Ibogaine: Difference between revisions
TheRingess (talk | contribs) Undid revision 369494330 by 66.190.236.23 (talk) |
|||
| Line 44: | Line 44: | ||
== Side effects and safety == |
== Side effects and safety == |
||
One of the first noticeable effects of large-dose ibogaine ingestion is [[ataxia]], a difficulty in coordinating muscle motion which makes standing and walking difficult without assistance. [[Xerostomia]] (dry mouth), [[nausea]], and vomiting may follow. These symptoms may be long in duration, ranging from 4 to 24 hours in some cases. Ibogaine is sometimes administered by enema to help the subject avoid vomiting up the dose. Psychiatric medications are strongly contraindicated in ibogaine therapy due to adverse interactions. Some studies also suggest the possibility of adverse interaction with heart conditions. In one study of canine subjects, ibogaine was observed to increase [[sinus arrhythmia]] (the normal change in heart rate during respiration).<ref>http://www.puzzlepiece.org/ibogaine/literature/gershon1962.pdf</ref> Ventricular [[ectopy]] has been observed in a minority of patients during ibogaine therapy.<ref>[http://www.doraweiner.org/aatod_hrc.html Dora Weiner Foundation Conferences: 2004, Reports and Exhibits - AATOD and HRC<!-- Bot generated title -->]</ref> It has been proposed that there is a risk of QT-interval prolongation following ibogaine administration.<ref>{{cite journal |author=Maas U, Strubelt S |title=Fatalities after taking ibogaine in addiction treatment could be related to sudden cardiac death caused by autonomic dysfunction |journal=Med. Hypotheses |volume=67 |issue=4 |pages=960–4 |year=2006 |pmid=16698188 |doi=10.1016/j.mehy.2006.02.050 |url=http://linkinghub.elsevier.com/retrieve/pii/S0306-9877(06)00209-X}}</ref> This risk was further demonstrated by a case reported in the [[New England Journal of Medicine]] documenting [[prolonged QT interval]] and [[ventricular tachycardia]] after initial use.<ref>{{cite journal |author=Hoelen DW, Spiering W, Valk GD |title=Long-QT syndrome induced by the antiaddiction drug ibogaine |journal=N. Engl. J. Med. |volume=360 |issue=3 |pages=308–9 |year=2009 |month=January |pmid=19144953 |doi=10.1056/NEJMc0804248 }}</ref> |
One of the first noticeable effects of large-dose ibogaine ingestion is [[ataxia]], a difficulty in coordinating muscle motion which makes standing and walking difficult without assistance. [[Xerostomia]] (dry mouth), [[nausea]], and vomiting may follow. These symptoms may be long in duration, ranging from 4 to 24 hours in some cases. Ibogaine is sometimes administered by enema to help the subject avoid vomiting up the dose. Ibogaine generally causes sleep disruption, decreased appetite, and extreme fatigue for approximately 5-7 days after its use. |
||
Psychiatric medications are strongly contraindicated in ibogaine therapy due to adverse interactions. Some studies also suggest the possibility of adverse interaction with heart conditions. In one study of canine subjects, ibogaine was observed to increase [[sinus arrhythmia]] (the normal change in heart rate during respiration).<ref>http://www.puzzlepiece.org/ibogaine/literature/gershon1962.pdf</ref> Ventricular [[ectopy]] has been observed in a minority of patients during ibogaine therapy.<ref>[http://www.doraweiner.org/aatod_hrc.html Dora Weiner Foundation Conferences: 2004, Reports and Exhibits - AATOD and HRC<!-- Bot generated title -->]</ref> It has been proposed that there is a risk of QT-interval prolongation following ibogaine administration.<ref>{{cite journal |author=Maas U, Strubelt S |title=Fatalities after taking ibogaine in addiction treatment could be related to sudden cardiac death caused by autonomic dysfunction |journal=Med. Hypotheses |volume=67 |issue=4 |pages=960–4 |year=2006 |pmid=16698188 |doi=10.1016/j.mehy.2006.02.050 |url=http://linkinghub.elsevier.com/retrieve/pii/S0306-9877(06)00209-X}}</ref> This risk was further demonstrated by a case reported in the [[New England Journal of Medicine]] documenting [[prolonged QT interval]] and [[ventricular tachycardia]] after initial use.<ref>{{cite journal |author=Hoelen DW, Spiering W, Valk GD |title=Long-QT syndrome induced by the antiaddiction drug ibogaine |journal=N. Engl. J. Med. |volume=360 |issue=3 |pages=308–9 |year=2009 |month=January |pmid=19144953 |doi=10.1056/NEJMc0804248 }}</ref> |
|||
There are 12 documented fatalities that have been loosely associated with ibogaine ingestion.<ref>[http://myeboga.com/fatalities.html Ibogaine & Eboga (Related) Recorded Fatalities<!-- Bot generated title -->]</ref> Exact determinations of the cause of death have proven elusive due to the quasi-legal status of ibogaine and the unfamiliarity of medical professionals with this relatively rare substance. No autopsy to date has implicated ibogaine as the sole cause of death. Causes given range from significant pre-existing medical problems to the surreptitious consumption of other drugs in conjunction with ibogaine. Many legal and illegal psychoactive drugs and even foods or supplements such as [[List of drugs affected by grapefruit|grapefruit juice]] and [[Goldenseal#How_goldenseal_works|goldenseal]] are strongly contraindicated immediately before, during or immediately after ibogaine treatment, which presents a risk in undersupervised or self-treating persons. |
There are 12 documented fatalities that have been loosely associated with ibogaine ingestion.<ref>[http://myeboga.com/fatalities.html Ibogaine & Eboga (Related) Recorded Fatalities<!-- Bot generated title -->]</ref> Exact determinations of the cause of death have proven elusive due to the quasi-legal status of ibogaine and the unfamiliarity of medical professionals with this relatively rare substance. No autopsy to date has implicated ibogaine as the sole cause of death. Causes given range from significant pre-existing medical problems to the surreptitious consumption of other drugs in conjunction with ibogaine. Many legal and illegal psychoactive drugs and even foods or supplements such as [[List of drugs affected by grapefruit|grapefruit juice]] and [[Goldenseal#How_goldenseal_works|goldenseal]] are strongly contraindicated immediately before, during or immediately after ibogaine treatment, which presents a risk in undersupervised or self-treating persons. |
||
Revision as of 22:04, 5 July 2010
 | |
 | |
| Clinical data | |
|---|---|
| Routes of administration | oral |
| ATC code |
|
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Elimination half-life | 2 hours |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| ChemSpider | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.001.363 |
| Chemical and physical data | |
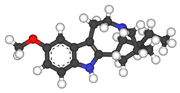
| Formula | C20H26N2O |
| Molar mass | 310.433 g/mol g·mol−1 |
| 3D model (JSmol) | |
| Melting point | 152 to 153 °C (306 to 307 °F) |
| |
Ibogaine is a naturally occurring psychoactive substance found in a number of plants, principally in a member of the Apocynaceae family known as iboga (Tabernanthe iboga). Ibogaine-containing preparations are used in medicinal and ritual purposes within African spiritual traditions of the Bwiti, who claim to have learned it from the Pygmy. In recent times, it has been identified as having anti-addictive properties. Ibogaine is an indole alkaloid that is obtained either by extraction from the iboga plant or by semi-synthesis from the precursor compound voacangine, another plant alkaloid. A full organic synthesis of ibogaine has been achieved but is too expensive and challenging to produce any commercially significant yield.
In the early 1960s, anecdotal reports appeared concerning ibogaine's effects.[1] Since that time, it has been the subject of investigation into its abilities to interrupt addictions to methadone, heroin, alcohol, and cocaine. It is thought that ibogaine may have potential to facilitate introspection, helping to elucidate the psychological issues and behavior patterns that drive addictions or other problems. However, ibogaine therapy for drug addiction is the subject of some controversy. Due to safety concerns, it has been placed in the strictest drug prohibition schedules in the United States and a handful of other countries. Canada and Mexico both allow ibogaine therapy facilities to operate and openly contribute to further understanding of the detoxification and therapeutic process that ibogaine has the potential to facilitate.
While ibogaine's prohibition in the U.S. has slowed scientific research into its anti-addictive properties, the use of ibogaine for drug treatment has grown in the form of a large worldwide medical subculture.[2] Ibogaine is now used by treatment clinics in 12 countries on six continents to facilitate detoxification and chemical dependence to substances such as methadone, heroin, alcohol, powder cocaine, crack cocaine, and methamphetamine, as well as to facilitate psychological introspection and spiritual exploration.
Psychoactive effects
At doses of around 3–5 mg/kg of body weight, ibogaine has a mild stimulant effect. The high-dose ibogaine experience of 10 mg/kg or greater most commonly occurs as two distinct phases: the visual phase and the introspective phase.[citation needed]
The visual phase is characterized by open-eye visuals, closed-eye visuals, and dreamlike sequences. Objects may be seen as distorted, projecting tracers, or having moving colors or textures. When the eyes are closed, extremely detailed and vivid geometric and fractal visions may be seen. Subjective reports often include a movie-like recollection of earlier life experiences as well as dreamlike sequences with symbolism of one's present or anticipated future. Other effects in the visual phase may include laughing, sensations of euphoria or fear, and temporary short-term memory impairment. The visual phase usually ends after one to four hours, after which the introspective phase begins.[citation needed]
The introspective phase is typically reported to bring elevated mood, a sense of calm and euphoria, and a distinct intellectual and emotional clarity. Subjects often report being able to accomplish deep emotional and intellectual introspection into psychological and emotional concerns. It is also during this period that opioid addicts first notice the absence of withdrawal symptoms or cravings. The duration of the introspective phase is highly variable, usually lasting hours but sometimes lasting days.[citation needed]
Side effects and safety
One of the first noticeable effects of large-dose ibogaine ingestion is ataxia, a difficulty in coordinating muscle motion which makes standing and walking difficult without assistance. Xerostomia (dry mouth), nausea, and vomiting may follow. These symptoms may be long in duration, ranging from 4 to 24 hours in some cases. Ibogaine is sometimes administered by enema to help the subject avoid vomiting up the dose. Ibogaine generally causes sleep disruption, decreased appetite, and extreme fatigue for approximately 5-7 days after its use.
Psychiatric medications are strongly contraindicated in ibogaine therapy due to adverse interactions. Some studies also suggest the possibility of adverse interaction with heart conditions. In one study of canine subjects, ibogaine was observed to increase sinus arrhythmia (the normal change in heart rate during respiration).[3] Ventricular ectopy has been observed in a minority of patients during ibogaine therapy.[4] It has been proposed that there is a risk of QT-interval prolongation following ibogaine administration.[5] This risk was further demonstrated by a case reported in the New England Journal of Medicine documenting prolonged QT interval and ventricular tachycardia after initial use.[6]
There are 12 documented fatalities that have been loosely associated with ibogaine ingestion.[7] Exact determinations of the cause of death have proven elusive due to the quasi-legal status of ibogaine and the unfamiliarity of medical professionals with this relatively rare substance. No autopsy to date has implicated ibogaine as the sole cause of death. Causes given range from significant pre-existing medical problems to the surreptitious consumption of other drugs in conjunction with ibogaine. Many legal and illegal psychoactive drugs and even foods or supplements such as grapefruit juice and goldenseal are strongly contraindicated immediately before, during or immediately after ibogaine treatment, which presents a risk in undersupervised or self-treating persons.
Therapeutic uses
Treatment for opiate addiction
The most-studied therapeutic effect of ibogaine is the reduction or elimination of addiction to opioids.[1] An integral effect is the alleviation of symptoms of opioid withdrawal. Research also suggests that ibogaine may be useful in treating dependence on other substances such as alcohol, methamphetamine, and nicotine and may affect compulsive behavioral patterns not involving substance abuse or chemical dependence.[1]
Proponents of ibogaine treatment for drug addiction have established formal and informal clinics or self-help groups in Canada, Mexico, the Caribbean, Costa Rica, the Czech Republic, France, Slovenia, the Netherlands, Brazil, South Africa, the United Kingdom and New Zealand, where ibogaine is administered as an experimental compound. Many users of ibogaine report experiencing visual phenomena during a waking dream state, such as instructive replays of life events that led to their addiction, while others report therapeutic shamanic visions that help them conquer the fears and negative emotions that might drive their addiction. It is proposed that intensive counseling, therapy and aftercare during the interruption period following treatment is of significant value. Some individuals require a second or third treatment session with ibogaine over the course of the next 12 to 18 months. A minority of individuals relapse completely into opiate addiction within days or weeks. A comprehensive article (Lotsof 1995) on the subject of ibogaine therapy detailing the procedure, effects and aftereffects is found in "Ibogaine in the Treatment of Chemical Dependence Disorders: Clinical Perspectives".[8] Ibogaine has also been reported in multiple small-study cohorts to reduce cravings for methamphetamine.[9]
Chronic pain management
In 1957, Jurg Schneider, a pharmacologist at CIBA, found that ibogaine potentiates morphine analgesia.[10] Further research was abandoned, and no additional data was ever published by Ciba researchers on ibogaine–opioid interactions. Almost 50 years later, Patrick Kroupa and Hattie Wells released the first treatment protocol for concomitant administration of ibogaine with opioids in human subjects, indicating ibogaine reduced tolerance to opioid drugs.[11] Kroupa et al. published their research in the Multidisciplinary Association for Psychedelic Studies Journal demonstrating that administration of low-"maintenance" doses of ibogaine HCl with opioids decreases tolerance. It should be noted however, that the potentiation action of ibogaine may make this a very risky procedure.
Psychotherapy
Ibogaine has been used as an adjunct to psychotherapy by Claudio Naranjo, documented in his book The Healing Journey.[12]
Recreational use
Casual use of ibogaine in a social or entertainment context is nearly unknown due to its high cost, constrained availability, long duration of effects, and uncomfortable short-term side effects. In the clandestine markets, ibogaine is typically sought as a drug addiction treatment, for ritual spiritual purposes, or psychological introspection.
History
It is uncertain exactly how long iboga has been used in African spiritual practice, but its activity was first observed by French and Belgian explorers in the 19th century. The first botanical description of the Tabernanthe iboga plant was made in 1889. Ibogaine was first isolated from T. iboga in 1901 by Dybowski and Landrin[13] and independently by Haller and Heckel in the same year using T. iboga samples from Gabon. In the 1930s, ibogaine was sold in France in 8 mg tablets under the name "Lambarene". The total synthesis of ibogaine was accomplished by G. Büchi in 1966.[14] Since then, several further totally synthetic routes have been developed.[15] The use of ibogaine in treating substance use disorders in human subjects was first observed by Howard Lotsof in 1962, for which he was later awarded U.S. patent 4,499,096 in 1985. In 1969, Claudio Naranjo was granted a French patent for the use of ibogaine in psychotherapy.
Ibogaine was placed in US Schedule 1 in 1967 as part of the US government's strong response to the upswing in popularity of psychedelic substances, though iboga itself was scarcely known at the time. Ibogaine's ability to attenuate opioid withdrawal confirmed in the rat was first published by Dzoljic et al. (1988).[16] Ibogaine's use in diminishing morphine self-administration in preclinical studies was shown by Glick et al. (1991)[17] and ibogaine's capacity to reduce cocaine self-administration in the rat was shown by Cappendijk et al. (1993).[18] Animal model support for ibogaine claims to treat alcohol dependence were established by Rezvani (1995).[19]
The name "Indra extract", in strict terms, refers to 44 kg of an iboga extract manufactured by an unnamed European industrial manufacturer in 1981. This stock was later purchased by Carl Waltenburg, who distributed it under the name "Indra extract". Waltenburg used this extract to treat heroin addicts in Christiania, Denmark, a squatter village where heroin addiction was widespread in 1982.[20] Indra extract was offered for sale over the Internet until 2006, when the Indra web presence disappeared. It is unclear whether the extracts currently sold as "Indra extract" are actually from Waltenburg's original stock, or whether any of that stock is even viable or in existence. Ibogaine and related indole compounds are susceptible to oxidation when exposed to oxygen[21] [22], as opposed to their salt form, which is stable. The exact methods and quality of the original Indra extraction was never documented, so the real composition of the product remains uncertain.
Data demonstrating ibogaine's efficacy in attenuating opioid withdrawal in drug-dependent human subjects was published by Alper et al. (1999)[23] and Mash et al. (2000).[24]
In 1972, journalist Hunter S. Thompson accused democratic candidate Edmund Muskie of being addicted to ibogaine in a satirical piece. Many readers, and even other journalists, did not realize that Thompson was being facetious. The claim, of course, was completely unfounded, and Thompson himself is documented in the movie Gonzo: The Life and Work of Dr. Hunter S. Thompson discussing the self-fabricated joke of Muskie's alleged ibogaine use and his surprise that anyone actually believed the claim.
Formulations
In Bwiti religious ceremonies, the rootbark is pulverized and swallowed in large amounts to produce intense psychoactive effects. In Africa, iboga rootbark is sometimes chewed, which releases small amounts of ibogaine to produce a stimulant effect. Ibogaine is also available in a total alkaloid extract of the Tabernanthe iboga plant, which also contains all the other iboga alkaloids and thus has only about one-fifth the potency by weight as standardized ibogaine hydrochloride.[25]
Total alkaloid extracts of T. iboga are often loosely called "Indra extract". However, that name actually refers to a particular stock of total alkaloid extract produced in Europe in 1981. The fate of that original stock (as well as its original quality) is unknown.
Currently, pure crystalline ibogaine hydrochloride is the most standardized formulation. It is typically produced by the semi-synthesis from voacangine in commercial laboratories. Ibogaine has two separate chiral centers which means that there a four different stereoisomers of ibogaine. These four isomers are difficult to resolve.[26]
A synthetic derivative of ibogaine, 18-methoxycoronaridine (18-MC), is a selective α3β4 antagonist that was developed collaboratively by the neurologist Stanley D. Glick (Albany) and the chemist Martin E. Kuehne (Vermont).[27] This discovery was stimulated by earlier studies on other naturally occurring analogues of ibogaine such as coronaridine and voacangine that showed these compounds also have anti-addictive properties.[28][29]
Pharmacology
The pharmacology of ibogaine is quite complex, affecting many different neurotransmitter systems simultaneously.[30][31] Because of its fairly low potency at any of its target sites, ibogaine is used in doses anywhere from 5 mg/kg of body weight for a minor effect to 30 mg/kg in the cases of strong polysubstance addiction. It is unknown whether doses greater than 30 mg/kg in humans produce effects that are therapeutically beneficial, medically risky, or simply prolonged in duration. In animal neurotoxicity studies, there was no observable neurotoxicity of ibogaine at 25 mg/kg, but at 50 mg/kg, one-third of the rats had developed patches of neurodegeneration, and at doses of 75 mg/kg or above, all rats showed a characteristic pattern of degeneration of Purkinje neurons, mainly in the cerebellum.[32] While caution should be exercised when extrapolating animal studies to humans, these results suggest that neurotoxicity of ibogaine is likely to be minimal when ibogaine is used in the 10–20 mg/kg range typical of drug addiction interruption treatment regimes, and indeed death from the other pharmacological actions of the alkaloids is likely to occur by the time the dose is high enough to produce consistent neurotoxic changes.[22][33]
Metabolites
Ibogaine is metabolized in the human body by cytochrome P450 2D6, and the major metabolite is noribogaine (12-hydroxyibogamine). Noribogaine is most potent as a serotonin reuptake inhibitor and acts as a moderate κ- and weak µ-opioid receptor full agonist and therefore, also has an aspect of an opiate replacement similar to compounds like methadone. It is possible that this action of noribogaine at the kappa opioid receptor may indeed contribute significantly to the psychoactive effects attributed to ibogaine ingestion; salvia divinorum, another plant recognized for its strong hallucinogenic properties, contains the chemical salvinorin-A which is a highly selective kappa opioid agonist. Both ibogaine and noribogaine have a plasma half-life of around two hours in the rat[34], although the half-life of noribogaine is slightly longer than the parent compound. It is proposed that ibogaine is deposited in fat and metabolized into noribogaine as it is released.[35] Noribogaine shows higher plasma levels than ibogaine and may therefore be detected for longer periods of time than ibogaine. Noribogaine is also more potent than ibogaine in rat drug discrimination assays when tested for the subjective effects of ibogaine.[36] The Noribogaine differs from ibogaine in that it contains a hydroxy instead of a methoxy group at the 12 position.
Research
An ibogaine research project was funded by the US National Institute on Drug Abuse in the early 1990s. The National Institute on Drug Abuse (NIDA) abandoned efforts to continue this project into clinical studies in 1995, citing other reports that suggested a risk of brain damage with extremely high doses and fatal heart arrhythmia in patients having a history of health problems,[citation needed] as well as inadequate funding for ibogaine development within their budget. However, NIDA funding for ibogaine research continues in indirect grants often cited in peer-reviewed ibogaine publications.
In addition, after years of work and a number of significant changes to the original protocol, on August 17, 2006, a MAPS-sponsored research team received "unconditional approval" from a Canadian Institutional Review Board (IRB) to proceed with a long-term observational case study that will examine changes in substance use in 20 consecutive people seeking ibogaine-based therapy for opiate dependence at the Iboga Therapy House in British Columbia, Canada.
Legal status
Ibogaine and its salts were regulated by the U.S. Food and Drug Administration in 1967 pursuant to its enhanced authority to regulate stimulants, depressants, and hallucinogens granted by the 1965 Drug Abuse Control Amendments (DACA) to the Federal Food, Drug, and Cosmetic Act. In 1970, with the passage of the Controlled Substances Act, it was classified as a Schedule I-controlled substance in the United States, along with other psychedelics such as DMT and mescaline. Since that time, several other countries, including Sweden, Denmark, Belgium, and Switzerland, have also banned the sale and possession of ibogaine. Although illegal in these countries, ibogaine has been used by hundreds of drug dependents in the United States and abroad. Howard Lotsof, a pioneer in bringing awareness to ibogaine's success in helping hardcore drug dependents to quit their addiction, and others have been offering willing persons the treatment. In the Czech Republic and Slovenia, taking advantage of less prohibitive legal systems, ibogaine has been applied to people coming from the U.S. and other countries seeking a safe haven.
Canada
Ibogaine is not the subject of any regulation in Canada.[37][38]
Sweden
In early 2006, a non-profit foundation addressing the issue of providing ibogaine for the purpose of addiction interruption within established drug treatment care was formed in Sweden.[39]
In popular culture
Ibogaine first appeared in popular culture in the writings of Hunter S. Thompson. While covering the Wisconsin primaries of the 1972 U.S. Presidential primaries for Rolling Stone magazine, Thompson claimed that presidential candidate Edmund Muskie showed symptoms of being under the influence of Ibogaine. This assertion was later revealed by Thompson to be false, one that he had planted as media bait. He himself was surprised when the leading media outlets picked up the story and ran with it.[40]
It also appeared in the seventh episode of the eleventh season of Law & Order: Special Victims Unit. In the episode, Doctor Huang administers Ibogaine to a heroin addict so that he can testify against a murderer.[41]
See also
References
- ^ a b c K.R. Alper, H.S. Lotsof, G.M. Frenken , D.J. Luciano , J. Bastiaans (1999). "Treatment of Acute Opioid Withdrawal with Ibogaine" (PDF). The American Journal on Addictions. 8 (3): 234–42. doi:10.1080/105504999305848. PMID 10506904. Retrieved 2009-06-16.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ K.R. Alper, H.S. Lotsof, C.D. Kaplan (2008). "The Ibogaine Medical Subculture". J. Ethnopharmacology. 115: 9–24. doi:10.1016/j.jep.2007.08.034. Retrieved 2008-02-22.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ http://www.puzzlepiece.org/ibogaine/literature/gershon1962.pdf
- ^ Dora Weiner Foundation Conferences: 2004, Reports and Exhibits - AATOD and HRC
- ^ Maas U, Strubelt S (2006). "Fatalities after taking ibogaine in addiction treatment could be related to sudden cardiac death caused by autonomic dysfunction". Med. Hypotheses. 67 (4): 960–4. doi:10.1016/j.mehy.2006.02.050. PMID 16698188.
- ^ Hoelen DW, Spiering W, Valk GD (2009). "Long-QT syndrome induced by the antiaddiction drug ibogaine". N. Engl. J. Med. 360 (3): 308–9. doi:10.1056/NEJMc0804248. PMID 19144953.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Ibogaine & Eboga (Related) Recorded Fatalities
- ^ H.S. Lotsof (1995). Ibogaine in the Treatment of Chemical Dependence Disorders: Clinical Perspectives (Originally published in MAPS Bulletin (1995) V(3):19-26)
- ^ Giannini, A. James (1997). Drugs of Abuse (2nd ed.). Practice Management Information Corporation. ISBN 1-57066-053-0.
- ^ Jurg Schneider (assignee: Ciba Pharmaceuticals), Tabernanthine, Ibogaine Containing Analgesic Compositions. US Patent No. 2,817,623 (1957) (pdf)
- ^ Patrick K. Kroupa, Hattie Wells (2005): Ibogaine in the 21st Century. Multidisciplinary Association for Psychedelic Studies. Volume XV, Number 1: 21-25 (pdf)
- ^ Naranjo, Claudio (1973). "V, Ibogaine: Fantasy and Reality". The healing journey: new approaches to consciousness. New York: Pantheon Books. pp. 197–231. ISBN 0-394-48826-1.
- ^ J. Dybowski, E. Landrin (1901). "PLANT CHEMISTRY. Concerning Iboga, its excitement-producing properties, its composition, and the new alkaloid it contains, ibogaine". C. R. Acad. Sci. 133: 748. Retrieved 2006-06-23.
- ^ G. Büchi, D.L. Coffen, Karoly Kocsis, P.E. Sonnet, and Frederick E. Ziegler (1966). "The Total Synthesis of Iboga Alkaloids" (pdf). J. Am. Chem. Soc. 88 (13): 3099–3109. doi:10.1021/ja00965a039. Retrieved 2006-06-23.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ C. Frauenfelder (1999) Doctoral Thesis, page 24 (pdf)
- ^ Dzoljic ED, Kaplan CD, Dzoljic MR (1988). "Effect of ibogaine on naloxone-precipitated withdrawal syndrome in chronic morphine-dependent rats". Arch Int Pharmacodyn Ther. 294: 64–70. PMID 3233054.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Glick SD, Rossman K, Steindorf S, Maisonneuve IM, Carlson JN (1991). "Effects and aftereffects of ibogaine on morphine self-administration in rats". Eur. J. Pharmacol. 195 (3): 341–345. doi:10.1016/0014-2999(91)90474-5. PMID 1868880.
{{cite journal}}:|access-date=requires|url=(help)CS1 maint: multiple names: authors list (link) - ^ Cappendijk SLT, Dzoljic MR (1993). "Inhibitory effects of ibogaine on cocaine self-administration in rats". European Journal of Pharmacology. 241 (2–3): 261–265. doi:10.1016/0014-2999(93)90212-Z. PMID 8243561.
- ^ Rezvani A, Overstreet D, Lee Y (1995). "Attenuation of alcohol intake by ibogaine in three strains of alcohol preferring rats". Pharmacology, Biochemistry, and Behaviour. 52 (3): 615–20. doi:10.1016/0091-3057(95)00152-M. PMID 8545483.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ A Contemporary History of Ibogaine in the United States and Europe
- ^ a)Taylor WI (1965): "The Iboga and Voacanga Alkaloids" (Journal?), Pages 203, 207 and 208. Oxidation products: peroxides; indolenine, iboquine and iboluteine. pdf
- ^ a b Kontrimaviciūte V, Mathieu O, Mathieu-Daudé JC; et al. (2006). "Distribution of ibogaine and noribogaine in a man following a poisoning involving root bark of the Tabernanthe iboga shrub". J Anal Toxicol. 30 (7): 434–40. PMID 16959135.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Alper KR, Lotsof HS, Frenken GM, Luciano DJ, Bastiaans J (1999). "Treatment of acute opioid withdrawal with ibogaine" (PDF). Am J Addict. 8 (3): 234–42. doi:10.1080/105504999305848. PMID 10506904.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Mash DC, Kovera CA, Pablo J; et al. (2000). "Ibogaine: complex pharmacokinetics, concerns for safety, and preliminary efficacy measures" (PDF). Ann. N. Y. Acad. Sci. 914: 394–401. PMID 11085338.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Jenks CW (2002)
- ^ Shulgin & Shulgin (1997), TiHKAL, p. 487.
- ^ Pace CJ, Glick SD, Maisonneuve IM; et al. (2004). "Novel iboga alkaloid congeners block nicotinic receptors and reduce drug self-administration". Eur. J. Pharmacol. 492 (2–3): 159–67. doi:10.1016/j.ejphar.2004.03.062. PMID 15178360.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Glick SD, Kuehne ME, Raucci J; et al. (1994). "Effects of iboga alkaloids on morphine and cocaine self-administration in rats: relationship to tremorigenic effects and to effects on dopamine release in nucleus accumbens and striatum". Brain Res. 657 (1–2): 14–22. doi:10.1016/0006-8993(94)90948-2. PMID 7820611.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Tsing Hua. Antiaddictive indole alkaloids in Ervatamia yunnanensis and their bioactivity. Academic Journal of Second Military Medical University. January 28, 2006.
- ^ P. Popik, P. Skolnick (1998). Pharmacology of Ibogaine and Ibogaine-Related Alkaloids. The Alkaloids 52, Chapter 3, 197-231, Academic Press, Editor: G.A. Cordell
- ^ Kenneth R. Alper; Glick, Stanley D. (2001). "Ibogaine: A Review". The alkaloids: chemistry and biology (PDF). Vol. 56. San Diego: Academic. pp. 1–38. ISBN 0-12-469556-6.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ^ Xu Z, Chang LW, Slikker W, Ali SF, Rountree RL, Scallet AC (2000). "A dose-response study of ibogaine-induced neuropathology in the rat cerebellum". Toxicol. Sci. 57 (1): 95–101. doi:10.1093/toxsci/57.1.95. PMID 10966515.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Maciulaitis R, Kontrimaviciute V, Bressolle FM, Briedis V (2008). "Ibogaine, an anti-addictive drug: pharmacology and time to go further in development. A narrative review". Hum Exp Toxicol. 27 (3): 181–94. doi:10.1177/0960327107087802. PMID 18650249.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Baumann MH, Rothman RB, Pablo JP, Mash DC (1 May 2001). "In vivo neurobiological effects of ibogaine and its O-desmethyl metabolite, 12-hydroxyibogamine (noribogaine), in rats". J. Pharmacol. Exp. Ther. 297 (2): 531–9. PMID 11303040.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Hough LB, Bagal AA, Glick SD (2000). "Pharmacokinetic characterization of the indole alkaloid ibogaine in rats". Methods Find Exp Clin Pharmacol. 22 (2): 77–81. doi:10.1358/mf.2000.22.2.796066. PMID 10849889.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Zubaran C, Shoaib M, Stolerman IP, Pablo J, Mash DC (1999). "Noribogaine generalization to the ibogaine stimulus: correlation with noribogaine concentration in rat brain". Neuropsychopharmacology. 21 (1): 119–26. doi:10.1016/S0893-133X(99)00003-2. PMID 10379526.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Johnson, Gail straight.com (January 2, 2003) Ibogaine: A one-way trip to sobriety, pot head says
- ^ Controlled Drugs and Substances Act (1996, c. 19), Canadian Department of Justice website. Accessed 5 November 2009.
- ^ Stiftelsen Iboga´s web site
- ^ The original article was republished as Fear and Loathing on the Campaign Trail '72 (New York: Popular Library, 1973), pp. 150-154
- ^ TV.com, "Law & Order: SVU: Users Episode Recap Season 11 Episode Seven," CBS, 2010, http://www.tv.com/law-and-order-special-victims-unit/users/episode/1304610/recap.html?tag=episode_recap;recap
Further reading
- Daniel Pinchbeck writes of his own experience with ibogaine (among other psychoactives) in Breaking Open the Head.
- Ibogaine: Rite Of Passage is a documentary film about the use of ibogaine in Bwiti tradition and addiction medicine.
