Clomipramine
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Anafranil, Clomicalm, others |
| Other names | Clomipramine; 3-Chloroimipramine; G-34586[1] |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a697002 |
| License data |
|
| Pregnancy category |
|
| Routes of administration | By mouth, intravenous[2] |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | ~50%[4] |
| Protein binding | 96–98%[4] |
| Metabolism | Hepatic (CYP2D6)[4] |
| Metabolites | Desmethylclomipramine[4] |
| Elimination half-life | CMI: 19–37 hours[4] DCMI: 54–77 hours[4] |
| Excretion | Renal (51–60%)[4] Feces (24–32%)[4] |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.005.587 |
| Chemical and physical data | |
| Formula | C19H23ClN2 |
| Molar mass | 314.86 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| (verify) | |
Clomipramine, sold under the brand name Anafranil among others, is a tricyclic antidepressant (TCA).[5] It is used in the treatment of various conditions, most-notably obsessive–compulsive disorder but also many other disorders, including hyperacusis, panic disorder, major depressive disorder, trichotillomania,[6] body dysmorphic disorder[7][8][9] and chronic pain.[5] It has also been notably used to treat premature ejaculation[5] and the cataplexy associated with narcolepsy.[10][11]
It may also address certain fundamental features surrounding narcolepsy besides cataplexy (especially hypnagogic and hypnopompic hallucinations).[12] The evidence behind this, however, is less robust.
As with other antidepressants (notably including selective serotonin reuptake inhibitors), it may paradoxically increase the risk of suicide in those under the age of 25, at least in the first few weeks of treatment.[5]
It is typically taken by mouth, although intravenous preparations are sometimes used.[13][14]
Common side effects include dry mouth, constipation, loss of appetite, sleepiness, weight gain, sexual dysfunction, and trouble urinating.[5] Serious side effects include an increased risk of suicidal behavior in those under the age of 25, seizures, mania, and liver problems.[5] If stopped suddenly, a withdrawal syndrome may occur with headaches, sweating, and dizziness.[5] It is unclear if it is safe for use in pregnancy.[5] Its mechanism of action is not entirely clear but is believed to involve increased levels of serotonin and norepinephrine.[5]
Clomipramine was discovered in 1964 by the Swiss drug manufacturer Ciba-Geigy.[15] It is on the World Health Organization's List of Essential Medicines.[16] It is available as a generic medication.[5]
Medical uses
[edit]Clomipramine has a number of uses in medicine, including in the treatment of:
- Obsessive–compulsive disorder (OCD), which happens to be its only U.S. FDA-labeled indication.[17][18] Other regulatory agencies (such as the TGA of Australia and the MHRA of the UK) have also approved clomipramine for this indication.[19][20][21][22]
- Major depressive disorder (MDD), a popular off-label use in the US. It is approved by the Australian TGA and the United Kingdom MHRA for this indication. In Japan it is also approved for depression.[19][20][21][22][23][24] Some have suggested the possible superior efficacy of clomipramine compared to other antidepressants in the treatment of MDD,[25][26][27][28][29] especially the more severe,[30][31][32] although at the current time the evidence may be insufficient to more fully substantiate this claim.[33]
As-with other tricyclic antidepressants, the antidepressant response specifically may be augmented, including in treatment-resistant cases, with triiodothyronine, at a dosage of 50 mcg.[34][35][36][37] In the case of clomipramine specifically, this may also be the case with obsessive-compulsive disorder.[38]
- Panic disorder with or without agoraphobia.[39][40]
- Body dysmorphic disorder[41]
- Repetitive self-injurious/self-harming behaviours in those with intellectual disability specifically.[42][43]
- The subtype of systemised paranoia characterised by somatic phenomena.[44][45]
- Compulsive nail-biting (onychophagia).[46]
- Cataplexy associated with narcolepsy. This is a TGA and MHRA-labeled indication for clomipramine.[21][22]
- Self-bloodletting[47]
- Premature ejaculation,[48] where it may be more effective than paroxetine[49]
- Depersonalization-derealization disorder[50]
- Chronic pain with or without organic disease, particularly headache of the tension type.[51]
- Developmental stuttering[52][53]
- Sleep paralysis, with or without narcolepsy
- Enuresis (involuntary urinating in sleep) in children. The effect may not be sustained following treatment, and alarm therapy may be more effective in both the short-term and the long-term.[54] Combining a tricyclic (such as clomipramine) with anticholinergic medication may be more effective for treating enuresis than the tricyclic alone.[54]
- Trichotillomania[55][56][57]
- In combination with lithium and tryptophan for severe, particularly treatment-resistant depression.[58] This combination, in a similar vein, has also been used for clomipramine-resistant obsessive-compulsive disorder.[59][60][61] When electro-convulsive therapy is performed alongside this treatment-regime (as may be the case in severe depression and accompanied with thyroxine,[62][63]) however, great care must be taken with lithium.[64][65] The overall risk of seizures may have to be weighted against the refractory severity of the current illness and necessity of the amalgamation of treatment(s).
- Isolated cataplexy unto itself (i.e., in the absence of characteristically associated narcolepsy), admittedly a rare condition[66]
- There is anecdotal and tentative, as-yet-undocumented information suggesting that clomipramine may address certain core features of hyperacusis, and possibly misophonia. In the case of hyperacusis, this appears to be especially the case at doses > 150 mg/d. As-with obsessive-compulsive disorder, a full response to any one dose may not be experienced for up to 12-16 weeks.
Although lithium is most-associated with the treatment of bipolar disorder (where it is known for its general mood-stabilising features and to be especially useful in treating and preventing mania), it may have a certain place in the management of treatment-resistant depression (which is often of higher severity than other depressions which have not been addressed with ECT). In these cases is often prescribed alongside SSRIs (e.g., fluoxetine, paroxetine), venlafaxine and various of the tricyclics (e.g., clomipramine, amitriptyline, nortriptyline, maprotiline), which is why it may feature sometimes in the discussion of depression being managed with clomipramine. Lithium also significantly reduces the long-term risk of suicide in general.[67][68][69] In any case, it is not necessary to have a diagnosis of bipolar affective disorder (manic-depressive illness), or even to be considered to have subtle elements of it (“soft bipolarity”), to benefit from lithium in the context of treatment with clomipramine.
In a meta-analysis of various trials involving fluoxetine (Prozac), fluvoxamine (Faverin/Luvox), and sertraline (Zoloft) to test their relative efficacies in treating OCD, clomipramine was found to be significantly more effective.[70][71] Other studies have borne similar results even when risk of bias is eliminated.[72] A potentially significantly greater inherent side-effect profile, however, makes it a second-line choice in the treatment of OCD. SSRIs are generally better-tolerated but appear to be inferior in terms of actual clinical efficacy.
Contraindications
[edit]Contraindications include:[20]
- Known hypersensitivity to clomipramine, or any of the excipients or cross-sensitivity to tricyclic antidepressants of the dibenzazepine group
- Recent myocardial infarction
- Any degree of heart block or other cardiac arrhythmias
- Mania
- Severe liver disease
- Narrow angle glaucoma
- Untreated urinary retention
- It must not be given in combination or within 3 weeks before or after treatment with a monoamine oxidase inhibitor. (Moclobemide-included; however, clomipramine may be initiated sooner at 48 hours following discontinuation of moclobemide.)
Pregnancy and lactation
[edit]Clomipramine use during pregnancy is associated with congenital heart defects in the newborn.[22][73] It is also associated with reversible withdrawal effects in the newborn.[74] Clomipramine is also distributed in breast milk and hence nursing while taking clomipramine is advised against.[18]
Side effects
[edit]Clomipramine has been associated with the side effects listed below:[17][18][19][20]
Very common (>10% frequency):
- Accommodation defect
- Blurred vision
- Nausea
- Dry mouth (Xerostomia)
- Constipation
- Fatigue
- Dizziness
- Tremor
- Headache
- Myoclonus
- Drowsiness
- Somnolence
- Restlessness
- Micturition disorder
- Sexual dysfunction (erectile dysfunction and loss of libido)
- Hyperhidrosis (profuse sweating)
Common (1–10% frequency):
- Weight loss
- Dystonia
- Cognitive impairment
- Orthostatic hypotension
- Sinus tachycardia
- Clinically irrelevant ECG changes (e.g. T- and ST-wave changes) in patients of normal cardiac status
- Palpitations
- Tinnitus (hearing ringing in one's ears)
- Mydriasis (dilated pupils)
- Vomiting
- Abdominal disorders
- Diarrhoea
- Decreased appetite
- Increased transaminases
- Increased Alkaline phosphatase
- Speech disorders
- Paraesthesia
- Muscle hypertonia
- Dysgeusia
- Memory impairment
- Muscular weakness
- Disturbance in attention
- Confusional state
- Disorientation
- Hallucinations (particularly in elderly patients and patients with Parkinson's disease)
- Anxiety
- Agitation
- Sleep disorders
- Mania
- Hypomania
- Aggression
- Depersonalization
- Insomnia
- Nightmares
- Aggravation of depression
- Delirium
- Galactorrhoea (lactation that is not associated with pregnancy or breastfeeding)
- Orgasms triggered by yawning[75][76][77]
- Hot flush
- Dermatitis allergic (skin rash, urticaria)
- Photosensitivity reaction
- Pruritus (itching)
Uncommon (0.1–1% frequency):
- Convulsions
- Ataxia
- Arrhythmias
- Elevated blood pressure
- Activation of psychotic symptoms
Very rare (<0.01% frequency):
- Pancytopaenia — an abnormally low amount of all the different types of blood cells in the blood (including platelets, white blood cells and red blood cells).
- Leukopenia — a low white blood cell count.
- Agranulocytosis — a more severe form of leukopenia; a dangerously low neutrophil count which leaves one open to life-threatening infections due to the role of the white blood cells in defending the body from invaders.
- Thrombocytopenia — an abnormally low amount of platelets in the blood which are essential to clotting and hence this leads to an increased tendency to bruise and bleed, including, potentially, internally.
- Eosinophilia — an abnormally high number of eosinophils — the cells that fight off parasitic infections — in the blood.
- Syndrome of inappropriate secretion of antidiuretic hormone (SIADH) — a potentially fatal reaction to certain medications that is due to an excessive release of antidiuretic hormone — a hormone that prevents the production of urine by increasing the reabsorption of fluids in the kidney — this results in the development of various electrolyte abnormalities (e.g. hyponatraemia [low blood sodium], hypokalaemia [low blood potassium], hypocalcaemia [low blood calcium]).
- Glaucoma
- Oedema (local or generalised)
- Alopecia (hair loss)
- Hyperpyrexia (a high fever that is above 41.5 °C)
- Hepatitis (liver swelling) with or without jaundice — the yellowing of the eyes, the skin, and mucous membranes due to impaired liver function.
- Abnormal ECG
- Anaphylactic and anaphylactoid reactions including hypotension
- Neuroleptic malignant syndrome (NMS) — a potentially fatal side effect of antidopaminergic agents such as antipsychotics, tricyclic antidepressants and antiemetics (drugs that relieve nausea and vomiting). NMS develops over a period of days or weeks and is characterised by the following symptoms:
- Tremor
- Muscle rigidity
- Mental status change (such as confusion, delirium, mania, hypomania, agitation, coma, etc.)
- Hyperthermia (high body temperature)
- Tachycardia (high heart rate)
- Blood pressure changes
- Diaphoresis (sweating profusely)
- Diarrhoea
- Alveolitis allergic (pneumonitis) with or without eosinophilia
- Purpura
- Conduction disorder (e.g. widening of QRS complex, prolonged QT interval, PR/PQ interval changes, bundle-branch block, torsade de pointes, particularly in patients with hypokalaemia)
Individual side-effects may or may not be amendable to treatment. As noted below, bethanechol may alleviate anti-muscarinic/anti-cholinergic side-effects. It may also treat sexual side-effects common to the likes of clomipramine, SSRIs and phenelzine.[78][79]
Topiramate has been used to off-set the weight-gain induced from various antidepressants and antipsychotics,[80] and more broadly for general weight-loss (likewise with bupropion[80]). This option may be especially attractive in patients either overweight prior to clomipramine treatment or who have gained an undesirable amount of weight on it.[81][82][83][84][85]
Another potential advantage of topiramate in the adjunctive treatment of people taking clomipramine is engendered in its status as an anti-convulsant medication, thereby theoretically increasing the seizure-threshold in patients (which clomipramine decreases to an extent which precludes its dosage ranging above 250 m.g./d. in normal circumstances, likewise with maprotiline and its 225 m.g./d. upper-ceiling). It may, thus, be useful and of increased importance in any case for patients with a familial or personal history of epilepsy or seizures of some other kind to concurrently take a daily dose of an anti-convulsant drug (topiramate, gabapentin, etc.) should they require or opt for treatment with an antidepressant which reduces the seizure-threshold significantly (bupropion, clomipramine, amoxapine, maprotiline, venlafaxine).
In the case of seizures occurring due to overdose of tricyclic antidepressants, intravenous lorazepam may successfully abort them. Phenytoin may or may not prevent them in the first instance but its status as an appropriate acute treatment for these seizures is somewhat controversial.[86][87][88]
Tremor may be relieved with a beta-blocker (e.g., pindolol, propranolol, atenolol). In certain cases of tremor, pindolol may be an especially sensible option for serious consideration, as there is substantial evidence that its utilisation is an effective augmentation-strategy for obsessive-compulsive disorder, an important indication for clomipramine.[89][90][91][92][93]
Withdrawal
[edit]Withdrawal symptoms may occur during gradual or particularly abrupt withdrawal of tricyclic antidepressant drugs. Possible symptoms include: nausea, vomiting, abdominal pain, diarrhea, insomnia, headache, nervousness, anxiety, dizziness and worsening of psychiatric status.[19] Differentiating between the return of the original psychiatric disorder and clomipramine withdrawal symptoms is important.[94] Clomipramine withdrawal can be severe.[95] Withdrawal symptoms can also occur in neonates when clomipramine is used during pregnancy.[74] A major mechanism of withdrawal from tricyclic antidepressants is believed to be due to a rebound effect of excessive cholinergic activity due to neuroadaptations as a result of chronic inhibition of cholinergic receptors by tricyclic antidepressants. Restarting the antidepressant and slow tapering is the treatment of choice for tricyclic antidepressant withdrawal. Some withdrawal symptoms may respond to anticholinergics, such as atropine or benztropine mesylate.[96]
Overdose
[edit]Clomipramine overdose usually presents with the following symptoms:[17][19][20]
- Signs of central nervous system depression such as:
- stupor
- coma
- drowsiness
- restlessness
- ataxia
- Mydriasis
- Convulsions
- Enhanced reflexes
- Muscle rigidity
- Athetoid and choreoathetoid movements
- Serotonin syndrome - a condition with many of the same symptoms as neuroleptic malignant syndrome but has a significantly more rapid onset
- Cardiovascular effects including:
- arrhythmias (including Torsades de pointes)
- tachycardia
- QTc interval prolongation
- conduction disorders
- hypotension
- shock
- heart failure
- cardiac arrest
- Apnoea
- Cyanosis
- Respiratory depression
- Vomiting
- Fever
- Sweating
- Oliguria
- Anuria
There is no specific antidote for overdose and all treatment is purely supportive and symptomatic.[19] Treatment with activated charcoal may be used to limit absorption in cases of oral overdose.[19] Anyone suspected of overdosing on clomipramine should be hospitalised and kept under close surveillance for at least 72 hours.[19] Clomipramine has been reported as being less toxic in overdose than most other TCAs in one meta-analysis but this may well be due to the circumstances surrounding most overdoses as clomipramine is more frequently used to treat conditions for which the rate of suicide is not particularly high such as OCD.[97] In another meta-analysis, however, clomipramine was associated with a significant degree of toxicity in overdose.[98]
Interactions
[edit]Clomipramine may interact with a number of different medications, including the monoamine oxidase inhibitors which include isocarboxazid, moclobemide, phenelzine, selegiline and tranylcypromine, antiarrhythmic agents (due to the effects of TCAs like clomipramine on cardiac conduction. There is also a potential pharmacokinetic interaction with quinidine due to the fact that clomipramine is metabolised by CYP2D6 in vivo), diuretics (due to the potential for hypokalaemia (low blood potassium) to develop which increases the risk for QT interval prolongation and torsades de pointes), the selective serotonin reuptake inhibitors [SSRIs; due to both potential additive serotonergic effects leading to serotonin syndrome and the potential for a pharmacokinetic interaction with the SSRIs that inhibit CYP2D6 (e.g., fluoxetine, paroxetine)] and serotonergic agents such as triptans, other tricyclic antidepressants, tramadol, etc. (due to the potential for serotonin-toxicity | serotonin syndrome).[19] Its use is also advised against in those concurrently on CYP2D6 inhibitors, due to the potential for increased plasma levels of clomipramine and the resulting potential for CNS and cardiotoxicity.[19]
Fluvoxamine increases the serotoninergic effects of clomipramine and, likewise, clomipramine increases fluvoxamine levels.[99]
Pharmacology
[edit]Pharmacodynamics
[edit]| Site | CMI | DMC | Species | Ref |
|---|---|---|---|---|
| SERT | 0.14–0.28 | 40 | Human/rat | [101][102][103] |
| NET | 38–53.7 | 0.32 | Human/rat | [101][102][103] |
| DAT | ≥2,190 | 2,100 | Human/rat | [101][102][103] |
| 5-HT1A | ≥7,000 | 19,000 | Human/und | [104][102][103] |
| 5-HT1B | >10,000 | ND | Human | [102] |
| 5-HT1D | >10,000 | ND | Human | [102] |
| 5-HT2A | 27–35.5 | 130 | Human/und | [104][102][103] |
| 5-HT2B | ND | ND | ND | ND |
| 5-HT2C | 64.6 | ND | Human | [102] |
| 5-HT3 | 460–985 | ND | Rodent | [102][105][106] |
| 5-HT6 | 53.8 | ND | Rat | [107] |
| 5-HT7 | 127 | ND | Rat | [108] |
| α1 | 3.2–38 | 190 | Human/und | [102][109][103] |
| α2 | 525–3,200 | 1,800 | Human/und | [102][109][103] |
| β | 22,000 | 16,000 | Undefined | [103] |
| D1 | 219 | 320 | Human/und | [105][103] |
| D2 | 77.6–190 | 1,200 | Human/und | [102][109][103] |
| D3 | 30–50.1 | ND | Human | [102][105] |
| D4 | ND | ND | ND | ND |
| D5 | ND | ND | ND | ND |
| H1 | 13–31 | 450 | Human/und | [110][109][103] |
| H2 | 209 | ND | Human | [110] |
| H3 | 9,770 | ND | Human | [110] |
| H4 | 5,750 | ND | Human | [110] |
| mACh | 37 | 92 | Human/und | [109][103] |
| σ1 | 546 | ND | Rat | [111] |
| hERG | 130 (IC50) | ND | Human | [112] |
| Values are Ki (nM), unless otherwise noted. The smaller the value, the more strongly the drug binds to the site. | ||||
Clomipramine is a reuptake inhibitor of serotonin and norepinephrine, or a serotonin–norepinephrine reuptake inhibitor (SNRI); that is, it blocks the reuptake of these neurotransmitters back into neurons by preventing them from interacting with their transporters, thereby increasing their extracellular concentrations in the synaptic cleft and resulting in increased serotonergic and noradrenergic neurotransmission.[113][101] In addition, clomipramine also has antiadrenergic, antihistamine, antiserotonergic, antidopaminergic, and anticholinergic activities. It is specifically an antagonist of the α1-adrenergic receptor, the histamine H1 receptor, the serotonin 5-HT2A, 5-HT2C, 5-HT3, 5-HT6, and 5-HT7 receptors, the dopamine D1, D2, and D3 receptors, and the muscarinic acetylcholine receptors (M1–M5).[109][102] Like other TCAs, clomipramine weakly blocks voltage-dependent sodium channels as well.[113][15][114]
Probably all “anticholinergic” side-effects may be successfully reversed in a majority of people with bethanechol chloride,[115][116][117] although knowledge of this amenability has unfortunately decreased in medical circles over the decades. It (bethanechol supplementation) arguably should, however, be seriously entertained when tricyclics which often carry significant anti-muscarinic effects (amitriptyline, protriptyline, imipramine, clomipramine) are prescribed, as it may alleviate potentially otherwise-limiting side-effects (blurry vision, dry mouth, urinary hesitancy/retention, etc.). This practice can make drugs of otherwise indispensably potent value more tolerable to certain patients and spare them needless suffering, hence-reducing the overall side-effect burden or concern thereof.
Although clomipramine shows around 100- to 200-fold preference in affinity for the serotonin transporter (SERT) over the norepinephrine transporter (NET), its major active metabolite, desmethylclomipramine (norclomipramine), binds to the NET with very high affinity (Ki = 0.32 nM) and with dramatically reduced affinity for the SERT (Ki = 31.6 nM).[118][119] Moreover, desmethylclomipramine circulates at concentrations that are approximately twice those of clomipramine.[120] In accordance, occupancy of both the SERT and the NET has been shown with clomipramine administration in positron emission tomography studies with humans and non-human primates.[121][122] As such, clomipramine is in fact a fairly balanced SNRI rather than only a serotonin reuptake inhibitor (SRI).[123]
The antidepressant effects of clomipramine are thought to be due to reuptake inhibition of serotonin and norepinephrine,[113] while serotonin reuptake inhibition only is thought to be responsible for the effectiveness of clomipramine in the treatment of OCD. Conversely, antagonism of the H1, α1-adrenergic, and muscarinic acetylcholine receptors is thought to contribute to its side effects.[113] Blockade of the H1 receptor is specifically responsible for the antihistamine effects of clomipramine and side effects like sedation and somnolence (sleepiness).[113] Antagonism of the α1-adrenergic receptor is thought to cause orthostatic hypotension and dizziness.[113] Inhibition of muscarinic acetylcholine receptors is responsible for the anticholinergic side effects of clomipramine like dry mouth, constipation, urinary retention, blurred vision, and cognitive/memory impairment.[113] In overdose, sodium channel blockade in the brain is believed to cause the coma and seizures associated with TCAs while blockade of sodium channels in the heart is considered to cause cardiac arrhythmias, cardiac arrest, and death.[113][15] On the other hand, sodium channel blockade is also thought to contribute to the analgesic effects of TCAs, for instance in the treatment of neuropathic pain.[124]
The exceptionally strong serotonin reuptake inhibition of clomipramine likely precludes the possibility of its antagonism of serotonin receptors (which it binds to with more than 100-fold lower affinity than the SERT) resulting in a net decrease in signaling by these receptors. In accordance, while serotonin receptor antagonists like cyproheptadine and chlorpromazine are effective as antidotes against serotonin syndrome,[125][126] clomipramine is nonetheless capable of inducing this syndrome.[123] In fact, while all TCAs are SRIs and serotonin receptor antagonists to varying extents, the only TCAs that are associated with serotonin syndrome are clomipramine and to a lesser extent its dechlorinated analogue imipramine,[123][125] which are the two most potent SRIs of the TCAs (and in relation to this have the highest ratios of serotonin reuptake inhibition to serotonin receptor antagonism).[127] As such, whereas other TCAs can be combined with monoamine oxidase inhibitors (with caution due to the risk of hypertensive crisis from NET inhibition; sometimes done in treatment-resistant depressives), clomipramine cannot be due to the risk of serotonin syndrome and death.[113] Unlike the case of its serotonin receptor antagonism, orthostatic hypotension is a common side effect of clomipramine, suggesting that its blockade of the α1-adrenergic receptor is strong enough to overcome the stimulatory effects on the α1-adrenergic receptor of its NET inhibition.[15][113]
Serotonergic activity
[edit]| Medication | SERT | NET | Dosage (mg/day) |
t1/2 (M) (hours) |
Cp (ng/mL) |
Cp / SERT ratio |
|---|---|---|---|---|---|---|
| Amitriptyline | 4.3 | 34.5 | 100–200 | 16 (30) | 100–250 | 23–58 |
| Amoxapine | 58.5 | 16.1 | 200–300 | 8 (30) | 200–500 | 3.4–8.5 |
| Butriptyline[101] | 1,360 | 5,100 | ? | ? | ? | ? |
| Clomipramine | 0.14–0.28 | 37 | 100–200 | 32 (70) | 150–500 | 536–3,570 |
| Desipramine | 17.5 | 0.8 | 100–200 | 30 | 125–300 | 7.1–17 |
| Dosulepin[128][129][130] | 8.3 | 45.5 | 150–225 | 25 (34) | 50–200 | 6.0–24 |
| Doxepin | 66.7 | 29.4 | 100–200 | 18 (30) | 150–250 | 2.2–3.7 |
| Imipramine | 1.4 | 37 | 100–200 | 12 (30) | 175–300 | 125–214 |
| Iprindole[101] | 1,620 | 1,262 | ? | ? | ? | ? |
| Lofepramine[101] | 70.0 | 5.4 | ? | ? | ? | ? |
| Nortriptyline | 18.5 | 4.4 | 75–150 | 31 | 60–150 | 3.2–8.1 |
| Protriptyline | 19.6 | 1.4 | 15–40 | 80 | 100–250 | 5.1–13 |
| Trimipramine[101] | 149 | 2,450 | 75–200 | 16 (30) | 100–300 | 0.67–2.0 |
| Citalopram | 1.4 | 5,100 | 20–40 | 36 | 75–150 | 54–107 |
| Escitalopram | 1.1 | 7,840 | 10–20 | 30 | 40–80 | 36–73 |
| Fluoxetine | 0.8 | 244 | 20–40 | 53 (240) | 100–500 | 125–625 |
| Fluvoxamine | 2.2 | 1,300 | 100–200 | 18 | 100–200 | 45–91 |
| Paroxetine | 0.34 | 40 | 20–40 | 17 | 30–100 | 300–1,000 |
| Sertraline | 0.4 | 417 | 100–150 | 23 (66) | 25–50 | 83–167 |
| Duloxetine | 1.6 | 11.2 | 80–100 | 11 | ? | ? |
| Milnacipran | 123 | 200 | ? | ? | ? | ? |
| Venlafaxine | 9.1 | 535 | 75–225 | 5 (11) | ? | ? |
| The values for the SERT and NET are Ki (nM). Note that in the Cp / SERT ratio, free versus protein-bound drug concentrations are not accounted for. | ||||||
| Medication | Dosage range (mg/day)[131] |
~80% SERT occupancy (mg/day)[132][133] |
Ratio (dosage / 80% occupancy) |
|---|---|---|---|
| Citalopram | 20–40 | 40 | 0.5–1 |
| Escitalopram | 10–20 | 10 | 1–2 |
| Fluoxetine | 20–80 | 20 | 1–4 |
| Fluvoxamine | 50–300 | 70 | 0.71–5 |
| Paroxetine | 10–60 | 20 | 0.5–3 |
| Sertraline | 25–200 | 50 | 0.5–4 |
| Duloxetine | 20–60 | 30 | 0.67–2 |
| Venlafaxine | 75–375 | 75 | 1–5 |
| Clomipramine | 50–250 | 10 | 5–25 |
Clomipramine is an extremely strong SRI by all accounts.[134][135] Its affinity for the SERT was reported in one study using human tissues to be 0.14 nM, which is considerably higher than that of other TCAs.[102][127] For example, the TCAs with the next highest affinities for the SERT in the study were imipramine, amitriptyline, and dosulepin (dothiepin), with Ki values of 1.4 nM, 4.3 nM, and 8.3 nM, respectively.[127] In addition, clomipramine has a terminal half-life that is around twice as long as that of amitriptyline and imipramine.[127][136] In spite of these differences however, clomipramine is used clinically at the same usual dosages as other serotonergic TCAs (100–200 mg/day).[127]Some health authorities recommend daily dosage is in the range of 30 to 75 mg in single or divided doses. Initial dosage should be 10 mg/day with gradual increments to 30-150 mg/day in divided doses or as a single dose at bedtime. Health Canada recommends maximum dose for outpatients is preferred at 200 mg/day.[137] Sustained-release 75 mg formulation may be preferable at doses above 150mg/day (i.e. 200mg to 250mg/day).[138][139] It achieves typical circulating concentrations that are similar in range to those of other TCAs but with an upper limit that is around twice that of amitriptyline and imipramine.[127] For these reasons, clomipramine is the most potent SRI among the TCAs and is far stronger as an SRI than other TCAs at typical clinical dosages.[134][135] In addition, clomipramine is more potent as an SRI than any selective serotonin reuptake inhibitors (SSRIs); it is more potent than paroxetine, which is the strongest SSRI.[127]
A positron emission tomography study found that a single low dose of 10 mg clomipramine to healthy volunteers resulted in 81.1% occupancy of the SERT, which was comparable to the 84.9% SERT occupancy by 50 mg fluvoxamine.[121] In the study, single doses of 5 to 50 mg clomipramine resulted in 67.2 to 94.0% SERT occupancy while single doses of 12.5 to 50 mg fluvoxamine resulted in 28.4 to 84.9% SERT occupancy.[121] Chronic treatment with higher doses was able to achieve up to 100.0% SERT occupancy with clomipramine and up to 93.6% SERT occupancy with fluvoxamine.[121] Other studies have found 83% SERT occupancy with 20 mg/day paroxetine and 77% SERT occupancy with 20 mg/day citalopram.[121][140] These results indicate that very low doses of clomipramine are able to substantially occupy the SERT and that clomipramine achieves higher occupancy of the SERT than SSRIs at comparable doses.[121][132] Moreover, clomipramine may be able to achieve more complete occupancy of the SERT at high doses, at least relative to fluvoxamine.[121]
If the ratios of the 80% SERT occupancy dosage and the approved clinical dosage range are calculated and compared for SSRIs, SNRIs, and clomipramine, it can be deduced that clomipramine is by far the strongest SRI used medically.[132][131] The lowest approved dosage of clomipramine can be estimated to be roughly comparable in SERT occupancy to the maximum approved dosages of the strongest SSRIs and SNRIs.[132][131] Because their mechanism of action was originally not known and dose-ranging studies were never conducted, first-generation antipsychotics were dramatically overdosed in patients.[132] It has been suggested that the same may have been true for clomipramine and other TCAs.[132] Nonetheless, there is little doubt that many may, indeed, benefit from much higher doses. 250 mg/d, as mentioned elsewhere, is the typical maximum recommended dose but some people may need as much as 300 mg/d or more to benefit from all clomipramine has to offer beyond its potent SNRI capacity alone.[141]
Obsessive–compulsive disorder
[edit]Clomipramine was the first drug that was investigated for and found to be effective in the treatment of OCD.[15][142] In addition, it was the first drug to be approved by the FDA in the United States for the treatment of OCD.[143] The effectiveness of clomipramine in the treatment of OCD is far greater than that of other TCAs, which are comparatively weak SRIs; a meta-analysis found pre- versus post-treatment effect sizes of 1.55 for clomipramine relative to a range of 0.67 for imipramine and 0.11 for desipramine.[144] In contrast to other TCAs, studies have found that clomipramine and SSRIs, which are more selective SRIs, have similar effectiveness in the treatment of OCD.[144] However, multiple meta-analyses have found that clomipramine nonetheless retains a significant effectiveness advantage relative to SSRIs;[145] in the same meta-analysis mentioned previously, the effect sizes of SSRIs in the treatment of OCD ranged from 0.81 for fluoxetine to 1.36 for sertraline (relative to 1.55 for clomipramine).[144] However, the effectiveness advantage for clomipramine has not been apparent in head-to-head comparisons of clomipramine versus SSRIs for OCD.[145] The differences in effectiveness findings could be due to differences in methodologies across non-head-to-head studies.[144][145]
Relatively high doses of SSRIs are needed for effectiveness in the treatment of OCD.[146] Studies have found that high dosages of SSRIs above the normally recommended maximums are significantly more effective in OCD treatment than lower dosages (e.g., 250 to 400 mg/day sertraline versus 200 mg/day sertraline).[146][147] In addition, the combination of clomipramine and SSRIs has also been found to be significantly more effective in alleviating OCD symptoms, and clomipramine is commonly used to augment SSRIs for this reason.[146][143] Studies have found that intravenous clomipramine, which is associated with very high circulating concentrations of the drug and a much higher ratio of clomipramine to its metabolite desmethylclomipramine, is more effective than oral clomipramine in the treatment of OCD.[146][15][143] There is a case report of complete remission from OCD for approximately one month following a massive overdose of fluoxetine, an SSRI with a uniquely long duration of action.[148] Taken together, stronger serotonin reuptake inhibition has consistently been associated with greater alleviation of OCD symptoms, and since clomipramine, at the clinical dosages in which it is employed, is effectively the strongest SRI used medically (see table above), this may underlie its unique effectiveness in the treatment of OCD.
In addition to serotonin reuptake inhibition, clomipramine is also a mild but clinically significant antagonist of the dopamine D1, D2, and D3 receptors at high concentrations.[127][145][149] Addition of antipsychotics, which are potent dopamine receptor antagonists, to SSRIs, has been found to significantly augment their effectiveness in the treatment of OCD.[145][150] As such, besides strong serotonin reuptake inhibition, clomipramine at high doses might also block dopamine receptors to treat OCD symptoms, and this could additionally or alternatively be involved in its possible effectiveness advantage over SSRIs.[151][152] For this reason, it may also be that augmentation with neuroleptics (a common procedure in the occurrence of inadequate response to monotherapy with an SRI) is needed with less frequency with clomipramine relative to SSRIs, the latter of-which apparently lack significant activity as dopamine-receptor antagonists.
Although clomipramine is probably more effective in the treatment of OCD compared to SSRIs, it is greatly inferior to them in terms of tolerability and safety due to its lack of selectivity for the SERT and promiscuous pharmacological activity.[145][153] In addition, clomipramine has high toxicity in overdose and can potentially result in death, whereas death rarely, if ever, occurs with overdose of SSRIs.[145][153] It is for these reasons that clomipramine, in spite of potentially superior effectiveness to SSRIs, is now rarely used as a first-line agent in the treatment of OCD, with SSRIs being used as first-line therapies instead and clomipramine generally being reserved for more severe cases and as a second-line agent.[153]
Pharmacokinetics
[edit]The oral bioavailability of clomipramine is approximately 50%.[17] Peak plasma concentrations occur around 2–6 hours (with an average of 4.7 hours) after taking clomipramine orally and are in the range of 56–154 ng/mL (178–489 nmol/L).[17] Steady-state concentrations of clomipramine are around 134–532 ng/mL (426–1,690 nmol/L), with an average of 218 ng/mL (692 nmol/L), and are reached after 7 to 14 days of repeated dosing.[17] Steady-state concentrations of the active metabolite, desmethylclomipramine, are around 230–550 ng/mL (730–1,750 nmol/L).[17] The volume of distribution (Vd) of clomipramine is approximately 17 L/kg.[18] It binds approximately 97–98% to plasma proteins,[17][18] primarily to albumin.[17] Clomipramine is metabolized in the liver mainly by CYP2D6.[18] It has a terminal half-life of 32 hours,[154][155] and its N-desmethyl metabolite, desmethylclomipramine, has a terminal half-life of approximately 69 hours.[18] Clomipramine is mostly excreted in urine (60%) and feces (32%).[18]
Although the normal maximum-recommended total daily dosage of clomipramine is 250 milligrams, treatment-resistant cases of depression[156] and obsessive-compulsive disorder may require corresponding doses within the range of 255 to 300 milligrams. Indeed, doses of 375 milligrams per day, sometimes in combination with venlafaxine[157] or aripiprazole, have not only been necessary but, remarkably, relatively well-tolerated. Caution, however, is generally prudent when doing this, as seizures, which are more likely to occur with clomipramine than every other tricyclic antidepressant besides maprotiline, become more and more of a risk beyond the normally-recommended upper-ceiling. At daily doses ≤ 250 m.g., the incidence of seizures may be reliably estimated to be around the order of 0.48%.[158] (All tricyclic antidepressants technically lower the seizure-threshold but this is only significant with amoxapine, maprotiline and, indeed, clomipramine.[159])
Dose-increases between 25 m.g. and 150 m.g., barring significant drug-drug interactions which may elevate clomipramine blood-levels, should be titrated in doses of 50 m.g. (25 m.g. in the case of panic disorder and 10 to 25 m.g. in the cases of premature ejaculation[160][161]and narcoleptic cataplexy) and above 150 m.g. in 25 m.g. increments. Average optimal total daily doses for depression (whether mild or severe), premature ejaculation, cataplexy-narcolepsy, obsessive-compulsive disorder, panic disorder and trichotilomania respectively are (in milligrams) 150, 50, 25 - 75, 150 - 250, 50 - 150 and 150 - 200. Some consider the minimum optimally-therapeutic dose of clomipramine in obsessive-compulsive disorder, which often requires much higher levels of serotoninergic concentration than other indications for these drugs, to be 200, rather than 150, milligrams per day. For premature ejaculation, clomipramine can be taken prn 3 to 5 hours before attempted sexual intercourse.
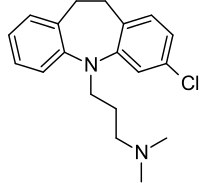
Chemistry
[edit]Clomipramine is a tricyclic compound, specifically a dibenzazepine, and possesses three rings fused together with a side chain attached in its chemical structure.[162] Other dibenzazepine TCAs include imipramine, desipramine, and trimipramine.[162] Clomipramine is a derivative of imipramine with a chlorine atom added to one of its rings and is also known as 3-chloroimipramine.[163] It is a tertiary amine TCA, with its side chain-demethylated metabolite desmethylclomipramine being a secondary amine.[164][165] Other tertiary amine TCAs include amitriptyline, imipramine, dosulepin (dothiepin), doxepin, and trimipramine.[166][167] The chemical name of clomipramine is 3-(3-chloro-10,11-dihydro-5H-dibenzo[b,f]azepin-5-yl)-N,N-dimethylpropan-1-amine and its free base form has a chemical formula of C19H23ClN2 with a molecular weight of 314.857 g/mol.[1] The drug is used commercially almost exclusively as the hydrochloride salt; the free base has been used rarely.[1][168] The CAS Registry Number of the free base is 303-49-1 and of the hydrochloride is 17321–77–6.[1][168]
History
[edit]Clomipramine was developed by Geigy as a chlorinated derivative of imipramine.[15][169] It was first referenced in the literature in 1961 and was patented in 1963.[169] The drug was first approved for medical use in Europe in the treatment of depression in 1970,[169] and was the last of the major TCAs to be marketed.[4] In fact, clomipramine was initially considered to be a "me-too drug" by the FDA, and in relation to this, was declined licensing for depression in the United States.[4] As such, to this day, clomipramine remains the only TCA that is available in the United States that is not approved for the treatment of depression, in spite of the fact that it is a highly effective antidepressant.[170]
Clomipramine was eventually approved in the United States for the treatment of OCD in 1989 and became available in 1990.[143][15] It was the first drug to be investigated and found effective in the treatment of OCD.[15][142] The benefits in OCD were first reported by Juan José López-Ibor in 1967,[171][172] and the first double-blind, placebo-controlled clinical trial of clomipramine for OCD was conducted in 1976,[142] with more rigorous clinical studies that solidified its effectiveness conducted in the 1980s.[15] It remained the "gold standard" for the treatment of OCD for many years until the introduction of the SSRIs, which have since largely superseded it due to greatly improved tolerability and safety (although notably not effectiveness).[173][174] Clomipramine is the only TCA that has been shown to be effective in the treatment of OCD and that is approved by the FDA for the treatment of OCD; the other TCAs failed clinical trials for this indication, likely due to insufficient serotonergic activity.[175][176]
Society and culture
[edit]Generic names
[edit]Clomipramine is the English and French generic name of the drug and its INN, BAN, and DCF, while clomipramine hydrochloride is its USAN, USP, BANM, and JAN.[1][168][177][178] Clomipramina is its generic name in Spanish, Portuguese and Italian and its DCIT, while clomipramin is its generic name in German and clomipraminum is its generic name in Latin.[168][178]
Brand names
[edit]Clomipramine is marketed throughout the world mainly under the brand names Anafranil and Clomicalm for use in humans and animals, respectively.[168][178]
Veterinary uses
[edit]In the U.S., clomipramine is only licensed to treat separation anxiety in dogs for which it is sold under the brand name Clomicalm.[179] It has proven effective in the treatment of obsessive–compulsive disorders in cats and dogs.[180][181] In dogs, it has also demonstrated similar efficacy to fluoxetine in treating tail chasing.[182] In dogs some evidence suggests its efficacy in treating noise phobia.[183]
Clomipramine has also demonstrated efficacy in treating urine spraying in cats.[184] Various studies have been done on the effects of clomipramine on cats to reduce urine spraying/marking behavior. It has been shown to be able to reduce this behavior by up to 75% in a trial period of four weeks.[185]
References
[edit]- ^ a b c d e Elks J (14 November 2014). The Dictionary of Drugs: Chemical Data: Chemical Data, Structures and Bibliographies. Springer. pp. 299–. ISBN 978-1-4757-2085-3. Archived from the original on 15 February 2017.
- ^ Taylor D, Paton C, Shitij K (2012). Maudsley Prescribing Guidelines in Psychiatry (11th ed.). West Sussex: Wiley-Blackwell. ISBN 978-0-470-97948-8.
- ^ Anvisa (31 March 2023). "RDC Nº 784 - Listas de Substâncias Entorpecentes, Psicotrópicas, Precursoras e Outras sob Controle Especial" [Collegiate Board Resolution No. 784 - Lists of Narcotic, Psychotropic, Precursor, and Other Substances under Special Control] (in Brazilian Portuguese). Diário Oficial da União (published 4 April 2023). Archived from the original on 3 August 2023. Retrieved 16 August 2023.
- ^ a b c d e f g h i j Lemke TL, Williams DA (24 January 2012). Foye's Principles of Medicinal Chemistry. Lippincott Williams & Wilkins. pp. 604–605. ISBN 978-1-60913-345-0. Archived from the original on 8 September 2017.
- ^ a b c d e f g h i j "Clomipramine Hydrochloride". The American Society of Health-System Pharmacists. Archived from the original on 8 December 2015. Retrieved 2 December 2015.
- ^ Swedo, S E et al. “A double-blind comparison of clomipramine and desipramine in the treatment of trichotillomania (hair pulling).” The New England journal of medicine vol. 321,8 (1989): 497-501. doi:10.1056/NEJM198908243210803
- ^ Adebayo, Kazeem Olaide et al. “Body dysmorphic disorder in a Nigerian boy presenting as depression: a case report and literature review.” International journal of psychiatry in medicine vol. 44,4 (2012): 367-72. doi:10.2190/PM.44.4.f
- ^ Phillips, K.A., Albertini, R.S., Siniscalchi, J.M., Khan, A. and Robinson, M., 2001. Effectiveness of pharmacotherapy for body dysmorphic disorder: a chart-review study. Journal of Clinical Psychiatry, 62(9), pp.721-727.
- ^ Pallanti, S. and Koran, L.M., 1996. Intravenous, pulse-loaded clomipramine in body dysmorphic disorder: two case reports. CNS Spectrums, 1(2), pp.54-57.
- ^ Shapiro, W. R. (1975). Treatment of cataplexy with clomipramine. Archives of neurology, 32(10), 653-656.
- ^ Dauvilliers Y, Siegel JM, Lopez R, Torontali ZA, Peever JH. Cataplexy—clinical aspects, pathophysiology and management strategy. Nature Reviews Neurology. 2014 Jul;10(7):386-95..
- ^ Chen C. N. (1980). The use of clomipramine as an REM sleep suppressant in narcolepsy. Postgraduate medical journal, 56 Suppl 1, 86–89.
- ^ Karameh, Wael Karameh, and Munir Khani. “Intravenous Clomipramine for Treatment-Resistant Obsessive-Compulsive Disorder.” The international journal of neuropsychopharmacology vol. 19,2 pyv084. 28 July 2015, doi:10.1093/ijnp/pyv084
- ^ Sallee, F R et al. “Pulse intravenous clomipramine for depressed adolescents: double-blind, controlled trial.” The American journal of psychiatry vol. 154,5 (1997): 668-73. doi:10.1176/ajp.154.5.668
- ^ a b c d e f g h i j Zohar J (31 May 2012). Obsessive Compulsive Disorder: Current Science and Clinical Practice. John Wiley & Sons. pp. 19–30, 32, 50, 59. ISBN 978-1-118-30801-1.
- ^ World Health Organization (2019). World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- ^ a b c d e f g h i "ANAFRANIL (CLOMIPRAMINE HYDROCHLORIDE) CAPSULE [MALLINCKRODT, INC.]". DailyMed. Mallinckrodt, Inc. October 2012. Archived from the original on 3 December 2013. Retrieved 30 November 2013.
- ^ a b c d e f g h "Anafranil (clomipramine) dosing, indications, interactions, adverse effects, and more". Medscape Reference. WebMD. Archived from the original on 3 December 2013. Retrieved 30 November 2013.
- ^ a b c d e f g h i j "ANAFRANIL (clomipramine)" (PDF). TGA eBusiness Services. NOVARTIS Pharmaceuticals Australia Pty Limited. 7 December 2012. Archived from the original on 12 August 2017. Retrieved 30 November 2013.
- ^ a b c d e "Anafranil 75mg SR Tablets - Summary of Product Characteristics (SPC) - (eMC)". electronic Medicines Compendium. Novartis Pharmaceuticals UK Ltd. 8 October 2012. Archived from the original on 14 July 2014. Retrieved 2 July 2014.
- ^ a b c Joint Formulary Committee (2013). British National Formulary (BNF) (65 ed.). London, UK: Pharmaceutical Press. ISBN 978-0-85711-084-8.
- ^ a b c d Rossi S, ed. (2013). Australian Medicines Handbook (2013 ed.). Adelaide: The Australian Medicines Handbook Unit Trust. ISBN 978-0-9805790-9-3.
- ^ "Clomipramine 50 mg Capsules, Hard - Summary of Product Characteristics (SmPC) - (eMC)". www.medicines.org.uk. Retrieved 27 January 2019.
- ^ "Kusuri-no-Shiori(Drug Information Sheet)". www.rad-ar.or.jp. Retrieved 28 September 2023.
- ^ Danish University Antidepressant Group. (1990). Paroxetine: a selective serotonin reuptake inhibitor showing better tolerance, but weaker antidepressant effect than clomipramine in a controlled multicenter study. Journal of Affective Disorders, 18(4), 289-299.
- ^ "Citalopram: clinical effect profile in comparison with clomipramine. A controlled multicenter study. Danish University Antidepressant Group". Psychopharmacology. 90 (1): 131–8. 1986. doi:10.1007/BF00172884. PMID 2876451. S2CID 837142.
- ^ Gillman, Ken, and Last updated Mar. "Clomipramine: Potent SNRI Anti-Depressant."
- ^ Vestergaard, P., Gram, L. F., Kragh-Sørensen, P., Bech, P., Reisby, N., & Bolwig, T. G. (1993). Therapeutic potentials of recently introduced antidepressants. Danish University Antidepressant Group. Psychopharmacology series, 10, 190–198. https://doi.org/10.1007/978-3-642-78010-3_18
- ^ Montgomery SA, Baldwin DS, Blier P, Fineberg NA, Kasper S, Lader M, Lam RW, Lépine JP, Möller HJ, Nutt DJ, Rouillon F. Which antidepressants have demonstrated superior efficacy? A review of the evidence. International clinical psychopharmacology. 2007 Nov 1;22(6):323-9.
- ^ Wijkstra J, Lijmer J, Balk FJ, Geddes JR, Nolen WA. Pharmacological treatment for unipolar psychotic depression: systematic review and meta-analysis. The British Journal of Psychiatry. 2006 May;188(5):410-5.
- ^ Bayes, A. and Parker, G., 2019. How to choose an antidepressant medication. Acta Psychiatrica Scandinavica, 139(3), pp.280-291.
- ^ Anderson, I.M., 2000. Selective serotonin reuptake inhibitors versus tricyclic antidepressants: a meta-analysis of efficacy and tolerability. Journal of affective disorders, 58(1), pp.19-36.
- ^ Montgomery SA, Baldwin DS, Blier P, Fineberg NA, Kasper S, Lader M, et al. (November 2007). "Which antidepressants have demonstrated superior efficacy? A review of the evidence". International Clinical Psychopharmacology. 22 (6): 323–329. doi:10.1097/YIC.0b013e3282eff7e0. PMID 17917550. S2CID 16921407.
- ^ Souche A, Baumann P, Koeb L, Thermoz P, Azorin JM, Dufour H. Traitement de la dépression par l'association de la clomipramine et de la triiodothyronine (LT3) [Treatment of depression by a combination of clomipramine and triiodothyronine]. Encephale. 1991 Jan-Feb;17(1):37-42. French. PMID 1669033.
- ^ Pigott TA, Pato MT, L'Heureux F, Hill JL, Grover GN, Bernstein SE, Murphy DL. A controlled comparison of adjuvant lithium carbonate or thyroid hormone in clomipramine-treated patients with obsessive-compulsive disorder. J Clin Psychopharmacol. 1991 Aug;11(4):242-8. PMID 1918422.
- ^ Martin P, Massol J, Soubrie P, Puech AJ. Effects of triiodothyronine (T3) on the potentiation by antidepressants of L-5-hydroxytryptophan-induced head-twitches in mice. Prog Neuropsychopharmacol Biol Psychiatry. 1989;13(5):735-48. doi: 10.1016/0278-5846(89)90061-4. PMID 2789414.
- ^ Gervasoni N, Aubry JM, Gex-Fabry M, Bertschy G, Bondolfi G. Is there a place for tricyclic antidepressants and subsequent augmentation strategies in obtaining remission for patients with treatment resistant depression? Pharmacol Res. 2009 Mar;59(3):202-6. doi: 10.1016/j.phrs.2008.11.005. Epub 2008 Nov 27. PMID 19073260.
- ^ McCracken JT, Hanna GL. Elevated thyroid indices in children and adolescents with obsessive-compulsive disorder: effects of clomipramine treatment. J Child Adolesc Psychopharmacol. 2005 Aug;15(4):581-7. doi: 10.1089/cap.2005.15.581. PMID 16190790.
- ^ Saeed SA, Bruce TJ (May 1998). "Panic disorder: effective treatment options". American Family Physician. 57 (10): 2405–12, 2419–20. PMID 9614411. Archived from the original on 3 December 2013.
- ^ Papp LA, Schneier FR, Fyer AJ, Leibowitz MR, Gorman JM, Coplan JD, et al. (October 1997). "Clomipramine treatment of panic disorder: pros and cons". The Journal of Clinical Psychiatry. 58 (10): 423–425. doi:10.4088/JCP.v58n1002. PMID 9375591.
- ^ Hollander E, Allen A, Kwon J, Aronowitz B, Schmeidler J, Wong C, et al. (November 1999). "Clomipramine vs desipramine crossover trial in body dysmorphic disorder: selective efficacy of a serotonin reuptake inhibitor in imagined ugliness" (PDF). Archives of General Psychiatry. 56 (11): 1033–1039. doi:10.1001/archpsyc.56.11.1033. PMID 10565503. Archived (PDF) from the original on 3 December 2013.
- ^ Garber HJ, McGonigle JJ, Slomka GT, Monteverde E (November 1992). "Clomipramine treatment of stereotypic behaviors and self-injury in patients with developmental disabilities". Journal of the American Academy of Child and Adolescent Psychiatry. 31 (6): 1157–1160. doi:10.1097/00004583-199211000-00027. PMID 1429420.
- ^ Lewis MH, Bodfish JW, Powell SB, Parker DE, Golden RN (May 1996). "Clomipramine treatment for self-injurious behavior of individuals with mental retardation: a double-blind comparison with placebo". American Journal of Mental Retardation. 100 (6): 654–665. PMID 8735578.
- ^ Wada T, Kawakatsu S, Nadaoka T, Okuyama N, Otani K (May 1999). "Clomipramine treatment of delusional disorder, somatic type". International Clinical Psychopharmacology. 14 (3): 181–183. doi:10.1097/00004850-199905030-00006. PMID 10435772.
- ^ Wada T, Kawakatsu S, Komatani A, Okuyama N, Otani K (February 1999). "Possible association between delusional disorder, somatic type and reduced regional cerebral blood flow". Progress in Neuro-Psychopharmacology & Biological Psychiatry. 23 (2): 353–357. doi:10.1016/s0278-5846(98)00098-0. PMID 10368875. S2CID 22832400.
- ^ Leonard HL, Lenane MC, Swedo SE, Rettew DC, Rapoport JL (September 1991). "A double-blind comparison of clomipramine and desipramine treatment of severe onychophagia (nail biting)". Archives of General Psychiatry. 48 (9): 821–827. doi:10.1001/archpsyc.1991.01810330045007. PMID 1929772.
- ^ Mestermann S, Rudtke L, Brazdis RM, Tsaktanis T, Kornhuber J, Thürauf N. Successful Pharmacologic Treatment of Self-Bloodletting with Factitious Chronic Anemia (Lasthénie de Ferjol Syndrome) with High-Dose Serotonergic Medication: A Case Report. Behav Sci (Basel). 2024 Mar 14;14(3):237. doi: 10.3390/bs14030237. PMID 38540540.
- ^ Palmer NR, Stuckey BG (June 2008). "Premature ejaculation: a clinical update" (PDF). The Medical Journal of Australia. 188 (11): 662–666. doi:10.5694/j.1326-5377.2008.tb01827.x. PMID 18513177. S2CID 12157287. Archived (PDF) from the original on 3 December 2013.
- ^ Waldinger, M. D., Zwinderman, A. H., & Olivier, B. (2004). On-demand treatment of premature ejaculation with clomipramine and paroxetine: a randomized, double-blind fixed-dose study with stopwatch assessment. European urology, 46(4), 510–516. https://doi.org/10.1016/j.eururo.2004.05.005
- ^ Hollander E, Hwang MY, Mullen LS, DeCaria C, Stein DJ, Cohen L (1993). "Clinical and research issues in depersonalization syndrome". Psychosomatics. 34 (2): 193–194. doi:10.1016/s0033-3182(93)71919-2. PMID 8456168.
- ^ Nilsson HL, Knorring LV (1989). "Review. Clomipramine in acute and chronic pain syndromes". Nordic Journal of Psychiatry. 43 (s20): 101–113. doi:10.3109/08039488909100841.
- ^ Gordon CT, Cotelingam GM, Stager S, Ludlow CL, Hamburger SD, Rapoport JL (June 1995). "A double-blind comparison of clomipramine and desipramine in the treatment of developmental stuttering". The Journal of Clinical Psychiatry. 56 (6): 238–242. PMID 7775365.
- ^ Brady JP, Ali Z (April 2000). "Alprazolam, citalopram, and clomipramine for stuttering". Journal of Clinical Psychopharmacology. 20 (2): 287. doi:10.1097/00004714-200004000-00037. PMID 10770483.
- ^ a b Caldwell PH, Sureshkumar P, Wong WC (January 2016). "Tricyclic and related drugs for nocturnal enuresis in children". The Cochrane Database of Systematic Reviews. 2016 (1): CD002117. doi:10.1002/14651858.CD002117.pub2. PMC 8741207. PMID 26789925.
- ^ "Trichotillomania Medication". Medscape Reference. WebMD. 10 October 2013. Archived from the original on 3 December 2013. Retrieved 1 December 2013.
- ^ Franklin ME, Zagrabbe K, Benavides KL (August 2011). "Trichotillomania and its treatment: a review and recommendations". Expert Review of Neurotherapeutics. 11 (8): 1165–1174. doi:10.1586/ern.11.93. PMC 3190970. PMID 21797657.
- ^ Hoffman J, Williams T, Rothbart R, Ipser JC, Fineberg N, Chamberlain SR, et al. (September 2021). "Pharmacotherapy for trichotillomania". The Cochrane Database of Systematic Reviews. 2021 (9): CD007662. doi:10.1002/14651858.CD007662.pub3. PMC 8478440. PMID 34582562.
- ^ Hale AS, Procter AW, Bridges PK (August 1987). "Clomipramine, tryptophan and lithium in combination for resistant endogenous depression: seven case studies". The British Journal of Psychiatry. 151 (2): 213–217. doi:10.1192/bjp.151.2.213. PMID 3690111. S2CID 34432532.
- ^ Rasmussen SA (October 1984). "Lithium and tryptophan augmentation in clomipramine-resistant obsessive-compulsive disorder". The American Journal of Psychiatry. 141 (10): 1283–1285. doi:10.1176/ajp.141.10.1283. PMID 6435460.
- ^ Goodman WK, McDougle CJ, Barr LC, Aronson SC, Price LH (June 1993). "Biological approaches to treatment-resistant obsessive compulsive disorder". The Journal of Clinical Psychiatry. 54 (Suppl): 16–26. PMID 8331098.
- ^ Murphy DL, Zohar J, Benkelfat C, Pato MT, Pigott TA, Insel TR (December 1989). "Obsessive-compulsive disorder as a 5-HT subsystem-related behavioural disorder". The British Journal of Psychiatry. Supplement. 155 (8): 15–24. doi:10.1192/S0007125000291721. PMID 2692636. S2CID 44813426.
- ^ Bauer M, Hellweg R, Gräf KJ, Baumgartner A (June 1998). "Treatment of refractory depression with high-dose thyroxine". Neuropsychopharmacology. 18 (6): 444–455. doi:10.1016/S0893-133X(97)00181-4. PMID 9571653. S2CID 25452860.
- ^ Chiu LP, Rimon R (September 1987). "Response to clomipramine after short course of lithium in treatment-resistant depression: Does lithium have a 'priming'effect?". Human Psychopharmacology: Clinical and Experimental. 2 (3): 191–193. doi:10.1002/hup.470020309. S2CID 146533651.
- ^ Rucker J, Cook M (December 2008). "A case of prolonged seizure after ECT in a patient treated with clomipramine, lithium, L-tryptophan, quetiapine, and thyroxine for major depression". The Journal of ECT. 24 (4): 272–274. doi:10.1097/YCT.0b013e31815bd768. PMID 18648320.
- ^ Wieben E, Kjeldsen MJ, Sørensen CH (2022). "Convulsive Status Epilepticus Induced by Electroconvulsive Therapy in a Patient with Major Depression". Case Reports in Psychiatry. 2022: 8545991. doi:10.1155/2022/8545991. PMC 8947920. PMID 35342656.
- ^ Mandagere, V. and Rayment, D., 2024. Atypical isolated cataplexy: two case reports and a mini-review. Neurocase, pp.1-3.
- ^ Sarai SK, Mekala HM, Lippmann S (November 2018). "Lithium Suicide Prevention: A Brief Review and Reminder". Innovations in Clinical Neuroscience. 15 (11–12): 30–32. PMC 6380616. PMID 30834169.
- ^ Guzzetta F, Tondo L, Centorrino F, Baldessarini RJ (March 2007). "Lithium treatment reduces suicide risk in recurrent major depressive disorder". The Journal of Clinical Psychiatry. 68 (3): 380–383. doi:10.4088/jcp.v68n0304. PMID 17388706.
- ^ Ohgami H, Terao T, Shiotsuki I, Ishii N, Iwata N (May 2009). "Lithium levels in drinking water and risk of suicide". The British Journal of Psychiatry. 194 (5): 464–5, discussion 446. doi:10.1192/bjp.bp.108.055798. PMID 19407280. S2CID 18029965.
- ^ Greist JH, Jefferson JW, Kobak KA, Katzelnick DJ, Serlin RC (January 1995). "Efficacy and tolerability of serotonin transport inhibitors in obsessive-compulsive disorder. A meta-analysis". Archives of General Psychiatry. 52 (1): 53–60. doi:10.1001/archpsyc.1995.03950130053006. PMID 7811162.
- ^ Wilson, M., & Tripp, J. (2022). Clomipramine. In StatPearls. StatPearls Publishing.
- ^ Cohen SE, Zantvoord JB (2024). "Influence of study characteristics, methodological rigour and publication bias on efficacy of pharmacotherapy in obsessive-compulsive disorder: A systematic review and meta-analysis of randomised, placebo-controlled trials". BMJ Mental Health. 27 (1): e300951. doi:10.1136/bmjment-2023-300951. PMC 10862307. PMID 38350669.
- ^ Källén B, Otterblad Olausson P (April 2006). "Antidepressant drugs during pregnancy and infant congenital heart defect". Reproductive Toxicology. 21 (3): 221–222. Bibcode:2006RepTx..21..221K. doi:10.1016/j.reprotox.2005.11.006. PMID 16406480.
- ^ a b Bloem BR, Lammers GJ, Roofthooft DW, De Beaufort AJ, Brouwer OF (July 1999). "Clomipramine withdrawal in newborns". Archives of Disease in Childhood. Fetal and Neonatal Edition. 81 (1): F77. doi:10.1136/fn.81.1.f77a. PMC 1720967. PMID 10744432.
- ^ Mikkelson B (19 August 1999). "Yin, Yang And Yawn". Snopes. Retrieved 16 July 2024.
- ^ "Sep 04, 1995, page 1 - The Daily Telegraph at Newspapers.com". Newspapers.com. Retrieved 16 July 2024.
- ^ "NEW BRITISH ANTI-DEPRESSANT DRUG HAS SIDE EFFECT: ORGASM WITH YAWN". Chicago Tribune. 5 September 1995. Retrieved 16 July 2024.
- ^ Shen WW, Sata LS (January 1990). "Inhibited female orgasm resulting from psychotropic drugs. A five-year, updated, clinical review". The Journal of Reproductive Medicine. 35 (1): 11–14. PMID 2405155.
- ^ Bernik M, Vieira AH, Nunes PV (December 2004). "Bethanecol chloride for treatment of clomipramine-induced orgasmic dysfunction in males". Revista do Hospital das Clinicas. 59 (6): 357–360. doi:10.1590/s0041-87812004000600008. PMID 15654489.
- ^ a b Ness-Abramof R, Apovian CM (August 2005). "Drug-induced weight gain". Drugs of Today. 41 (8): 547–555. doi:10.1358/dot.2005.41.8.893630. PMID 16234878. S2CID 34960274.
- ^ Lundt L, Brownsmith C (May 2005). "Why me? One youth's quest for sanity" (PDF). Current Psychiatry. 4 (5): 85–99.
- ^ Cosentino G, Conrad AO, Uwaifo GI (2013). "Phentermine and topiramate for the management of obesity: a review". Drug Design, Development and Therapy. 7: 267–278. doi:10.2147/DDDT.S31443. PMC 3623549. PMID 23630412.
- ^ Berman C, Naguib M, Hegedus E, Vidmar AP (June 2023). "Topiramate for Weight Management in Children With Severe Obesity". Childhood Obesity. 19 (4): 219–225. doi:10.1089/chi.2022.0062. PMC 10398729. PMID 35767803.
- ^ Khazaal Y, Zullino DF (March 2007). "Rebound of weight gain following topiramate cessation". Pharmacopsychiatry. 40 (2): 85–86. doi:10.1055/s-2007-970139. PMID 17447182. S2CID 260239945.
- ^ Italiano D, Spina E, de Leon J (November 2014). "Pharmacokinetic and pharmacodynamic interactions between antiepileptics and antidepressants". Expert Opinion on Drug Metabolism & Toxicology. 10 (11): 1457–1489. doi:10.1517/17425255.2014.956081. PMID 25196459. S2CID 1925913.
- ^ Sarko J (November 2000). "Antidepressants, old and new. A review of their adverse effects and toxicity in overdose". Emergency Medicine Clinics of North America. 18 (4): 637–654. doi:10.1016/s0733-8627(05)70151-6. PMID 11130931.
- ^ Franson KL, Hay DP, Neppe V, Dahdal WY, Mirza WU, Grossberg GT, et al. (July 1995). "Drug-induced seizures in the elderly. Causative agents and optimal management". Drugs & Aging. 7 (1): 38–48. doi:10.2165/00002512-199507010-00005. PMID 7579780. S2CID 54136953.
- ^ Body R, Bartram T, Azam F, Mackway-Jones K (April 2011). "Guidelines in Emergency Medicine Network (GEMNet): guideline for the management of tricyclic antidepressant overdose". Emergency Medicine Journal. 28 (4): 347–368. doi:10.1136/emj.2010.091553. PMID 21436332. S2CID 46037419.
- ^ Dannon PN, Sasson Y, Hirschmann S, Iancu I, Grunhaus LJ, Zohar J (May 2000). "Pindolol augmentation in treatment-resistant obsessive compulsive disorder: a double-blind placebo controlled trial". European Neuropsychopharmacology. 10 (3): 165–169. doi:10.1016/s0924-977x(00)00065-1. PMID 10793318. S2CID 28452756.
- ^ Blier P, Bergeron R (March 1996). "Sequential administration of augmentation strategies in treatment-resistant obsessive-compulsive disorder: preliminary findings". International Clinical Psychopharmacology. 11 (1): 37–44. doi:10.1097/00004850-199603000-00005. PMID 8732312. S2CID 12336027.
- ^ Sassano-Higgins SA, Pato MT (2015). "Pindolol augmentation of selective serotonin reuptake inhibitors and clomipramine for the treatment of obsessive-compulsive disorder: A meta-analysis". Journal of Pharmacology & Pharmacotherapeutics. 6 (1): 36–38. doi:10.4103/0976-500X.149144. PMC 4319248. PMID 25709352.
- ^ Mundo E, Guglielmo E, Bellodi L (September 1998). "Effect of adjuvant pindolol on the antiobsessional response to fluvoxamine: a double-blind, placebo-controlled study". International Clinical Psychopharmacology. 13 (5): 219–224. doi:10.1097/00004850-199809000-00005. PMID 9817627. S2CID 23946424.
- ^ Koran LM, Mueller K, Maloney A (June 1996). "Will pindolol augment the response to a serotonin reuptake inhibitor in obsessive-compulsive disorder?". Journal of Clinical Psychopharmacology. 16 (3): 253–254. doi:10.1097/00004714-199606000-00011. PMID 8784659.
- ^ Zemishlany Z, Aizenberg D, Hermesh H, Weizman A (October 1992). "[Withdrawal reactions after clomipramine]". Harefuah. 123 (7–8): 252–5, 307. PMID 1459499.
- ^ Kraft TB (August 1977). "[Severe withdrawal symptoms following use of clomipramine]". Nederlands Tijdschrift voor Geneeskunde. 121 (33): 1293. PMID 895917.
- ^ Wolfe RM (August 1997). "Antidepressant withdrawal reactions". American Family Physician. 56 (2): 455–462. PMID 9262526.
- ^ White N, Litovitz T, Clancy C (December 2008). "Suicidal antidepressant overdoses: a comparative analysis by antidepressant type". Journal of Medical Toxicology. 4 (4): 238–250. doi:10.1007/BF03161207. PMC 3550116. PMID 19031375.
- ^ Hawton K, Bergen H, Simkin S, Cooper J, Waters K, Gunnell D, et al. (May 2010). "Toxicity of antidepressants: rates of suicide relative to prescribing and non-fatal overdose". The British Journal of Psychiatry. 196 (5): 354–358. doi:10.1192/bjp.bp.109.070219. PMC 2862059. PMID 20435959.
- ^ Fung R, Elbe D, Stewart SE (August 2021). "Retrospective Review of Fluvoxamine-Clomipramine Combination Therapy in Obsessive-Compulsive Disorder in Children and Adolescents". Journal of the Canadian Academy of Child and Adolescent Psychiatry. 30 (3): 150–155. PMC 8315223. PMID 34381507.
- ^ Roth BL, Driscol J. "PDSP Ki Database". Psychoactive Drug Screening Program (PDSP). University of North Carolina at Chapel Hill and the United States National Institute of Mental Health. Archived from the original on 8 September 2017. Retrieved 14 August 2017.
- ^ a b c d e f g h Tatsumi M, Groshan K, Blakely RD, Richelson E (December 1997). "Pharmacological profile of antidepressants and related compounds at human monoamine transporters". European Journal of Pharmacology. 340 (2–3): 249–258. doi:10.1016/S0014-2999(97)01393-9. PMID 9537821.
- ^ a b c d e f g h i j k l m n o Millan MJ, Gobert A, Lejeune F, Newman-Tancredi A, Rivet JM, Auclair A, et al. (August 2001). "S33005, a novel ligand at both serotonin and norepinephrine transporters: I. Receptor binding, electrophysiological, and neurochemical profile in comparison with venlafaxine, reboxetine, citalopram, and clomipramine". The Journal of Pharmacology and Experimental Therapeutics. 298 (2): 565–580. PMID 11454918.
- ^ a b c d e f g h i j k l Hyttel J (March 1994). "Pharmacological characterization of selective serotonin reuptake inhibitors (SSRIs)". International Clinical Psychopharmacology. 9 (Suppl 1): 19–26. doi:10.1097/00004850-199403001-00004. PMID 8021435. S2CID 30166780.
- ^ a b Wander TJ, Nelson A, Okazaki H, Richelson E (December 1986). "Antagonism by antidepressants of serotonin S1 and S2 receptors of normal human brain in vitro". European Journal of Pharmacology. 132 (2–3): 115–121. doi:10.1016/0014-2999(86)90596-0. PMID 3816971.
- ^ a b c Toll L, Berzetei-Gurske IP, Polgar WE, Brandt SR, Adapa ID, Rodriguez L, et al. (March 1998). "Standard binding and functional assays related to medications development division testing for potential cocaine and opiate narcotic treatment medications". NIDA Research Monograph. 178: 440–466. PMID 9686407.
- ^ Schmidt AW, Hurt SD, Peroutka SJ (November 1989). "'[3H]quipazine' degradation products label 5-HT uptake sites". European Journal of Pharmacology. 171 (1): 141–143. doi:10.1016/0014-2999(89)90439-1. PMID 2533080.
- ^ Monsma FJ, Shen Y, Ward RP, Hamblin MW, Sibley DR (March 1993). "Cloning and expression of a novel serotonin receptor with high affinity for tricyclic psychotropic drugs". Molecular Pharmacology. 43 (3): 320–327. PMID 7680751.
- ^ Ruat M, Traiffort E, Leurs R, Tardivel-Lacombe J, Diaz J, Arrang JM, et al. (September 1993). "Molecular cloning, characterization, and localization of a high-affinity serotonin receptor (5-HT7) activating cAMP formation". Proceedings of the National Academy of Sciences of the United States of America. 90 (18): 8547–8551. Bibcode:1993PNAS...90.8547R. doi:10.1073/pnas.90.18.8547. PMC 47394. PMID 8397408.
- ^ a b c d e f Richelson E, Nelson A (July 1984). "Antagonism by antidepressants of neurotransmitter receptors of normal human brain in vitro". The Journal of Pharmacology and Experimental Therapeutics. 230 (1): 94–102. PMID 6086881.
- ^ a b c d Appl H, Holzammer T, Dove S, Haen E, Strasser A, Seifert R (February 2012). "Interactions of recombinant human histamine H₁R, H₂R, H₃R, and H₄R receptors with 34 antidepressants and antipsychotics". Naunyn-Schmiedeberg's Archives of Pharmacology. 385 (2): 145–170. doi:10.1007/s00210-011-0704-0. PMID 22033803. S2CID 14274150.
- ^ Shirayama Y, Nishikawa T, Umino A, Takahashi K (June 1993). "p-chlorophenylalanine-reversible reduction of sigma binding sites by chronic imipramine treatment in rat brain". European Journal of Pharmacology. 237 (1): 117–126. doi:10.1016/0014-2999(93)90100-v. PMID 8359206.
- ^ Jo SH, Hong HK, Chong SH, Won KH, Jung SJ, Choe H (September 2008). "Clomipramine block of the hERG K+ channel: accessibility to F656 and Y652". European Journal of Pharmacology. 592 (1–3): 19–25. doi:10.1016/j.ejphar.2008.06.094. PMID 18634780.
- ^ a b c d e f g h i j Stahl SM (28 October 2013). Mood Disorders and Antidepressants: Stahl's Essential Psychopharmacology. Cambridge University Press. pp. 103–104, 106–108. ISBN 978-1-107-72992-6.
- ^ Ressler K, Pine D, Rothbaum B (15 April 2015). Anxiety Disorders. Oxford University Press. pp. 254–. ISBN 978-0-19-939514-9. Archived from the original on 8 September 2017.
- ^ Boyson S. J. (1988). Bethanechol for anticholinergic side effects. Annals of neurology, 23(4), 422–423. https://doi.org/10.1002/ana.410230429
- ^ Hermesh H, Aizenberg D, Weizman A, Lapidot M, Munitz H (November 1987). "Clomipramine-induced urinary dysfunction in an obsessive-compulsive adolescent". Drug Intelligence & Clinical Pharmacy. 21 (11): 877–879. doi:10.1177/106002808702101105. PMID 3678059. S2CID 42755526.
- ^ Rosen J, Pollock BG, Altieri LP, Jonas EA (August 1993). "Treatment of nortriptyline's side effects in elderly patients: a double-blind study of bethanechol". The American Journal of Psychiatry. 150 (8): 1249–1251. doi:10.1176/ajp.150.8.1249. PMID 8101048.
- ^ Baldessarini RJ (2 October 2012). Chemotherapy in Psychiatry: Pharmacologic Basis of Treatments for Major Mental Illness. Springer Science & Business Media. pp. 173–. ISBN 978-1-4614-3710-9. Archived from the original on 8 September 2017.
- ^ Progress in Drug Research. Birkhäuser. 6 December 2012. pp. 80–. ISBN 978-3-0348-8391-7. Archived from the original on 8 September 2017.
- ^ Hedges DE, Burchfield C (2006). Mind, Brain, and Drug: An Introduction to Psychopharmacology. Pearson/Allyn and Bacon. p. 205. ISBN 978-0-205-35556-3.
[...] desmethylclomipramine levels may be twice as high as those of clomipramine (Rudorfer & Potter, 1999).
- ^ a b c d e f g Suhara T, Takano A, Sudo Y, Ichimiya T, Inoue M, Yasuno F, et al. (April 2003). "High levels of serotonin transporter occupancy with low-dose clomipramine in comparative occupancy study with fluvoxamine using positron emission tomography". Archives of General Psychiatry. 60 (4): 386–391. doi:10.1001/archpsyc.60.4.386. PMID 12695316. S2CID 12259485.
- ^ Takano A, Nag S, Gulyás B, Halldin C, Farde L (July 2011). "NET occupancy by clomipramine and its active metabolite, desmethylclomipramine, in non-human primates in vivo". Psychopharmacology. 216 (2): 279–286. doi:10.1007/s00213-011-2212-9. PMID 21336575. S2CID 14928733.
- ^ a b c Gillman PK (July 2007). "Tricyclic antidepressant pharmacology and therapeutic drug interactions updated". British Journal of Pharmacology. 151 (6): 737–748. doi:10.1038/sj.bjp.0707253. PMC 2014120. PMID 17471183.
- ^ Wilson P, Watson P, Haythornwaite J, Jensen (26 September 2008). Clinical Pain Management Second Edition: Chronic Pain. CRC Press. pp. 345–. ISBN 978-0-340-94008-2. Archived from the original on 8 September 2017.
- ^ a b Wang RZ, Vashistha V, Kaur S, Houchens NW (November 2016). "Serotonin syndrome: Preventing, recognizing, and treating it". Cleveland Clinic Journal of Medicine. 83 (11): 810–817. doi:10.3949/ccjm.83a.15129. PMID 27824534.
- ^ Alusik S, Kalatova D, Paluch Z (2014). "Serotonin syndrome". Neuro Endocrinology Letters. 35 (4): 265–273. PMID 25038602.
- ^ a b c d e f g h i Brunton L, Chabner BA, Knollman B (14 January 2011). Goodman and Gilman's The Pharmacological Basis of Therapeutics, Twelfth Edition. McGraw Hill Professional. p. 400,406,409. ISBN 978-0-07-176939-6.
- ^ Doran CM (20 March 2013). Prescribing Mental Health Medication: The Practitioner's Guide. Routledge. pp. 506–. ISBN 978-1-136-28009-2.
- ^ Dart RC (2004). Medical Toxicology. Lippincott Williams & Wilkins. pp. 835–. ISBN 978-0-7817-2845-4.
- ^ Tiziani AP (24 May 2017). Havard's Nursing Guide to Drugs - Mobile optimised site. Elsevier Health Sciences. pp. 1464–. ISBN 978-0-7295-8605-4.
- ^ a b c Koocher GP, Norcross JC, Greene BA (4 September 2013). Psychologists' Desk Reference. Oxford University Press. pp. 442–. ISBN 978-0-19-984550-7.
- ^ a b c d e f Gründer G, Hiemke C, Paulzen M, Veselinovic T, Vernaleken I (September 2011). "Therapeutic plasma concentrations of antidepressants and antipsychotics: lessons from PET imaging". Pharmacopsychiatry. 44 (6): 236–248. doi:10.1055/s-0031-1286282. PMID 21959785. S2CID 30691618.
- ^ Kasper S, Sacher J, Klein N, Mossaheb N, Attarbaschi-Steiner T, Lanzenberger R, et al. (May 2009). "Differences in the dynamics of serotonin reuptake transporter occupancy may explain superior clinical efficacy of escitalopram versus citalopram". International Clinical Psychopharmacology. 24 (3): 119–125. doi:10.1097/YIC.0b013e32832a8ec8. PMID 19367152. S2CID 17470375.
- ^ a b Brown SL, Praag HM (1991). The Role of Serotonin in Psychiatric Disorders. Psychology Press. pp. 174–. ISBN 978-0-87630-589-8.
- ^ a b Stein DJ, Stone MH (1 February 1997). Essential Papers on Obsessive-Compulsive Disorder. NYU Press. pp. 453–. ISBN 978-0-8147-8661-1.
- ^ Li JJ (2015). Top Drugs: History, Pharmacology, Syntheses. Oxford University Press. pp. 121–. ISBN 978-0-19-936258-5.
- ^ "PrANAFRANIL® Clomipramine Hydrochloride Tablets" (PDF). Health Canada drug database.
- ^ "Anafranil SR 75 mg Prolonged-release Tablets; Summary of Product Characteristics" (PDF). Health Products Regulatory Authority of Ireland. 20 December 2021. CRN00CP8H.
- ^ "Clomipramine Capsules, Hard; Package leaflet: Information for the patient" (PDF). Electronic Medicines Compendium (EMC). July 2017.
- ^ Meyer JH, Wilson AA, Ginovart N, Goulding V, Hussey D, Hood K, et al. (November 2001). "Occupancy of serotonin transporters by paroxetine and citalopram during treatment of depression: a [(11)C]DASB PET imaging study". The American Journal of Psychiatry. 158 (11): 1843–1849. doi:10.1176/appi.ajp.158.11.1843. PMID 11691690.
- ^ Ananth, J., 1986. Clomipramine: an antiobsessive drug. The Canadian Journal of Psychiatry, 31(3), pp.253-258.
- ^ a b c Yaryura-Tobias JA, Neziroglu FA (1997). Obsessive-compulsive Disorder Spectrum: Pathogenesis, Diagnosis, and Treatment. American Psychiatric Pub. pp. 36–. ISBN 978-0-88048-707-8.
- ^ a b c d Hudak R, Dougherty DD (17 February 2011). Clinical Obsessive-Compulsive Disorders in Adults and Children. Cambridge University Press. pp. 31–. ISBN 978-1-139-49626-1.
- ^ a b c d Eddy KT, Dutra L, Bradley R, Westen D (December 2004). "A multidimensional meta-analysis of psychotherapy and pharmacotherapy for obsessive-compulsive disorder". Clinical Psychology Review. 24 (8): 1011–1030. doi:10.1016/j.cpr.2004.08.004. PMID 15533282. S2CID 6582600.
- ^ a b c d e f g Hollander E, Kaplan A, Allen A, Cartwright C (September 2000). "Pharmacotherapy for obsessive-compulsive disorder". The Psychiatric Clinics of North America. 23 (3): 643–656. doi:10.1016/s0193-953x(05)70186-6. PMID 10986733.
- ^ a b c d Kellner M (2010). "Drug treatment of obsessive-compulsive disorder". Dialogues in Clinical Neuroscience. 12 (2): 187–197. doi:10.31887/DCNS.2010.12.2/mkellner. PMC 3181958. PMID 20623923.
- ^ Byerly MJ, Goodman WK, Christensen R (September 1996). "High doses of sertraline for treatment-resistant obsessive-compulsive disorder". The American Journal of Psychiatry. 153 (9): 1232–1233. doi:10.1176/ajp.153.9.1232b. PMID 8780435.
- ^ Leonard HL, Topol D, Bukstein O, Hindmarsh D, Allen AJ, Swedo SE (1994). "Clonazepam as an augmenting agent in the treatment of childhood-onset obsessive-compulsive disorder". Journal of the American Academy of Child and Adolescent Psychiatry. 33 (6): 792–794. doi:10.1097/00004583-199407000-00003. PMID 8083135.
- ^ Austin LS, Lydiard RB, Ballenger JC, Cohen BM, Laraia MT, Zealberg JJ, et al. (August 1991). "Dopamine blocking activity of clomipramine in patients with obsessive-compulsive disorder". Biological Psychiatry. 30 (3): 225–232. doi:10.1016/0006-3223(91)90107-w. PMID 1832972. S2CID 7172333.
- ^ Dold M, Aigner M, Lanzenberger R, Kasper S (April 2013). "Antipsychotic augmentation of serotonin reuptake inhibitors in treatment-resistant obsessive-compulsive disorder: a meta-analysis of double-blind, randomized, placebo-controlled trials". The International Journal of Neuropsychopharmacology. 16 (3): 557–574. doi:10.1017/S1461145712000740. PMID 22932229.
- ^ Fontenelle LF, Nascimento AL, Mendlowicz MV, Shavitt RG, Versiani M (April 2007). "An update on the pharmacological treatment of obsessive-compulsive disorder". Expert Opinion on Pharmacotherapy. 8 (5): 563–583. doi:10.1517/14656566.8.5.563. PMID 17376013. S2CID 40042242.
- ^ Hood S, Alderton D, Castle D (2016). "Obsessive–Compulsive Disorder: Treatment and Treatment Resistance". Australasian Psychiatry. 9 (2): 118–127. doi:10.1046/j.1440-1665.2001.00316.x. ISSN 1039-8562. S2CID 73291517.
- ^ a b c Abramowitz JS, McKay D, Storch EA (12 June 2017). The Wiley Handbook of Obsessive Compulsive Disorders. Wiley. pp. 1076–. ISBN 978-1-118-89025-7.
- ^ Peters MD, Davis SK, Austin LS (March 1990). "Clomipramine: an antiobsessional tricyclic antidepressant". Clinical Pharmacy. 9 (3): 165–178. PMID 2180623.
- ^ Balant-Gorgia AE, Gex-Fabry M, Balant LP (June 1991). "Clinical pharmacokinetics of clomipramine". Clinical Pharmacokinetics. 20 (6): 447–462. doi:10.2165/00003088-199120060-00002. PMID 2044329. S2CID 6818721.
- ^ Amsterdam, J.D., García‐España, F. and Rosenzweig, M., 1997. Clomipramine augmentation in treatment‐resistant depression. Depression and Anxiety, 5(2), pp.84-90.
- ^ Gomez, J.M. and Perramon, C.T., 2000. Combined treatment with venlafaxine and tricyclic antidepressants in depressed patients who had partial response to clomipramine or imipramine: initial findings. J Clin Psychiatry, 61(4), pp.285-289.
- ^ DeVeaugh-Geiss, J., Landau, P. and Katz, R., 1989. Treatment of obsessive compulsive disorder with clomipramine. Psychiatric Annals, 19(2), pp.97-99.
- ^ Górska, N., Słupski, J., Cubała, W.J., Wiglusz, M.S. and Gałuszko-Węgielnik, M., 2018. Antidepressants in epilepsy. neurologia i neurochirurgia polska, 52(6), pp.657-661.
- ^ Rowland, D.L., De Gouveia Brazao, C.A. and Koos Slob, A., 2001. During the initial titration, it may be necessary to divide the total daily dose up to thrice (to reduce certain side-effects) but once the full optimal dose has been reached, most people can be sustained on a once-at-bedtime dose, or on a prn basis 3 to 5 hours before sexual intercourse in the case of premature ejaculation. Effective daily treatment with clomipramine in men with premature ejaculation when 25 mg (as required) is ineffective. BJU international, 87(4), pp.357-360.
- ^ Mohammed, M.A., CLOMIPRAMINE AS DAILY DOSE IN THE TREATMENT OF PATIENTS WITH PREMATURE.
- ^ a b Ritsner MS (15 February 2013). Polypharmacy in Psychiatry Practice, Volume I: Multiple Medication Use Strategies. Springer Science & Business Media. pp. 270–271. ISBN 978-94-007-5805-6. Archived from the original on 8 September 2017.
- ^ Psychopharmacology Bulletin. National Institute of Mental Health. 1984.
Clomipramine or 3-chloro-imipramine (Figure 4) is imipramine with a chlorine atom added to one of its rings.
- ^ Cutler NR, Sramek JJ, Narang PK (20 September 1994). Pharmacodynamics and Drug Development: Perspectives in Clinical Pharmacology. John Wiley & Sons. pp. 160–. ISBN 978-0-471-95052-3.
- ^ Anzenbacher P, Zanger UM (23 February 2012). Metabolism of Drugs and Other Xenobiotics. John Wiley & Sons. pp. 302–. ISBN 978-3-527-64632-6. Archived from the original on 8 September 2017.
- ^ Anthony PK (2002). Pharmacology Secrets. Elsevier Health Sciences. pp. 39–. ISBN 978-1-56053-470-9.
- ^ Cowen P, Harrison P, Burns T (9 August 2012). Shorter Oxford Textbook of Psychiatry. OUP Oxford. pp. 532–. ISBN 978-0-19-162675-3. Archived from the original on 8 September 2017.
- ^ a b c d e Index Nominum 2000: International Drug Directory. Taylor & Francis. 2000. pp. 259–. ISBN 978-3-88763-075-1.
- ^ a b c Andersen J, Kristensen AS, Bang-Andersen B, Strømgaard K (July 2009). "Recent advances in the understanding of the interaction of antidepressant drugs with serotonin and norepinephrine transporters". Chemical Communications (25): 3677–3692. doi:10.1039/b903035m. PMID 19557250.
- ^ Bonder B (2010). Psychopathology and Function. SLACK. pp. 239–. ISBN 978-1-55642-922-4.
- ^ Osborn I (1999). Tormenting Thoughts and Secret Rituals: The Hidden Epidemic of Obsessive-Compulsive Disorder. New York: Dell Publishing. ISBN 978-0-440-50847-2.
- ^ "The history of obsessive-compulsive disorder". ocdhistory.net. Retrieved 4 November 2023.
- ^ Swanson RW (1996). Family Practice Review: A Problem Oriented Approach. Mosby. p. 313. ISBN 978-0-8151-8624-3.
Until very recently, the "gold standard" of pharmacologic therapy for obsessive-compulsive disorder has been clomipramine. At this time, however, the SSRIs (selective serotonin reuptake inhibitors) have become the drugs of choice.
- ^ Schlaepfer TE, Nemeroff CB (2012). Neurobiology of Psychiatric Disorders. Elsevier. pp. 677–. ISBN 978-0-444-52002-9.
- ^ Antony MM, Stein MB (2009). Oxford Handbook of Anxiety and Related Disorders. Oxford University Press, USA. pp. 376–. ISBN 978-0-19-530703-0.
- ^ McGinn LK, Sanderson WC (1 June 1999). Treatment of Obsessive Compulsive Disorder. Jason Aronson, Incorporated. pp. 61–. ISBN 978-1-4616-3230-6.
- ^ Morton IK, Hall JM (6 December 2012). Concise Dictionary of Pharmacological Agents: Properties and Synonyms. Springer Science & Business Media. pp. 79–. ISBN 978-94-011-4439-1. Archived from the original on 15 February 2017.
- ^ a b c "Clomipramine". Archived from the original on 12 August 2017. Retrieved 12 August 2017.
- ^ "CLOMICALM clomipramine tablet CLOMIPRAMINE- clomipramine powder Novartis Animal Health US, Inc". Drugs@FDA. Novartis Animal Health US, Inc. December 1998. Archived from the original on 3 December 2013. Retrieved 1 December 2013.
- ^ Seksel K, Lindeman MJ (May 1998). "Use of clomipramine in the treatment of anxiety-related and obsessive-compulsive disorders in cats". Australian Veterinary Journal. 76 (5): 317–321. doi:10.1111/j.1751-0813.1998.tb12353.x. PMID 9631696.
- ^ Overall KL, Dunham AE (November 2002). "Clinical features and outcome in dogs and cats with obsessive-compulsive disorder: 126 cases (1989-2000)" (PDF). Journal of the American Veterinary Medical Association. 221 (10): 1445–1452. doi:10.2460/javma.2002.221.1445. PMID 12458615. S2CID 42730627. Archived from the original (PDF) on 3 December 2013. Retrieved 30 November 2013.
- ^ Yalcin E (2010). "Comparison of clomipramine and fluoxetine treatment of dogs with tail chasing". Tierarztliche Praxis. Ausgabe K, Kleintiere/Heimtiere. 38 (5): 295–299. doi:10.1055/s-0038-1622860. PMID 22215314. S2CID 2817066. Archived from the original (PDF) on 3 December 2013. Retrieved 30 November 2013.
- ^ Seksel K, Lindeman MJ (April 2001). "Use of clomipramine in treatment of obsessive-compulsive disorder, separation anxiety and noise phobia in dogs: a preliminary, clinical study". Australian Veterinary Journal. 79 (4): 252–256. doi:10.1111/j.1751-0813.2001.tb11976.x. PMID 11349411.
- ^ King JN, Steffan J, Heath SE, Simpson BS, Crowell-Davis SL, Harrington LJ, et al. (September 2004). "Determination of the dosage of clomipramine for the treatment of urine spraying in cats". Journal of the American Veterinary Medical Association. 225 (6): 881–887. doi:10.2460/javma.2004.225.881. PMID 15485047.
- ^ Landsberg GM, Wilson AL (2005). "Effects of clomipramine on cats presented for urine marking". Journal of the American Animal Hospital Association. 41 (1): 3–11. doi:10.5326/0410003. PMID 15634861.
- Alpha-1 blockers
- Antihistamines
- Chloroarenes
- CYP2D6 inhibitors
- Drugs developed by Novartis
- Dibenzazepines
- Dimethylamino compounds
- Dopamine antagonists
- Muscarinic antagonists
- Serotonin receptor antagonists
- Serotonin–norepinephrine reuptake inhibitors
- Tricyclic antidepressants
- World Health Organization essential medicines
- Treatment of obsessive–compulsive disorder
