Alcohol (drug): Difference between revisions
→Social Damage: Added content Tags: Reverted Mobile edit Mobile web edit |
m Reverted edits by FelixFelton800 (talk) to last version by Kurousagi |
||
| Line 117: | Line 117: | ||
Alcohol has a variety of short-term and long-term [[adverse effect]]s. It also has [[reinforcement]]-related adverse effects, including [[drug addiction|addiction]], [[drug dependence|dependence]], and [[drug withdrawal|withdrawal]]. |
Alcohol has a variety of short-term and long-term [[adverse effect]]s. It also has [[reinforcement]]-related adverse effects, including [[drug addiction|addiction]], [[drug dependence|dependence]], and [[drug withdrawal|withdrawal]]. |
||
===Social |
===Social harm=== |
||
[[File:HarmCausedByDrugsTable.svg|thumb|left|upright=1.4| |
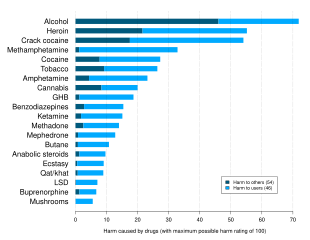
[[File:HarmCausedByDrugsTable.svg|thumb|left|upright=1.4|A 2010 study ranking various illegal and legal drugs based on statements by drug-harm experts. Alcohol was found to be the overall most dangerous drug, and the only drug that mostly damaged others.<ref>{{cite journal|last1=Nutt|first1=David J|last2=King|first2=Leslie A|last3=Phillips|first3=Lawrence D|title=Drug harms in the UK: a multicriteria decision analysis|journal=The Lancet|date=November 2010|volume=376|issue=9752|pages=1558–1565|doi=10.1016/S0140-6736(10)61462-6|pmid=21036393|citeseerx=10.1.1.690.1283|s2cid=5667719}}</ref>]] |
||
Alcohol causes a plethora of |
Alcohol causes a plethora of detrimental effects in society, both to the individual and to others.<ref name="ButcherHooley2013">{{cite book | first1 = James N. | last1 = Butcher | first2 = Jill M. | last2 = Hooley | first3 = Susan M | last3 = Mineka | name-list-style = vanc |title=Abnormal Psychology|url=https://books.google.com/books?id=_aksAAAAQBAJ&pg=PA370|date=25 June 2013|publisher=Pearson Education|isbn=978-0-205-97175-6|page=370}}</ref> It is highly associated with [[automobile accident]]s, [[sexual assault]]s, and both [[violent crime|violent]] and non-violent crime.<ref name="ButcherHooley2013" /> About one-third of [[arrest]]s in the [[United States]] involve alcohol misuse.<ref name="ButcherHooley2013" /> Many [[emergency room]] visits also involve alcohol use.<ref name="ButcherHooley2013" /> As many as 15% of employees show problematic alcohol-related behaviors in the workplace, such as drinking before going to work or even drinking on the job.<ref name="ButcherHooley2013" /> [[Heavy drinking]] is associated with vulnerability to [[injury]], [[marital discord]], and [[domestic violence]].<ref name="ButcherHooley2013" /> Alcohol use is directly related to considerable [[morbidity]] and [[mortality rate|mortality]], for instance due to [[overdose]] and alcohol-related health problems.<ref name="Friedman2011">{{cite book | first = Howard S. | last = Friedman | name-list-style = vanc |title=The Oxford Handbook of Health Psychology|url=https://books.google.com/books?id=J3-78PdF83kC&pg=PA699|date=26 August 2011|publisher=Oxford University Press, USA|isbn=978-0-19-534281-9|pages=699–}}</ref> |
||
====Alcohol-related crimes==== |
====Alcohol-related crimes==== |
||
| Line 127: | Line 127: | ||
=====Automobile accidents===== |
=====Automobile accidents===== |
||
{{Main|Drunk driving|Driving under the influence|l2=Driving under influence}} |
{{Main|Drunk driving|Driving under the influence|l2=Driving under influence}} |
||
A 2002 study found 41% of people fatally injured in traffic accidents were in alcohol-related crashes.<ref name="pmid15301401">{{cite journal | vauthors = Hingson R, Winter M | title = Epidemiology and consequences of drinking and driving | journal = Alcohol Research & Health | volume = 27 | issue = 1 | pages = 63–78 | year = 2003 | pmid = 15301401 | pmc = 6676697 }}</ref> Misuse of alcohol is associated with more than 40% of deaths that occur in automobile accidents every year.<ref name="ButcherHooley2013" /> The risk of a fatal [[car accident]] increases exponentially with the level of alcohol in the driver's blood.<ref name="pmid8448514">{{cite journal | vauthors = Naranjo CA, Bremner KE | title = Behavioural correlates of alcohol intoxication | journal = Addiction | volume = 88 | issue = 1 | pages = 25–35 | date = January 1993 | pmid = 8448514 | doi = 10.1111/j.1360-0443.1993.tb02761.x }}</ref> Most [[drunk driving]] laws in the United States governing the acceptable levels in the blood while driving or operating heavy machinery set typical upper limits of legal |
A 2002 study found 41% of people fatally injured in traffic accidents were in alcohol-related crashes.<ref name="pmid15301401">{{cite journal | vauthors = Hingson R, Winter M | title = Epidemiology and consequences of drinking and driving | journal = Alcohol Research & Health | volume = 27 | issue = 1 | pages = 63–78 | year = 2003 | pmid = 15301401 | pmc = 6676697 }}</ref> Misuse of alcohol is associated with more than 40% of deaths that occur in automobile accidents every year.<ref name="ButcherHooley2013" /> The risk of a fatal [[car accident]] increases exponentially with the level of alcohol in the driver's blood.<ref name="pmid8448514">{{cite journal | vauthors = Naranjo CA, Bremner KE | title = Behavioural correlates of alcohol intoxication | journal = Addiction | volume = 88 | issue = 1 | pages = 25–35 | date = January 1993 | pmid = 8448514 | doi = 10.1111/j.1360-0443.1993.tb02761.x }}</ref> Most [[drunk driving]] laws in the United States governing the acceptable levels in the blood while driving or operating heavy machinery set typical upper limits of legal [[blood alcohol content]] (BAC) at 0.08%.<ref name="NHTSA2001">{{cite web|title=Legislative History of .08 per se Laws – NHTSA|url=https://one.nhtsa.gov/people/injury/research/pub/alcohol-laws/08History/|website=NHTSA|publisher=National Highway Traffic Safety Administration|access-date=21 July 2017|date=July 2001}}</ref> |
||
| Line 138: | Line 138: | ||
=====Violent crime===== |
=====Violent crime===== |
||
{{Main|Crime|Felony|Alcohol-related crime}} |
{{Main|Crime|Felony|Alcohol-related crime}} |
||
Over 40% of all [[assault]]s and 40 to 50% of all [[murder]]s involve alcohol.<ref name="ButcherHooley2013" /> More than 43% of violent encounters with police involve alcohol.<ref name="ButcherHooley2013" /> Alcohol is implicated in more than two-thirds of cases of [[intimate partner violence]].<ref name="ButcherHooley2013" /> In 2002, it was estimated that 1 million violent crimes in the United States were related to alcohol use.<ref name="ButcherHooley2013" /> Alcohol is more commonly associated with both violent and non-violent crime than are drugs like |
Over 40% of all [[assault]]s and 40 to 50% of all [[murder]]s involve alcohol.<ref name="ButcherHooley2013" /> More than 43% of violent encounters with police involve alcohol.<ref name="ButcherHooley2013" /> Alcohol is implicated in more than two-thirds of cases of [[intimate partner violence]].<ref name="ButcherHooley2013" /> In 2002, it was estimated that 1 million violent crimes in the United States were related to alcohol use.<ref name="ButcherHooley2013" /> Alcohol is more commonly associated with both violent and non-violent crime than are drugs like marijuana.<ref name="ButcherHooley2013" /> |
||
====Health |
====Health consequences==== |
||
{{Main|Alcohol and health|Moderate drinking}} |
{{Main|Alcohol and health|Alcoholism#Moderate drinking}} |
||
[[ |
[[Alcohol use disorder]] is a major problem and many health problems as well as death can result from excessive alcohol use.<ref name="ButcherHooley2013" /><ref name="Friedman2011" /> Alcohol dependence is linked to a [[Life expectancy|lifespan]] that is reduced by about 12 years relative to the average person.<ref name="ButcherHooley2013" /> In 2004, it was estimated that 4% of deaths worldwide were attributable to alcohol use.<ref name="Friedman2011" /> Deaths from alcohol are split about evenly between acute causes (e.g., overdose, accidents) and chronic conditions.<ref name="Friedman2011" /> The leading chronic alcohol-related condition associated with death is [[alcoholic liver disease]].<ref name="Friedman2011" /> Alcohol dependence is also associated with [[cognitive impairment]] and [[organic brain syndrome|organic brain damage]].<ref name="ButcherHooley2013" /> Some researchers have found that even one alcoholic drink a day increases an individual's risk of health problems.<ref>{{Cite news|url=https://www.nytimes.com/2018/08/27/health/alcohol-drinking-health.html|title=How Much Alcohol Is Safe to Drink? None, Say These Researchers|access-date=2018-09-17|language=en}}</ref> |
||
===Adverse effects=== |
===Adverse effects=== |
||
Revision as of 08:11, 4 March 2021
 | |||
| |||
| Clinical data | |||
|---|---|---|---|
| Pronunciation | /ˈɛθənɒl/ | ||
| Other names | Absolute alcohol; Alcohol (USP); Cologne spirit; Drinking alcohol; Ethanol (JAN); Ethylic alcohol; EtOH; Ethyl alcohol; Ethyl hydrate; Ethyl hydroxide; Ethylol; Grain alcohol; Hydroxyethane; Methylcarbinol | ||
| Dependence liability | Moderate[1] | ||
| Addiction liability | Moderate (10–15%)[2] | ||
| Routes of administration | Common: by mouth, topical Uncommon: suppository, inhalation, ocular, insufflation,[3] injection[4] | ||
| Drug class | Analgesic; Depressants; Sedatives; Anxiolytics; Euphoriants; GABAA receptor positive modulators | ||
| ATC code | |||
| Legal status | |||
| Legal status |
| ||
| Pharmacokinetic data | |||
| Bioavailability | 80%+[5][6] | ||
| Protein binding | Weakly or not at all[5][6] | ||
| Metabolism | Liver (90%):[7][9] • Alcohol dehydrogenase • MEOS (CYP2E1) | ||
| Metabolites | Acetaldehyde; Acetate; Acetyl-CoA; Carbon dioxide; Water; Ethyl glucuronide; Ethyl sulfate | ||
| Onset of action | Peak concentrations:[7][5] • Range: 30–90 minutes • Mean: 45–60 minutes • Fasting: 30 minutes | ||
| Elimination half-life | Constant-rate elimination at typical concentrations:[8][9][7] • Range: 10–34 mg/dL/hour • Mean (men): 15 mg/dL/hour • Mean (women): 18 mg/dL/hr At very high concentrations (t1/2): 4.0–4.5 hours[6][5] | ||
| Duration of action | 6–16 hours (amount of time that levels are detectable)[10] | ||
| Excretion | • Major: metabolism (into carbon dioxide and water)[5] • Minor: urine, breath, sweat (5–10%)[7][5] | ||
| Identifiers | |||
| |||
| CAS Number | |||
| PubChem CID | |||
| IUPHAR/BPS | |||
| DrugBank | |||
| ChemSpider | |||
| UNII | |||
| KEGG | |||
| ChEBI | |||
| ChEMBL | |||
| PDB ligand | |||
| Chemical and physical data | |||
| Formula | C2H6O | ||
| Molar mass | 46.069 g·mol−1 | ||
| 3D model (JSmol) | |||
| Density | 0.7893 g/cm3 (at 20 °C)[11] | ||
| Melting point | −114.14 ± 0.03 °C (−173.45 ± 0.05 °F) [11] | ||
| Boiling point | 78.24 ± 0.09 °C (172.83 ± 0.16 °F) [11] | ||
| Solubility in water | Miscible | ||
| |||
| |||
Alcohol, sometimes referred to by the chemical name ethanol, is a psychoactive drug that is the active ingredient in drinks such as beer, wine, and distilled spirits (hard liquor).[12] It is one of the oldest and most common recreational substances, causing the characteristic effects of alcohol intoxication ("drunkenness").[13] Among other effects, alcohol produces happiness and euphoria, decreased anxiety, increased sociability, sedation, impairment of cognitive, memory, motor, and sensory function, and generalized depression of central nervous system function. Ethanol is only one of several types of alcohol, but it is the only type of alcohol that is found in alcoholic beverages or commonly used for recreational purposes; other alcohols such as methanol and isopropyl alcohol are significantly more toxic.[12] A mild, brief exposure to isopropanol, being only moderately more toxic than ethanol, is unlikely to cause any serious harm. Methanol, being profoundly more toxic than ethanol, is lethal in quantities as small as 10–15 milliliters (2–3 tsp).
Alcohol has a variety of short-term and long-term adverse effects. Short-term adverse effects include generalized impairment of neurocognitive function, dizziness, nausea, vomiting, and hangover-like symptoms. Alcohol can be addictive to humans, as in alcohol use disorder, and can result in dependence and withdrawal. It can have a variety of long-term adverse effects on health, for instance liver damage,[14] brain damage,[15] and its consumption is the fifth leading cause of cancer.[16][failed verification] The adverse effects of alcohol on health are most important when it is used in excessive quantities or with heavy frequency. However, some of them, such as increased risk of certain cancers, may occur even with light or moderate alcohol consumption.[17][18] In high amounts, alcohol may cause loss of consciousness or, in severe cases, death.
Alcohol works in the brain primarily by increasing the effects of a neurotransmitter called γ-aminobutyric acid, or GABA.[19] This is the major inhibitory neurotransmitter in the brain, and by facilitating its actions, alcohol suppresses the activity of the central nervous system.[19] The substance also directly affects a number of other neurotransmitter systems including those of glutamate, glycine, acetylcholine, and serotonin.[20][21] The pleasurable effects of alcohol ingestion are the result of increased levels of dopamine and endogenous opioids in the reward pathways of the brain.[22][23] Alcohol also has toxic and unpleasant actions in the body, many of which are mediated by its byproduct acetaldehyde.[24]
Alcohol has been produced and consumed by humans for its psychoactive effects for almost 10,000 years.[25] Drinking alcohol is generally socially acceptable and is legal in most countries, unlike with many other recreational substances. However, there are often restrictions on alcohol sale and use, for instance a minimum age for drinking and laws against public drinking and drinking and driving.[26] Alcohol has considerable societal and cultural significance and has important social roles in much of the world. Drinking establishments, such as bars and nightclubs, revolve primarily around the sale and consumption of alcoholic beverages, and parties, festivals, and social gatherings commonly involve alcohol consumption. Its use is also related to various societal problems, including driving accidents and fatalities, accidental injuries, sexual assaults, domestic abuse, and violent crime.[27] Alcohol remains illegal for sale and consumption in a number of countries, mainly in the Middle East.
Use and effects
Ethanol is typically consumed as a recreational substance by mouth in the form of alcoholic beverages such as beer, wine, and spirits. It is commonly used in social settings due to its capacity to enhance sociability.
The amount of ethanol in the body is typically quantified by blood alcohol content (BAC); weight of ethanol per unit volume of blood. Small doses of ethanol, in general, are stimulant-like[28] and produce euphoria and relaxation; people experiencing these symptoms tend to become talkative and less inhibited, and may exhibit poor judgement. At higher dosages (BAC > 1 g/L), ethanol acts as a central nervous system depressant,[28] producing at progressively higher dosages, impaired sensory and motor function, slowed cognition, stupefaction, unconsciousness, and possible death. Ethanol is commonly consumed as a recreational substance, especially while socializing, due to its psychoactive effects.
Caloric content
Ethanol is a source of energy and pure ethanol provides 7 calories per gram. For distilled spirits, a standard serving in the United States is 44 ml (1.5 US fl oz), which at 40% ethanol (80 proof), would be 14 grams and 98 calories. Wine and beer contain a similar range of ethanol quantity for servings of 150 ml (5 US fl oz) and 350 ml (12 US fl oz), respectively, but these beverages also contain non-ethanol food energy. A 150 ml serving of wine contains 100 to 130 calories. A 350 ml serving of beer contains 95 to 200 calories. According to the U.S. Department of Agriculture, based on NHANES 2013–2014 surveys, women in the US ages 20 and up consume on average 6.8 grams/day and men consume on average 15.5 grams/day.[29] Ignoring the non-alcohol contribution of those beverages, the average energy contributions are 48 and 108 cal/day, respectively. Alcoholic beverages are considered empty calorie foods because other than food energy they contribute no essential nutrients.
Toxicity
Alcohol has a variety of short-term and long-term adverse effects. It also has reinforcement-related adverse effects, including addiction, dependence, and withdrawal.
Social harm
Alcohol causes a plethora of detrimental effects in society, both to the individual and to others.[27] It is highly associated with automobile accidents, sexual assaults, and both violent and non-violent crime.[27] About one-third of arrests in the United States involve alcohol misuse.[27] Many emergency room visits also involve alcohol use.[27] As many as 15% of employees show problematic alcohol-related behaviors in the workplace, such as drinking before going to work or even drinking on the job.[27] Heavy drinking is associated with vulnerability to injury, marital discord, and domestic violence.[27] Alcohol use is directly related to considerable morbidity and mortality, for instance due to overdose and alcohol-related health problems.[31]
Alcohol-related crimes
Automobile accidents
A 2002 study found 41% of people fatally injured in traffic accidents were in alcohol-related crashes.[32] Misuse of alcohol is associated with more than 40% of deaths that occur in automobile accidents every year.[27] The risk of a fatal car accident increases exponentially with the level of alcohol in the driver's blood.[33] Most drunk driving laws in the United States governing the acceptable levels in the blood while driving or operating heavy machinery set typical upper limits of legal blood alcohol content (BAC) at 0.08%.[34]
Sexual assault
Alcohol is often used to facilitate sexual assault or rape.[35][36] Over 50% of reported rapes involve alcohol.[clarification needed][27] It is the most commonly used date rape drug.[37]
Violent crime
Over 40% of all assaults and 40 to 50% of all murders involve alcohol.[27] More than 43% of violent encounters with police involve alcohol.[27] Alcohol is implicated in more than two-thirds of cases of intimate partner violence.[27] In 2002, it was estimated that 1 million violent crimes in the United States were related to alcohol use.[27] Alcohol is more commonly associated with both violent and non-violent crime than are drugs like marijuana.[27]
Health consequences
Alcohol use disorder is a major problem and many health problems as well as death can result from excessive alcohol use.[27][31] Alcohol dependence is linked to a lifespan that is reduced by about 12 years relative to the average person.[27] In 2004, it was estimated that 4% of deaths worldwide were attributable to alcohol use.[31] Deaths from alcohol are split about evenly between acute causes (e.g., overdose, accidents) and chronic conditions.[31] The leading chronic alcohol-related condition associated with death is alcoholic liver disease.[31] Alcohol dependence is also associated with cognitive impairment and organic brain damage.[27] Some researchers have found that even one alcoholic drink a day increases an individual's risk of health problems.[38]
Adverse effects
Short-term effects

Central nervous system impairment
Alcohol causes generalized central nervous system depression, is a positive allosteric GABAA modulator and is associated and related with cognitive, memory or memory loss, motor, and sensory impairment. It slows and impairs cognition and reaction time and the cognitive skills, impairs judgement, interferes with motor function resulting in motor incoordination, loss of balance, confusion, sedation, numbness and slurred speech, impairs memory formation, and causes sensory impairment. At high concentrations, could induce amnesia, analgesia, spins, stupor, and unconsciousness as result of high levels of ethanol in blood.
At very high concentrations, could cause anterograde amnesia, markedly decreased heart rate, pulmonary aspiration, positional alcohol nystagmus (PAN), respiratory depression, shock, coma and death can result due to profound suppression of central nervous system function because to the alcohol overdose and can finish in consequent dysautonomia.
Gastrointestinal effects

Alcohol can cause nausea and vomiting in sufficiently high amounts (varies by person).
Alcohol stimulates gastric juice production, even when food is not present, and as a result, its consumption stimulates acidic secretions normally intended to digest protein molecules. Consequently, the excess acidity may harm the inner lining of the stomach. The stomach lining is normally protected by a mucosal layer that prevents the stomach from, essentially, digesting itself. However, in patients who have a peptic ulcer disease (PUD), this mucosal layer is broken down. PUD is commonly associated with the bacteria H. pylori. H. pylori secrete a toxin that weakens the mucosal wall, which as a result lead to acid and protein enzymes penetrating the weakened barrier. Because alcohol stimulates a person's stomach to secrete acid, a person with PUD should avoid drinking alcohol on an empty stomach. Drinking alcohol causes more acid release, which further damages the already-weakened stomach wall.[40] Complications of this disease could include a burning pain in the abdomen, bloating and in severe cases, the presence of dark black stools indicate internal bleeding.[41] A person who drinks alcohol regularly is strongly advised to reduce their intake to prevent PUD aggravation.[41]
Ingestion of alcohol can initiate systemic pro-inflammatory changes through two intestinal routes: (1) altering intestinal microbiota composition (dysbiosis), which increases lipopolysaccharide (LPS) release, and (2) degrading intestinal mucosal barrier integrity – thus allowing this (LPS) to enter the circulatory system. The major portion of the blood supply to the liver is provided by the portal vein. Therefore, while the liver is continuously fed nutrients from the intestine, it is also exposed to any bacteria and/or bacterial derivatives that breach the intestinal mucosal barrier. Consequently, LPS levels increase in the portal vein, liver and systemic circulation after alcohol intake. Immune cells in the liver respond to LPS with the production of reactive oxygen species (ROS), leukotrienes, chemokines and cytokines. These factors promote tissue inflammation and contribute to organ pathology.[42]
Allergic-like reactions
Ethanol-containing beverages can cause alcohol flush reactions, exacerbations of rhinitis and, more seriously and commonly, bronchoconstriction in patients with a history of asthma, and in some cases, urticarial skin eruptions, and systemic dermatitis. Such reactions can occur within 1–60 minutes of ethanol ingestion, and may be caused by:[43]
- genetic abnormalities in the metabolism of ethanol, which can cause the ethanol metabolite, acetaldehyde, to accumulate in tissues and trigger the release of histamine, or
- true allergy reactions to allergens occurring naturally in, or contaminating, alcoholic beverages (particularly wine and beer), and
- other unknown causes.
Long-term effects
Prolonged heavy consumption of alcohol can cause significant permanent damage to the brain and other organs resulting in disfunction or death.
Brain damage
Alcohol can cause brain damage, Wernicke's encephalopathy and Alcoholic Korsakoff syndrome (AKS) which frequently occur simultaneously, known as Wernicke–Korsakoff syndrome (WKS).[44] Lesions, or brain abnormalities, are typically located in the diencephalon which result in anterograde and retrograde amnesia, or memory loss.[44]
Liver damage
During the metabolism of alcohol via the respective dehydrogenases, NAD (nicotinamide adenine dinucleotide) is converted into reduced NAD. Normally, NAD is used to metabolize fats in the liver, and as such alcohol competes with these fats for the use of NAD. Prolonged exposure to alcohol means that fats accumulate in the liver, leading to the term 'fatty liver'. Continued consumption (such as in alcohol use disorder) then leads to cell death in the hepatocytes as the fat stores reduce the function of the cell to the point of death. These cells are then replaced with scar tissue, leading to the condition called cirrhosis.
Birth defects
Ethanol is classified as a teratogen.
This article needs additional citations for verification. (February 2016) |
According to the U.S. Centers for Disease Control (CDC), alcohol consumption by women who are not using birth control increases the risk of fetal alcohol syndrome. The CDC currently recommends complete abstinence from alcoholic beverages for women of child-bearing age who are pregnant, trying to become pregnant, or are sexually active and not using birth control.[45]
Cancer
IARC list ethanol in alcoholic beverages are classified as a Group 1 carcinogens in human beings and argues that "There is sufficient evidence and research showing the carcinogenicity of acetaldehyde (the major metabolite of ethanol) which is excreted by the liver enzyme when one drinks alcohol."[46]
Other effects
Frequent drinking of alcoholic beverages is a major contributing factor in cases of elevated blood levels of triglycerides.[47]
Reinforcement disorders
Addiction
Alcohol addiction is termed alcohol use disorder.
Two or more consecutive alcohol-free days a week have been recommended to improve health and break dependence.[48][49][50]
Dependence and withdrawal
Discontinuation of alcohol after extended heavy use and associated tolerance development (resulting in dependence) can result in withdrawal. Alcohol withdrawal can cause confusion, anxiety, insomnia, agitation, tremors, fever, nausea, vomiting, autonomic dysfunction, seizures, and hallucinations. In severe cases, death can result. Delirium tremens is a condition that requires people with a long history of heavy drinking to undertake an alcohol detoxification regimen.
Overdose
Death from ethanol consumption is possible when blood alcohol levels reach 0.4%. A blood level of 0.5% or more is commonly fatal. Levels of even less than 0.1% can cause intoxication, with unconsciousness often occurring at 0.3–0.4%.[51]
The oral median lethal dose (LD50) of ethanol in rats is 5,628 mg/kg. Directly translated to human beings, this would mean that if a person who weighs 70 kg (150 lb) drank a 500 mL (17 US fl oz) glass of pure ethanol, they would theoretically have a 50% risk of dying. Symptoms of ethanol overdose may include nausea, vomiting, central nervous system depression, coma, acute respiratory failure, or death
Interactions
Alcohol can intensify the sedation caused by other central nervous system depressants such as barbiturates, benzodiazepines, opioids, nonbenzodiazepines/Z-drugs (such as zolpidem and zopiclone), antipsychotics, sedative antihistamines, and certain antidepressants.[51] It interacts with cocaine in vivo to produce cocaethylene, another psychoactive substance.[52] Ethanol enhances the bioavailability of methylphenidate (elevated plasma dexmethylphenidate).[53][irrelevant citation] In combination with cannabis, ethanol increases plasma tetrahydrocannabinol levels, which suggests that ethanol may increase the absorption of tetrahydrocannabinol.[54]
Disulfiram-like drugs
Disulfiram
Disulfiram inhibits the enzyme acetaldehyde dehydrogenase, which in turn results in buildup of acetaldehyde, a toxic metabolite of ethanol with unpleasant effects. The medication or drug is commonly used to treat alcohol use disorder, and results in immediate hangover-like symptoms upon consumption of alcohol, this effect is widely known as disulfiram effect.
Metronidazole
One of the most important drug/food interactions is between alcohol and metronidazole.
Metronidazole is an antibacterial agent that kills bacteria by damaging cellular DNA and hence cellular function.[55] Metronidazole is usually given to people who have diarrhea caused by Clostridium difficile bacteria. C. difficile is one of the most common microorganisms that cause diarrhea and can lead to complications such as colon inflammation and even more severely, death.
Patients who are taking metronidazole are sometimes advised to avoid alcohol, even after 1 hour following the last dose. Although older data suggested a possible disulfiram-like effect of metronidazole, newer data has challenged this and suggests it does not actually have this effect.
Methanol and ethylene glycol
The rate-limiting steps for the elimination of ethanol are in common with certain other substances. As a result, the blood alcohol concentration can be used to modify the rate of metabolism of methanol and ethylene glycol. Methanol itself is not highly toxic, but its metabolites formaldehyde and formic acid are; therefore, to reduce the rate of production and concentration of these harmful metabolites, ethanol can be ingested.[56] Ethylene glycol poisoning can be treated in the same way.
Pharmacology
Dynamics
The precise mechanism of action of ethanol has proven elusive and remains not fully understood.[19][57] Identifying molecular targets for ethanol has proven unusually difficult, in large part due to its unique biochemical properties.[57] Specifically, ethanol is a very low molecular weight compound and is of exceptionally low potency in its actions, causing effects only at very high (millimolar (mM)) concentrations.[57][58] For these reasons, unlike with most drugs, it has not yet been possible to employ traditional biochemical techniques to directly assess the binding of ethanol to receptors or ion channels.[57][58] Instead, researchers have had to rely on functional studies to elucidate the actions of ethanol.[57] Moreover, although it has been established that ethanol modulates ion channels to mediate its effects,[21] ion channels are complex proteins, and their interactions and functions are complicated by diverse subunit compositions and regulation by conserved cellular signals (e.g. signaling lipids).[19][57]
Much progress has been made in understanding the pharmacodynamics of ethanol over the last few decades.[20][57] While no binding sites have been identified and established unambiguously for ethanol at present, it appears that it affects ion channels, in particular ligand-gated ion channels, to mediate its effects in the central nervous system.[19][20][21][57] Ethanol has specifically been found in functional assays to enhance or inhibit the activity of a variety of ion channels, including the GABAA receptor, the ionotropic glutamate AMPA, kainate, and NMDA receptors, the glycine receptor,[59] the nicotinic acetylcholine receptors,[60] the serotonin 5-HT3 receptor, voltage-gated calcium channels, and BK channels, among others.[19][20][21][61][62] However, many of these actions have been found to occur only at very high concentrations that may not be pharmacologically significant at recreational doses of ethanol, and it is unclear how or to what extent each of the individual actions is involved in the effects of ethanol.[57] In any case, ethanol has long shown a similarity in its effects to positive allosteric modulators of the GABAA receptor like benzodiazepines, barbiturates, and various general anesthetics.[19][57] Indeed, ethanol has been found to enhance GABAA receptor-mediated currents in functional assays.[19][57] In accordance, it is theorized and widely believed that the primary mechanism of action is as a GABAA receptor positive allosteric modulator.[19][57] However, the diverse actions of ethanol on other ion channels may be and indeed likely are involved in its effects as well.[20][57]
Recently, a study showed the accumulation of an unnatural lipid phosphatidylethanol (PEth) competes with PIP2 agonists sites on lipid-gated ion channels.[63] This presents a novel indirect mechanism and suggests that a metabolite, not the ethanol itself, can effect the primary targets of ethanol intoxication. Many of the primary targets of ethanol are known to bind PIP2 including GABAA receptors,[64] but the role of PEth will need to be investigated for each of the primary targets.
In 2007, it was discovered that ethanol potentiates extrasynaptic δ subunit-containing GABAA receptors at behaviorally relevant (as low as 3 mM) concentrations.[19][57][65] [66] This is in contrast to previous functional assays of ethanol on γ subunit-containing GABAA receptors, which it enhances only at far higher concentrations (> 100 mM) that are in excess of recreational concentrations (up to 50 mM).[19][57][67] Ro15-4513, a close analogue of the benzodiazepine antagonist flumazenil (Ro15-1788), has been found to bind to the same site as ethanol and to competitively displace it in a saturable manner.[57][65] In addition, Ro15-4513 blocked the enhancement of δ subunit-containing GABAA receptor currents by ethanol in vitro.[57] In accordance, the drug has been found to reverse many of the behavioral effects of low-to-moderate doses of ethanol in rodents, including its effects on anxiety, memory, motor behavior, and self-administration.[57][65] Taken together, these findings suggest a binding site for ethanol on subpopulations of the GABAA receptor with specific subunit compositions via which it interacts with and potentiates the receptor.[19][57][65][68]
Rewarding and reinforcing actions
The reinforcing effects of alcohol consumption are mediated by acetaldehyde generated by catalase and other oxidizing enzymes such as cytochrome P-4502E1 in the brain.[69] Although acetaldehyde has been associated with some of the adverse and toxic effects of ethanol, it appears to play a central role in the activation of the mesolimbic dopamine system.[70]
Ethanol's rewarding and reinforcing (i.e., addictive) properties are mediated through its effects on dopamine neurons in the mesolimbic reward pathway, which connects the ventral tegmental area to the nucleus accumbens (NAcc).[71][72] One of ethanol's primary effects is the allosteric inhibition of NMDA receptors and facilitation of GABAA receptors (e.g., enhanced GABAA receptor-mediated chloride flux through allosteric regulation of the receptor).[73] At high doses, ethanol inhibits most ligand-gated ion channels and voltage-gated ion channels in neurons as well.[73]
With acute alcohol consumption, dopamine is released in the synapses of the mesolimbic pathway, in turn heightening activation of postsynaptic D1 receptors.[71][72] The activation of these receptors triggers postsynaptic internal signaling events through protein kinase A, which ultimately phosphorylate cAMP response element binding protein (CREB), inducing CREB-mediated changes in gene expression.[71][72]
With chronic alcohol intake, consumption of ethanol similarly induces CREB phosphorylation through the D1 receptor pathway, but it also alters NMDA receptor function through phosphorylation mechanisms;[71][72] an adaptive downregulation of the D1 receptor pathway and CREB function occurs as well.[71][72] Chronic consumption is also associated with an effect on CREB phosphorylation and function via postsynaptic NMDA receptor signaling cascades through a MAPK/ERK pathway and CAMK-mediated pathway.[72] These modifications to CREB function in the mesolimbic pathway induce expression (i.e., increase gene expression) of ΔFosB in the NAcc,[72] where ΔFosB is the "master control protein" that, when overexpressed in the NAcc, is necessary and sufficient for the development and maintenance of an addictive state (i.e., its overexpression in the nucleus accumbens produces and then directly modulates compulsive alcohol consumption).[72][74][75][76]
Relationship between concentrations and effects
| mg/dL | mM | % v/v | Effects |
|---|---|---|---|
| 50 | 11 | 0.05% | Euphoria, talkativeness, relaxation, happiness, gladness, pleasure, joyfulness. |
| 100 | 22 | 0.1% | Central nervous system depression, anxiety supression, stress supression, sedation, nausea, possible vomiting, impaired motor and sensory function,impaired memory impaired cognition |
| >140 | 30 | >0.14% | Decreased blood flow to brain, slurred speech, double or blurry vission. |
| 300 | 65 | 0.3% | Stupefaction, confussion, numbness, dizzyness, loss of consciousness. |
| 400 | 87 | 0.4% | Ethylic intoxication, drunkeness, enebriation, alcohol poisoning or possible death. |
| 500 | 109 | >0.55% | Unconsciouness, Coma and Death. |
Recreational concentrations of ethanol are typically in the range of 1 to 50 mM.[67][19] Very low concentrations of 1 to 2 mM ethanol produce zero or undetectable effects except in alcohol-naive individuals.[67] Slightly higher levels of 5 to 10 mM, which are associated with light social drinking, produce measurable effects including changes in visual acuity, decreased anxiety, and modest behavioral disinhibition.[67] Further higher levels of 15 to 20 mM result in a degree of sedation and motor incoordination that is contraindicated with the operation of motor vehicles.[67] In jurisdictions in the United States, maximum blood alcohol levels for legal driving are about 17 to 22 mM.[78][79] In the upper range of recreational ethanol concentrations of 20 to 50 mM, depression of the central nervous system is more marked, with effects including complete drunkenness, profound sedation, amnesia, emesis, hypnosis, and eventually unconsciousness.[67][78] Levels of ethanol above 50 mM are not typically experienced by normal individuals and hence are not usually physiologically relevant; however, such levels – ranging from 50 to 100 mM – may be experienced by alcoholics with high tolerance to ethanol.[67] Concentrations above this range, specifically in the range of 100 to 200 mM, would cause death in all people except alcoholics.[67]
List of known actions in the central nervous system
Ethanol has been reported to possess the following actions in functional assays at varying concentrations:[58]
- GABAA receptor positive allosteric modulator (primarily of δ subunit-containing receptors)[73]
- NMDA receptor negative allosteric modulator[62][73]
- Increased levels of dopamine and endogenous opioids in the mesolimbic pathway, secondary to other actions[70][73]
- AMPA receptor negative allosteric modulator[62]
- Kainate receptor negative allosteric modulator[62]
- Glycine receptor positive allosteric modulator[59]
- Serotonin receptor positive allosteric modulator[59]
- Opioid receptor endogenous positive alloteric modulator[62]
- Muscarinic acetylcholine receptor positive allosteric modulator.
- Nicotinic acetylcholine receptor positive allosteric modulator[60][80]
- 5-HT3 receptor positive allosteric modulator
- Glycine reuptake inhibitor[81]
- Adenosine reuptake inhibitor[82]
- Dopamine reuptake inhibitor
- L-type calcium channel blocker
- GIRK channel opener
Some of the actions of ethanol on ligand-gated ion channels, specifically the nicotinic acetylcholine receptors and the glycine receptor, are dose-dependent, with potentiation or inhibition occurring dependent on ethanol concentration.[58] This seems to be because the effects of ethanol on these channels are a summation of positive and negative allosteric modulatory actions.[58]
Kinetics
Absorption
Ethanol can be taken orally, by inhalation, rectally, or by injection (e.g., intravenous),[7][83] though it is typically ingested simply via oral administration.[5] The oral bioavailability of ethanol is around 80% or more.[5][6] In fasting volunteers, blood levels of ethanol increase proportionally with the dose of ethanol administered.[83] Blood alcohol concentrations may be estimated by dividing the amount of ethanol ingested by the body weight of the individual and correcting for water dilution.[7] Peak circulating levels of ethanol are usually reached within a range of 30 to 90 minutes of ingestion, with an average of 45 to 60 minutes.[7][5]
Food in the gastrointestinal system and hence gastric emptying is the most important factor that influences the absorption of orally ingested ethanol.[7][83] The absorption of ethanol is much more rapid on an empty stomach than with a full one.[7] The delay in ethanol absorption caused by food is similar regardless of whether food is consumed just before, at the same time, or just after ingestion of ethanol.[7] The type of food, whether fat, carbohydrates, or protein, also is of little importance.[83] Not only does food slow the absorption of ethanol, but it also reduces the bioavailability of ethanol, resulting in lower circulating concentrations.[7] People who have fasted overnight have been found to reach peak ethanol concentrations more rapidly, at within 30 minutes of ingestion.[7]
Distribution
Upon ingestion, ethanol is rapidly distributed throughout the body.[5] It is distributed most rapidly to tissues with the greatest blood supply.[7] As such, ethanol primarily affects the brain, liver, and kidneys.[5] Other tissues with lower circulation, such as bone, require more time for ethanol to distribute into.[7] Ethanol crosses biological membranes and the blood–brain barrier easily, through a simple process of passive diffusion.[5][83] The volume of distribution of ethanol is around .55 L/kg (0.53 US pt/lb).[5] It is only weakly or not at all plasma protein bound.[5][6]
Metabolism
Approximately 90% of the metabolism of ethanol occurs in the liver.[7][9] This occurs predominantly via the enzyme alcohol dehydrogenase, which transforms ethanol into its metabolite acetaldehyde (ethanal).[7][9] Acetaldehyde is subsequently metabolized by the enzyme aldehyde dehydrogenase into acetate (ethanoate), which in turn is broken down into carbon dioxide and water.[7] Acetate also combines with coenzyme A to form acetyl-CoA, and hence may participate in metabolic pathways.[5] Alcohol dehydrogenase and aldehyde dehydrogenase are present at their highest concentrations in the liver, but are widely expressed throughout the body, and alcohol dehydrogenase may also be present in the stomach and small intestine.[5] Aside from alcohol dehydrogenase, the microsomal ethanol-oxidizing system (MEOS), specifically mediated by the cytochrome P450 enzyme CYP2E1, is the other major route of ethanol metabolism.[7][9] CYP2E1 is inducible by ethanol, so while alcohol dehydrogenase handles acute or low concentrations of ethanol, MEOS is predominant with higher concentrations or with repeated/chronic use.[7][9] A small amount of ethanol undergoes conjugation to form ethyl glucuronide and ethyl sulfate.[5] There may also be another metabolic pathway that metabolizes as much as 25 to 35% of ethanol at typical concentrations.[6]
At even low physiological concentrations, ethanol completely saturates alcohol dehydrogenase.[7] This is because ethanol has high affinity for the enzyme and very high concentrations of ethanol occur when it is used as a recreational substance.[7] For this reason, the metabolism of ethanol follows zero-order kinetics at typical physiological concentrations.[9] That is, ethanol does not have an elimination half-life (i.e., is not metabolized at an exponential rate), and instead, is eliminated from the circulation at a constant rate.[9][8] The mean elimination rates for ethanol are 15 mg/dL per hour for men and 18 mg/dL per hour for women, with a range of 10 to 34 mg/dL per hour.[9][7] At very high concentrations, such as in overdose, it has been found that the rate of elimination of ethanol is increased.[6] In addition, ethanol metabolism follows first-order kinetics at very high concentrations, with an elimination half-life of about 4 or 4.5 hours (which implies a clearance rate of approximately 6 L/hour/70 kg).[6][5] This seems to be because other processes, such as the MEOS/CYP2E1, also become involved in the metabolism of ethanol at higher concentrations.[5] However, the MEOS/CYP2E1 alone does not appear sufficient to fully explain the increase in ethanol metabolism rate.[6]
Some individuals have less effective forms of one or both of the metabolizing enzymes of ethanol, and can experience more marked symptoms from ethanol consumption than others.[84] However, those having acquired alcohol tolerance have a greater quantity of these enzymes, and metabolize ethanol more rapidly.[84]
Elimination
Ethanol is mainly eliminated from the body via metabolism into carbon dioxide and water.[7] Around 5 to 10% of ethanol that is ingested is eliminated unchanged in urine, breath, and sweat.[5] Ethanol or its metabolites may be detectable in urine for up to 96 hours (3-5 days) after ingestion.[5]
Chemistry
Ethanol is also known chemically as alcohol, ethyl alcohol, or drinking alcohol. It is a simple alcohol with a molecular formula of C2H6O and a molecular weight of 46.0684 g/mol. The molecular formula of ethanol may also be written as CH3−CH2−OH or as C2H5−OH. The latter can also be thought of as an ethyl group linked to a hydroxyl (alcohol) group and can be abbreviated as EtOH. Ethanol is a volatile, flammable, colorless liquid with a slight characteristic odor. Aside from its use as a psychoactive and recreational substance, ethanol is also commonly used as an antiseptic and disinfectant, a chemical and medicinal solvent, and a fuel.
Production
Ethanol is produced naturally as a byproduct of the metabolic processes of yeast and hence is present in any yeast habitat, including even endogenously in humans. It is manufactured as a petrochemical through hydration of ethylene or by brewing via fermentation of sugars with yeast (most commonly Saccharomyces cerevisiae). In the case of the latter, the sugars are commonly obtained from sources like steeped cereal grains (e.g., barley), grape juice, and sugarcane products (e.g., molasses, sugarcane juice). Petrochemical and yeast manufacturing routes both produce an ethanol–water mixture which can be further purified via distillation.
Analogues
This article may require cleanup to meet Wikipedia's quality standards. The specific problem is: Puncuation in complex sounding sentences. (February 2021) |
Ethanol has a variety of analogues, many of which have similar actions and effects. Methanol (methyl alcohol), isopropyl alcohol also called rubbing alcohol and 2-Methyl-2-Butanol 2M2B Ether or Butanol are lightly toxic and are not so much safe for human consumption.[12] Methanol is the most toxic alcohol; the toxicity of isopropyl alcohol lies between that of ethanol and methanol, and is about twice that of ethanol.[85] In general, higher alcohols are less toxic.[85] n-Butanol is reported to produce similar effects to those of ethanol and relatively low toxicity (one-sixth of that of ethanol in one rat study).[86][87] However, its vapors can produce eye irritation and inhalation can cause pulmonary edema.[85] Acetone (propanone) is a ketone rather than an alcohol, and is reported to produce similar toxic effects; it can be extremely damaging to the cornea.[85]
The tertiary alcohol tert-amyl alcohol (TAA), also known as 2-methylbutan-2-ol (2M2B), has a history of use as a hypnotic and anesthetic, as do other tertiary alcohols such as methylpentynol, ethchlorvynol, and chloralodol. Unlike primary alcohols like ethanol, these tertiary alcohols cannot be oxidized into aldehyde or carboxylic acid metabolites, which are often toxic, and for this reason, these compounds are safer in comparison.[88] Other relatives of ethanol with similar effects include chloral hydrate, paraldehyde, and many volatile and inhalational anesthetics (e.g., chloroform, diethyl ether, and isoflurane).
History
Alcohol was brewed as early as 7,000 to 6,650 BCE in northern China.[25] The earliest evidence of winemaking was dated at 6,000 to 5,800 BCE in Georgia in the South Caucasus.[89] Beer was likely brewed from barley as early as the 6th century BCE (600–500 BCE) in Egypt.[90] Pliny the Elder wrote about the golden age of winemaking in Rome, the 2nd century BCE (200–100 BCE), when vineyards were planted.[91]
Society and culture
Legal status
Alcohol is fully legal and available in most countries of the world.[92] However, laws banning alcohol are found in the Middle East and some Indian states as well as some Native American reservations in the United States.[92] In addition, besides are several regulations on alcohol sales and use in many countries throughout the world.[92] For instance, some countries have a minimum legal age to purchase or consume alcoholic beverages. Also, some countries have bans on public intoxication.[92] Drinking while driving or intoxicated driving is frequently outlawed and it may be illegal to have an open container of alcohol or liquor bottle in an automobile, bus or aircraft.[92]
See also
References
- ^ WHO Expert Committee on Problems Related to Alcohol Consumption : second report (PDF). Geneva, Switzerland: World Health Organization. 2007. p. 23. ISBN 9789241209441. Retrieved 3 March 2015.
...alcohol dependence (is) a substantial risk of regular heavy drinking...
- ^ Vengeliene V, Bilbao A, Molander A, Spanagel R (May 2008). "Neuropharmacology of alcohol addiction". British Journal of Pharmacology. 154 (2): 299–315. doi:10.1038/bjp.2008.30. PMC 2442440. PMID 18311194.
(Compulsive alcohol use) occurs only in a limited proportion of about 10–15% of alcohol users....
- ^ Stogner JM, Eassey JM, Baldwin JM, Miller BL (September 2014). "Innovative alcohol use: assessing the prevalence of alcohol without liquid and other non-oral routes of alcohol administration". Drug and Alcohol Dependence. 142: 74–8. doi:10.1016/j.drugalcdep.2014.05.026. PMID 25012895.
- ^ Gilman JM, Ramchandani VA, Crouss T, Hommer DW (January 2012). "Subjective and neural responses to intravenous alcohol in young adults with light and heavy drinking patterns". Neuropsychopharmacology. 37 (2): 467–77. doi:10.1038/npp.2011.206. PMC 3242308. PMID 21956438.
- ^ a b c d e f g h i j k l m n o p q r s t u Principles of Addiction: Comprehensive Addictive Behaviors and Disorders. Academic Press. 17 May 2013. pp. 162–. ISBN 978-0-12-398361-9.
- ^ a b c d e f g h i Holford NH (November 1987). "Clinical pharmacokinetics of ethanol". Clinical Pharmacokinetics. 13 (5): 273–92. doi:10.2165/00003088-198713050-00001. PMID 3319346. S2CID 19723995.
- ^ a b c d e f g h i j k l m n o p q r s t u v w Pohorecky LA, Brick J (1988). "Pharmacology of ethanol". Pharmacology & Therapeutics. 36 (2–3): 335–427. doi:10.1016/0163-7258(88)90109-x. PMID 3279433.
- ^ a b Becker CE (September 1970). "The clinical pharmacology of alcohol". California Medicine. 113 (3): 37–45. PMC 1501558. PMID 5457514.
- ^ a b c d e f g h i Levine B (2003). Principles of Forensic Toxicology. Amer. Assoc. for Clinical Chemistry. pp. 161–. ISBN 978-1-890883-87-4.
- ^ Iber FL (26 November 1990). Alcohol and Drug Abuse as Encountered in Office Practice. CRC Press. pp. 74–. ISBN 978-0-8493-0166-7.
- ^ a b c Haynes, William M., ed. (2011). CRC Handbook of Chemistry and Physics (92nd ed.). Boca Raton, FL: CRC Press. p. 3.246. ISBN 1-4398-5511-0.
- ^ a b c Collins SE, Kirouac M (2013). "Alcohol Consumption". Encyclopedia of Behavioral Medicine: 61–65. doi:10.1007/978-1-4419-1005-9_626. ISBN 978-1-4419-1004-2.
- ^ "10th Special Report to the U.S. Congress on Alcohol and Health: Highlights from Current Research" (PDF). National Institute of Health. National Institute on Alcohol Abuse and Alcoholism. June 2000. p. 134. Retrieved 21 October 2014.
The brain is a major target for the actions of alcohol, and heavy alcohol consumption has long been associated with brain damage. Studies clearly indicate that alcohol is neurotoxic, with direct effects on nerve cells. Chronic alcohol abusers are at additional risk for brain injury from related causes, such as poor nutrition, liver disease, and head trauma.
- ^ Bruha R, Dvorak K, Petrtyl J (March 2012). "Alcoholic liver disease". World Journal of Hepatology. 4 (3): 81–90. doi:10.4254/wjh.v4.i3.81. PMC 3321494. PMID 22489260.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Brust JC (April 2010). "Ethanol and cognition: indirect effects, neurotoxicity and neuroprotection: a review". International Journal of Environmental Research and Public Health. 7 (4): 1540–57. doi:10.3390/ijerph7041540. PMC 2872345. PMID 20617045.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ de Menezes RF, Bergmann A, Thuler LC (2013). "Alcohol consumption and risk of cancer: a systematic literature review". Asian Pacific Journal of Cancer Prevention. 14 (9): 4965–72. doi:10.7314/apjcp.2013.14.9.4965. PMID 24175760.
- ^ Bagnardi V, Rota M, Botteri E, Tramacere I, Islami F, Fedirko V, Scotti L, Jenab M, Turati F, Pasquali E, Pelucchi C, Bellocco R, Negri E, Corrao G, Rehm J, Boffetta P, La Vecchia C (February 2013). "Light alcohol drinking and cancer: a meta-analysis". Annals of Oncology. 24 (2): 301–8. doi:10.1093/annonc/mds337. PMID 22910838.
- ^ Yasinski, Emma, Even If You Don’t Drink Daily, Alcohol Can Mess With Your Brain, Discover (magazine), January 12, 2021
- ^ a b c d e f g h i j k l m Lobo IA, Harris RA (July 2008). "GABA(A) receptors and alcohol". Pharmacology Biochemistry and Behavior. 90 (1): 90–4. doi:10.1016/j.pbb.2008.03.006. PMC 2574824. PMID 18423561.
- ^ a b c d e Narahashi T, Kuriyama K, Illes P, Wirkner K, Fischer W, Mühlberg K, Scheibler P, Allgaier C, Minami K, Lovinger D, Lallemand F, Ward RJ, DeWitte P, Itatsu T, Takei Y, Oide H, Hirose M, Wang XE, Watanabe S, Tateyama M, Ochi R, Sato N (May 2001). "Neuroreceptors and ion channels as targets of alcohol". Alcoholism, Clinical and Experimental Research. 25 (5 Suppl ISBRA): 182S–188S. doi:10.1097/00000374-200105051-00030. PMID 11391069.
- ^ a b c d Olsen RW, Li GD, Wallner M, Trudell JR, Bertaccini EJ, Lindahl E, Miller KW, Alkana RL, Davies DL (March 2014). "Structural models of ligand-gated ion channels: sites of action for anesthetics and ethanol". Alcoholism, Clinical and Experimental Research. 38 (3): 595–603. doi:10.1111/acer.12283. PMC 3959612. PMID 24164436.
- ^ Charlet K, Beck A, Heinz A (2013). "The dopamine system in mediating alcohol effects in humans". Current Topics in Behavioral Neurosciences. 13: 461–88. doi:10.1007/7854_2011_130. ISBN 978-3-642-28719-0. PMID 21533679.
- ^ Méndez M, Morales-Mulia M (June 2008). "Role of mu and delta opioid receptors in alcohol drinking behaviour". Current Drug Abuse Reviews. 1 (2): 239–52. doi:10.2174/1874473710801020239. PMID 19630722.
- ^ Burcham PC (19 November 2013). An Introduction to Toxicology. Springer Science & Business Media. pp. 42–. ISBN 978-1-4471-5553-9.
- ^ a b McGovern PE, Zhang J, Tang J, Zhang Z, Hall GR, Moreau RA, Nuñez A, Butrym ED, Richards MP, Wang CS, Cheng G, Zhao Z, Wang C (December 2004). "Fermented beverages of pre- and proto-historic China". Proceedings of the National Academy of Sciences of the United States of America. 101 (51): 17593–8. Bibcode:2004PNAS..10117593M. doi:10.1073/pnas.0407921102. PMC 539767. PMID 15590771.
- ^ Alcohol : No Ordinary Commodity : Research and Public Policy. Babor, Thomas. (2nd ed.). Oxford: Oxford University Press. 2010. ISBN 978-0-19-955114-9. OCLC 656362316.
{{cite book}}: CS1 maint: others (link) - ^ a b c d e f g h i j k l m n o p q Butcher JN, Hooley JM, Mineka SM (25 June 2013). Abnormal Psychology. Pearson Education. p. 370. ISBN 978-0-205-97175-6.
- ^ a b Hendler RA, Ramchandani VA, Gilman J, Hommer DW (2013). "Stimulant and sedative effects of alcohol". Current Topics in Behavioral Neurosciences. 13: 489–509. doi:10.1007/7854_2011_135. ISBN 978-3-642-28719-0. PMID 21560041.
- ^ "What We Eat in America, NHANES 2013-2014" (PDF).
- ^ Nutt, David J; King, Leslie A; Phillips, Lawrence D (November 2010). "Drug harms in the UK: a multicriteria decision analysis". The Lancet. 376 (9752): 1558–1565. CiteSeerX 10.1.1.690.1283. doi:10.1016/S0140-6736(10)61462-6. PMID 21036393. S2CID 5667719.
- ^ a b c d e Friedman HS (26 August 2011). The Oxford Handbook of Health Psychology. Oxford University Press, USA. pp. 699–. ISBN 978-0-19-534281-9.
- ^ Hingson R, Winter M (2003). "Epidemiology and consequences of drinking and driving". Alcohol Research & Health. 27 (1): 63–78. PMC 6676697. PMID 15301401.
- ^ Naranjo CA, Bremner KE (January 1993). "Behavioural correlates of alcohol intoxication". Addiction. 88 (1): 25–35. doi:10.1111/j.1360-0443.1993.tb02761.x. PMID 8448514.
- ^ "Legislative History of .08 per se Laws – NHTSA". NHTSA. National Highway Traffic Safety Administration. July 2001. Retrieved 21 July 2017.
- ^ Hall JA, Moore CB (July 2008). "Drug facilitated sexual assault--a review". Journal of Forensic and Legal Medicine. 15 (5): 291–7. doi:10.1016/j.jflm.2007.12.005. PMID 18511003.
- ^ Beynon CM, McVeigh C, McVeigh J, Leavey C, Bellis MA (July 2008). "The involvement of drugs and alcohol in drug-facilitated sexual assault: a systematic review of the evidence". Trauma, Violence & Abuse. 9 (3): 178–88. doi:10.1177/1524838008320221. PMID 18541699. S2CID 27520472.
- ^ Schwartz RH, Milteer R, LeBeau MA (June 2000). "Drug-facilitated sexual assault ('date rape')". Southern Medical Journal. 93 (6): 558–61. doi:10.1097/00007611-200093060-00002. PMID 10881768.
- ^ "How Much Alcohol Is Safe to Drink? None, Say These Researchers". Retrieved 17 September 2018.
- ^ Nutt D, King LA, Saulsbury W, Blakemore C (March 2007). "Development of a rational scale to assess the harm of drugs of potential misuse". Lancet. 369 (9566): 1047–53. doi:10.1016/s0140-6736(07)60464-4. PMID 17382831. S2CID 5903121.
- ^ Overview of Peptic Ulcer Disease: Etiology and Pathophysiology. Medscape.com. Retrieved 27 April 2013.
- ^ a b Peptic Ulcer Disease (Stomach Ulcers) Cause, Symptoms, Treatments. Webmd.com. Retrieved 27 April 2013.
- ^ Patel S, Behara R, Swanson GR, Forsyth CB, Voigt RM, Keshavarzian A (October 2015). "Alcohol and the Intestine". Biomolecules. 5 (4): 2573–88. doi:10.3390/biom5042573. PMC 4693248. PMID 26501334.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Adams KE, Rans TS (December 2013). "Adverse reactions to alcohol and alcoholic beverages". Annals of Allergy, Asthma & Immunology. 111 (6): 439–45. doi:10.1016/j.anai.2013.09.016. PMID 24267355.
- ^ a b Arts, Nicolaas JM; Walvoort, Serge JW; Kessels, Roy PC (27 November 2017). "Korsakoff's syndrome: a critical review". Neuropsychiatric Disease and Treatment. 13: 2875–2890. doi:10.2147/NDT.S130078. ISSN 1176-6328. PMC 5708199. PMID 29225466.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ "More than 3 million US women at risk for alcohol-exposed pregnancy". Centers for Disease Control and Prevention. Retrieved 3 March 2016.
'drinking any alcohol at any stage of pregnancy can cause a range of disabilities for their child,' said Coleen Boyle, Ph.D., director of CDC's National Center on Birth Defects and Developmental Disabilities.
- ^ Agents Classified by the IARC Monographs, Volumes 1–111 Archived 25 October 2011 at the Wayback Machine. monographs.iarc.fr
- ^ "Triglycerides". American Heart Association. Archived from the original on 27 August 2007. Retrieved 4 September 2007.
- ^ Tomlinson, Angie (26 June 2018). "Tips and Tricks on How to Cut Down on the Booze". The West Australian. Seven West Media (WA). Retrieved 22 March 2019.
- ^ "'Middle-Aged' Urged to Have Alcohol-free Day". The Big Alcohol Conversation. Greater Manchester Combined Authority. Retrieved 22 March 2019.[permanent dead link]
- ^ "Alcohol". British Liver Trust. Retrieved 22 March 2019.
- ^ a b Yost DA (2002). "Acute care for alcohol intoxication" (PDF). 112 (6). Postgraduate Medicine Online. Archived from the original (PDF) on 14 December 2010. Retrieved 29 September 2007.
{{cite journal}}: Cite journal requires|journal=(help) - ^ Laizure SC, Mandrell T, Gades NM, Parker RB (January 2003). "Cocaethylene metabolism and interaction with cocaine and ethanol: role of carboxylesterases". Drug Metabolism and Disposition. 31 (1): 16–20. doi:10.1124/dmd.31.1.16. PMID 12485948.
- ^ Sakalo VS, Romanenko AM, Klimenko IA, Persidskiĭ I (1988). "[Effects of chemotherapy on regional metastases of non-seminomatous tumors of the testis]". Voprosy Onkologii. 34 (10): 1219–24. PMID 3188424.
- ^ Lukas SE, Orozco S (October 2001). "Ethanol increases plasma Delta(9)-tetrahydrocannabinol (THC) levels and subjective effects after marihuana smoking in human volunteers". Drug and Alcohol Dependence. 64 (2): 143–9. doi:10.1016/S0376-8716(01)00118-1. PMID 11543984.
- ^ Repchinsky C (ed.) (2012). Compendium of pharmaceuticals and specialties, Ottawa: Canadian Pharmacists Association.[full citation needed]
- ^ McCoy HG, Cipolle RJ, Ehlers SM, Sawchuk RJ, Zaske DE (November 1979). "Severe methanol poisoning. Application of a pharmacokinetic model for ethanol therapy and hemodialysis". The American Journal of Medicine. 67 (5): 804–7. doi:10.1016/0002-9343(79)90766-6. PMID 507092.
- ^ a b c d e f g h i j k l m n o p q r s Santhakumar V, Wallner M, Otis TS (May 2007). "Ethanol acts directly on extrasynaptic subtypes of GABAA receptors to increase tonic inhibition". Alcohol. 41 (3): 211–21. doi:10.1016/j.alcohol.2007.04.011. PMC 2040048. PMID 17591544.
- ^ a b c d e Spanagel R (April 2009). "Alcoholism: a systems approach from molecular physiology to addictive behavior". Physiological Reviews. 89 (2): 649–705. doi:10.1152/physrev.00013.2008. PMID 19342616.
- ^ a b c Söderpalm B, Lidö HH, Ericson M (November 2017). "The Glycine Receptor-A Functionally Important Primary Brain Target of Ethanol". Alcoholism, Clinical and Experimental Research. 41 (11): 1816–1830. doi:10.1111/acer.13483. PMID 28833225.
- ^ a b Wu J, Gao M, Taylor DH (March 2014). "Neuronal nicotinic acetylcholine receptors are important targets for alcohol reward and dependence". Acta Pharmacologica Sinica. 35 (3): 311–5. doi:10.1038/aps.2013.181. PMC 4647894. PMID 24464050.
- ^ Dopico AM, Bukiya AN, Kuntamallappanavar G, Liu J (2016). "Modulation of BK Channels by Ethanol". International Review of Neurobiology. 128: 239–79. doi:10.1016/bs.irn.2016.03.019. ISBN 978-0-12-803619-8. PMC 5257281. PMID 27238266.
- ^ a b c d e Möykkynen T, Korpi ER (July 2012). "Acute effects of ethanol on glutamate receptors". Basic & Clinical Pharmacology & Toxicology. 111 (1): 4–13. doi:10.1111/j.1742-7843.2012.00879.x. PMID 22429661.
- ^ Chung, HW; Petersen, EN; Cabanos, C; Murphy, KR; Pavel, MA; Hansen, AS; Ja, WW; Hansen, SB (18 January 2019). "A Molecular Target for an Alcohol Chain-Length Cutoff". Journal of Molecular Biology. 431 (2): 196–209. doi:10.1016/j.jmb.2018.11.028. PMC 6360937. PMID 30529033.
- ^ Laverty, D; Desai, R; Uchański, T; Masiulis, S; Stec, WJ; Malinauskas, T; Zivanov, J; Pardon, E; Steyaert, J; Miller, KW; Aricescu, AR (January 2019). "Cryo-EM structure of the human α1β3γ2 GABAA receptor in a lipid bilayer". Nature. 565 (7740): 516–520. doi:10.1038/s41586-018-0833-4. PMC 6364807. PMID 30602789.
- ^ a b c d Wallner M, Olsen RW (May 2008). "Physiology and pharmacology of alcohol: the imidazobenzodiazepine alcohol antagonist site on subtypes of GABAA receptors as an opportunity for drug development?". British Journal of Pharmacology. 154 (2): 288–98. doi:10.1038/bjp.2008.32. PMC 2442438. PMID 18278063.
- ^ Alkattan, A.; Alsalameen, E.; Ahmed, A. Central Nervous System Depressant Drugs: Updated Review. Preprints 2021, 2021010503 (doi: 10.20944/preprints202101.0503.v1).
- ^ a b c d e f g h Harrison NL, Skelly MJ, Grosserode EK, Lowes DC, Zeric T, Phister S, Salling MC (August 2017). "Effects of acute alcohol on excitability in the CNS". Neuropharmacology. 122: 36–45. doi:10.1016/j.neuropharm.2017.04.007. PMC 5657304. PMID 28479395.
- ^ Förstera B, Castro PA, Moraga-Cid G, Aguayo LG (2016). "Potentiation of Gamma Aminobutyric Acid Receptors (GABAAR) by Ethanol: How Are Inhibitory Receptors Affected?". Frontiers in Cellular Neuroscience. 10: 114. doi:10.3389/fncel.2016.00114. PMC 4858537. PMID 27199667.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Karahanian E, Quintanilla ME, Tampier L, Rivera-Meza M, Bustamante D, Gonzalez-Lira V, Morales P, Herrera-Marschitz M, Israel Y (April 2011). "Ethanol as a prodrug: brain metabolism of ethanol mediates its reinforcing effects". Alcoholism, Clinical and Experimental Research. 35 (4): 606–12. doi:10.1111/j.1530-0277.2011.01439.x. PMC 3142559. PMID 21332529.
- ^ a b Melis M, Enrico P, Peana AT, Diana M (November 2007). "Acetaldehyde mediates alcohol activation of the mesolimbic dopamine system". The European Journal of Neuroscience. 26 (10): 2824–33. doi:10.1111/j.1460-9568.2007.05887.x. PMID 18001279. S2CID 25110014.
- ^ a b c d e "Alcoholism – Homo sapiens (human) Database entry". KEGG Pathway. 29 October 2014. Retrieved 9 February 2015.
- ^ a b c d e f g h Kanehisa Laboratories (29 October 2014). "Alcoholism – Homo sapiens (human)". KEGG Pathway. Retrieved 31 October 2014.
- ^ a b c d e Malenka RC, Nestler EJ, Hyman SE (2009). "Chapter 15: Reinforcement and Addictive Disorders". In Sydor A, Brown RY (eds.). Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (2nd ed.). New York: McGraw-Hill Medical. p. 372. ISBN 978-0-07-148127-4.
- ^ Ruffle JK (November 2014). "Molecular neurobiology of addiction: what's all the (Δ)FosB about?". The American Journal of Drug and Alcohol Abuse. 40 (6): 428–37. doi:10.3109/00952990.2014.933840. PMID 25083822. S2CID 19157711.
- ^ Nestler EJ (December 2013). "Cellular basis of memory for addiction". Dialogues in Clinical Neuroscience. 15 (4): 431–43. PMC 3898681. PMID 24459410.
Despite the Importance of Numerous Psychosocial Factors, at its Core, Drug Addiction Involves a Biological Process: the ability of repeated exposure to a drug of abuse to induce changes in a vulnerable brain that drive the compulsive seeking and taking of drugs, and loss of control over drug use, that define a state of addiction. ... A large body of literature has demonstrated that such ΔFosB induction in D1-type NAc neurons increases an animal's sensitivity to drug as well as natural rewards and promotes drug self-administration, presumably through a process of positive reinforcement
- ^ Robison AJ, Nestler EJ (October 2011). "Transcriptional and epigenetic mechanisms of addiction". Nature Reviews. Neuroscience. 12 (11): 623–37. doi:10.1038/nrn3111. PMC 3272277. PMID 21989194.
- ^ Pohorecky LA, Brick J (1988). "Pharmacology of ethanol". Pharmacology & Therapeutics. 36 (2–3): 335–427. doi:10.1016/0163-7258(88)90109-X. PMID 3279433.
- ^ a b Liu Y, Hunt WA (6 December 2012). The "Drunken" Synapse: Studies of Alcohol-Related Disorders. Springer Science & Business Media. pp. 40–. ISBN 978-1-4615-4739-6.
- ^ Rubin R, Strayer DS, Rubin E, McDonald JM (2008). Rubin's Pathology: Clinicopathologic Foundations of Medicine. Lippincott Williams & Wilkins. pp. 257–. ISBN 978-0-7817-9516-6.
- ^ Steffensen SC, Shin SI, Nelson AC, Pistorius SS, Williams SB, Woodward TJ, Park HJ, Friend L, Gao M, Gao F, Taylor DH, Foster Olive M, Edwards JG, Sudweeks SN, Buhlman LM, Michael McIntosh J, Wu J (September 2017). "α6 subunit-containing nicotinic receptors mediate low-dose ethanol effects on ventral tegmental area neurons and ethanol reward". Addiction Biology. 23 (5): 1079–1093. doi:10.1111/adb.12559. PMC 5849490. PMID 28901722.
- ^ Sitte H, Freissmuth M (2 August 2006). Neurotransmitter Transporters. Springer Science & Business Media. pp. 472–. ISBN 978-3-540-29784-0.
- ^ Allen-Gipson DS, Jarrell JC, Bailey KL, Robinson JE, Kharbanda KK, Sisson JH, Wyatt TA (May 2009). "Ethanol blocks adenosine uptake via inhibiting the nucleoside transport system in bronchial epithelial cells". Alcoholism, Clinical and Experimental Research. 33 (5): 791–8. doi:10.1111/j.1530-0277.2009.00897.x. PMC 2940831. PMID 19298329.
- ^ a b c d e Begleiter H, Kissin B (1996). The Pharmacology of Alcohol and Alcohol Dependence. Oxford University Press. pp. 18–. ISBN 978-0-19-510094-5.
- ^ a b Agarwal DP, Goedde HW (April 1992). "Pharmacogenetics of alcohol metabolism and alcoholism". Pharmacogenetics. 2 (2): 48–62. doi:10.1097/00008571-199204000-00002. PMID 1302043.
- ^ a b c d Philp RB (15 September 2015). Ecosystems and Human Health: Toxicology and Environmental Hazards, Third Edition. CRC Press. pp. 216–. ISBN 978-1-4987-6008-9.
- ^ n-Butanol (PDF), SIDS Initial Assessment Report, Geneva: United Nations Environment Programme, April 2005.
- ^ McCreery MJ, Hunt WA (July 1978). "Physico-chemical correlates of alcohol intoxication". Neuropharmacology. 17 (7): 451–61. doi:10.1016/0028-3908(78)90050-3. PMID 567755. S2CID 19914287.
- ^ Carey, Francis (2000). Organic Chemistry (4 ed.). ISBN 0-07-290501-8. Retrieved 5 February 2013.
- ^ McGovern P, Jalabadze M, Batiuk S, Callahan MP, Smith KE, Hall GR, Kvavadze E, Maghradze D, Rusishvili N, Bouby L, Failla O, Cola G, Mariani L, Boaretto E, Bacilieri R, This P, Wales N, Lordkipanidze D (November 2017). "Early Neolithic wine of Georgia in the South Caucasus". Proceedings of the National Academy of Sciences of the United States of America. 114 (48): E10309–E10318. doi:10.1073/pnas.1714728114. PMC 5715782. PMID 29133421.
- ^ Rosso AM (2012). "Beer and wine in antiquity: beneficial remedy or punishment imposed by the Gods?". Acta Medico-Historica Adriatica. 10 (2): 237–62. PMID 23560753.
- ^ Brostrom GG, Brostrom J (30 December 2008). The Business of Wine: An Encyclopedia: An Encyclopedia. ABC-CLIO. pp. 6–. ISBN 978-0-313-35401-4.
- ^ a b c d e Boyle P (7 March 2013). Alcohol: Science, Policy and Public Health. OUP Oxford. pp. 363–. ISBN 978-0-19-965578-6.
Further reading
- The National Institute on Alcohol Abuse and Alcoholism maintains a database of alcohol-related health effects. ETOH Archival Database (1972–2003) Alcohol and Alcohol Problems Science Database.
External links
- ChEBI – biology related
- Kyoto Encyclopedia of Genes and Genomes signal transduction pathway: KEGG – human alcohol addiction
- 17β-Hydroxysteroid dehydrogenase inhibitors
- 5-HT3 agonists
- AMPA receptor antagonists
- Adenosine reuptake inhibitors
- Alcohol dehydrogenase inhibitors
- Alcohol
- Alcohols
- Analgesics
- Anxiolytics
- Calcium channel blockers
- Dopamine agonists
- Drinking culture
- Drug culture
- Drugs acting on the nervous system
- Ethanol
- Euphoriants
- GABAA receptor positive allosteric modulators
- General anesthetics
- Glycine reuptake inhibitors
- Hepatotoxins
- Hypnotics
- IARC Group 1 carcinogens
- Kainate receptor antagonists
- NMDA receptor antagonists
- Neurotoxins
- Nicotinic agonists
- Psychoactive drugs
- Sedatives
- Teratogens


