenesis in the hippocampus, and studies suggest that depressed patients have decreased levels of BDNF and reduced hippocampal neurogenesis. It is not clear how neurogenesis restores mood, as ablation of hippocampal neurogenesis in murine models do not show anxiety related or depression related behaviours. Chronic imipramine administration results in increased histone acetylation (which is associated with transcriptional activation and decondensed chromatin) at the hippocampal BDNF promoter, and also reduced expression of hippocampal HDAC5.[54][55]
Pharmacokinetics
[edit]This section needs expansion. You can help by adding to it. (June 2024) |
Imipramine has a varied absolute oral bioavailability ranging from 22% to 77%, leading to significant variability in pharmacokinetics. While the drug has rapid and complete absorption after oral administration, much of the drug is affected by first pass metabolism. Food has no effect on absorption, peak drug concentration, or time to peak drug concentration.[56]
Within the body, imipramine is converted into desipramine (desmethylimipramine) as a metabolite.[56]
Chemistry
[edit]Imipramine is a tricyclic compound, specifically a dibenzazepine, and possesses three rings fused together with a side chain attached in its chemical structure.[57] Other dibenzazepine TCAs include desipramine (N-desmethylimipramine), clomipramine (3-chloroimipramine), trimipramine (2′-methylimipramine or β-methylimipramine), and lofepramine (N-(4-chlorobenzoylmethyl)desipramine).[57][58] Imipramine is a tertiary amine TCA, with its side chain-demethylated metabolite desipramine being a secondary amine.[59][60] Other tertiary amine TCAs include amitriptyline, clomipramine, dosulepin (dothiepin), doxepin, and trimipramine.[61][62] The chemical name of imipramine is 3-(10,11-dihydro-5H-dibenzo[b,f]azepin-5-yl)-N,N-dimethylpropan-1-amine and its free base form has a chemical formula of C19H24N2 with a molecular weight of 280.407 g/mol.[63] The drug is used commercially mostly as the hydrochloride salt; the embonate (pamoate) salt is used for intramuscular administration and the free base form is not used.[63][64] The CAS Registry Number of the free base is 50-49-7, of the hydrochloride is 113-52-0, and of the embonate is 10075-24-8.[63][64]
History
[edit]The parent compound of imipramine, 10,11-dihydro-5H-dibenz[b,f]azepine (dibenzazepine), was first synthesized in 1899, but no pharmacological assessment of this compound or any substituted derivatives was undertaken until the late 1940s.[65][66][67] Imipramine was first synthesized in 1951, as an antihistamine.[68][69] The antipsychotic effects of chlorpromazine were discovered in 1952,[70] and imipramine was then developed and studied as an antipsychotic for use in patients with schizophrenia.[33][71] The medication was tested in several hundred patients with psychosis, but showed little effectiveness.[72] However, imipramine was serendipitously found to possess antidepressant effects in the mid-1950s following a case report of symptom improvement in a woman with severe depression who had been treated with it.[33][71][73] This was followed by similar observations in other patients and further clinical research.[74][72] Subsequently, imipramine was introduced for the treatment of depression in Europe in 1958 and in the United States in 1959.[75] Along with the discovery and introduction of the monoamine oxidase inhibitor iproniazid as an antidepressant around the same time, imipramine resulted in the establishment of monoaminergic drugs as antidepressants.[73][74][72]
In the late 1950s, imipramine was the first TCA to be developed (by Ciba). At the first international congress of neuropharmacology in Rome, September 1958 Dr Freyhan from the University of Pennsylvania discussed as one of the first clinicians the effects of imipramine in a group of 46 patients, most of them diagnosed as "depressive psychosis". The patients were selected for this study based on symptoms such as depressive apathy, kinetic retardation and feelings of hopelessness and despair. In 30% of all patients, he reported optimal results, and in around 20%, failure. The side effects noted were atropine-like, and most patients experienced dizziness. Imipramine was first tried for treating psychotic disorders such as schizophrenia, but proved ineffective. As an antidepressant, it did well in clinical studies and it is known to work well in even the most severe cases of depression.[76] It is not surprising, therefore, that imipramine may cause a high rate of manic and hypomanic reactions in hospitalized patients with pre-existing bipolar disorder, with one study showing that up to 25% of such patients maintained on Imipramine switched into mania or hypomania.[77] Such powerful antidepressant properties have made it favorable in the treatment of treatment-resistant depression.
Before the advent of selective serotonin reuptake inhibitors (SSRIs), its sometimes intolerable side-effect profile was considered more tolerable. Therefore, it became extensively used as a standard antidepressant and later served as a prototypical drug for the development of the later-released TCAs. Since SSRIs are superior in terms of inherent side-effect tolerability (although probably inferior in terms of actual efficacy), it has, as of the 1990s, no longer been used as commonly, but is sometimes still prescribed as a second-line treatment for treating major depression. It has also seen limited use in the treatment of migraines, ADHD, and post-concussive syndrome. Imipramine has additional indications for the treatment of panic attacks, chronic pain, and Kleine-Levin syndrome. In pediatric patients, it is relatively frequently used to treat pavor nocturnus and nocturnal enuresis.
Society and culture
[edit]Generic names
[edit]Imipramine is the English and French generic name of the drug and its INN, BAN, and DCF, while imipramine hydrochloride is its USAN, USP, BANM, and JAN.[63][64][78][79] Its generic name in Spanish and Italian and its DCIT are imipramina, in German is imipramin, and in Latin is imipraminum.[64][79] The embonate salt is known as imipramine pamoate.[64][79]
Brand names
[edit]Imipramine is marketed throughout the world mainly under the brand name Tofranil.[64][79] Imipramine pamoate is marketed under the brand name Tofranil-PM for intramuscular injection.[64][79][80]
Availability
[edit]Imipramine is available for medical use widely throughout the world, including in the United States, the United Kingdom, elsewhere in Europe, India, Brazil, South Africa, Australia, and New Zealand.[79]
Prescription trends
[edit]Between 1998 and 2017, along with amitriptyline, imipramine was the most commonly prescribed first antidepressant for children aged 5-11 years in England.[81]
See also
[edit]References
[edit]- ^ a b "Imipramine Use During Pregnancy". Drugs.com. 28 August 2019. Retrieved 7 February 2020.
- ^ Anvisa (2023-03-31). "RDC Nº 784 - Listas de Substâncias Entorpecentes, Psicotrópicas, Precursoras e Outras sob Controle Especial" [Collegiate Board Resolution No. 784 - Lists of Narcotic, Psychotropic, Precursor, and Other Substances under Special Control] (in Brazilian Portuguese). Diário Oficial da União (published 2023-04-04). Archived from the original on 2023-08-03. Retrieved 2023-08-16.
- ^ Heck HA, Buttrill SE, Flynn NW, Dyer RL, Anbar M, Cairns T, et al. (June 1979). "Bioavailability of imipramine tablets relative to a stable isotope-labeled internal standard: increasing the power of bioavailability tests". Journal of Pharmacokinetics and Biopharmaceutics. 7 (3): 233–248. doi:10.1007/BF01060015. PMID 480146. S2CID 23232584.
- ^ a b c d e "Product Information Tolerade (imipramine hydrochloride)". TGA eBusiness Services. PMIP Pty Ltd. 4 June 2013. Archived from the original on 10 December 2019. Retrieved 16 October 2013.
- ^ Michelson LK, Marchione K (February 1991). "Behavioral, cognitive, and pharmacological treatments of panic disorder with agoraphobia: critique and synthesis". Journal of Consulting and Clinical Psychology. 59 (1): 100–14. doi:10.1037/0022-006x.59.1.100. PMID 2002125.
- ^ Schwartz TL, Nihalani N, Simionescu M, Hopkins G (2005). "History repeats itself: pharmacodynamic trends in the treatment of anxiety disorders". Current Pharmaceutical Design. 11 (2): 255–63. doi:10.2174/1381612053382214. PMID 15638761.
- ^ Robert R, Blakeney PE, Villarreal C, Rosenberg L, Meyer WJ (July 1999). "Imipramine treatment in pediatric burn patients with symptoms of acute stress disorder: a pilot study". Journal of the American Academy of Child and Adolescent Psychiatry. 38 (7): 873–882. doi:10.1097/00004583-199907000-00018. PMID 10405506.
- ^ Tcheung WJ, Robert R, Rosenberg L, Rosenberg M, Villarreal C, Thomas C, et al. (November 2005). "Early treatment of acute stress disorder in children with major burn injury". Pediatric Critical Care Medicine. 6 (6): 676–681. doi:10.1097/01.pcc.0000165562.04157.da. PMID 16276335. S2CID 43261789.
- ^ Robert R, Tcheung WJ, Rosenberg L, Rosenberg M, Mitchell C, Villarreal C, et al. (November 2008). "Treating thermally injured children suffering symptoms of acute stress with imipramine and fluoxetine: a randomized, double-blind study". Burns. 34 (7): 919–928. doi:10.1016/j.burns.2008.04.009. PMID 18675519.
- ^ Weizman R, Laor N, Schujovitsky A, Wolmer L, Abramovitz-Schnaider P, Freudstein-Dan A, et al. (July 1996). "Platelet imipramine binding in patients with posttraumatic stress disorder before and after phenelzine treatment". Psychiatry Research. 63 (2–3): 143–150. doi:10.1016/0165-1781(96)02760-6. PMID 8878310. S2CID 11314379.
- ^ Astill Wright L, Sijbrandij M, Sinnerton R, Lewis C, Roberts NP, Bisson JI (December 2019). "Pharmacological prevention and early treatment of post-traumatic stress disorder and acute stress disorder: a systematic review and meta-analysis". Translational Psychiatry. 9 (1): 334. doi:10.1038/s41398-019-0673-5. PMC 6901463. PMID 31819037.
- ^ Boaden K, Tomlinson A, Cortese S, Cipriani A (2020). "Antidepressants in Children and Adolescents: Meta-Review of Efficacy, Tolerability and Suicidality in Acute Treatment". Frontiers in Psychiatry. 11: 717. doi:10.3389/fpsyt.2020.00717. PMC 7493620. PMID 32982805.
- ^ Ghanizadeh A (July 2013). "A systematic review of the efficacy and safety of desipramine for treating ADHD". Current Drug Safety. 8 (3): 169–174. doi:10.2174/15748863113089990029. PMID 23914752.
- ^ Rosenbaum TG, Kou M (February 2005). "Are one or two dangerous? Tricyclic antidepressant exposure in toddlers". The Journal of Emergency Medicine. 28 (2): 169–174. doi:10.1016/j.jemermed.2004.08.018. PMID 15707813.
- ^ Bennett HJ (June 1982). "Imipramine and enuresis: never forget its dangers". Pediatrics. 69 (6): 831–832. doi:10.1542/peds.69.6.831. PMID 7079058. S2CID 29104331.
- ^ Delini-Stula A, Mikkelsen H, Angst J (October 1995). "Therapeutic efficacy of antidepressants in agitated anxious depression--a meta-analysis of moclobemide studies". Journal of Affective Disorders. 35 (1–2): 21–30. doi:10.1016/0165-0327(95)00034-K. PMID 8557884.
- ^ Orsulak PJ (September 1989). "Therapeutic monitoring of antidepressant drugs: guidelines updated". Therapeutic Drug Monitoring. 11 (5): 497–507. doi:10.1097/00007691-198909000-00002. PMID 2683251.
- ^ a b c d "Imipramine: MedlinePlus Drug Information". medlineplus.gov. Retrieved 2024-04-01.
- ^ a b "Imipramine Oral: Uses, Side Effects, Interactions, Pictures, Warnings & Dosing - WebMD". www.webmd.com. Retrieved 2024-04-01.
- ^ Skidmore-Roth L, ed. (2010). Mosby's Nursing Drug Reference (23rd ed.). St. Louis, MO: Mosby Elsevier.
- ^ a b Roth BL, Driscol J. "PDSP Ki Database". Psychoactive Drug Screening Program (PDSP). University of North Carolina at Chapel Hill and the United States National Institute of Mental Health. Retrieved 7 May 2022.
- ^ Roth BL, Driscol J. "PDSP Ki Database". Psychoactive Drug Screening Program (PDSP). University of North Carolina at Chapel Hill and the United States National Institute of Mental Health. Retrieved 7 May 2022.
- ^ a b c Tatsumi M, Groshan K, Blakely RD, Richelson E (December 1997). "Pharmacological profile of antidepressants and related compounds at human monoamine transporters". European Journal of Pharmacology. 340 (2–3): 249–258. doi:10.1016/s0014-2999(97)01393-9. PMID 9537821.
- ^ a b c d Owens MJ, Morgan WN, Plott SJ, Nemeroff CB (December 1997). "Neurotransmitter receptor and transporter binding profile of antidepressants and their metabolites". The Journal of Pharmacology and Experimental Therapeutics. 283 (3): 1305–1322. PMID 9400006.
- ^ a b c d e f Cusack B, Nelson A, Richelson E (May 1994). "Binding of antidepressants to human brain receptors: focus on newer generation compounds". Psychopharmacology. 114 (4): 559–565. doi:10.1007/bf02244985. PMID 7855217. S2CID 21236268.
- ^ a b c d e f Toll L, Berzetei-Gurske IP, Polgar WE, Brandt SR, Adapa ID, Rodriguez L, et al. (March 1998). "Standard binding and functional assays related to medications development division testing for potential cocaine and opiate narcotic treatment medications". NIDA Research Monograph. 178: 440–466. PMID 9686407.
- ^ a b Wander TJ, Nelson A, Okazaki H, Richelson E (December 1986). "Antagonism by antidepressants of serotonin S1 and S2 receptors of normal human brain in vitro". European Journal of Pharmacology. 132 (2–3): 115–121. doi:10.1016/0014-2999(86)90596-0. PMID 3816971.
- ^ Roth BL, Kroeze WK (2006). "Screening the receptorome yields validated molecular targets for drug discovery". Current Pharmaceutical Design. 12 (14): 1785–1795. doi:10.2174/138161206776873680. PMID 16712488.
- ^ Pälvimäki EP, Roth BL, Majasuo H, Laakso A, Kuoppamäki M, Syvälahti E, et al. (August 1996). "Interactions of selective serotonin reuptake inhibitors with the serotonin 5-HT2c receptor". Psychopharmacology. 126 (3): 234–240. doi:10.1007/bf02246453. PMID 8876023. S2CID 24889381.
- ^ Schmidt AW, Hurt SD, Peroutka SJ (November 1989). "'[3H]quipazine' degradation products label 5-HT uptake sites". European Journal of Pharmacology. 171 (1): 141–143. doi:10.1016/0014-2999(89)90439-1. PMID 2533080.
- ^ Monsma FJ, Shen Y, Ward RP, Hamblin MW, Sibley DR (March 1993). "Cloning and expression of a novel serotonin receptor with high affinity for tricyclic psychotropic drugs". Molecular Pharmacology. 43 (3): 320–327. PMID 7680751.
- ^ Shen Y, Monsma FJ, Metcalf MA, Jose PA, Hamblin MW, Sibley DR (August 1993). "Molecular cloning and expression of a 5-hydroxytryptamine7 serotonin receptor subtype". The Journal of Biological Chemistry. 268 (24): 18200–18204. doi:10.1016/S0021-9258(17)46830-X. PMID 8394362.
- ^ a b c d e f g Richelson E, Nelson A (July 1984). "Antagonism by antidepressants of neurotransmitter receptors of normal human brain in vitro". The Journal of Pharmacology and Experimental Therapeutics. 230 (1): 94–102. PMID 6086881.
- ^ Andersen PH (August 1989). "The dopamine inhibitor GBR 12909: selectivity and molecular mechanism of action". European Journal of Pharmacology. 166 (3): 493–504. doi:10.1016/0014-2999(89)90363-4. PMID 2530094.
- ^ Muth EA, Haskins JT, Moyer JA, Husbands GE, Nielsen ST, Sigg EB (December 1986). "Antidepressant biochemical profile of the novel bicyclic compound Wy-45,030, an ethyl cyclohexanol derivative". Biochemical Pharmacology. 35 (24): 4493–4497. doi:10.1016/0006-2952(86)90769-0. PMID 3790168.
- ^ Sánchez C, Hyttel J (August 1999). "Comparison of the effects of antidepressants and their metabolites on reuptake of biogenic amines and on receptor binding". Cellular and Molecular Neurobiology. 19 (4): 467–489. doi:10.1023/A:1006986824213. PMID 10379421. S2CID 19490821.
- ^ a b Deupree JD, Montgomery MD, Bylund DB (December 2007). "Pharmacological properties of the active metabolites of the antidepressants desipramine and citalopram". European Journal of Pharmacology. 576 (1–3): 55–60. doi:10.1016/j.ejphar.2007.08.017. PMC 2231336. PMID 17850785.
- ^ a b c d Appl H, Holzammer T, Dove S, Haen E, Strasser A, Seifert R (February 2012). "Interactions of recombinant human histamine H₁R, H₂R, H₃R, and H₄R receptors with 34 antidepressants and antipsychotics". Naunyn-Schmiedeberg's Archives of Pharmacology. 385 (2): 145–170. doi:10.1007/s00210-011-0704-0. PMID 22033803. S2CID 14274150.
- ^ a b c d e Stanton T, Bolden-Watson C, Cusack B, Richelson E (June 1993). "Antagonism of the five cloned human muscarinic cholinergic receptors expressed in CHO-K1 cells by antidepressants and antihistaminics". Biochemical Pharmacology. 45 (11): 2352–2354. doi:10.1016/0006-2952(93)90211-e. PMID 8100134.
- ^ Arias HR, Targowska-Duda KM, Feuerbach D, Sullivan CJ, Maciejewski R, Jozwiak K (March 2010). "Different interaction between tricyclic antidepressants and mecamylamine with the human alpha3beta4 nicotinic acetylcholine receptor ion channel". Neurochemistry International. 56 (4): 642–649. doi:10.1016/j.neuint.2010.01.011. PMID 20117161. S2CID 29461221.
- ^ Weber E, Sonders M, Quarum M, McLean S, Pou S, Keana JF (November 1986). "1,3-Di(2-[5-3H]tolyl)guanidine: a selective ligand that labels sigma-type receptors for psychotomimetic opiates and antipsychotic drugs". Proceedings of the National Academy of Sciences of the United States of America. 83 (22): 8784–8788. Bibcode:1986PNAS...83.8784W. doi:10.1073/pnas.83.22.8784. PMC 387016. PMID 2877462.
- ^ a b Hindmarch I, Hashimoto K (April 2010). "Cognition and depression: the effects of fluvoxamine, a sigma-1 receptor agonist, reconsidered". Human Psychopharmacology. 25 (3): 193–200. doi:10.1002/hup.1106. PMID 20373470. S2CID 26491662.
- ^ a b Robson MJ, Elliott M, Seminerio MJ, Matsumoto RR (April 2012). "Evaluation of sigma (σ) receptors in the antidepressant-like effects of ketamine in vitro and in vivo". European Neuropsychopharmacology. 22 (4): 308–317. doi:10.1016/j.euroneuro.2011.08.002. PMID 21911285. S2CID 24494428.
- ^ Teschemacher AG, Seward EP, Hancox JC, Witchel HJ (September 1999). "Inhibition of the current of heterologously expressed HERG potassium channels by imipramine and amitriptyline". British Journal of Pharmacology. 128 (2): 479–485. doi:10.1038/sj.bjp.0702800. PMC 1571643. PMID 10510461.
- ^ Imipramine hydrochloride | DrugBank Online
- ^ Smiałowski A (May 1991). "Dopamine D2 receptor blocking effect of imipramine in the rat hippocampus". Pharmacology, Biochemistry, and Behavior. 39 (1): 105–108. doi:10.1016/0091-3057(91)90404-p. PMID 1924491. S2CID 36818141.
- ^ Schulze DR, Carroll FI, McMahon LR (August 2012). "Interactions between dopamine transporter and cannabinoid receptor ligands in rhesus monkeys". Psychopharmacology. 222 (3): 425–438. doi:10.1007/s00213-012-2661-9. PMC 3620032. PMID 22374253.
- ^ Dickinson KE, Matsumoto H, Anderson W, Pruitt RE, Uemura N, Hirschowitz BI (September 1988). "Muscarinic cholinergic receptor subtype on frog esophageal peptic cells: binding and secretion studies". The Journal of Pharmacology and Experimental Therapeutics. 246 (3): 879–886. PMID 2901489.
- ^ Everett HC (November 1975). "The use of bethanechol chloride with tricyclic antidepressants". The American Journal of Psychiatry. 132 (11): 1202–1204. doi:10.1176/ajp.132.11.1202. PMID 1166898.
- ^ Rosen J, Pollock BG, Altieri LP, Jonas EA (August 1993). "Treatment of nortriptyline's side effects in elderly patients: a double-blind study of bethanechol". The American Journal of Psychiatry. 150 (8): 1249–1251. doi:10.1176/ajp.150.8.1249. PMID 8101048.
- ^ Yager J (April 1986). "Bethanechol chloride can reverse erectile and ejaculatory dysfunction induced by tricyclic antidepressants and mazindol: case report". The Journal of Clinical Psychiatry. 47 (4): 210–211. PMID 3957884.
- ^ Segraves RT (September 1987). "Reversal by bethanechol of imipramine-induced ejaculatory dysfunction". The American Journal of Psychiatry. 144 (9): 1243–1244. doi:10.1176/ajp.144.9.1243b. PMID 3631333.
- ^ Bernik M, Vieira AH, Nunes PV (December 2004). "Bethanecol chloride for treatment of clomipramine-induced orgasmic dysfunction in males". Revista do Hospital das Clinicas. 59 (6): 357–360. doi:10.1590/s0041-87812004000600008. PMID 15654489.
- ^ Tsankova NM, Berton O, Renthal W, Kumar A, Neve RL, Nestler EJ (April 2006). "Sustained hippocampal chromatin regulation in a mouse model of depression and antidepressant action". Nature Neuroscience. 9 (4): 519–525. doi:10.1038/nn1659. PMID 16501568. S2CID 21547891.
- ^ Krishnan V, Nestler EJ (October 2008). "The molecular neurobiology of depression". Nature. 455 (7215): 894–902. Bibcode:2008Natur.455..894K. doi:10.1038/nature07455. PMC 2721780. PMID 18923511.
- ^ a b Sallee FR, Pollock BG (May 1990). "Clinical pharmacokinetics of imipramine and desipramine". Clinical Pharmacokinetics. 18 (5): 346–364. doi:10.2165/00003088-199018050-00002. PMID 2185906.
- ^ a b Ritsner MS (15 February 2013). "Appendix 2: List of Psychotropic Medications". Polypharmacy in Psychiatry Practice, Volume I: Multiple Medication Use Strategies. Springer Science & Business Media. pp. 270–271. ISBN 978-94-007-5805-6.
- ^ Williams DA (2008). "Antidepressants". In Lemke TL, Williams DA (eds.). Foye's Principles of Medicinal Chemistry. Lippincott Williams & Wilkins. p. 580. ISBN 978-0-7817-6879-5.
- ^ Dawkins K, Manji HK, Potter TW (20 September 1994). "Dawkins Manji Potter pharmacodynamics of antidepressants". In Cutler NR, Sramek JJ, Narang PK (eds.). Pharmacodynamics and Drug Development: Perspectives in Clinical Pharmacology. John Wiley & Sons. p. 160. ISBN 978-0-471-95052-3.
- ^ Baumann P, Hiemke C (23 February 2012). "Central Nervous System Drugs". In Anzenbacher P, Zanger UM (eds.). Metabolism of Drugs and Other Xenobiotics. John Wiley & Sons. pp. 302–. ISBN 978-3-527-64632-6.
- ^ Anthony PK, Powers A (2002). "Drugs Used in the Therapy of Depression". In Anthony PK (ed.). Pharmacology Secrets. Elsevier Health Sciences. p. 39. ISBN 1-56053-470-2.
- ^ Cowen P, Harrison P, Burns T (9 August 2012). "Drugs and other physical treatments". Shorter Oxford Textbook of Psychiatry. OUP Oxford. p. 532. ISBN 978-0-19-162675-3.
- ^ a b c d Elks J (14 November 2014). The Dictionary of Drugs: Chemical Data: Chemical Data, Structures and Bibliographies. Springer. p. 680. ISBN 978-1-4757-2085-3.
- ^ a b c d e f g Index Nominum 2000: International Drug Directory. Taylor & Francis. 2000. p. 546. ISBN 978-3-88763-075-1.
- ^ Boschmans SA, Perkin MF, Terblanche SE (1987). "Antidepressant drugs: imipramine, mianserin and trazodone". Comparative Biochemistry and Physiology. C, Comparative Pharmacology and Toxicology. 86 (2): 225–232. doi:10.1016/0742-8413(87)90073-9. PMID 2882911.
- ^ Ban TA (May 2001). "Pharmacotherapy of mental illness--a historical analysis". Progress in Neuro-Psychopharmacology & Biological Psychiatry. 25 (4): 709–727. doi:10.1016/S0278-5846(01)00160-9. PMID 11383974. S2CID 20630716.
- ^ Joergensen TK, Andersen KE, Lau J, Madsen P, Huusfeldt PO (1999). "Synthesis of substituted 10,11-dihydro-5H-dibenz[b,f]azepines; key synthons in syntheses of pharmaceutically active compounds". Journal of Heterocyclic Chemistry. 36 (1): 57–64. doi:10.1002/jhet.5570360110. ISSN 0022-152X.
- ^ Newbould NN (2012). "The future of drug discovery". In Walker SR (ed.). Trends and Changes in Drug Research and Development. Springer Science & Business Media. p. 109. ISBN 9789400926592.
- ^ Kanba S, Wada H (22 February 1991). "Interactions with Psychotropic Drugs". In Watanabe T, Wada H (eds.). Histaminergic Neurons: Morphology and Function. CRC Press. p. 272. ISBN 978-0-8493-6425-9.
- ^ Bennett MR (21 April 2014). "Monoaminergic Synapses and Schziophrenia: The Discovery of Neuroleptics". History of the Synapse. CRC Press. p. 90. ISBN 978-1-4822-8417-1.
- ^ a b Mitchell ES, Triggle DJ (2009). "Introduction, History, and Brain Basics". Antidepressants. Infobase Publishing. p. 15. ISBN 978-1-4381-0192-7.
- ^ a b c Wilkinson ST, Ostroff RB, Katz RB, Krystal JH (2 January 2018). "Ketamine: A Promising Rapid-Acting Antidepressant". In Kim YK (ed.). Understanding Depression: Volume 2. Clinical Manifestations, Diagnosis and Treatment. Springer. p. 224. ISBN 978-981-10-6577-4.
- ^ a b Abdallah CG, Sanacora G, Duman RS, Krystal JH (October 2018). "The neurobiology of depression, ketamine and rapid-acting antidepressants: Is it glutamate inhibition or activation?". Pharmacology & Therapeutics. 190: 148–158. doi:10.1016/j.pharmthera.2018.05.010. PMC 6165688. PMID 29803629.
- ^ a b Bernadt M (April 2007). "Drug Treatment of Depression". In Stein G, Wilkinson G (eds.). Seminars in General Adult Psychiatry. RCPsych Publications. p. 71. ISBN 978-1-904671-44-2.
- ^ Lowry W (6 December 2012). "Controlled and Non-controlled but Commonly Abused Substances". Forensic Toxicology: Controlled Substances and Dangerous Drugs. Springer Science & Business Media. p. 248. ISBN 978-1-4684-3444-6.
- ^ Healy D (1997). The Antidepressant Era. Harvard University Press. p. 211. ISBN 9780674039575.
- ^ Bottlender R, Rudolf D, Strauss A, Möller HJ (1998). "Antidepressant-associated maniform states in acute treatment of patients with bipolar-I depression". European Archives of Psychiatry and Clinical Neuroscience. 248 (6): 296–300. doi:10.1007/s004060050053. PMID 9928908. S2CID 25542287.
- ^ Morton IK, Hall JM (6 December 2012). Concise Dictionary of Pharmacological Agents: Properties and Synonyms. Springer Science & Business Media. p. 151. ISBN 978-94-011-4439-1.
- ^ a b c d e f "Imipramine Uses, Side Effects & Warnings". Drugs.com.
- ^ Pies RW (2 April 2007). Handbook of Essential Psychopharmacology. American Psychiatric Publishing. p. 79. ISBN 978-1-58562-660-1.
- ^ Jack RH, Hollis C, Coupland C, Morriss R, Knaggs RD, Butler D, et al. (July 2020). Hellner C (ed.). "Incidence and prevalence of primary care antidepressant prescribing in children and young people in England, 1998-2017: A population-based cohort study". PLOS Medicine. 17 (7): e1003215. doi:10.1371/journal.pmed.1003215. PMC 7375537. PMID 32697803.
Further reading
[edit]- Dean L (2017). "Imipramine Therapy and CYP2D6 and CYP2C19 Genotype". In Pratt VM, McLeod HL, Rubinstein WS, Scott SA, Dean LC, Kattman BL, et al. (eds.). Medical Genetics Summaries. National Center for Biotechnology Information (NCBI). PMID 28520379. Bookshelf ID: NBK425164.
- Alpha-1 blockers
- CYP2D6 inhibitors
- D2 antagonists
- Dibenzazepines
- Dimethylamino compounds
- Drugs developed by Novartis
- Glycine receptor antagonists
- H1 receptor antagonists
- M1 receptor antagonists
- M2 receptor antagonists
- M3 receptor antagonists
- M4 receptor antagonists
- M5 receptor antagonists
- Nicotinic antagonists
- Serotonin receptor antagonists
- Serotonin–norepinephrine reuptake inhibitors
- Tricyclic antidepressants
