Doxepin: Difference between revisions
| Line 114: | Line 114: | ||
| [[Histamine H4 receptor|H<sub>4</sub>]] || 106 || Human || <ref name="pmid11179435">{{cite journal |vauthors=Nguyen T, Shapiro DA, George SR, et al. |title=Discovery of a novel member of the histamine receptor family |journal=Mol. Pharmacol. |volume=59 |issue=3 |pages=427–33 |year=2001 |pmid=11179435 |doi= |url=}}</ref> |
| [[Histamine H4 receptor|H<sub>4</sub>]] || 106 || Human || <ref name="pmid11179435">{{cite journal |vauthors=Nguyen T, Shapiro DA, George SR, et al. |title=Discovery of a novel member of the histamine receptor family |journal=Mol. Pharmacol. |volume=59 |issue=3 |pages=427–33 |year=2001 |pmid=11179435 |doi= |url=}}</ref> |
||
|- |
|- |
||
| [[ |
| [[5-HT1A receptor|5-HT<sub>1A</sub>]] || 276 || Human || <ref name="pmid7855217" /> |
||
|- |
|- |
||
| [[ |
| [[5-HT2A receptor|5-HT<sub>2A</sub>]] || 11–27 || Human || <ref name="pmid23357028" /><ref name="pmid7855217" /> |
||
|- |
|- |
||
| [[5-HT2C receptor|5-HT<sub>2C</sub>]] || 8.8–200 || Human/rat || <ref name="pmid8876023">{{cite journal | vauthors = Pälvimäki EP, Roth BL, Majasuo H, Laakso A, Kuoppamäki M, Syvälahti E, Hietala J | title = Interactions of selective serotonin reuptake inhibitors with the serotonin 5-HT2c receptor | journal = Psychopharmacology (Berl.) | volume = 126 | issue = 3 | pages = 234–40 | year = 1996 | pmid = 8876023 | doi = | url = }}</ref><ref name="pmid23357028" /> |
|||
| ⚫ | |||
|- |
|- |
||
| [[5-HT3 receptor|5-HT<sub>3</sub>]] || {{abbr|ND|No data}} || Human || <ref name="pmid18314100">{{cite journal | vauthors = Gumilar F, Bouzat C | title = Tricyclic antidepressants inhibit homomeric Cys-loop receptors by acting at different conformational states | journal = Eur. J. Pharmacol. | volume = 584 | issue = 1 | pages = 30–9 | year = 2008 | pmid = 18314100 | doi = 10.1016/j.ejphar.2008.01.023 | url = }}</ref> |
|||
| ⚫ | |||
|- |
|- |
||
| ⚫ | | [[5-HT6 receptor|5-HT<sub>6</sub>]] || 136 || Rat || <ref name="pmid7680751">{{cite journal |vauthors=Monsma FJ, Shen Y, Ward RP, Hamblin MW, Sibley DR |title=Cloning and expression of a novel serotonin receptor with high affinity for tricyclic psychotropic drugs |journal=Mol. Pharmacol. |volume=43 |issue=3 |pages=320–7 |year=1993 |pmid=7680751 |doi= |url=}}</ref> |
||
| ⚫ | |||
|- |
|- |
||
| [[ |
| [[Alpha-1 adrenergic receptor|α<sub>1</sub>]] || 24 || Human || <ref name="pmid23357028" /> |
||
|- |
|- |
||
| [[ |
| [[Alpha-1B adrenergic receptor|α<sub>1B</sub>]] || 12 || Human || <ref name="pmid23357028" /> |
||
|- |
|- |
||
| [[ |
| [[Alpha-2A adrenergic receptor|α<sub>2A</sub>]] || 1,100–1,270 || Human || <ref name="pmid23357028" /><ref name="pmid23357028" /> |
||
|- |
|- |
||
| ⚫ | |||
| ⚫ | | [[5-HT6 receptor|5-HT<sub>6</sub>]] || 136 || Rat || <ref name="pmid7680751">{{cite journal |vauthors=Monsma FJ, Shen Y, Ward RP, Hamblin MW, Sibley DR |title=Cloning and expression of a novel serotonin receptor with high affinity for tricyclic psychotropic drugs |journal=Mol. Pharmacol. |volume=43 |issue=3 |pages=320–7 |year=1993 |pmid=7680751 |doi= |url=}}</ref> |
||
| ⚫ | |||
| ⚫ | |||
|- |
|||
| ⚫ | |||
|- |
|- |
||
| [[Muscarinic acetylcholine receptor M1|M<sub>1</sub>]] || 18–38 || Human || <ref name="pmid23357028" /><ref name="pmid8100134">{{cite journal | vauthors = Stanton T, Bolden-Watson C, Cusack B, Richelson E | title = Antagonism of the five cloned human muscarinic cholinergic receptors expressed in CHO-K1 cells by antidepressants and antihistaminics | journal = Biochem. Pharmacol. | volume = 45 | issue = 11 | pages = 2352–4 | year = 1993 | pmid = 8100134 | doi = | url = }}</ref> |
| [[Muscarinic acetylcholine receptor M1|M<sub>1</sub>]] || 18–38 || Human || <ref name="pmid23357028" /><ref name="pmid8100134">{{cite journal | vauthors = Stanton T, Bolden-Watson C, Cusack B, Richelson E | title = Antagonism of the five cloned human muscarinic cholinergic receptors expressed in CHO-K1 cells by antidepressants and antihistaminics | journal = Biochem. Pharmacol. | volume = 45 | issue = 11 | pages = 2352–4 | year = 1993 | pmid = 8100134 | doi = | url = }}</ref> |
||
| Line 141: | Line 145: | ||
|- |
|- |
||
| [[Muscarinic acetylcholine receptor M5|M<sub>5</sub>]] || 5.6–75 || Human || <ref name="pmid23357028" /><ref name="pmid8100134" /> |
| [[Muscarinic acetylcholine receptor M5|M<sub>5</sub>]] || 5.6–75 || Human || <ref name="pmid23357028" /><ref name="pmid8100134" /> |
||
| ⚫ | |||
| [[Dopamine D2 receptor|D<sub>2</sub>]] || 360 || Human || <ref name="pmid7855217" /> |
|||
|- |
|- |
||
|} |
|} |
||
Revision as of 00:50, 16 August 2017
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Sinequan, Silenor, others |
| Other names | NSC-108160[1] |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682390 |
| License data | |
| Pregnancy category |
|
| Routes of administration | Oral, topical, intravenous, intramuscular[2] |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 13–45% (mean 29%)[3][4] |
| Protein binding | 76%[5] |
| Metabolism | Hepatic (CYP2D6, CYP2C19)[6][3] |
| Metabolites | Nordoxepin, glucuronide conjugates[6] |
| Elimination half-life | Doxepin: 8–24 hours (mean 17 hours)[5] Nordoxepin: 31 hours[5] |
| Excretion | Urine: ~50%[6][3] Feces: minor[3] |
| Identifiers | |
| |
| CAS Number |
|
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| Chemical and physical data | |
| Formula | C19H21NO |
| Molar mass | 279.376 g/mol g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| | |
Doxepin, sold under the brand names Sinequan and Silenor among others, is an antidepressant and sleep aid medication used to treat depression and trouble sleeping.[2] It belongs to a class of antidepressants known as the tricyclic antidepressants (TCAs). It is believed to counteract depression by inhibiting the reuptake of serotonin and norepinephrine (via blocking their transporters), thereby increasing the concentrations of these neurotransmitters in the synapse and increasing the activity of their respective receptors. The drug also has antiadrenergic, antihistamine, antiserotonergic, and anticholinergic activities, which are thought to contribute largely to its side effects. At very low doses, it is a pure antihistamine and is used in the treatment of insomnia.[6]
Medical uses
Doxepin is used to treat depression, anxiety disorders, itchiness, trouble sleeping,[7] and as a second-line treatment of chronic idiopathic urticaria (hives).[2][8] Its oral formulations are FDA-approved for the treatment of depression, anxiety, and insomnia and its topical formulations are FDA-approved the short-term management (up to 8 days) of atopic dermatitis and lichen simplex chronicus.[9] Whereas in Australia and the United Kingdom, the only licensed indication(s) is/are in the treatment of major depression and pruritus in eczema, respectively.[10][11]
Contraindications
Known contraindications include:[12]
- Hypersensitivities to doxepin, other TCAs, or any of the excipients inside the product used
- Glaucoma
- A predisposition to developing urinary retention such as in benign prostatic hyperplasia
- Use of monoamine oxidase inhibitors in last 14 days[13]
Pregnancy and lactation
Its use in pregnant and lactating women is advised against, although the available preclinical (based on animal studies) evidence suggests it is unlikely to cause any deleterious effects on fetal development.[5] The lack of evidence from human studies, however, means it is currently impossible to rule out any risk to the fetus[5] and it is known to cross the placenta.[5] Doxepin is secreted in breast milk[2] and neonatal cases of respiratory depression in association with maternal doxepin use have been reported.[10]
Side effects
- Central nervous system: fatigue, dizziness, drowsiness, lightheadedness, confusion, nightmares, agitation, increased anxiety, insomnia, seizures (infrequently), delirium, rarely induction of hypomania and schizophrenia (stop medication immediately), extrapyramidal side effects (rarely), abuse in patients with polytoxicomania (rarely), tinnitus
- Anticholinergic: dry mouth, constipation, even ileus (rarely), difficulties in urinating, sweating, precipitation of glaucoma
- Antiadrenergic: hypotension, postural collapse (if patient arises too fast from lying/sitting position to standing), arrhythmias (sinus-tachycardia, bradycardia, AV-blockade)
- Allergic/toxic: skin rash, photosensitivity, liver damage of the cholestatic type (rarely), hepatitis (extremely rare), leuko- or thrombopenia (rarely), agranulocytosis (very rarely), hypoplastic anemia (rarely)
- Others: frequently increased appetite, weight gain, rarely nausea, frequently impaired sexual function in men (impotence, ejaculation-difficulties), rarely hypertension, rarely polyneuropathy, in both sexes breast-enlargement and galactorrhea (rarely)
- May increase or decrease liver function in some patients.[14]
- A large study linked the development of Alzheimer's disease and other forms of dementia to the use of doxepin, due to its anticholinergic properties.[15]
Overdose
Like other TCAs, doxepin is highly toxic in cases of overdose.[16] Mild symptoms include drowsiness, stupor, blurred vision, and excessive dryness of mouth. More serious adverse effects include respiratory depression, hypotension, coma, convulsions, cardiac arrhythmia, and tachycardia. Urinary retention, decreased gastrointestinal motility (paralytic ileus), hyperthermia (or hypothermia), hypertension, dilated pupils, and hyperactive reflexes are other possible symptoms of doxepin overdose.[5] Management of overdose is mostly supportive and symptomatic, and can include the administration of a gastric lavage so as to reduce absorption of the doxepin.[5] Supportive measures to prevent respiratory aspiration is also advisable.[5] Antiarrhythmic agents may be an appropriate measure to treat cardiac arrhythmias resulting from doxepin overdose.[5] Slow intravenous administration of physostigmine may reverse some of the toxic effects of overdose such as anticholinergic effects.[5] Haemodialysis is not recommended due to the high degree of protein binding with doxepin.[5] ECG monitoring is recommended for several days after doxepin overdose due to the potential for cardiac conduction abnormalities.[5]
Interactions
It should not be used within 14 days of using a monoamine oxidase inhibitor such as phenelzine due to the potential for hypertensive crisis or serotonin syndrome to develop.[12] Its use in those on CYP2D6 inhibitors such as fluoxetine or quinidine is recommended against due to the potential for its accumulation in the absence of full CYP2D6 catalytic activity.[12] Hepatic enzyme inducers such as carbamazepine, phenytoin, and barbiturates are advised against in patients receiving TCAs like doxepin due to the potential for problematically rapid metabolism of doxepin to occur in these individuals.[12] Sympathomimetic agents may have their effects potentiated by TCAs like doxepin.[12] Doxepin also may potentiate the adverse effects of anticholinergic agents such as benztropine, atropine and hyoscine (scopolamine).[12] Tolazamide, when used in conjunction with doxepin has been associated with a case of severe hypoglycaemia in a type II diabetic individual.[12] Cimetidine may influence the absorption of doxepin.[12] Alcohol may potentiate some of the CNS depressant effects of doxepin.[12] Antihypertensive agents may have their effects mitigated by doxepin.[12] Cotreatment with CNS depressants such as the benzodiazepines can cause additive CNS depression.[5] Co-treatment with thyroid hormones may also increase the potential for adverse reactions.[5]
Pharmacology
| Site | Ki (nM) | Species | Ref |
|---|---|---|---|
| SERT | 68–210 | Human | [18][17][6] |
| NET | 13–58 | Human | [6][18][17] |
| DAT | ≥4,600 | Human | [18][6] |
| H1 | 0.09–0.78 | Human | [19][20][17] |
| H2 | 160 | Undefined | [21][22] |
| H3 | >10,000 | Human | [17] |
| H4 | 106 | Human | [23] |
| 5-HT1A | 276 | Human | [20] |
| 5-HT2A | 11–27 | Human | [17][20] |
| 5-HT2C | 8.8–200 | Human/rat | [24][17] |
| 5-HT3 | ND | Human | [25] |
| 5-HT6 | 136 | Rat | [26] |
| α1 | 24 | Human | [17] |
| α1B | 12 | Human | [17] |
| α2A | 1,100–1,270 | Human | [17][17] |
| α2B | 28 | Human | [17] |
| α2C | 96 | Human | [17] |
| D2 | 360 | Human | [20] |
| M1 | 18–38 | Human | [17][27] |
| M2 | 160–230 | Human | [17][27] |
| M3 | 25–52 | Human | [17][27] |
| M4 | 20–82 | Human | [17][27] |
| M5 | 5.6–75 | Human | [17][27] |
Doxepin is a reuptake inhibitor of serotonin and norepinephrine, or a serotonin–norepinephrine reuptake inhibitor (SNRI), and has additional antiadrenergic, antihistamine, antiserotonergic, and anticholinergic activities.[28] It is specifically an antagonist of the histamine H1 and H2 receptors, the serotonin 5-HT2A and 5-HT2C receptors, the α1-adrenergic receptor, and the muscarinic acetylcholine receptors (M1–M5).[28] Similarly to other TCAs, doxepin is also a potent blocker of voltage-gated sodium channels, and this action is thought to be involved in both its lethality in overdose[29] and its effectiveness as an analgesic (including in the treatment of neuropathic pain,[30] as a migraine prophylactic,[31] and as a local anesthetic).[32] The potencies of doxepin in terms of its receptor antagonism specifically are as follows:[32][33]
- Extremely strong: H1 receptor
- Strong: 5-HT2, α1-adrenergic, and mACh receptors
- Moderate: 5-HT1 receptors
- Weak: α2-adrenergic and D2 receptors
A study reported the IC50 values of doxepin for human monoamine reuptake inhibition as 13 nM for norepinephrine, 210 nM for serotonin, and 4,600 nM for dopamine, suggesting that doxepin is relatively selective for inhibition of norepinephrine reuptake with weaker effects on serotonin reuptake and negligible influence on dopamine reuptake.[18][17]
The major metabolite of doxepin, nordoxepin (desmethyldoxepin), is pharmacologically active similarly,[6] but in contrast to doxepin, is a relatively selective norepinephrine reuptake inhibitor.[34][35] In general, the demethylated variants of tertiary amine TCAs like doxepin are much more potent inhibitors of norepinephrine reuptake, less potent inhibitors of serotonin reuptake, and less potent in their antiadrenergic, antihistamine, and anticholinergic activities.[34][35][36]
Antidepressant doses of doxepin are defined as 25 to 300 mg/day, although are typically above 75 mg/day.[37][38] Antihistamine doses, including for dermatological uses and as a sedative/hypnotic for insomnia, are considered to be 3 to 25 mg,[39][38] although higher doses between 25 and 50 mg and in some cases even up to 150 mg have been used to treat insomnia.[40] At low doses, below 25 mg, doxepin is a pure antihistamine.[37] At antidepressant doses of above 25 mg, doxepin has significant antiadrenergic, antiserotonergic, and anticholinergic effects, and these activities contribute to its side effects.[39][37][38]
As a hypnotic
| Drug | H1 | mACh |
|---|---|---|
| Amitriptyline | 1.1 | 18 |
| Amoxapine | 25 | 1,000 |
| Clomipramine | 31 | 37 |
| Desipramine | 110 | 196 |
| Dosulepin[39] | 4.0 | 38 |
| Doxepin | 0.24 | 83 |
| Imipramine | 11 | 91 |
| Lofepramine[20] | 360 | 67 |
| Maprotiline | 2.0 | 560 |
| Mianserin | 0.40 | 820 |
| Mirtazapine | 0.14 | 670 |
| Nortriptyline | 10 | 149 |
| Protriptyline | 25 | 25 |
| Trimipramine | 0.27 | 58 |
| All values are Ki (nM) | ||
Doxepin is a highly potent antihistamine, with this being its strongest activity.[33][37][43][6] In fact, doxepin has been said to be the most or one of the most potent H1 receptor antagonists available, with one study finding an in vitro Ki of 0.17 nM.[20] It is the most potent and selective H1 receptor antagonist of the TCAs (although the tetracyclic antidepressant (TeCA) mirtazapine is slightly more potent),[39][44][45] and other sedating antihistamines, for instance the over-the-counter diphenhydramine (Ki = 16 nM) and doxylamine (Ki = 42 nM), show far lower affinities for this receptor in comparison.[6] The affinity of doxepin for the H1 receptor is far greater than its affinity for other sites,[6] and 10- to 100-fold higher doses are needed for antidepressant effects.[46][43] In accordance, although it is often described as a "dirty drug" due to its highly promiscuous binding profile,[43] doxepin acts as a highly selective antagonist of the H1 receptor at very low doses (less than 10 mg; typically 3 to 6 mg).[37][6][38] At these doses, it notably has no clinically relevant anticholinergic effects such as dry mouth or cognitive/memory impairment, unlike most other sedating antihistamines, and similarly has no effect on other receptors such as adrenergic and serotonin receptors.[37][6][38]
The H1 receptor antagonism of doxepin is responsible for its hypnotic effects and its effectiveness in the treatment of insomnia at low doses.[6][43] The incidence of side effects with doxepin and its safety at these doses was similar to that of placebo in clinical trials; the most frequent side effects were headache and somnolence/sedation, both with an incidence of less than 5%.[37][6] Other side effects sometimes associated with antihistamines, including daytime sedation, increased appetite, and weight gain, all were not observed.[43] Clinical evidence of H1 receptor antagonists and TCAs for the treatment insomnia shows mixed effectiveness and is limited in its quality due to weaknesses like small sample sizes and poor generalizability.[38][47] However, doxepin is a unique and notable exception; it has been well-studied in the treatment of insomnia and shows consistent benefits with excellent tolerability and safety.[38][47] Aside from diphenhydramine and doxylamine, which have historical approval as hypnotics, doxepin is the only H1 receptor antagonist that is specifically approved for the treatment of insomnia in the United States.[47][48]
The effect sizes of very-low-dose doxepin in the treatment of insomnia range from small to medium.[38] These include subjective and objective measures of sleep maintenance, sleep duration, and sleep efficiency.[38] Conversely, very-low-dose doxepin shows relatively weak effects on sleep initiation and does not significantly separate from placebo on this measure.[38] This is in contrast to benzodiazepines and nonbenzodiazepine (Z-drug) hypnotics, which are additionally effective in improving sleep onset latency.[38] However, it is also in contrast to higher doses of doxepin (50 to 300 mg/day), which have been found to significantly reduce latency to sleep onset.[38] A positive dose–response relationship on sleep measures was observed for doses of doxepin between 1 and 6 mg in clinical studies, whereas the incidence of adverse effects remained constant across this dose range in both young and older adults.[38] However, the incidence of adverse effects appeared to increase with longer treatment duration.[38] A dose of doxepin as low as 1 mg/day was found to significantly improve most of the assessed sleep measures, but unlike the 3 and 6 mg/day doses, was not able to improve wake time during sleep.[38] This, along with greater effect sizes with the higher doses, was likely the basis for the approval of the 3 and 6 mg doses of doxepin for insomnia and not the 1 mg dose.[38]
At very low doses, doxepin has not shown discontinuation or withdrawal effects nor rebound insomnia.[6] Sustained effectiveness without apparent tolerance was demonstrated in clinical studies of up to 12 weeks duration.[47] This appears to be in contrast to over-the-counter antihistamines like diphenhydramine and doxylamine and all other first-generation antihistamines, which are associated with rapid development of tolerance and dependence (by day 3 or 4 of continuous dosing) and loss of hypnotic effectiveness.[47] It is for this reason that, unlike doxepin, they are not recommended for the chronic management of insomnia and are advised for only short-term treatment (i.e., 1 week).[47] It is not entirely clear why doxepin and first-generation antihistamines are different in this regard, but it has been suggested that it may have to do with the lack of selectivity for the H1 receptor of the latter or may have to do with the use of optimal doses.[43] Unlike very-low-dose doxepin, most first-generation antihistamines also have marked anticholinergic activity as well as associated side effects such as dry mouth, constipation, urinary retention, and confusion.[47] This is particularly true in older people, and antihistamines with concomitant anticholinergic effects are not recommended in adults over the age of 65.[47] Anticholinergic activity notably may interfere with the sleep-promoting effects of H1 receptor blockade.[17]
Antagonism of the H1, 5-HT2A, 5-HT2C, and α1-adrenergic receptors is thought to have sleep-promoting effects and to be responsible for the sedative effects of TCAs including those of doxepin.[49][50][51] Although doxepin is selective for the H1 receptor at doses lower than 25 mg, blockade of serotonin and adrenergic receptors may also be involved in the hypnotic effects of doxepin at higher doses.[49] However, in contrast to very low doses of doxepin, rebound insomnia and daytime sedation are significantly more frequent than placebo with moderate doses (25 to 50 mg/day) of the drug.[38] In addition, one study found that although such doses of doxepin improved sleep measures initially, most of the benefits were lost with chronic treatment (by 4 weeks).[38] Due to limited data however, more research on potential tolerance and withdrawal effects of moderate doses of doxepin is needed.[38] At these doses of doxepin, dry mouth, an anticholinergic effect, was common (71%), and other side effects such as headache (25%), increased appetite (21%), and dizziness (21%) were also frequently observed, although these adverse effects were notably not significantly more frequent than with placebo in the study in question.[38] In any case, taken together, higher doses of doxepin than very low doses are associated with an increased rate of side effects as well as apparent loss of hypnotic effectiveness with chronic treatment.[43]
Doxepin at a dose of 25 mg/day for 3 weeks has been found to decrease cortisol levels by 16% in adults with chronic insomnia and to increase melatonin production by 26% in healthy volunteers.[6] In individuals with neuroendocrine dysregulation in the form of nocturnal melatonin deficiency presumably due to chronic insomnia, very-low-dose doxepin was found to restore melatonin levels to near-normal values after 3 weeks of treatment.[32] These findings suggest that normalization of the hypothalamic–pituitary–adrenal axis and the circadian sleep–wake cycle may be involved in the beneficial effects of doxepin on sleep and insomnia.[6][32]
Pharmacokinetics
| Parameters | Value |
|---|---|
| Tmax (doxepin) | 2–4 hours (mean 2.9 hours) |
| Cmax (doxepin) | 8.8–45.8 ng/mL |
| Tmax (nordoxepin) | 2–10 hours |
| Cmax (nordoxepin) | 4.8–14.5 ng/mL (mean 9.7 ng/mL) |
| VD | 20 L/kg |
| Protein bound | 76% |
| t1/2 (doxepin) | 8–24 hours (mean 17 hours) |
| t1/2 (nordoxepin) | 31 hours |
| Metabolic enzymes |
CYP2D6, CYP1A2, CYP3A4, CYP2C19 |
| Metabolic pathways |
N-demethylation, N-oxidation, hydroxylation, and glucuronidation |
Doxepin is well-absorbed from the gastrointestinal tract but between 55 and 87% undergoes first-pass metabolism in the liver,[6] resulting in a mean oral bioavailability of approximately 29%.[4] Following a single very low dose of 6 mg, peak plasma levels of doxepin are 0.854 ng/mL (3.06 nmol/L) at 3 hours without food and 0.951 ng/mL (3.40 nmol/L) at 6 hours with food.[6] Plasma concentrations of doxepin with antidepressant doses are far greater, ranging between 50 to 250 ng/mL (180 to 900 nmol/L).[52] Area-under-curve levels of of the drug are increased significantly when it is taken with food.[6] It is widely distributed throughout the body and is approximately 80% plasma protein bound, specifically to albumin and α1-acid glycoprotein.[6][53]
Doxepin is extensively metabolized via oxidation and demethylation.[6] The major enzymes involved in its metabolism are the cytochrome P450 enzymes CYP2D6 and CYP2C19, with CYP1A2 and CYP2C9 also involved to a lesser extent.[6] The major metabolite of doxepin, nordoxepin, is formed mainly by CYP2C19.[54] Both doxepin and nordoxepin are transformed into glucuronide conjugates.[32][6] The terminal half-life of doxepin is about 15–18 hours, whereas that of nordoxepin is around 28–31 hours.[6][55] Up to 10% of Caucasian individuals show reduced metabolism of doxepin that can result in up to 8-fold elevated plasma concentrations of the drug compared to normal.[33][32]
Doxepin is eliminated primarily in the urine and predominantly in the form of glucuronide conjugates, with less than 3% of a dose excreted unchanged as doxepin or nordoxepin.[6]
Chemistry
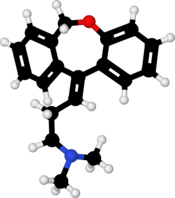
Doxepin is a tricyclic compound, specifically a dibenzoxepin, and possesses three rings fused together with a side chain attached in its chemical structure.[32] It is the only tricyclic medication with a dibenzoxepin ring system to have been marketed.[56] Doxepin is a tertiary amine TCA, with its side chain-demethylated metabolite nordoxepin being a secondary amine.[34][35] The drug is a mixture of (E) and (Z) stereoisomers (the latter being known as cidoxepin or cis-doxepin) and is used commercially in a ratio of approximately 85:15.[1][57] Its chemical name is (E/Z)-3-(dibenzo[b,e]oxepin-11(6H)-ylidene)-N,N-dimethylpropan-1-amine[32][58] and its free base form has a chemical formula of C19H21NO with a molecular weight of 279.376 g/mol.[58] The drug is used commercially almost exclusively as the hydrochloride salt; the free base has been used rarely.[1][59] The CAS Registry Number of the free base is 1668-19-5 and of the hydrochloride is 1229-29-4.[1][59]
History
Doxepin was discovered in Germany in 1963 and was introduced in the United States as an antidepressant in 1969.[32] It was subsequently approved at very low doses in the United States for the treatment of insomnia in 2010.[38][59]
Society and culture
Generic names
Doxepin is the generic name of the drug in English and German and its INN and BAN, while doxepin hydrochloride is its USAN, USP, BANM, and JAN.[1][59][60][61] Its generic name in Spanish and Italian and its DCIT are doxepina, in French and its DCF are doxépine, and in Latin is doxepinum.[61]
The cis or (Z) stereoisomer of doxepin is known as cidoxepin, and this is its INN while cidoxepin hydrochloride is its USAN.[1]
Brand names
Doxepin has been marketed as an antidepressant most commonly under the brand names Adapin, Curatin, and Sinequan.[1][59][60][61] It is approved specifically for the treatment of insomnia under the brand name Silenor in the United States and Canada.[6][61]
Research
Antihistamine
Cidoxepin is under development by Elorac, Inc. for the treatment of chronic urticaria (hives).[62] As of 2017, it is in phase II clinical trials for this indication.[62] The drug was also under investigation for the treatment of allergic rhinitis, atopic dermatitis, and contact dermatitis, but development for these indications was discontinued.[62]
References
- ^ a b c d e f g J. Elks (14 November 2014). The Dictionary of Drugs: Chemical Data: Chemical Data, Structures and Bibliographies. Springer. pp. 469–. ISBN 978-1-4757-2085-3.
- ^ a b c d "Doxepin Hydrochloride". Martindale: The Complete Drug Reference. London, UK: Pharmaceutical Press. 30 January 2013. Retrieved 3 December 2013.
- ^ a b c d Thomas L. Lemke; David A. Williams (24 January 2012). Foye's Principles of Medicinal Chemistry. Lippincott Williams & Wilkins. pp. 604–. ISBN 978-1-60913-345-0.
- ^ a b Yan JH, Hubbard JW, McKay G, Korchinski ED, Midha KK (2002). "Absolute bioavailability and stereoselective pharmacokinetics of doxepin". Xenobiotica. 32 (7): 615–23. doi:10.1080/00498250210131879. PMID 12162857.
- ^ a b c d e f g h i j k l m n o p "Sinepin Capsules 25mg - Summary of Product Characteristics (SPC)". electronic Medicines Compendium. Marlborough Pharmaceuticals Ltd. 22 September 2011. Retrieved 3 December 2013.
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab Weber J, Siddiqui MA, Wagstaff AJ, McCormack PL (2010). "Low-dose doxepin: in the treatment of insomnia". CNS Drugs. 24 (8): 713–20. doi:10.2165/11200810-000000000-00000. PMID 20658801.
- ^ Hajak G; Rodenbeck A; Voderholzer U; et al. (2001). "Doxepin in the treatment of primary insomnia: a placebo-controlled, double-blind, polysomnographic study". J Clin Psychiatry. 62 (6): 453–63. doi:10.4088/JCP.v62n0609. PMID 11465523.
- ^ "Doxepin". The American Society of Health-System Pharmacists. Retrieved 3 April 2011.
- ^ "PRUDOXIN (doxepin hydrochloride) cream [HEALTHPOINT, LTD]". DailyMed. HEALTHPOINT, LTD. August 2010. Retrieved 3 December 2013.
- ^ a b Rossi, S, ed. (2013). Australian Medicines Handbook (2013 ed.). Adelaide: The Australian Medicines Handbook Unit Trust. ISBN 978-0-9805790-9-3.
- ^ Joint Formulary Committee (2013). British National Formulary (BNF) (65 ed.). London, UK: Pharmaceutical Press. ISBN 978-0-85711-084-8.
- ^ a b c d e f g h i j k "Deptran Doxepin (as hydrochloride)" (PDF). TGA eBusiness Services. Alphapharm Pty Ltd. 6 May 2013. Retrieved 3 December 2013.
- ^ "Silenor (doxepin) dosing, indications, interactions, adverse effects, and more". Medscape Reference. WebMD. Retrieved 3 December 2013.
- ^ Lippincott "nursing 2007 drug handbook" LWW press. 2007
- ^ Gray, Shelly L.; Anderson, Melissa L. (January 26, 2015). "Cumulative Use of Strong Anticholinergics and Incident Dementia: A Prospective Cohort Study". JAMA Intern. Med. 175: 401–7. doi:10.1001/jamainternmed.2014.7663. PMC 4358759. PMID 25621434. Retrieved January 27, 2015.
- ^ White, N; Litovitz, T; Clancy, C (December 2008). "Suicidal antidepressant overdoses: a comparative analysis by antidepressant type" (PDF). Journal of Medical Toxicology. 4 (4): 238–250. doi:10.1007/BF03161207. PMC 3550116. PMID 19031375.
- ^ a b c d e f g h i j k l m n o p q r s t Krystal AD, Richelson E, Roth T (2013). "Review of the histamine system and the clinical effects of H1 antagonists: basis for a new model for understanding the effects of insomnia medications". Sleep Med Rev. 17 (4): 263–72. doi:10.1016/j.smrv.2012.08.001. PMID 23357028.
- ^ a b c d Tatsumi M, Groshan K, Blakely RD, Richelson E (1997). "Pharmacological profile of antidepressants and related compounds at human monoamine transporters". Eur. J. Pharmacol. 340 (2–3): 249–58. PMID 9537821.
- ^ Booth RG, Moniri NH, Bakker RA, Choksi NY, Nix WB, Timmerman H, Leurs R (2002). "A novel phenylaminotetralin radioligand reveals a subpopulation of histamine H(1) receptors". J. Pharmacol. Exp. Ther. 302 (1): 328–36. PMID 12065734.
- ^ a b c d e f Cusack B, Nelson A, Richelson E (1994). "Binding of antidepressants to human brain receptors: focus on newer generation compounds". Psychopharmacology (Berl.). 114 (4): 559–65. PMID 7855217.
- ^ Leslie Iversen (29 June 2013). Biochemical Studies of CNS Receptors. Springer Science & Business Media. pp. 404–. ISBN 978-1-4684-4361-5.
- ^ Ross J. Baldessarini (1985). Chemotherapy in Psychiatry: Principles and Practice. Harvard University Press. pp. 156–. ISBN 978-0-674-11383-1.
- ^ Nguyen T, Shapiro DA, George SR, et al. (2001). "Discovery of a novel member of the histamine receptor family". Mol. Pharmacol. 59 (3): 427–33. PMID 11179435.
- ^ Pälvimäki EP, Roth BL, Majasuo H, Laakso A, Kuoppamäki M, Syvälahti E, Hietala J (1996). "Interactions of selective serotonin reuptake inhibitors with the serotonin 5-HT2c receptor". Psychopharmacology (Berl.). 126 (3): 234–40. PMID 8876023.
- ^ Gumilar F, Bouzat C (2008). "Tricyclic antidepressants inhibit homomeric Cys-loop receptors by acting at different conformational states". Eur. J. Pharmacol. 584 (1): 30–9. doi:10.1016/j.ejphar.2008.01.023. PMID 18314100.
- ^ Monsma FJ, Shen Y, Ward RP, Hamblin MW, Sibley DR (1993). "Cloning and expression of a novel serotonin receptor with high affinity for tricyclic psychotropic drugs". Mol. Pharmacol. 43 (3): 320–7. PMID 7680751.
- ^ a b c d e Stanton T, Bolden-Watson C, Cusack B, Richelson E (1993). "Antagonism of the five cloned human muscarinic cholinergic receptors expressed in CHO-K1 cells by antidepressants and antihistaminics". Biochem. Pharmacol. 45 (11): 2352–4. PMID 8100134.
- ^ a b Roth, BL; Driscol, J (12 January 2011). "PDSP Ki Database". Psychoactive Drug Screening Program (PDSP). University of North Carolina at Chapel Hill and the United States National Institute of Mental Health. Archived from the original on 8 November 2013. Retrieved 20 October 2013.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Thanacoody HK, Thomas SH (2005). "Tricyclic antidepressant poisoning : cardiovascular toxicity". Toxicol Rev. 24 (3): 205–14. PMID 16390222.
- ^ Bertelsen, Anne K.; Backonja, Misha-Miroslav (2007). "Drugs Targeting Voltage-Gated Sodium and Calcium Channels": 651–651. doi:10.1007/978-3-540-29805-2_1205.
{{cite journal}}: Cite journal requires|journal=(help) - ^ Cohen GL (2005). "Migraine prophylactic drugs work via ion channels". Med. Hypotheses. 65 (1): 114–22. doi:10.1016/j.mehy.2005.01.027. PMID 15893128.
- ^ a b c d e f g h i Singh H, Becker PM (2007). "Novel therapeutic usage of low-dose doxepin hydrochloride". Expert Opin Investig Drugs. 16 (8): 1295–305. doi:10.1517/13543784.16.8.1295. PMID 17685877.
- ^ a b c Lankford, Alan (2011). "Low-dose doxepin (3 and 6 mg) for the treatment of insomnia". Future Neurology. 6 (2): 143–154. doi:10.2217/fnl.10.83. ISSN 1479-6708.
- ^ a b c Neal R. Cutler; John J. Sramek; Prem K. Narang (20 September 1994). Pharmacodynamics and Drug Development: Perspectives in Clinical Pharmacology. John Wiley & Sons. pp. 160–. ISBN 978-0-471-95052-3.
- ^ a b c Pavel Anzenbacher; Ulrich M. Zanger (23 February 2012). Metabolism of Drugs and Other Xenobiotics. John Wiley & Sons. pp. 302–. ISBN 978-3-527-64632-6.
- ^ Alan F. Schatzberg; Charles B. Nemeroff (2009). The American Psychiatric Publishing Textbook of Psychopharmacology. American Psychiatric Pub. pp. 264–. ISBN 978-1-58562-309-9.
- ^ a b c d e f g Rojas-Fernandez CH, Chen Y (2014). "Use of ultra-low-dose (≤6 mg) doxepin for treatment of insomnia in older people". Can Pharm J (Ott). 147 (5): 281–9. doi:10.1177/1715163514543856. PMC 4213269. PMID 25364337.
- ^ a b c d e f g h i j k l m n o p q r s t u Yeung WF, Chung KF, Yung KP, Ng TH (2015). "Doxepin for insomnia: a systematic review of randomized placebo-controlled trials". Sleep Med Rev. 19: 75–83. doi:10.1016/j.smrv.2014.06.001. PMID 25047681.
- ^ a b c d Gillman PK (2007). "Tricyclic antidepressant pharmacology and therapeutic drug interactions updated". Br. J. Pharmacol. 151 (6): 737–48. doi:10.1038/sj.bjp.0707253. PMC 2014120. PMID 17471183.
- ^ Tariq SH, Pulisetty S (2008). "Pharmacotherapy for insomnia". Clin. Geriatr. Med. 24 (1): 93–105, vii. doi:10.1016/j.cger.2007.08.009. PMID 18035234.
- ^ Laurence Brunton; Bruce A. Chabner; Bjorn Knollman (14 January 2011). Goodman and Gilman's The Pharmacological Basis of Therapeutics, Twelfth Edition. McGraw Hill Professional. p. 410. ISBN 978-0-07-176939-6.
- ^ Richelson E, Nelson A (1984). "Antagonism by antidepressants of neurotransmitter receptors of normal human brain in vitro". J. Pharmacol. Exp. Ther. 230 (1): 94–102. PMID 6086881.
- ^ a b c d e f g Stahl SM (2008). "Selective histamine H1 antagonism: novel hypnotic and pharmacologic actions challenge classical notions of antihistamines". CNS Spectr. 13 (12): 1027–38. PMID 19179941.
- ^ Richelson E (1979). "Tricyclic antidepressants and histamine H1 receptors". Mayo Clin. Proc. 54 (10): 669–74. PMID 39202.
- ^ Alan F. Schatzberg; Charles B. Nemeroff (10 May 2017). The American Psychiatric Association Publishing Textbook of Psychopharmacology. American Psychiatric Pub. pp. 322–. ISBN 978-1-61537-122-8.
- ^ Stahl SM (2009). "Multifunctional drugs: a novel concept for psychopharmacology". CNS Spectr. 14 (2): 71–3. PMID 19238121.
- ^ a b c d e f g h Vande Griend JP, Anderson SL (2012). "Histamine-1 receptor antagonism for treatment of insomnia". J Am Pharm Assoc (2003). 52 (6): e210–9. doi:10.1331/JAPhA.2012.12051. PMID 23229983.
- ^ "Sleep Disorder (Sedative-Hypnotic) Drug Information - U.S. FDA" (HTML). 13 June 2017. Retrieved 9 August 2017.
- ^ a b Katwala, Jigar; Kumar, Ananda K; Sejpal, Jaykumar J; Terrence, Marcelle; Mishra, Manish (2013). "Therapeutic rationale for low dose doxepin in insomnia patients". Asian Pacific Journal of Tropical Disease. 3 (4): 331–336. doi:10.1016/S2222-1808(13)60080-8. ISSN 2222-1808. PMC 4027305.
In general, sedating properties of anti-depressant agents are related to antagonism of serotonin 5HT2, histamines, and α-1 adrenergic receptors[14]–[16].
- ^ Landolt HP, Wehrle R (2009). "Antagonism of serotonergic 5-HT2A/2C receptors: mutual improvement of sleep, cognition and mood?". Eur. J. Neurosci. 29 (9): 1795–809. doi:10.1111/j.1460-9568.2009.06718.x. PMID 19473234.
- ^ Broese M, Riemann D, Hein L, Nissen C (2012). "α-Adrenergic receptor function, arousal and sleep: mechanisms and therapeutic implications". Pharmacopsychiatry. 45 (6): 209–16. doi:10.1055/s-0031-1299728. PMID 22290201.
- ^ Leucht S, Steimer W, Kreuz S, Abraham D, Orsulak PJ, Kissling W (2001). "Doxepin plasma concentrations: is there really a therapeutic range?". J Clin Psychopharmacol. 21 (4): 432–9. PMID 11476128.
- ^ Virtanen R, Iisalo E, Irjala K (1982). "Protein binding of doxepin and desmethyldoxepin". Acta Pharmacol Toxicol (Copenh). 51 (2): 159–64. PMID 7113722.
- ^ Härtter S, Tybring G, Friedberg T, Weigmann H, Hiemke C (2002). "The N-demethylation of the doxepin isomers is mainly catalyzed by the polymorphic CYP2C19". Pharm. Res. 19 (7): 1034–7. PMID 12180536.
- ^ Virtanen R, Scheinin M, Iisalo E (1980). "Single dose pharmacokinetics of doxepin in healthy volunteers". Acta Pharmacol Toxicol (Copenh). 47 (5): 371–6. PMID 7293791.
- ^ Manuchair Ebadi (31 October 2007). Desk Reference of Clinical Pharmacology, Second Edition. CRC Press. pp. 329–. ISBN 978-1-4200-4744-8.
- ^ Shufeng Zhou (6 April 2016). Cytochrome P450 2D6: Structure, Function, Regulation and Polymorphism. CRC Press. pp. 142–. ISBN 978-1-4665-9788-4.
- ^ a b https://chem.nlm.nih.gov/chemidplus/rn/1668-19-5
- ^ a b c d e Index Nominum 2000: International Drug Directory. Taylor & Francis. 2000. pp. 370–. ISBN 978-3-88763-075-1.
- ^ a b I.K. Morton; Judith M. Hall (6 December 2012). Concise Dictionary of Pharmacological Agents: Properties and Synonyms. Springer Science & Business Media. pp. 106–. ISBN 978-94-011-4439-1.
- ^ a b c d Drugs.com International brands of doxepin Page accessed August 23, 2016
- ^ a b c http://adisinsight.springer.com/drugs/800032883
